Abstract
Background:
The hypothesis of this study is that latent class analysis could identify the subphenotypes of out-of-hospital cardiac arrest (OHCA) patients associated with the outcomes and allow us to explore heterogeneity in the effects of extracorporeal cardiopulmonary resuscitation (ECPR).
Methods and Results:
This study was a retrospective analysis of a multicenter prospective observational study (CRITICAL study) of OHCA patients. It included adult OHCA patients with initial shockable rhythm. Patients from 2012 to 2016 (development dataset) were included in the latent class analysis, and those from 2017 (validation dataset) were included for evaluation. The association between subphenotypes and outcomes was investigated. Further, the heterogeneity of the association between ECPR implementation and outcomes was explored. In the study results, a total of 920 patients were included for latent class analysis. Three subphenotypes (Groups 1, 2, and 3) were identified, mainly characterized by the distribution of partial pressure of O2
(PO2), partial pressure of CO2
(PCO2) value of blood gas assessment, cardiac rhythm on hospital arrival, and estimated glomerular filtration rate. The 30-day survival outcomes were varied across the groups: 15.7% in Group 1; 30.7% in Group 2; and 85.9% in Group 3. Further, the association between ECPR and 30-day survival outcomes by subphenotype groups in the development dataset was as varied. These results were validated using the validation dataset.
Conclusions:
The latent class analysis identified 3 subphenotypes with different survival outcomes and potential heterogeneity in the effects of ECPR.
Out-of-hospital cardiac arrest (OHCA) with shockable rhythm, such as ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT), is the focus of resuscitation strategies because these arrhythmias are treatable by defibrillation, and the implementation of extracorporeal cardiopulmonary resuscitation (ECPR) is expected to better patient outcomes.1–3
However, these patients are heterogeneous, and several factors such as low-flow time duration, cardiac rhythm conversion or some biomarkers were reported to be associated with the different outcomes.4–6
Among OHCA patients with high clinical heterogeneity, these single factors were not suitable for differentiating and determining which OHCA patients are suitable for this invasive treatment or are expected to have favorable neurological outcomes.
Editorial p 677
The concept of “subphenotypes”, identified by unsupervised machine learning, is a current research focus in medicine.7–9
A phenotype is a category of patients with common features such as a syndrome (e.g., sepsis or acute respiratory distress syndrome), and a subphenotype is a subgroup of the phenotype with different risk factors, clinical features, and responses to treatment compared with other subphenotypes.10,11
Latent class analysis, which is an explanatory modeling technique, has been used to differentiate subphenotypes using continuous and categorical variables.12
Our hypothesis is that this data-based clustering approach could identify the clinical subphenotypes of the OHCA patients associated with different outcomes. It could allow us to explore heterogeneity in the effect of ECPR, which would potentially lead to the clinical use of precision treatments that reduce morbidity and mortality.13
However, no clinical studies have investigated the clinical patterns associated with different outcomes using the unsupervised clustering technique for OHCA patients with initial shockable rhythm.
This study aimed to identify the subphenotypes among the OHCA patients with initial shockable rhythm by applying a machine learning-based unsupervised clustering technique, and investigated the association between the subphenotypes and clinical outcomes. Further, this study aimed to explore the heterogeneity of the effect of ECPR on patient clinical outcomes.
Methods
Study Design, Settings, and Patients
This study was a retrospective analysis of the database of the Comprehensive Registry of Intensive Care for OHCA Survival (CRITICAL) study. This database was created to collect pre-hospital and in-hospital data of OHCA patients in Osaka Prefecture, Japan, for a multicenter prospective observational study. The details of this registry have been described previously.4,14,15
Briefly, the pre-hospital data were obtained from the All-Japan Utstein Registry from the Fire and Disaster Management Agency (FDMA),14,16
and the in-hospital data were collected from 15 tertiary critical care medical centers and 1 community hospital with an emergency department, all in Osaka Prefecture in Japan. This study was conducted according to the Declaration of Helsinki.
This study included all adult OHCA patients (aged ≥18 years) with an internal medical cause and initial shockable rhythm between 1 July 2012 and 31 December 2017, from the CRITICAL database. Initial shockable rhythm was defined as VF or pVT confirmed by paramedics at the scene because the guideline of advanced life support proposed different resuscitation algorithms according to the rhythms.1
The following patients were excluded: those who did not receive any resuscitation or treatment in the hospital; whose pre-hospital record was unavailable; whose age was ≤17 years or unknown; whose mechanism of cardiac arrest was caused externally such as trauma; and whose spontaneous circulation was obtained by paramedics at contact.
Development Cohort and Validation Dataset
The data were split into a development dataset for clustering subphenotypes and a validation dataset for assessing the validity of the subphenotypes. The development dataset contained data from 2012 to 2016, and the validation dataset contained data from 2017.
Latent Class Analysis/Variable Section
We performed latent class analysis with variable selection for clustering subphenotypes according to the suggested key steps in the literature.13
The details of variables and methodology are described in the
Supplementary Appendix 1; the concept of latent class analysis is presented in
Figure 1.
