2020 Volume 84 Issue 8 Pages 1312-1319
2020 Volume 84 Issue 8 Pages 1312-1319
Background: The latest guidelines recommend early intervention in adult atrial septal defect (ASD) patients with signs of right ventricular (RV) enlargement. However, the criteria of RV enlargement for optimal intervention remain unclear. We investigated the preoperative determinants for normalizing the RV volume after transcatheter closure of ASD in adults.
Methods and Results: We retrospectively analyzed 52 ASD patients who underwent transcatheter closure. Cardiac magnetic resonance imaging (CMR) measured RV volume before and 1 year after the closure. The patients were divided into normalized (postoperative RV end-systolic volume index [RVESVI] <47 mL/m2 and end-diastolic volume index [RVEDVI] <108 mL/m2) and non-normalized (postoperative RVESVI ≥47 mL/m2 or RVEDVI ≥108 mL/m2) groups. Preoperative RVESVI was significantly smaller (72 mL/m2 vs. 80 mL/m2) and RVEF was higher (56% vs. 51%) in the normalized group compared with the non-normalized group. Receiver-operating characteristic analysis for the normalization of postoperative RV volume showed that the preoperative threshold value of RVESVI was 75 mL/m2. In addition, multivariate analysis showed that preoperative RVESVI was an independent predictor for normalization of RV volume.
Conclusions: Preoperative RVESVI is an independent predictor for normalization of RV volume at 1 year after transcatheter closure of ASD in adults. Early intervention before RVESVI reaches 75 mL/m2 may confer optimal timing for normalizing RV volume.
Atrial septal defect (ASD) is a common congenital heart disease in adults,1 which if left untreated, can lead to progressive right ventricular (RV) volume overload that decreases left ventricular (LV) filling pressure and cardiac output.2 Transcatheter closure of ASD has become established as a secure and effective treatment for ASD,3–5 because it is much less invasive than surgical repair and offers the advantages of cosmetic superiority and shorter hospital stay.5,6 It is now an alternative to surgical repair for ASD in many centers worldwide.
Recent clinical studies have indicated that transcatheter closure reduces symptoms, such as dyspnea, by reducing the RV volume in ASD patients.7,8 However, after transcatheter closure, some patients have shown impaired exercise tolerance and reduced quality of life due to residual RV enlargement and subsequent dysfunction.9,10 Thus, it is important that ASD closure prevents long-term RV enlargement. According to the latest ESC and AHA/ACC guidelines, early intervention for ASD is recommended as class I in the patients with signs of right atrial and/or RV enlargement despite their symptoms.11,12 However, the preoperative threshold for normalizing the RV volume after transcatheter closure of ASD remains unclear.
The present study aimed to determine the preoperative threshold of RV volume for its normalization after transcatheter closure of ASD in adults using cardiac magnetic resonance imaging (CMR), the gold standard for precise evaluation of RV volume.13,14 Moreover, we assessed possible influential factors related to normalization of RV volume after transcatheter closure.
We retrospectively studied 67 consecutive patients aged >15 years who had undergone transcatheter closure of ASD at Kyushu University Hospital from July 2014 to December 2016. We excluded 11 patients for whom CMR data were unavailable because of implantation of permanent pacemaker in 2 patients, claustrophobia in 1 patient, allergy to contrast agent in 1 patient, pregnancy in 1 patient, and no follow-up CMR in 6 patients. In addition, we excluded 4 patients because of prior old myocardial infarction in 1 patient, pulmonary artery stenosis in 1 patient, coarctation of the aorta in 1 patient, and staged transcatheter closure of ASD for multiple defects in 1 patient. Finally, we analyzed the remaining 52 patients (Figure 1).
