2021 Volume 85 Issue 11 Pages 2050-2052
2021 Volume 85 Issue 11 Pages 2050-2052
Favorable prognoses have been reported for patients in whom myocardial ischemia was not identified from stress myocardial perfusion imaging (MPI).1 Therefore, coronary revascularization is indicated for coronary stenosis based on the assessment of myocardial ischemia. Furthermore, MPI enables semiquantitative evaluation of the size of the ischemic territory. Revascularization for an ischemic territory size >10% may improve prognosis compared with medical therapy alone.2 However, according to the ISCHEMIA trial,3 the event risk in stable coronary artery disease corresponding to initial medical therapy was equivalent to that with an initial invasive strategy even in patients with either moderate or severe ischemic territory size such that not only the size of the ischemic territory, but also the ischemic depth, namely the plaque vulnerability, might be crucial in the assessment of event risk.
Article p 2043
Currently, fractional flow reserve (FFR) is being widely used for the invasive evaluation of myocardial ischemia in clinical settings.4,5 According to the FAME 2 study, patients in whom FFR revealed myocardial ischemia benefitted from percutaneous coronary intervention (PCI) rather than medical therapy alone.6 However, these events mainly consisted of coronary revascularization, and the difference in the events of death or myocardial infarction (MI) was nonsignificant. Considering the long-term follow-up (3–5 years) of the ISCHEMIA trial and the FAME 2 study, a trend of widening the difference for MI occurrence was observed. Therefore, long-term observation of an event is necessary for a conclusion, and we must focus on the detection of unstable or high-risk situations. Clinically, prediction and prevention of an event are most important.
In the IRIS-FFR registry,7 the FFR cutoff for major adverse cardiovascular events (MACE) was 0.79. In lesions with FFR ≤0.75, the risk of MACE was significantly lower in revascularized lesions than in deferred lesions. As the FFR cutoff for death or MI was 0.64 and in the border zone FFR was 0.64–0.80, differences in death or MI were nonsignificant between revascularization and medical therapy.
The focal pressure gradient value in addition to the whole-vessel FFR value might be important. The Emerald study,8 which used FFR-CT to predict events, demonstrated that the focal pressure gradient value across a lesion was an important predictor of acute coronary syndrome (ACS) events. Both FFR pullback recording9 and FFR-CT can reveal the distribution of the pressure gradient in a vessel. If a large pressure gradient exists at the proximal coronary artery, the size of the ischemic territory increases (Figure 1, Left). In the case of a large focal pressure gradient, the stress against the plaque becomes greater, which may be related to the ACS events. However, there are many cases of diffuse pressure gradient in the entire coronary artery (Figure 1, Right). Whether coronary revascularization with placement of a coronary stent can remove the diffuse pressure gradient is a recent concern. A pressure gradient is noted even after satisfactory coronary stent implantation in some cases, and such diffuse pressure gradient patterns may be related to poor prognoses.10,11 Information on the distribution of the pressure gradient is useful and crucial.