We selected clinically important variables that are measurable or available in the emergency departments at hospital admission and were registered in the database; 22 variables were considered as candidates for analysis in this study (Supplementary Appendix 2). Covariates encompassed a range of domains including demographic information (age and sex), pre-hospital data (e.g., presence of witness, bystander CPR, bystander defibrillation, and time from the emergency call to arrival at the hospital), and in-hospital data (e.g., initial cardiac rhythm, blood gas analysis, and the laboratory data at hospital arrival).
Data Setup
Implausible data and unreasonable outliers were double-checked and treated as missing data, as in previous studies.14
Missing data were imputed by random forest imputation as a multiple imputation technique using the “missForest” package in R 3.5.1 prior to variable selection and clustering.9,17,18
The details of missing data are available in
Supplementary Table 1. Variables with a correlation coefficient >0.5 or <−0.5 were filtered; the most clinically meaningful one was selected, and others were excluded from the clustering (Supplementary Table 2).9,13
The estimated glomerular filtration rate (eGFR) value was calculated by using creatinine level, age, and sex and using the equation widely accepted in Japan.19
The adequate sample size depends on the data; for sample sizes >500, models and fit statistics have been shown to perform consistently with high accuracy from simulation-based studies.13,20
Model Fitting and Evaluation
We fitted the model using the development dataset and calculated the Bayesian information criterion (BIC) value to determine the optimal number of clusters. To identify the optimal number of subphenotypes that have potential clinical implications, we evaluated the BIC value of the model by applying “the Elbow method”.13
The discriminative power of each variable was calculated as the logarithm of the ratio between the probability that the variable is relevant for clustering and the probability that the variable is irrelevant for clustering.21
The greater the index variable, the more important the variable is for clustering. For better understanding, the discriminative power was scaled so that the sum value was 100%. To identify the optimal number of clusters and most relevant discriminatory variables, clustering using the VarSelLCM package in R 3.5.1 was conducted with 3–8 clusters.
Once subphenotypes were developed by the model, we compared the differences in demographics, pre-hospital data, and in-hospital data by using the Pearson’s Chi-squared test or Kruskal-Wallis rank sum test. Continuous variables were summarized by median and interquartile range (IQR), whereas categorical variables were summarized by frequencies and percentages.
Subphenotypes and Outcome Association
We evaluated the association between the identified subphenotypes and clinical outcomes including the 30-day survival as the primary outcome and the 30-day survival with favorable neurological outcomes as the secondary outcome, which was defined by Cerebral Performance Category 1 or 2 (Supplementary Appendix 2).22
Logistic regression analysis was performed to calculate the crude odds ratio (OR) with 95% confidence interval (CI) for the outcomes of each group. We did not perform the adjustment of other covariates by multivariable analysis, the detailed explanation for which is provided in
Supplementary Appendix 1.
Heterogeneity Between ECPR and Outcomes
We evaluated the heterogeneity of the association between ECPR and outcomes among the subphenotypes. ECPR was defined as emergency implementation of veno-arterial extracorporeal membrane oxygenation in the resuscitation phase. The implementation of ECPR was decided by the physician in charge of the patient based on the protocol of each institution. Logistic regression analysis, with 95% CI, was performed to calculate the crude OR of patients treated with ECPR compared to those without ECPR for the 30-day survival outcomes by each group. Further, the P value for the interaction was evaluated using the interaction term. Adjustment of the covariates was not performed, as mentioned above. Regarding the 30-day neurological outcomes, we did not perform this analysis because the number of outcomes was assumed to be limited.
Validation of the Derived Subphenotypes
To assess the external validity and replicability, the clustering model was applied to the validation dataset using the “predict” function of the VarSelLCM package, and the subphenotypes were identified. The characteristics of the subphenotypes, association between subphenotypes and outcomes, and heterogeneity of the association between ECPR and outcomes were assessed in the same manner, as described above.
Results
Study Participants
From the 12,594 patients in the CRITICAL database, 1,169 OHCA patients with initial shockable rhythm were included in the analysis; 920 patients were allocated to the development dataset (median [IQR] age: 65 [53–75] years, men: 749 [81.4%]), and 249 patients were allocated to the validation dataset (median [IQR] age: 66 [56–73] years, men: 744 [80.7%]). The flowchart of the study and the details of exclusion are indicated in
Supplementary Figure 1. Patient characteristics and in-hospital data are described in
Table
and
Supplementary Tables 3
and
4. The 30-day survival with favorable neurological outcome in the development and validation datasets was 265 (28.8%) and 63 (25.3%), respectively.
Table.
