2020 Volume 84 Issue 3 Pages 384-385
2020 Volume 84 Issue 3 Pages 384-385
The number of patients with coronary artery disease (CAD) has increased worldwide because of the high prevalence of glucose intolerance, hypertension and dyslipidemia, resulting in not only a medical but also an economic burden even after the robust development of drugs and treatment procedures. Throughout the decades, great efforts have been paid to overcome CAD, and the inflammatory reactions followed by organic remodeling of the plaque in diseased vessels have been elucidated as the central dogma of atherosclerosis. On the other hand, significant contributions by Japanese researchers proposed coronary vasoconstriction as a distinctive cause of a specific type of angina, which had been mentioned as “variant angina” in Western countries since Prinzmetal et al first described this disease in 1959.1 This type of angina, referred to as coronary spastic angina (CSA), has been reported to show a definitely higher prevalence in East Asian countries, including Japan,2 than in others. In patients with CSA, both impaired release and metabolism of nitric oxide (NO) play the central role in the pathological changes of coronary arteries. Acetylcholine used for a diagnostic test for CSA in clinically diagnosed angina patients without organic disease induces NO release from the healthy endothelium, which results in vasodilation, but causes direct vasoconstriction of smooth muscles in impaired endothelium. However, neither abnormal NO synthesis nor metabolism explains the high prevalence of CSA in the Asian population. One genome-wide association study revealed in 2012 that single-nucleotide polymorphisms from loci near aldehyde dehydrogenase 2 (ALDH2) showed a strong association with CAD.3 Following that report, with perfect timing in 2015, Mizuno et al published their intriguing paper reporting that an ALDH2 variant is associated with CSA in the East Asian population.4 The human genome encodes 19 ALDH enzymes, and ALDH2 among them is particularly important in various physiological reactions. Most of all, the main and most well-known function is detoxification of acetaldehyde after ethanol intake (Figure); it is well established that the mutation of ALDH2, described as ALDH2*2, has remarkably reduced enzymatic activity compared with the wild type (ALDH2*1) and is common among Mongoloid ethnic group (35–45%), but quite rare in other ethnic background, including Caucasians.5 This phenomenon explains well the alcohol flushing syndrome that is common only in Asian populations. In their paper, Mizuno et al analyzed 202 Japanese patients with CSA and found that ALDH2*2 was prevalent in patients with alcohol flushing syndrome and also independently associated with CSA, suggesting that the distribution of ALDH2*2 can be, at least in part, the cause of the high prevalence of CSA in East Asian countries.
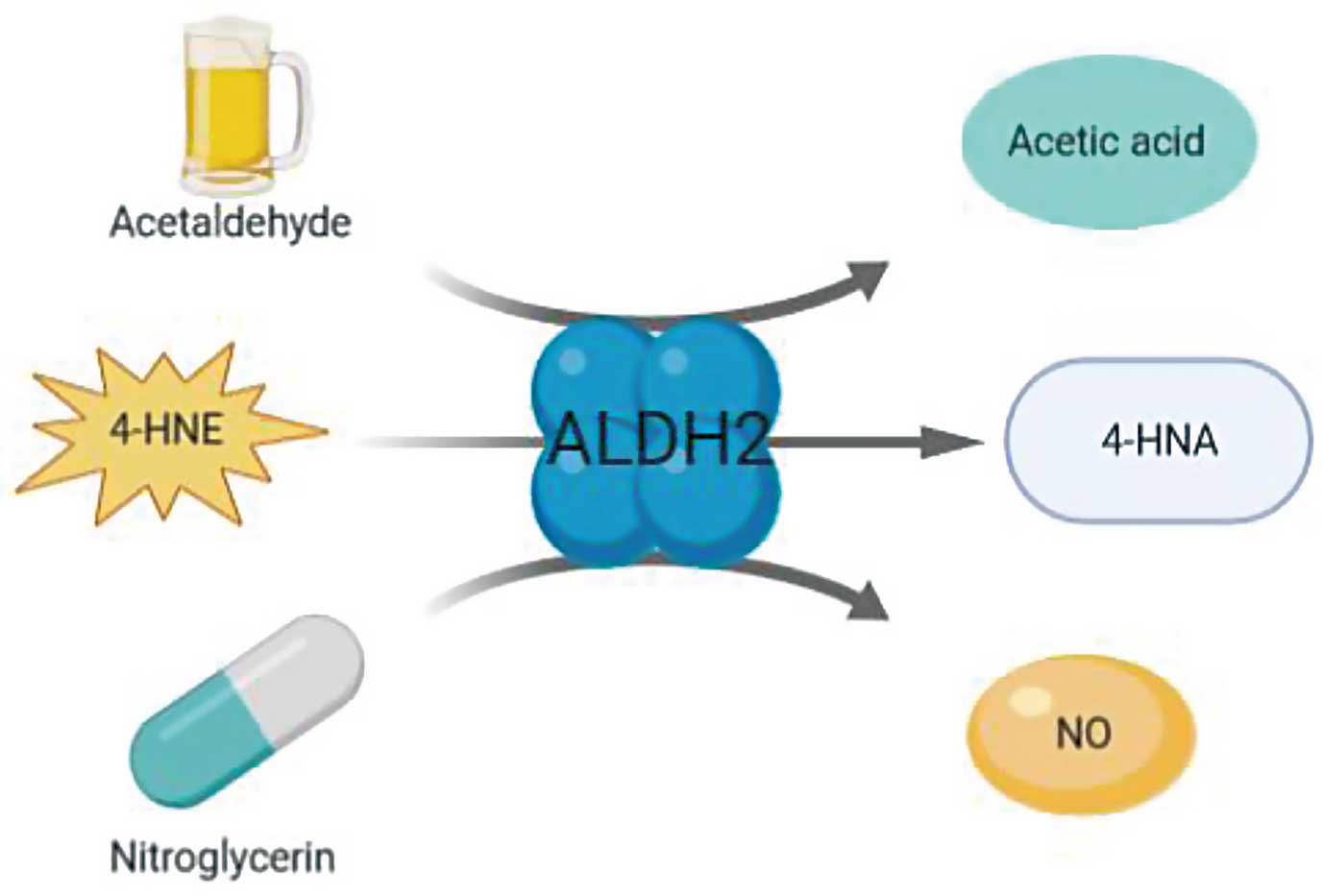
Major biological reactions mediated by aldehyde dehydrogenase 2 (ALDH2). ALDH2 detoxifies substances including acetaldehyde and 4-HNE, both of which are known to cause toxic damage to various tissues including the heart. ALDH2 is also required to generate NO from nitroglycerin. 4-HNE, 4-hydroxynonenal; 4-HNA, 4-hydroxy-trans-2-nonenoic acid; NO, nitric oxide.