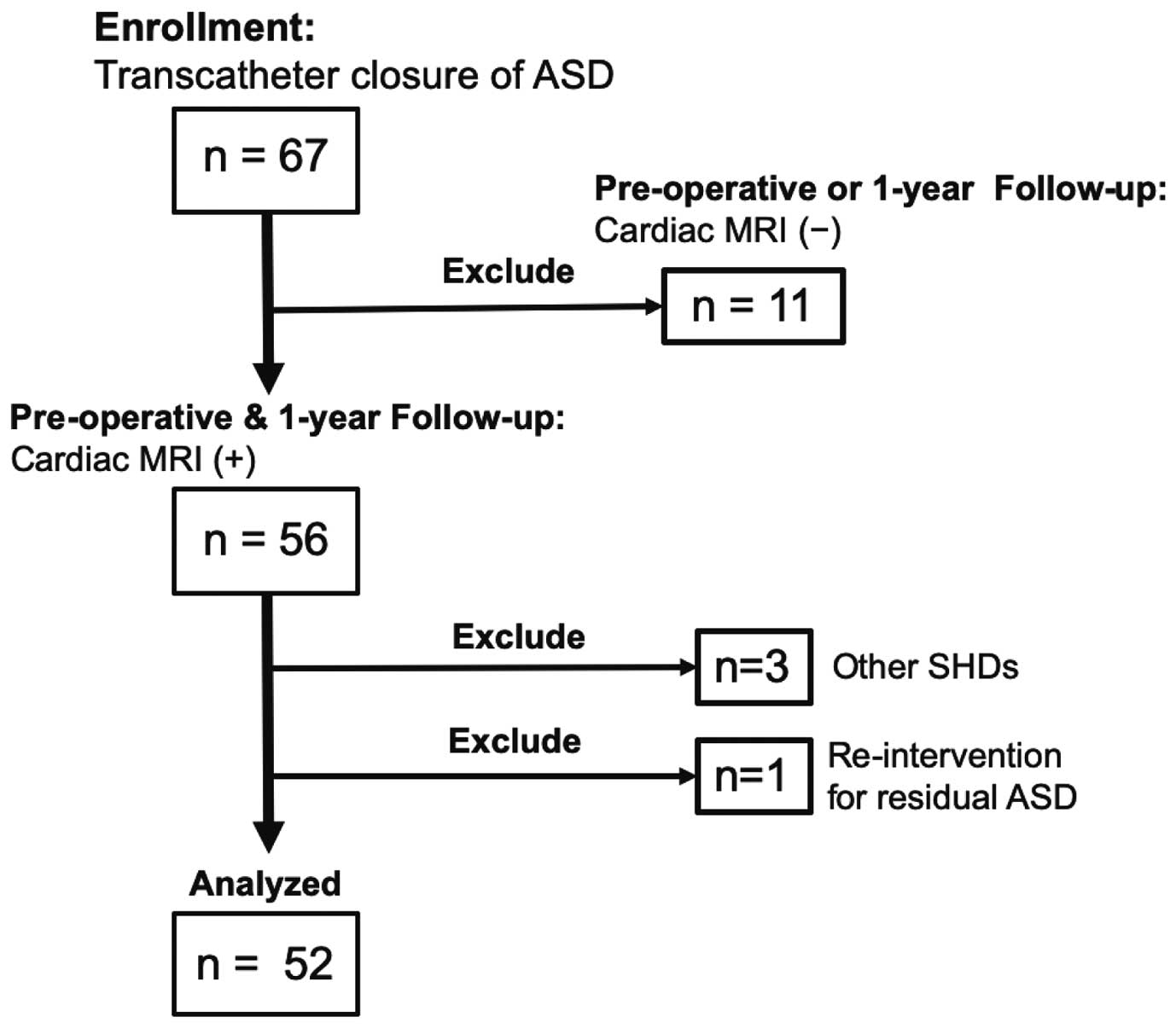
Study flow diagram. ASD, atrial septal defect; MRI, magnetic resonance imaging; SHD, structural heart disease.
We analyzed the following demographic data: New York Heart Association (NYHA) functional class, 12-lead ECG, transthoracic echocardiography (TTE), laboratory data, and maximum ASD diameter measured using transesophageal echocardiography (TEE), preoperative hemodynamic parameters using cardiac catheterization, data of transcatheter closure of ASD, and CMR data. We also obtained the data of thromboembolic events and hospitalization for heart failure and the information regarding comorbidities, such as atrial fibrillation and chronic obstructive pulmonary disease, that could be associated with RV dysfunction.15 Information about perioperative medications, such as diuretics and pulmonary vasodilators, were collected from the medical records of Kyushu University Hospital. Informed consent was given by each patient and the study complied with the Declaration of Helsinki. The Ethical Committee at Kyushu University Hospital approved this study (approval no.: 2019-83).