Characteristics of Patients in the Development Dataset
| Characteristics |
Overall
(N=920) |
Subphenotypes |
P value* |
Group 1
(N=453) |
Group 2
(N=212) |
Group 3
(N=255) |
| Sex (men) |
749 (81) |
372 (82) |
173 (82) |
204 (80) |
0.8 |
| Age (years) |
65.0 (53.0, 75.0) |
66.0 (54.0, 76.0) |
64.0 (53.0, 73.2) |
64.0 (51.5, 73.0) |
0.015 |
| Witness |
718 (78) |
344 (76) |
166 (78) |
208 (82) |
0.2 |
| Bystander CPR |
410 (45) |
196 (43) |
82 (39) |
132 (52) |
0.013 |
| Bystander shock |
36 (3.9) |
19 (4.2) |
5 (2.4) |
12 (4.7) |
0.4 |
| Cardiac rhythm at hospital arrival |
|
|
|
|
<0.001 |
| VF/VT |
287 (31) |
137 (30) |
111 (52) |
39 (15) |
|
| PEA/Asystole |
394 (43) |
290 (64) |
79 (37) |
25 (9.8) |
|
| ROSC |
239 (26) |
26 (5.7) |
22 (10) |
191 (75) |
|
| Time from call to hospital (min) |
30 (24, 39) |
31 (26, 40) |
30 (24, 36) |
29 (23, 39) |
<0.001 |
| BT (℃) |
35.5 (34.8, 36.0) |
35.6 (34.9, 36.0) |
34.9 (33.9, 35.8) |
35.7 (35.2, 36.3) |
<0.001 |
| PCO2 (mmHg) |
63 (42, 83) |
80 (66, 97) |
54 (40, 72) |
38 (32, 47) |
<0.001 |
| PO2 (mmHg) |
78 (37, 226) |
42 (21, 64) |
240 (104, 400) |
211 (106, 333) |
<0.001 |
| BE (mEq/L) |
−14.5 (−19.4, −9.9) |
−15.6 (−19.6, −12.2) |
−18.2 (−23.8, −14.8) |
−9.4 (−12.5, −6.2) |
<0.001 |
| Glu (mg/dL) |
277 (219, 345) |
287 (227, 353) |
314 (235, 387) |
241 (199, 287) |
<0.001 |
| Alb (g/dL) |
3.3 (3.0, 3.7) |
3.3 (3.1, 3.6) |
2.9 (2.5, 3.2) |
3.7 (3.5, 4.0) |
<0.001 |
| Na+ (mEq/L) |
140 (138, 142) |
141 (139, 143) |
140 (137, 143) |
139 (137, 140) |
<0.001 |
| K+ (mEq/L) |
4.2 (3.7, 4.9) |
4.6 (3.9, 5.2) |
4.3 (3.6, 5.3) |
3.8 (3.4, 4.1) |
<0.001 |
| eGFR (mL/min/1.73 m2) |
47 (38, 59) |
43 (37, 53) |
47 (33, 62) |
56 (47, 65) |
<0.001 |
Continuous variables are summarized as median and interquartile range (IQR), whereas categorical variables are summarized as frequencies and percentages (%). *P value: Pearson’s Chi-squared test or Kruskal-Wallis rank sum test. Probability of misclassification is indicated in
Supplementary Figure 3. Alb, albumin; BE, base excess; BT, body temperature (℃); CPR, cardiopulmonary resuscitation; eGFR, estimated glomerular filtration rate; Glu, glucose; K+, serum potassium (mEq/L); Na+, serum sodium (mEq/L); PCO2, partial pressure of CO2 (mmHg); PEA, pulseless electrical activity; PO2, partial pressure of O2 (mmHg); ROSC, return of spontaneous circulation; VF, ventricular fibrillation; VT, pulseless ventricular tachycardia.
In the development dataset, 16 variables were used in the subphenotype clustering (Supplementary Appendix 2). The optimal clustering number was 3, based on the BIC values (Supplementary Figure 2). For identifying these 3 groups, the variable with the highest discriminative power was partial pressure of O2
(PO2), followed by partial pressure of CO2
(PCO2), cardiac rhythm on arrival, eGFR and albumin (Alb) (Figure 2, Supplementary Figure 4).
The characteristics and distribution of variables with high discriminative power among the patients in the development dataset are shown by groups in
Table
and
Figure 3. The patients in Group 1 had the lowest PO2
values and the highest PCO2
values. Group 2 had higher PO2
values and lower PCO2
values than Group 1. Group 3 had high PO2
values as per Group 2, the lowest PCO2
values, the highest pH value, proportion of return of spontaneous circulation (ROSC) at hospital arrival, and eGFR value.
Association Between Subphenotypes and Outcomes in the Development Dataset
As the primary outcome, 30-day survival was 15.7% (71/453) in Group 1, 30.7% (65/212) in Group 2, and 85.9% (219/255) in Group 3 (Figure 4). The crude OR [95% CI] for the primary outcome was 0.031 [0.02–0.047] for Group 1 and 0.073 [0.045–0.114] for Group 2 compared with Group 3.
As the secondary outcome, 30-day survival with favorable neurological outcome was 7.3% (33/453) in Group 1, 18.9% (40/212) in Group 2, and 75.3% (192/255) in Group 3 (Figure 4). The crude OR [95% CI] for the secondary outcome was 0.026 [0.016–0.04] for Group 1 and 0.076 [0.048–0.118] for Group 2 compared with Group 3.