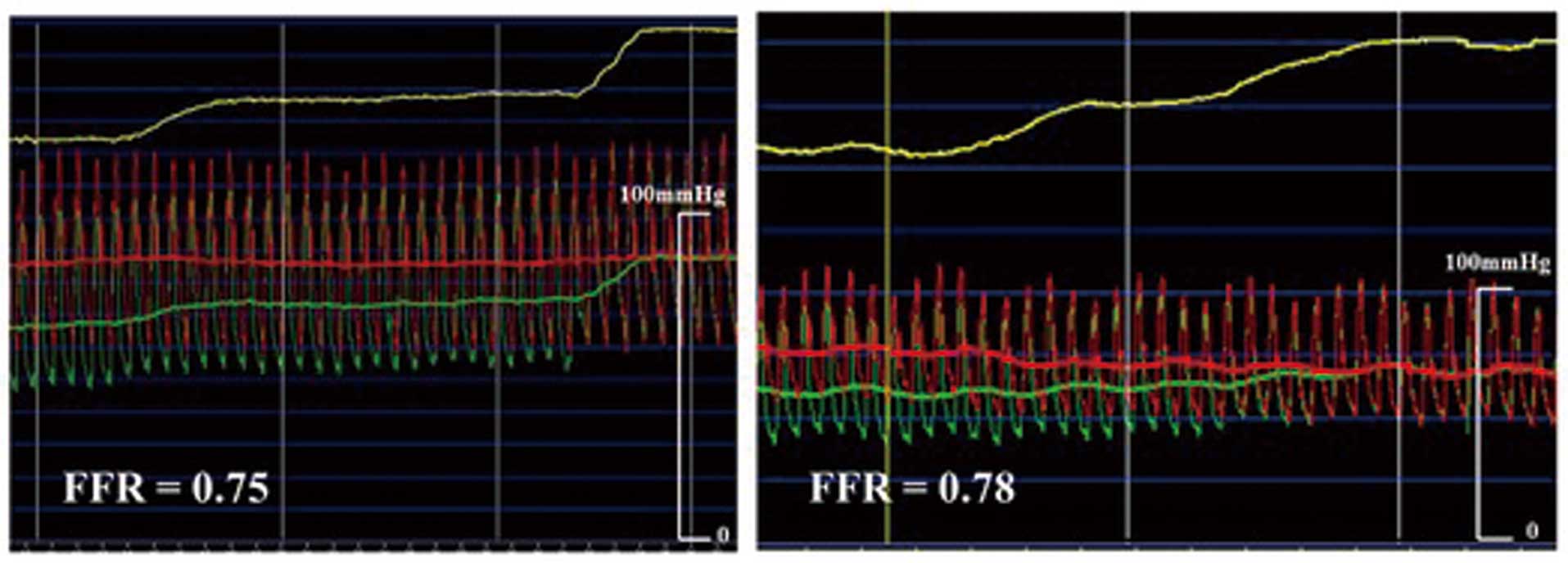
FFR pullback recording performed under maximal hyperemic conditions. (Left) Tandem lesion with focal gradient, which is showing that the proximal gradient is larger than the distal gradient. (Right) Diffuse pressure gradient pattern with border zone FFR value, which is showing that a coronary stent is unsuitable in this case. FFR, fractional flow reserve.
From these points of view, FFR should be considered not only as a binary discriminator of myocardial ischemia, but also as a surrogate marker for atherosclerotic change, which can be a predictive marker of an event (Figure 2).
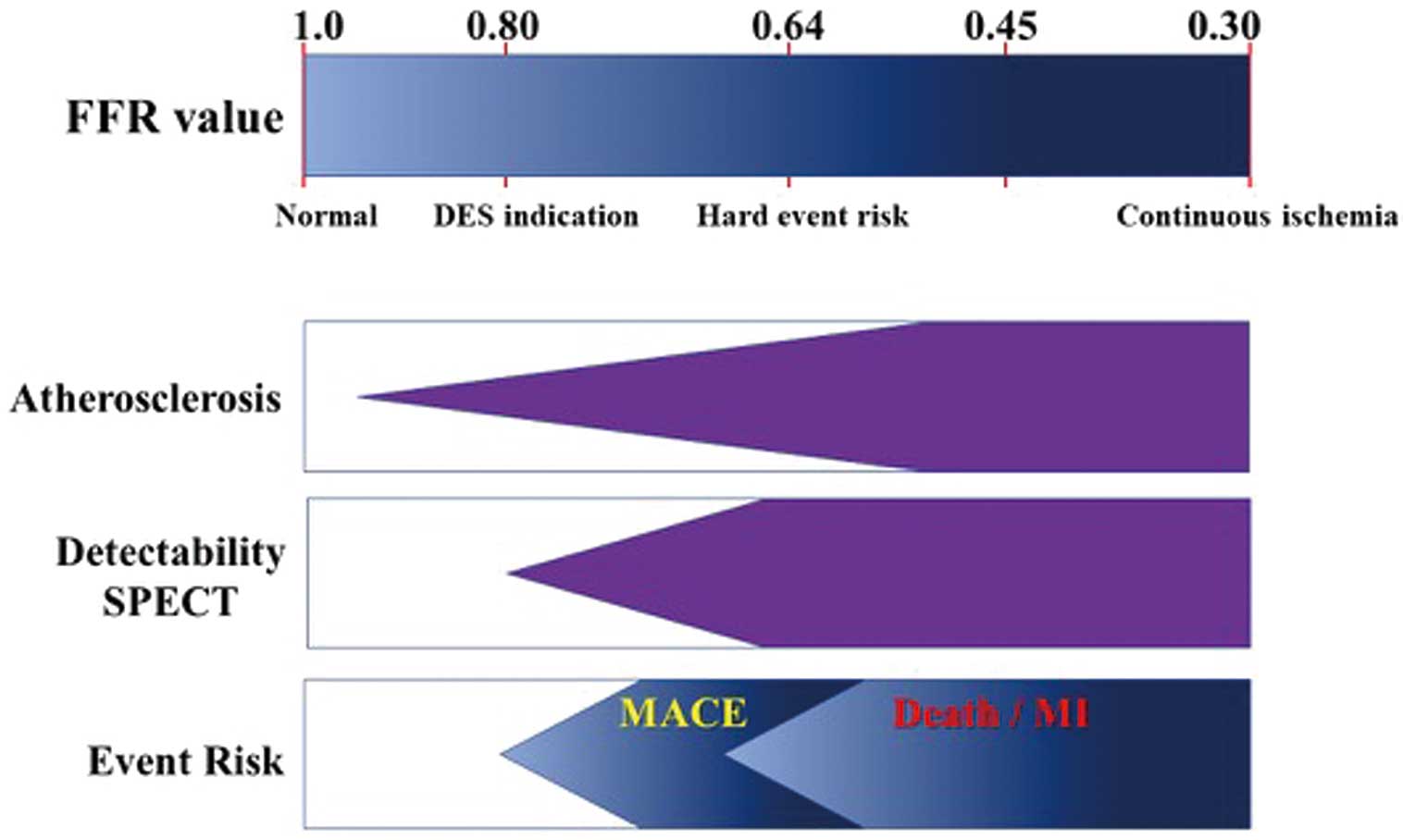
FFR value and its significance. The normal value of FFR is 1.0. As coronary atherosclerotic changes progress, the FFR value decreases. FFR value for the ischemic threshold in stress MPI is 0.80, and the FFR cutoff for hard event risk is 0.64. DES, drug-eluting stent; FFR, fractional flow reserve; MACE, major adverse cardiac event; MI, myocardial infarction; SPECT, single-photon emission computed tomography.
MPI and FFR have been compared,12 and although a positive correlation between MPI and FFR has been demonstrated, conflicting results have been occasionally observed and present the challenge of the appropriate choice of a therapeutic strategy. In this issue of the Journal, Kawamura et al13 demonstrate that (1) most cases of discordance between FFR and MPI have mildly positive FFRs ranging from 0.65 to 0.80 with normal MPI and (2) there are few other discordant cases with severely positive FFRs <0.65 with normal MPI. They conclude that an abnormal MPI may effectively identify high-risk groups.
In diffuse lesions with gray-zone FFR values at the distal part, a diffuse pressure gradient is present throughout the vessel. As a result of such a gradual pressure gradient pattern, only the left ventricular apex can be detected as ischemic with MPI. Such a pattern is unsuitable for treatment with a coronary stent.
Before the ISCHEMIA trial era, we chose a treatment strategy based on the MPI or FFR results, which were regarded as indicative of myocardial ischemia. However, after the ISCHEMIA trial era, we now consider MPI and FFR as predictors for events, wherein the ischemic territory size, ischemic depth, and focal stress on plaques must be considered. MPI is useful in the assessment of myocardial ischemia and the ischemic territory size, whereas FFR is useful in the assessment of myocardial ischemia and ischemic depth. Discordance of the results from the 2 modalities may provide some information regarding event risk. In a case with border zone ischemia, treatment strategies and the purpose of treatment must be carefully considered.
N.T. has received lecture fees from Abbott Vascular and Daiichi-Sankyo.