Hemodynamic Evaluation and Transcatheter Closure of ASDRight heart catheterization was performed under local anesthesia before transcatheter closure of ASD. The mean pulmonary artery pressure (mPAP), pulmonary vascular resistance (PVR), mean pulmonary capillary wedge pressure (mPCWP), and Qp/Qs were analyzed. PVR was calculated as (mPAP−mPCWP)/Qp.16 With oxygen uptake measured at rest, Qp/Qs was calculated with oximetry using the Fick principle.
Transcatheter closure of ASD was performed under general anesthesia with continuous TEE monitoring. We used the Amplatzer septal occluder (ASO; St. Jude Medical, St. Paul, MN, USA) or the Occlutech Figulla septal occluder (OFSO; Occlutech GmbH, Jena, Germany) for ASD closure.3,17,18 Before deploying the closure device, the operator closed the ASD with a sizing balloon catheter to measure the ASD size, then determined the size and type of the device, while considering the measurement result of the maximum ASD diameter on TEE. The ASO was used in 42 patients and the OFSO in 10 patients. Transcatheter closure of ASD was successful in all 52 patients. All the patients were discharged after confirmation of no complications by TTE and chest radiography on postoperative day 1.
CMRTo evaluate the RV and LV volumes and function, CMR was performed before transcatheter closure of ASD and at 1 year after the treatment. The median follow-up period from the time of transcatheter closure of ASD to follow-up CMR was 367 days (interquartile range [IQR]: 359–374 days).
All the patients underwent scanning with a 3-Tesla MRI (Achieva3.0T TX or Ingenia3.0T Quasar Dual; Philips Healthcare, Best, Netherlands) that was equipped with dual-source parallel radiofrequency transmission, 32-channel phased-array torso coils used for radiofrequency reception, and a 4-lead vector cardiogram used for cardiac gating.
Cine MR images were analyzed semi-automatically, followed by manual correction using a workstation (IntelliSpace Portal, Philips Healthcare). The RV volume was measured on axial images, as reported previously.19 LV volumes were measured from the short-axis images. Papillary muscles, moderator bands, and trabeculations were assigned to the intracavitary lumen of the ventricles. All the volumes were indexed to body surface area. End-diastolic and end-systolic phases were identified visually on the images that showed the largest and smallest LV and RV cavity areas, respectively. RVEF was calculated using the RVEDV and RVESV data. Based on a previous report, we defined RVEDVI ≤108 mL/m2 and RVESVI ≤47 mL/m2 as indicative of RV volume normalization.20 The median follow-up period from the time of transcatheter closure of ASD to the follow-up CMR was 367 days (IQR: 359–374 days).
Statistical AnalysisData are expressed as frequency, frequency (%), or median (IQR) values, as appropriate. Comparisons between paired groups were performed using the Wilcoxon signed-rank test. Chi-square tests were utilized for comparing the categorical variables, and the Mann-Whitney test was utilized to compare NYHA functional class.
Independent predictors for the normalization of RV volume after transcatheter closure of ASD were analyzed using multivariate logistic regression analysis. RVEDVI and RVEF were excluded because of their high correlation with RVESVI (r=0.91 and r=−0.65, respectively).
We selected age, Qp/Qs, and preoperative RVESVI as predictors for normalization of RV volume in the multivariate logistic regression analysis. Thresholds of preoperative RV volumes and RVEF for normalization of RV volume were identified using receiver-operating characteristic (ROC) curve analysis. A probability value <0.05 was considered statistically significant. Statistical analyses were performed with JMP Pro ver.13 (SAS Institute Inc., Cary, NC, USA).
Table 1 shows the preoperative characteristics of the 52 patients: median age was 47 years (IQR 33–63 years), and 40 (77%) female patients were included; 23 (44%) patients were classified as NYHA functional class I, and 28 (54%) patients as class II. The median Qp/Qs ratio was 2.4. Both the mean PAP and the PVR were within their normal ranges. During the 1-year follow-up, no patients were hospitalized because of heart failure or thromboembolic complications.