Association Between Subphenotypes and Outcomes in the Validation Dataset
In the validation dataset, the characteristics of Groups 1 to 3 were similar to those of the development dataset (Supplementary Table 4, Supplementary Figure 5). The association between groups and outcomes in the validation dataset were also similar to those in the development dataset (Supplementary Figure 6, Supplementary Appendix 3).
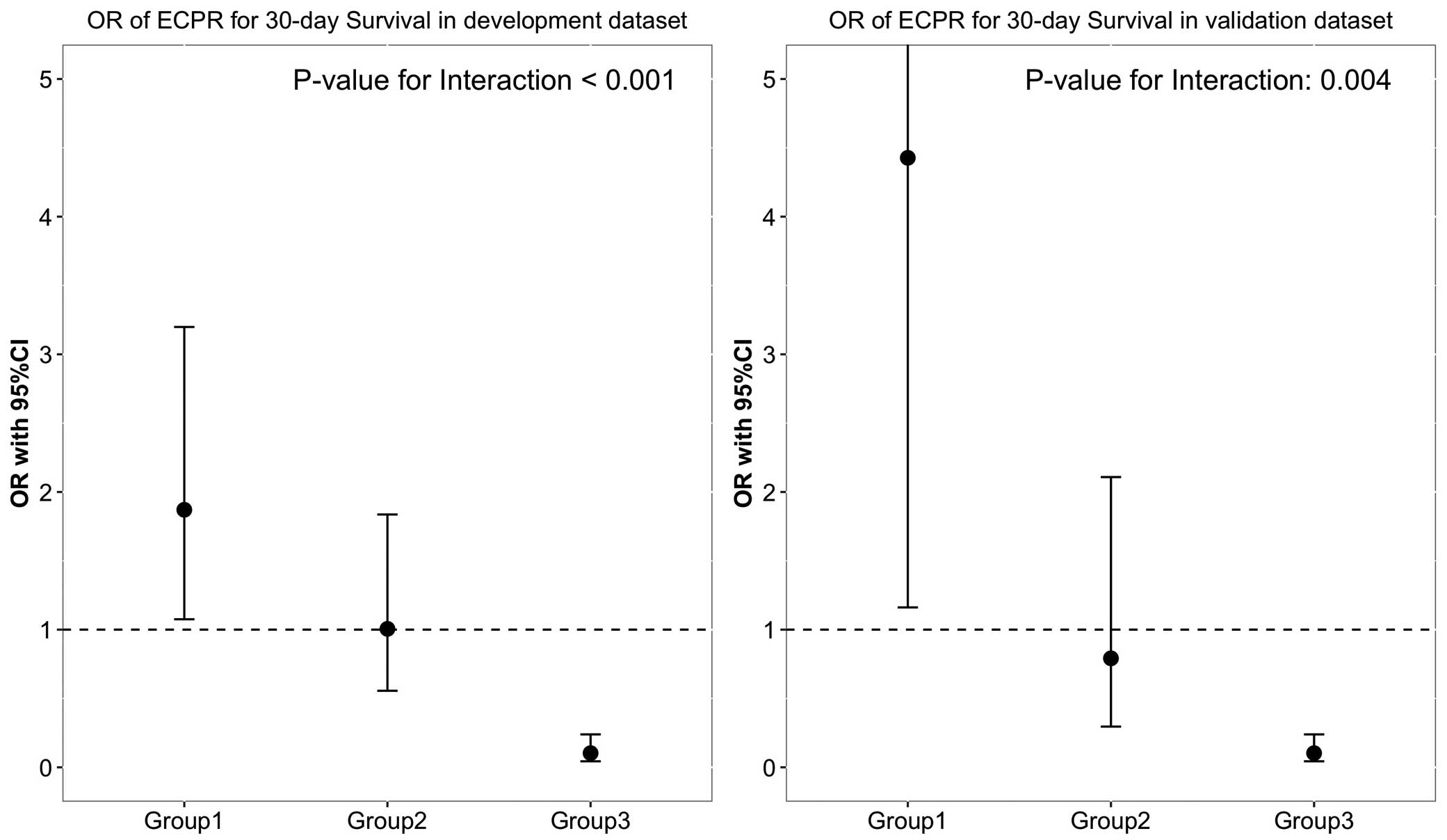
Heterogeneity of the Association Between ECPR and Outcomes Among Subphenotypes
In the development dataset, ECPR was performed for 24.5% (111/453) of Group 1, 59.9% (127/212) of Group 2, and 11.8% (30/255) of Group 3. The association between ECPR and 30-day survival outcome by subphenotype group in the development dataset was as follows: Group 1: 1.87 (1.08–3.2); Group 2: 1.01 (0.56–1.84); and Group 3: 0.1 (0.04–0.24) (P value for interaction <0.001;
Figure 4). In the validation dataset, the association between ECPR and 30-day survival outcome by subphenotype groups was also similar to those in the development dataset (Figure 4, Supplementary Appendix 3).
Discussion
This study, using a multi-institutional prospective OHCA registry and an unsupervised machine learning-based clustering approach, revealed 3 types of subphenotypes among OHCA patients with shockable rhythm. These subphenotypes were associated with 30-day survival and favorable neurological outcomes. Further, the subphenotypes had heterogeneity of association between ECPR implementation and survival outcome. The replicability of these subphenotypes was confirmed with the validation dataset.