Article p 479
The enzymatic reaction by ALDH2 is not limited to alcohol metabolism. The most important reactions catalyzed by ALDH2 in the cardiovascular field are detoxification of 4-hydroxynonenal (4-HNE), a toxic endproduct of polyunsaturated fatty acids on the membrane under excessive reactive oxygen species, and biotransformation of nitroglycerin into NO (Figure). Nitroglycerin such as glyceryl trinitrate (GTN) generates NO to show a vasodilatory effect and this reaction is mediated by ALDH2. However, GTN itself provokes inactivation of ALDH2 in several mechanisms resulting in GTN tolerance.6 As expected, ALDH2*2 reduces the effect of GTN,7 but whether the ALDH2*2 allele affects the development and severity of GTN tolerance in patients with CSA has not been well elucidated until now.
In this issue of the Journal, Mizuno’s group8 investigated the GTN tolerance in patients with CSA. The study enrolled 55 patients diagnosed as CSA through coronary angiography using the acetylcholine test. The numbers of participants with (ALDH2*2 group) and without the ALDH2*2 allele (ALDH2*1 group) were 24 and 31, respectively. The basic characteristics of the patients in each group did not show significant differences except for the prevalence of alcohol flushing syndrome and habitual drinking (91.7% vs. 32.3%, 37.5% vs. 70.6% in ALDH2*2 vs. ALDH2*1 group, respectively). To determine the effect of the ALDH2*2 allele on GTN tolerance, they measured both nitroglycerin-mediated dilation (NMD) and flow-mediated dilation (FMD) before and after administration of continuous GTN for 48 hours, where FMD reflected NO release from endothelial cells under shear stress while NMD represented GTN-mediated NO generation in the endothelium. As expected, both NMD and FMD decreased after GTN, indicating that GTN leads to endothelial dysfunction. However, FMD decreased to the same extent in both groups, whereas NMD decreased more in the ALDH2*2 group. Actually, the NMD change rate was significantly larger in the ALDH2*2 group (−67.9 vs. −39.9, P=0.0081), but the FMD change rate failed to show a significant difference, suggesting that the deterioration in GTN tolerance was more severe in patients with CSA and the ALDH2*2 allele.
These findings allow us to re-evaluate the treatment strategies for CSA patients. As shown in this study,8 as well as in other consistent reports,9,10 chronic use of GTN itself may become a risk for inducing adverse clinical outcomes, at least in part, through endothelial dysfunction. The impaired release and generation of NO indicates decreased capacity to control vascular tone, leading to a lack of dynamic control of blood flow, which is obviously disadvantageous for maintaining cardiovascular homeostasis. We have to carefully evaluate the absolute pathological effect of the difference in NMD after GTN treatment in this study (6.0% vs. 12.2% in ALDH2*2 vs. ALDH2*1, respectively) because GTN tolerance was not evaluated by clinical outcome such as angina. However, it is still noteworthy that individuals with the ALDH2*2 allele may suffer more from GTN treatment-induced endothelial dysfunction, especially among CSA patients.
The aforementioned information leads naturally to other questions. Even in the Japanese CSA patients who participated in this study, nearly half did not have the ALDH2*2 allele, which suggests the existence of other backgrounds specific to Asian ethnicity that may or may not be related to the function of ALDH2. Also, whether the epidemiological characteristics of CSA, such as a high prevalence in the fourth to fifth decades of life and association with smoking and male sex, have correlations with ALDH2*2 may give an important insight into the biological etiology of CSA. Additionally, it is of interest to unveil if ALDH2*2 in the Asian population has an effect on cardiovascular diseases through effects on pathways including, but not limited to, NO and 4-HNE.
Both CSA and the alcohol flushing syndrome are known to be common almost solely in Asians, but the hidden link via ALDH2*2 has just started to be unveiled. Because the culprit genotype is mainly distributed among the East Asian population, further studies to investigate the biology and clinical importance of CSA will be encouraged in these countries.
M.K. is a member of Circulation Journal ’ Editorial Team.