| Age at ASD closure (years) | 47 (33–63) |
| Sex (M/F), n/n | 12/40 |
| Baseline BNP (pg/mL) | 24.9 (13.8–51.3) |
| ASD diameter measured by TEE (mm) | 18.6 (15.2–22.3) |
| NYHA functional class, n (%) | |
| I | 23 (44) |
| II | 28 (54) |
| III | 1 (2) |
| IV | 0 (0) |
| Comorbidities | |
| Hypertension, n (%) | 8 (15) |
| Diabetes mellitus, n (%) | 1 (2) |
| History of hospitalization for HF, n (%) | 3 (6) |
| History of thromboembolic event, n (%) | 4 (8) |
| Chronic pulmonary obstructive disease, n (%) | 2 (4) |
| Chronic AF, n (%) | 3 (6) |
| Medications, n (%) | |
| Diuretics | 9 (17) |
| Prostanoids | 2 (4) |
| PDE-5 inhibitors | 2 (4) |
| Endothelin receptor antagonists | 1 (2) |
| Hemodynamic data | |
| Mean pulmonary artery pressure (mmHg) | 16 (14–19) |
| Pulmonary vascular resistance (w.u.) | 0.98 (0.79–1.5) |
| Systolic right ventricular pressure (mmHg) | 34.5 (29–39) |
| Qp/Qs | 2.4 (1.7–3.1) |
Data are n; n (%); or median (interquartile range). AF, atrial fibrillation; ASD, atrial septal defect; BNP, B-type natriuretic peptide; HF, heart failure; NYHA, New York Heart Association; PDE-5, phosphodiesterase type 5; TEE, transesophageal echocardiography.
No major complications, such as cardiovascular or cerebrovascular events, or deaths occurred. With respect to patient comorbidities, 2 patients had paroxysmal atrial fibrillation after transcatheter closure of ASD. However, no patient was rehospitalized because of heart failure. NYHA functional class significantly improved 1 year after transcatheter closure of ASD as follows: NYHA functional class I, 23 patients (44%) to 36 patients (69%); class II, 28 patients (54%) to 16 patients (31%); and class III, 1 patient (2%) to 0 patients (0%).
Cardiac MRI DataFigure 2 shows the preoperative and 1-year follow-up CMR data. RVEDVI decreased from 165 mL/m2 (143–201 mL/m2) to 109 mL/m2 (90–122 mL/m2) (P<0.0001), RVESVI decreased from 77 mL/m2 (69–99 mL/m2) to 56 mL/m2 (48–66 mL/m2) (P<0.0001), and RVEF decreased from 52% (48–56%) to 47% (43–50%) (P<0.0001). LVEDVI increased from 67 mL/m2 (59–77 mL/m2) to 82 mL/m2 (60–93 mL/m2) (P<0.0001), LVESVI increased from 32 mL/m2 (23–37 mL/m2) to 34 mL/m2 (28–42 mL/m2) (P=0.03), and LVEF increased from 55% (52–61%) to 58% (51–64%) (P=0.34). Although LVEDVI and LVESVI increased significantly, LVEF did not change significantly. RVESVI decreased from 83 mL/m2 (71–98 mL/m2) to 47 mL/m2 (41–54 mL/m2) (P<0.0001); however, the LV stroke volume index increased significantly from 35 mL/m2 (29–41 mL/m2) to 45 mL/m2 (39–48 mL/m2) at the end of the 1-year follow-up (P<0.0001).

Changes in the right and left ventricular cardiac MRI data at the preoperative stage and at 1-year follow-up (n=52). *P<0.0001 (Wilcoxon’s signed-rank test). EDVI, end-diastolic volume index; EF, ejection fraction; ESVI, end-systolic volume index; LV, left ventricular; RV, right ventricular; SVI, stroke volume index.
Preoperative data were divided into normalized and non-normalized RV groups after transcatheter closure of ASD (Table 2). The RVEDVI normalized in 23 (44%) patients, and RVESVI normalized in 10 (19%) patients. There were no significant differences in age and sex between groups. There were no significant differences in mean PAP, PVR, and Qp/Qs ratio between groups. Preoperative RVEDVI was not significantly different between groups; however, the preoperative RVESVI was significantly smaller, and the preoperative RVEF was significantly higher in the normalized group.