We believe it is reasonable that the 3 variables with the highest discriminative power to differentiate the clusters associated with the outcomes were parameters of circulation (PO2, PCO2, and ROSC). This is because we assume that the most important hidden comprehensive factors that decide the prognosis among OHCA patients may be the hemodynamic state, which consists of the quality of the CPR and ROSC, and we believe that the blood test parameters (PO2
and PCO2) are the surrogate markers of the quality of CPR. Generally, arterial oxygen tension indicates alveolar oxygenation and delivery of the oxygen in systemic circulation. During resuscitation, arterial oxygen tension may be considered as indicative of the quality of CPR, and it was reported to be associated with ROSC and survival outcome.23–25
Moreover, arterial carbon dioxide tension is representative of inadequate carbon dioxide discharge and is mostly caused by low venous return by chest compressions and deficient alveolar ventilation during resuscitation.26,27
Thus, it is reasonable that PCO2
can distinguish the subphenotypes between Groups 2 and 3, which were patients who had a high PO2
value. Further, cardiac rhythm (ROSC) on hospital arrival, which has the third highest discriminative power, is normally associated with adequate perfusion and venous return.
Surprisingly, the fourth highest discriminative power was eGFR value. This may largely reflect the condition of chronic kidney disease (CKD) rather than acute kidney injury, because time from call to hospital arrival is within 45 min in most cases; however, acute kidney injury physiologically progresses in several hours.28
In general, CKD is a well-known major risk factor for cardiovascular events or sudden death.29,30
Previous studies have shown that low eGFR value is associated with death and unfavorable neurological outcome among OHCA patients.31,32
Moreover, CKD was reported as a risk factor for ventricular arrhythmia among patients with myocardial infarction.33,34
Additionally, animal experiments reported that CKD could lead to increasing vulnerability to lethal ventricular arrhythmia.35,36
Similarly, the results for Group 3, who had a higher eGFR value than that in other groups, found that the proportion of ROSC at hospital arrival was high. Therefore, it might be reasoned that the patients in Groups 1 or 2 would have a high possibility of reoccurrence or sustaining of the VF, even if defibrillation were performed, and that they would have poor neurological outcomes.
Thus, these parameters may reasonably be assumed to have discriminative power to distinguish between the groups of OHCA patients with shockable rhythm.
This study has several strengths compared to previous studies. First, to the best of our knowledge, this was the first study to investigate the subphenotypes of OHCA patients with initial shockable rhythm. Previous studies used traditional methods such as logistic analysis to identify factors associated with the outcomes such as age, duration of low-flow time, cardiac rhythm conversion, metabolic or respiratory acidosis, or some biomarkers.4–6,37–44
Generally, these single factors are not suitable for detecting and classifying heterogeneous patient groups because other factors are ignored.12
However, our clustering technique considers multidimensional clinical factors for identifying the subphenotypes. Second, we used the latent class analysis to be able to consider clinically meaningful categorical variables, such as cardiac rhythm on hospital arrival or the presence of a witness, in addition to continuous variables. Some previous studies used other clustering methods, such as k-means clustering;7,45,46
however, these methods are limited because they cannot include categorical variables that may be clinically important. Finally, there are general concerns about the validation and replicability of clustering results.12
In this study, the results with the validation dataset supported the validation and replicability of the clustering subphenotypes; thus, it may be reasonable to conclude that this result is generalizable to other similar settings.
We described several clinical and research implications. First, developing the subphenotypes may be valuable in understanding the conditions and pathogenesis of OHCA patients with shockable rhythm. Thus, we assume that the subphenotypes may represent the cardiovascular risk and quality of CPR. This hypothesis suggests a potential association between the eGFR value and the incidence of refractory VF. Further, the results suggest that the blood gas parameters would be valuable factors when considering the association between CPR quality and outcomes or monitoring the CPR quality. These hypotheses could lead to further research to understand the pathogenesis of OHCA patients.
Second, this study suggests clinical and research implications to consider in the indication of ECPR. Currently, the assumed favorable effect of ECPR for OHCA is still controversial. Only one small size randomized controlled trial (RCT) including 30 participants reported the proportion of survivors in the ECPR group being higher than in the conventional CPR group;2
however, a systematic review of observational studies indicated that the effect is controversial.47
We consider that it may be because patients treated by ECPR were heterogeneous48,49
and the appropriate target population of ECPR has not yet been clearly defined. Further, some RCTs or most observational studies that investigate the efficacy of ECPR focus on the following patients: aged <70 or 75 years who experience OHCA with initial shockable rhythm but do not obtain ROSC with or without witnesses or bystanders CPR.2,50–52
In these criteria, excluding patients with ROSC is consistent with our result for Group 3 who mostly obtained ROSC and were not suitable as the target population for ECPR. Meanwhile, these criteria for ECPR do not consist of the physiological state and could not appropriately differentiate Groups 1 and 2. We believe that excluding the physiological state from these inclusion criteria is one of the reasons that the results in previous observational studies were heterogeneous. Hence, we suggest that when considering the indication of ECPR or planning the studies investigating the effects of ECPR, the concept of subphenotypes based on the physiological biomarkers may be valuable.
This study has several limitations. First, although the clinical data were prospectively collected using a pre-specified datasheet, some of the data were missed, or had measurement errors. Specifically, the blood test was defined as a blood sample collected on hospital arrival; however, the timing might have been different in each institution, possibly biasing the results. Second, we lacked other data that might have been significant for clustering; for example, details of patient characteristics such as comorbidities or the situation of the cardiac arrest. If more variables were available, more accurate clustering could be developed. Third, although there is no standard in considering sample size, and we believe that this study had an adequate sample size for clustering, small sample sizes have a risk of inaccurate estimation. Fourth, regarding the association between ECPR and outcomes, there might be unmeasured confounding factors that we could not control. Fifth, although we confirmed similar results with the split dataset to address the concerns of validity in clustering, there is currently no gold standard to validate data clustering results. Therefore, the validity of the clustering could be limited. Finally, the replication and generalizability of the results to other settings is unclear. Therefore, further research is necessary to manage these bias risks and applicability concerns.
Conclusions
In summary, using a machine learning-based unsupervised clustering technique, this study identified 3 subphenotypes which were associated with different outcomes. Further, among the subphenotypes, the heterogeneity of the association between ECPR implementation and outcomes was observed. This concept of subphenotypes might be valuable when considering the appropriate target population of ECPR. Further research is necessary to validate these results.
Acknowledgments
The authors are deeply grateful to all EMS personnel for collecting Utstein data and to Ms. Ikuko Nakamura and Yumiko Murai for supporting the CRITICAL study. The authors thank their colleagues from Osaka University Centre of Medical Data Science and Advanced Clinical Epidemiology Investigator’s Research Project for providing their insight and expertise for the research.
Sources of Funding
This work was supported by the Ministry of Education, Culture, Sports, Science and Technology of Japan (grant numbers 15H05006 and 19K09393).
Disclosures
A.H. is a member of
Circulation Journal’s Editorial Team. All other authors declare that they have no conflicts of interests.
IRB Information
The Ethics Committee of Kyoto University and each participating institution approved this study protocol and retrospective analysis, and written informed consent was waived (Approval ID: R1045).
Data Availability
The datasets and/or analysis in this study are not publicly available because the ethics committee does not permit it.
Supplementary Files
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-21-0675
References
- 1.
Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020; 142: S366–S468.
- 2.
Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): A phase 2, single centre, open-label, randomised controlled trial. The Lancet 2020; 396: 1807–1816.
- 3.
Nakashima T, Noguchi T, Tahara Y, Nishimura K, Ogata S, Yasuda S, et al. Patients with refractory out-of-cardiac arrest and sustained ventricular fibrillation as candidates for extracorporeal cardiopulmonary resuscitation: Prospective multi-center observational study. Circ J 2019; 83: 1011–1018.
- 4.
Okada Y, Kiguchi T, Irisawa T, Yoshiya K, Yamada T, Hayakawa K, et al. Association between low pH and unfavorable neurological outcome among out-of-hospital cardiac arrest patients treated by extracorporeal CPR: A prospective observational cohort study in Japan. J Intensive Care 2020; 8: 34.
- 5.
Matsuyama T, Irisawa T, Yamada T, Hayakawa K, Yoshiya K, Noguchi K, et al. Impact of low-flow duration on favorable neurological outcomes of extracorporeal cardiopulmonary resuscitation after out-of-hospital cardiac arrest: A multicenter prospective study. Circulation 2020; 141: 1031–1033.
- 6.
Kandori K, Okada Y, Okada A, Nakajima S, Okada N, Matsuyama T, et al. Association between cardiac rhythm conversion and neurological outcome among cardiac arrest patients with initial shockable rhythm: A nationwide prospective study in Japan. Eur Heart J Acute Cardiovasc Care 2021; 10: 119–126.
- 7.
Seymour CW, Kennedy JN, Wang S, Chang CCH, Elliott CF, Xu Z, et al. Derivation, validation, and potential treatment implications of novel clinical phenotypes for sepsis. JAMA 2019; 321: 2003–2017.
- 8.
Sinha P, Churpek MM, Calfee CS. Machine learning classifier models can identify acute respiratory distress syndrome phenotypes using readily available clinical data. Am J Respir Crit Care Med 2020; 202: 996–1004.
- 9.
Segar MW, Patel KV, Ayers C, Basit M, Tang WHW, Willett D, et al. Phenomapping of patients with heart failure with preserved ejection fraction using machine learning-based unsupervised cluster analysis. Eur J Heart Fail 2020; 22: 148–158.
- 10.
Reddy K, Sinha P, O’Kane CM, Gordon AC, Calfee CS, McAuley DF. Subphenotypes in critical care: Translation into clinical practice. Lancet Respir Med 2020; 8: 631–643.
- 11.