| Normalized group (n=10) |
Non-normalized group (n=42) |
P value | |
|---|---|---|---|
| Age at ASD closure (years) | 45 (18–58) | 50 (34–64) | 0.28 |
| Sex (M/F), n/n | 1/9 | 11/31 | 0.24 |
| Serum BNP (pg/mL) | 25.7 (13.5–42.4) | 24.9 (13.5–56.4) | 0.62 |
| NYHA class (I/II/III/IV) | 7/3/0/0 | 16/25/1/0 | 0.23 |
| History of hospitalization for HF, n | 0 | 3 | 0.25 |
| Chronic AF, n | 0 | 3 | 0.25 |
| ASD size on TEE (mm) | 18.2 (16.1–22.5) | 18.6 (15.0–22.2) | 0.87 |
| Closure device size (mm) | 20 (18–23) | 22 (17–26) | 0.29 |
| Hemodynamic data | |||
| Mean PAP (mmHg) | 15.0 (14.0–18.0) | 16.5 (13.3–20.5) | 0.58 |
| PVR (w.u.) | 1.1 (0.75–1.5) | 1.0 (0.80–1.4) | 0.69 |
| Qp/Qs | 2.2 (1.5–3.2) | 2.4 (1.9–3.1) | 0.54 |
| CMR data | |||
| Preoperative RVEDVI (mL/m2) | 146 (131–177) | 169 (149–211) | 0.08 |
| Preoperative RVESVI (mL/m2) | 71 (58–73) | 80 (70–104) | 0.02 |
| Preoperative RVEF (%) | 56 (52–59) | 51 (47–55) | 0.02 |
Data are median (interquartile range) or n. CMR, cardiac magnetic resonance imaging; PAP, pulmonary artery pressure; PVR, pulmonary vascular resistance; Qp/Qs, pulmonary-to-systemic flow ratio; RVEDVI, right ventricular end-diastolic volume index; RVEF, right ventricular ejection fraction; RVESVI, right ventricular end-systolic volume index. Other abbreviations as in Table 1.
In order to identify the predictors for the normalization of RV volume after transcatheter closure of ASD, we performed multivariate logistic analysis (Table 3). The correlation coefficients between age and RVESVI, and between Qp/Qs and RVESVI were r=0.02 (P=0.91) and r=0.37 (P=0.009), respectively. Thus, preoperative RVESVI was an independent predictor for the normalization of RV volume (odds ratio (OR): 0.940, 95% confidence interval (CI): 0.886–0.999, P=0.007).
| Variables | Univariate analysis | Multivariate analysis | |
|---|---|---|---|
| P value | OR (95% CI) | P value | |
| Age at ASD closure | 0.209 | 0.970 (0.930–1.01) | 0.133 |
| Male | 0.241 | ||
| ASD size on TEE | 0.796 | ||
| History of hospitalization for HF | 0.250 | ||
| Baseline BNP | 0.236 | ||
| Mean PAP | 0.211 | ||
| PVR | 0.755 | ||
| Qp/Qs | 0.444 | 1.44 (0.578–3.59) | 0.442 |
| Preoperative RVEDVI | 0.076 | ||
| Preoperative RVESVI | 0.018 | 0.940 (0.886–0.999) | 0.007 |
| Preoperative RVEF | 0.021 | ||
OR, odds ratio. Other abbreviations as in Tables 1,2.
ROC analysis was performed to identify the threshold of preoperative RVEDVI, RVESVI, and RVEF for normalization of RV volume after transcatheter closure of ASD (Figure 3). The respective threshold values were 183 mL/m2 (area under the curve [AUC] 0.68, 95% CI: 0.51–0.82, sensitivity 100%, specificity 40%), 75 mL/m2 (AUC 0.75, 95% CI: 0.59–0.86, sensitivity 90%, specificity was 69%) and 56% (AUC 0.74, 95% CI: 0.53–0.88, sensitivity 60%, specificity 85%).