Wildi K, Livingstone S, Palmieri C, LiBassi G, Suen J, Fraser J. The discovery of biological subphenotypes in ARDS: A novel approach to targeted medicine? J Intensive Care 2021; 9: 14.
- 12.
Mori M, Krumholz HM, Allore HG. Using latent class analysis to identify hidden clinical phenotypes. JAMA 2020; 324: 700–701.
- 13.
Sinha P, Calfee CS, Delucchi KL. Practitioner’s guide to latent class analysis: Methodological considerations and common pitfalls. Crit Care Med 2021; 49: e63–e79.
- 14.
Yamada T, Kitamura T, Hayakawa K, Yoshiya K, Irisawa T, Abe Y, et al. Rationale, design, and profile of Comprehensive Registry of In-Hospital Intensive Care for OHCA Survival (CRITICAL) study in Osaka, Japan. J Intensive Care 2016; 4: 10.
- 15.
Yoshimura S, Hirayama A, Kiguchi T, Irisawa T, Yamada T, Yoshiya K, et al. Trends in in-hospital advanced management and survival of out-of-hospital cardiac arrest among adults from 2013 to 2017: A multicenter, prospective registry in Osaka, Japan. Circ J 2021; 85: 1851–1859.
- 16.
Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update and simplification of the Utstein templates for resuscitation registries: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 2004; 110: 3385–3397.
- 17.
Waljee AK, Mukherjee A, Singal AG, Zhang Y, Warren J, Balis U, et al. Comparison of imputation methods for missing laboratory data in medicine. BMJ Open 2013; 3: e002847, doi:10.1136/bmjopen-2013-002847.
- 18.
Stekhoven DJ, Bühlmann P. MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics 2012; 28: 112–118.
- 19.
Japanese Society of Nephrology. Evidence-based clinical practice guidelines for CKD 2018. The Japanese Journal of Nephrology 2018; 60: 1037–1193.
- 20.
Finch WH, Bronk KC. Conducting confirmatory latent class analysis using M plus. Structural Equation Modeling 2011; 18: 132–151.
- 21.
Marbac M, Sedki M. VarSelLCM: An R/C++ package for variable selection in model-based clustering of mixed-data with missing values. Bioinformatics 2019; 35: 1255–1257.
- 22.
Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: The Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation 1991; 84: 960–975.
- 23.
Patel JK, Schoenfeld E, Parikh PB, Parnia S. Association of arterial oxygen tension during in-hospital cardiac arrest with return of spontaneous circulation and survival. J Intensive Care Med 2018; 33: 407–414.
- 24.
Spindelboeck W, Schindler O, Moser A, Hausler F, Wallner S, Strasser C, et al. Increasing arterial oxygen partial pressure during cardiopulmonary resuscitation is associated with improved rates of hospital admission. Resuscitation 2013; 84: 770–775.
- 25.
Skrifvars MB, Olasveengen TM, Ristagno G. Oxygen and carbon dioxide targets during and after resuscitation of cardiac arrest patients. Intensive Care Med 2019; 45: 284–286.
- 26.
Magliocca A, Olivari D, De Giorgio D, Zani D, Manfredi M, Boccardo A, et al. LUCAS versus manual chest compression during ambulance transport: A hemodynamic study in a porcine model of cardiac arrest. J Am Heart Assoc 2019; 8: e011189.
- 27.
Sandroni C, De Santis P, D’Arrigo S. Capnography during cardiac arrest. Resuscitation 2018; 132: 73–77.
- 28.
Endre ZH, Pickering JW, Walker RJ. Clearance and beyond: The complementary roles of GFR measurement and injury biomarkers in acute kidney injury (AKI). Am J Physiol Renal Physiol 2011; 301: F697–F707.
- 29.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004; 351: 1296–1305.
- 30.
Nakamura K, Okamura T, Hayakawa T, Kadowaki T, Kita Y, Ohnishi H, et al. Chronic kidney disease is a risk factor for cardiovascular death in a community-based population in Japan: NIPPON DATA90. Circ J 2006; 70: 954–959.
- 31.
Tamura T, Suzuki M, Hayashida K, Sasaki J, Yonemoto N, Sakurai A, et al. Renal function and outcome of out-of-hospital cardiac arrest: Multicenter Prospective Study (SOS-KANTO 2012 Study). Circ J 2018; 83: 139–146.
- 32.
Kuroki N, Abe D, Iwama T, Sugiyama K, Akashi A, Hamabe Y, et al. Prognostic effect of estimated glomerular filtration rate in patients with cardiogenic shock or cardiac arrest undergoing percutaneous veno-arterial extracorporeal membrane oxygenation. Journal of Cardiology 2016; 68: 439–446.
- 33.
Oikawa J, Fukaya H, Ako J, Nakao K, Ozaki Y, Kimura K, et al. Risk factors of in-hospital lethal arrhythmia following acute myocardial infarction in patients undergoing primary percutaneous coronary intervention: Insight From the J-MINUET Study. Circulation Reports 2020; 2: 17–23.
- 34.
Piccini JP, Berger JS, Brown DL. Early sustained ventricular arrhythmias complicating acute myocardial infarction. Am J Med 2008; 121: 797–804.
- 35.
Tang X, Shi L, Cui X, Yu Y, Qi T, Chen C, et al. Renal denervation decreases susceptibility of the heart to ventricular fibrillation in a canine model of chronic kidney disease. Exp Physiol 2017; 102: 1414–1423.
- 36.
Hsueh CH, Chen NX, Lin SF, Chen PS, Gattone VH, Allen MR, et al. Pathogenesis of arrhythmias in a model of CKD. J Am Soc Nephrol 2014; 25: 2812–2821.
- 37.
Orban JC, Novain M, Cattet F, Plattier R, Nefzaoui M, Hyvernat H, et al. Association of serum lactate with outcome after out-of-hospital cardiac arrest treated with therapeutic hypothermia. PLoS One 2017; 12: e0173239.
- 38.
Nagao K, Nonogi H, Yonemoto N, Gaieski DF, Ito N, Takayama M, et al. Duration of prehospital resuscitation efforts after out-of-hospital cardiac arrest. Circulation 2016; 133: 1386–1396.
- 39.
McKenzie N, Williams TA, Tohira H, Ho KM, Finn J. A systematic review and meta-analysis of the association between arterial carbon dioxide tension and outcomes after cardiac arrest. Resuscitation 2017; 111: 116–126.
- 40.
Jamme M, Ben Hadj Salem O, Guillemet L, Dupland P, Bougouin W, Charpentier J, et al. Severe metabolic acidosis after out-of-hospital cardiac arrest: Risk factors and association with outcome. Ann Intensive Care 2018; 8: 62.
- 41.
Hope Kilgannon J, Hunter BR, Puskarich MA, Shea L, Fuller BM, Jones C, et al. Partial pressure of arterial carbon dioxide after resuscitation from cardiac arrest and neurological outcome: A prospective multi-center protocol-directed cohort study. Resuscitation 2019; 135: 212–220.
- 42.
Nakamura F, Kajino K, Kitamura T, Daya MR, Ong ME, Matsuyama T, et al. Impact of age on survival of patients with out-of-hospital cardiac arrest transported to tertiary emergency medical institutions in Osaka, Japan. Geriatr Gerontol Int 2019; 19: 1088–1095.
- 43.
Okabayashi S, Matsuyama T, Kitamura T, Kiyohara K, Kiguchi T, Nishiyama C, et al. Outcomes of patients 65 years or older after out-of-hospital cardiac arrest based on location of cardiac arrest in Japan. JAMA Netw Open 2019; 2: e191011.
- 44.
Shida H, Matsuyama T, Iwami T, Okabayashi S, Yamada T, Hayakawa K, et al. Serum potassium level on hospital arrival and survival after out-of-hospital cardiac arrest: The CRITICAL study in Osaka, Japan. Eur Heart J Acute Cardiovasc Care 2020; 9(4_suppl): S175–S183.
- 45.
Nowak RM, Reed BP, Nanayakkara P, DiSomma S, Moyer ML, Millis S, et al. Presenting hemodynamic phenotypes in ED patients with confirmed sepsis. Am J Emerg Med 2016; 34: 2291–2297.
- 46.
Zampieri FG, Costa EL, Iwashyna TJ, Carvalho CRR, Damiani LP, Taniguchi LU, et al. Heterogeneous effects of alveolar recruitment in acute respiratory distress syndrome: A machine learning reanalysis of the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial. Br J Anaesth 2019; 123: 88–95.
- 47.
Miraglia D, Miguel LA, Alonso W. Extracorporeal cardiopulmonary resuscitation for in- and out-of-hospital cardiac arrest: Systematic review and meta-analysis of propensity score-matched cohort studies. J Am Coll Emerg Physicians Open 2020; 1: 342–361.
- 48.
Koen TJ, Nathanaël T, Philippe D. A systematic review of current ECPR protocols: A step towards standardisation. Resusc Plus 2020; 3: 100018.
- 49.
Okada Y, Kiguchi T, Irisawa T, Yamada T, Yoshiya K, Park C, et al. Development and validation of a clinical score to predict neurological outcomes in patients with out-of-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation. JAMA Network Open 2020; 3: e2022920.
- 50.
Bol ME, Suverein MM, Lorusso R, Delnoij TSR, Brandon Bravo Bruinsma GJ, Otterspoor L, et al. Early initiation of extracorporeal life support in refractory out-of-hospital cardiac arrest: Design and rationale of the INCEPTION trial. Am Heart J 2019; 210: 58–68.
- 51.
Holmberg MJ, Geri G, Wiberg S, Guerguerian AM, Donnino MW, Nolan JP, et al. Extracorporeal cardiopulmonary resuscitation for cardiac arrest: A systematic review. Resuscitation 2018; 131: 91–100.
- 52.
Ahn C, Kim W, Cho Y, Choi KS, Jang BH, Lim TH. Efficacy of extracorporeal cardiopulmonary resuscitation compared to conventional cardiopulmonary resuscitation for adult cardiac arrest patients: A systematic review and meta-analysis. Sci Rep 2016; 6: 34208.