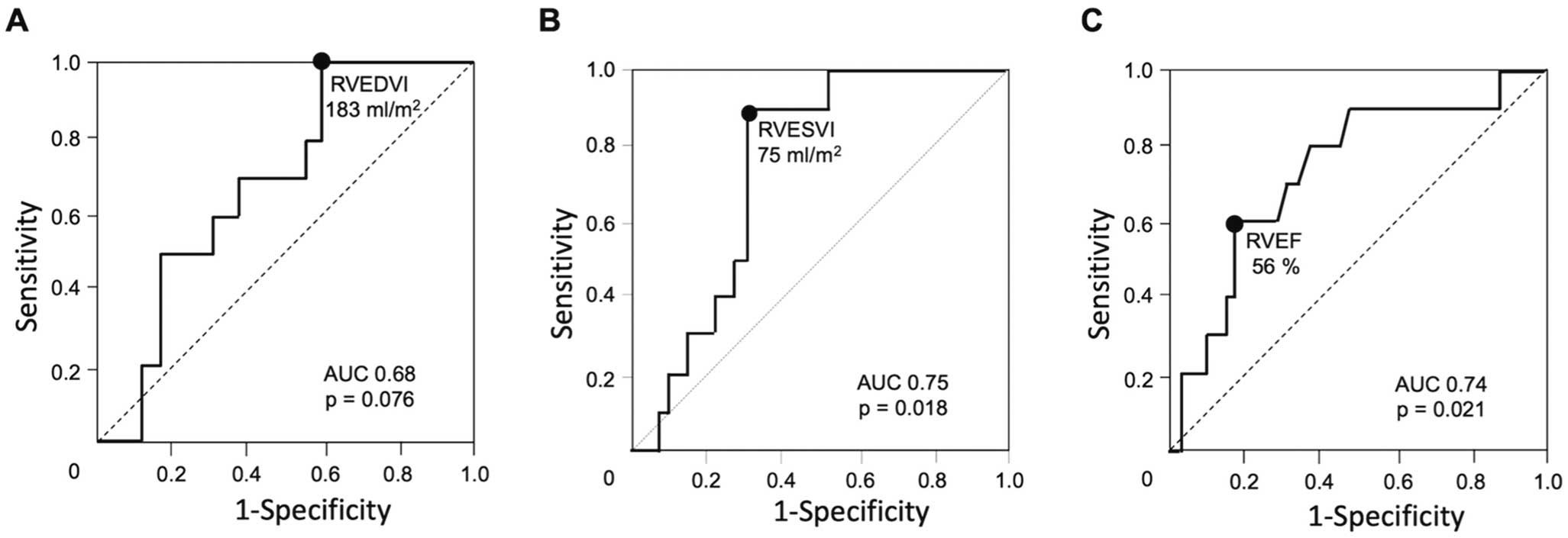
Receiver-operating characteristic curves to determine the thresholds for normalization of RV volume. Preoperative (A) RVEDVI, (B) RVESVI and (C) RVEF. AUC, area under the curve; RVEDVI, right ventricular end-diastolic volume index; RVEF, right ventricular ejection fraction; RVESVI, right ventricular end-systolic volume index.
The present study used CMR to show the preoperative threshold for normalization of RV volume 1 year after transcatheter closure in adult patients with ASD. Based on ROC analysis, a threshold preoperative RVESVI value of 75 mL/m2 assisted in predicting the normalization of RV volume after transcatheter closure of ASD. Multivariate regression analysis showed that preoperative RVESVI was an independent predictor for normalization of the RV volume after transcatheter closure of ASD. These data suggest that early transcatheter closure of ASD before RVESVI reaches 75 mL/m2 may confer the optimal timing.
Several retrospective studies using TTE have analyzed the relationship between postoperative RV size and symptoms after transcatheter closure of ASD.10,21,22 Veldtman et al7 investigated the changes in RV size and symptoms 1 year after transcatheter closure of ASD. Although there was significant improvement in terms of the average RV size and symptoms, 29% of the patients showed persistent RV enlargement and 10% patients exhibited symptoms associated with RV enlargement at the 1-year follow-up. Another study9 evaluated the RV dimensions using echocardiography and mean V˙O2 max in 37 adult ASD patients with mild or no symptoms (NYHA functional class: I or II, mean Qp/Qs: 2.1). Similar to the aforementioned study, transcatheter closure of ASD significantly reduced the RV size and increased the mean V˙O2 max at the 6-month follow-up. However, mild RV enlargement was found in 17 patients, and severe enlargement of the RV was observed in 1 patient. These data suggest that although transcatheter closure of ASD can improve exercise tolerance by reducing the size of the RV, some patients still experience RV enlargement and symptoms. In addition, accurate echocardiographic evaluation of the RV is often limited by the complex RV geometry.23 Therefore, cardiac CMR should be used to obtain reliable RV volumes without such limitations.13,14
In the present study, 42 patients (81%) showed residual RV enlargement at the 1-year follow-up. A comparison of the postoperative RV volumes between groups with postoperative NYHA functional classes I and II/III showed that the RV volume tended to be smaller in the postoperative NYHA I group (RVEDVI: 107.6 vs. 110.5 mL/m2, P=0.36; RVESVI: 55.5 vs. 60.6 mL/m2, P=0.31). In addition, the proportion of postoperative NYHA functional class I was higher in the normalized group than in the non-normalized group (9 in 10 90% vs. 27 in 42 64%). These data suggest that normalization of postoperative RV volumes may contribute to improvement in NYHA functional class.
Aging and the Qp/Qs ratio are reported as influential factors for postoperative RV size after transcatheter closure of ASD.7,21 Veldtman et al reported that a higher proportion of elderly patients (aged >40 years) had residual RV enlargement.7 Consistent with that report, we also found a higher proportion of elderly patients (>40 years) in the non-normalized group than in the normalized group (74% vs. 60%). However, there were no significant correlations between age and postoperative RV volumes (RVEDVI: −0.19 (P=0.18); RVESVI: −0.17 (P=0.21), respectively) (Figure 4). We also divided all patients into 3 age groups (<50, 50–69, and >70 years) and compared RV parameters (Supplementary Table 1). There were no significant differences in RVEDVI, RVESVI and RVEF before or after ASD closure among those groups. Recently, the efficacy and safety of transcatheter closure of ASD in older patients have been reported.24,25 Therefore, further investigation is needed to determine the factors influencing normalization of RV volume after transcatheter closure in such patients. Regarding the Qp/Qs, Giardini et al reported that patients with higher Qp/Qs showed significant reduction in the blood volume in the RV after transcatheter closure of ASD, resulting in marked RV reverse remodeling, followed by an increase in the LV cardiac output.21 In the present study, the preoperative Qp/Qs ratio significantly correlated with reduced volumes of RVEDVI and RVESVI (r=0.44 and r=0.36, respectively, P<0.05) (Figure 5). Thus, we entered aging and Qp/Qs into our multivariate regression analysis model in addition to preoperative RVESVI as a predictor for normalization of the RV volume after transcatheter closure of ASD. Among these factors, only preoperative RVESVI was identified as an independent predictor for the normalization of RV volume (Table 3).

Correlation between age and postoperative right ventricular (RV) volume. Postoperative RVEDVI and RVESVI did not show a significant correlation with patient age. RVEDVI, right ventricular end-diastolic volume index; RVESVI, right ventricular end-systolic volume index.

Correlation between the changes in the reduced volumes of RV and Qp/Qs. ∆Pre–Post RVEDVI=Pre RVEDVI−Post RVEDVI; ∆Pre−Post RVESVI=Pre RVESVI−Post RVESVI, RVEDVI, right ventricular end-diastolic volume index; RVESVI, right ventricular end-systolic volume index.
The specificity of preoperative RVESVI to predict RV normalization after transcatheter closure of ASD was relatively low (69%). In other words, some of patients with preoperative RVESVI <75 mL/m2 showed non-normalization of RV volumes at 1 year after ASD closure. As shown in Supplementary Table 2, 13 (64%) of 22 patients with preoperative RVESVI <75 mL/m2 did not show normalized RV volumes at 1-year follow-up. However, there were no statistical differences in various parameters between the normalized and non-normalized RV groups in 22 patients. We did not speculate on any other factors to explain non-normalization after ASD closure.
As another factor that influences RV remodeling, pulmonary hypertension with RV dysfunction should be considered. However, our patients showed normal mPAP and PVR (16 (IQR: 14–19) mmHg and 0.98 (0.79–1.5) w.u., respectively). We therefore excluded mPAP as a possible influence on normalization of the RV volume after transcatheter closure by univariate regression analysis.
It remains unclear as to why the preoperative RVESVI but not RVEDVI or RVEF was identified as a sensitive predictor for RV volume normalization following transcatheter closure of ASD. Several studies have investigated the effect of pulmonary valve replacement on the RV parameters in repaired tetralogy of Fallot (TOF) with severe pulmonary regurgitation (PR),26–32 which causes volume overload of the RV and dilatation similar to that in ASD. Bokma et al used CMR to investigate the predictor for RV volume normalization in the long term (>3 years) after PVR. Similar to our results, preoperative RVESVI, compared with RVESVI and RVEF, was the more sensitive predictor for RV reversibility in TOF patients with PVR.30 Another study by Uebing et al that used conductance catheter showed that in comparison with RVEDVI and RVEF, RVESVI had a significant correlation with Ees as a parameter of intrinsic RV contractility (r=−0.64, P<0.001).33 Taken together, preoperative RV contractility reflected by RVESVI might greatly contribute to postoperative reversibility in RV volume-overload diseases such as ASD and TOF.
Study LimitationsThe present study includes several limitations. First, the follow-up period of CMR was 1 year after transcatheter closure of ASD. Schoen et al retrospectively reported that RVESVI and RVEDVI measured using CMR significantly decreased in 6 months after transcatheter closure of ASD and that there were no significant changes in both parameters between 6 and 12 months.34 Therefore, we believe that a 1-year follow-up period was sufficient to detect RV normalization after ASD closure. However, the long-term clinical outcomes in the normalized and non-normalized RV volume groups remain unclear in the present study. In addition, the number of patients in the normalized RV size group was small (n=10), and this study was a single-center retrospective analysis. In order to evaluate the long-term effects of RV volume reversal on clinical outcomes, such as prognosis and hospitalization for heart failure, a long-term, large-scale multicenter registry is needed. Second, diuretics and pulmonary vasodilators might affect the RV volume after transcatheter closure of ASD. However, only 4 patients changed the dose of their diuretics between transcatheter closure of ASD and the 1-year follow-up, and 2 patients were prescribed pulmonary vasodilators. In fact, there were no significant differences in the RV volumes as per the dose changes in the diuretics and initiation of pulmonary vasodilators (data not shown). Thus, we considered that these drugs had limited effect on the RV volume after ASD closure. Third, this study indicated no major complications, such as cardiovascular or cerebrovascular events, and no deaths occurred. However, 2 patients were complicated with paroxysmal atrial fibrillation during the follow-up period. These patients showed preoperative enlarged RVESVI (134.9 and 89.0 mL/m2, respectively), and ASD closure failed to normalize RV volume (65.6 and 47.1 mL/m2, respectively). It is considered that further follow-up of clinical outcomes is needed in those patients. Fourth, we did not determine the influence of reduction of tricuspid valve regurgitation (TR) on changes in RV volume after transcatheter closure of ASD because of no scan the phase-contrast sequence on tricuspid valvular flow in our study protocol. Instead, we additionally analyzed the TR evaluated by echocardiography and 13 of 52 (25%) patients showed moderate to severe TR before ASD closure. After ASD closure, moderate to severe TR was found in only 3 patients (P=0.04). However, by univariate regression analysis, the improvement in TR grade was not statistically significant to predict RV normalization (OR 2.3, 95% CI: 0.53–10.3, P=0.26). We therefore consider that TR improvement did not greatly contribute to RV normalization in the present study. However, for detailed analysis of changes in TR flow, using the phase-contrast method by CMR is needed in any further studies. Finally, we did not assess the exercise tolerance data obtained using cardiopulmonary exercise tests in this study. Giardini et al reported that transcatheter closure of ASD improved V˙O2 max even in asymptomatic patients (84%: NYHA-FC class I).10 Thus, further research is necessary to investigate the relationship between RV volumes and V˙O2 max before and after transcatheter closure of ASD.
Preoperative RVESVI was identified as an independent predictor for normalization of RV volume at 1 year after transcatheter closure of ASD in adults. Early intervention before the RVESVI reaches 75 mL/m2 may confer optimal timing for normalizing the size of the RV.
The authors declare no conflicts of interest. T.I. and H.T. are members of Circulation Journal ’ Editorial Team.
This work was in part supported by Grants-in-Aid for Scientific Research from the Japan Society for the Promotion Science (17K09509).
The Ethics Committee of the Faculty of Medicine at Kyushu University, Reference no.: 2019-8.
1. Will the individual deidentified participant data (including data dictionaries) be shared? Yes.
2. What data in particular will be shared? All de-identified participant data collected during the study.
3. Will any additional, related documents be available? If so, what is it? None.
4. When will the data become available and for how long? After this article is accepted, and for 1 year.
5. By what access criteria will the data be shared (including with whom)? E-mail to the corresponding authors. The data will be shared with anyone on a request basis.
6. For what types of analyses, and by what mechanism will the data be available? For any purpose, the data will be shared as Excel files via E-mail.
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-20-0136