2023 Volume 87 Issue 9 Pages 1238-1239
2023 Volume 87 Issue 9 Pages 1238-1239
Since the TACT trial was first reported, numerous follow-up studies have demonstrated the efficacy of therapeutic angiogenesis with cell therapy.1 Therapeutic angiogenesis is a treatment intended to restore blood flow to ischemic tissue by artificially stimulating the regeneration and development of blood vessels at the capillary level. Therapeutic angiogenesis for Critical Limb-Threatening Ischemia (CLTI) is attracting attention worldwide as a next-generation treatment for patients whose limbs cannot be saved with any other conventional therapies including surgical bypass.2–4
Article p 1229
Thromboangiitis obliterans (TAO), as known as Buerger’s disease, is condition in which vascular inflammation occurs at the level of peripheral arteries in the extremities, resulting in vascular occlusion and disruption due to thrombus formation.5 Epidemiological studies have shown that the estimated prevalence of the disease per 105 individuals is ≈5–6.6 Although life expectancy is relatively unaffected, it is a social problem because it often requires extremity lower limb amputation if the limb becomes severely ischemic, resulting in a significant decrease in the quality of life among young patients of working age.6 The etiology of this intractable disease has been reported to be associated with specific genetic polymorphisms and smoking; however, the precise mechanism of disease remains largely unknown.7 Smoking cessation is strongly recommended in treatment guidelines, and in fact, there have been cases in which smoking cessation has relieved the disease.8 Other therapies include antiplatelet therapy and vasodilators for ischemic symptoms.8 Endovascular therapy and bypass surgery are also performed for severely occluded lesions; however, these procedures are often ineffective because the lesions are located at the level of peripheral capillary and small to medium-sized arteries and have little vascular bed.8 Recently, low-density lipoprotein apheresis or therapeutic angiogenesis has appeared as a promising treatment option. Regarding therapeutic angiogenesis, TAO has been shown to have a better response to treatment than atherosclerotic peripheral artery disease.9
In this issue of the Journal, Fujioka and colleagues10 provide several novel findings regarding therapeutic angiogenesis using bone marrow-derived mononuclear cells (BM-MNCs) implantation for patients with CLTI caused by TAO in a multicenter setting. They demonstrated the therapy for 22 patients in 6 institutions in Japan, and reported that only one of the 22 patients with the no-conventional treatment option underwent major amputation (i.e., the major amputation free survival rate was 95.5%) 180 days after therapy and 89.5% at 3years after therapy. Importantly, this has of significant clinical importance because it demonstrated the feasibility, safety, and efficacy of this therapy in a prospective multicenter setting. An interesting finding of their study is that 42.9% of patients who received this treatment did not successfully quit smoking.
This is a unique report that demonstrates favorable efficacy in the face of expected treatment resistance (i.e., smoking), and furthermore, the study shows that even in such a patient population, the long-term results show that the legacy effect of the initial treatment was maintained for up to 3 years.10 Another interesting finding of note is that its classified parameters improved in all patients (9 of 9 patients) 180 days after the therapy in Fontaine class III patients, whereas in Fontaine class IV patients, the classified parameters improved in only one of 12 patients (8.3%).10 This suggests that the most severe-stage patients may have a poor response to this treatment. Currently, most of the studies on therapeutic angiogenesis have been conducted in patients with no treatment options. In addition, most studies have been conducted in patients with advanced-stage disease (Fontaine class III or IV). In other words, the results of the present study suggest that, given the increased responsiveness of this therapy in earlier stages, early administration in the course of disease progression may improve the overall lifetime lower extremity limb salvage rate.
The current study has some limitations. First, the study was limited to 22 patients, and it is necessary to verify the results in a larger number of patients in the future to confirm the current evidence. Second, there was no control group for comparison with the treatment group. In Japan, planning of clinical research on regenerative medicine is problematic owing to the difficulty in setting up control groups, especially for patients with no treatment options.4 We need to consider the construction of a clinical trial design that will enable the establishment of a group that can be used as a comparative target.
This study showed favorable results for cell therapy for angiogenesis in CLTI patients as reported in previous studies.4 On the other hand, it similarly showed that there are cases in which lower limb salvage was not achieved even with this therapy (non-responder). Thus, we need to clarify more detailed mechanisms of angiogenesis at the molecular level in these cases, detect the factors that cause treatment resistance or promote angiogenesis from multiple perspectives, search for more efficient and capable cell sources other than the currently used cells, and develop optimal transplantation methods for cells for these cases (Figure). Additional reverse translational research to solve these issues and innovative medical engineering applications are expected in this field. Nevertheless, this study by Fujioka et al has successfully demonstrated the feasibility, efficacy, and safety of therapeutic angiogenesis using BM-MNCs for TAO in a multicenter setting.
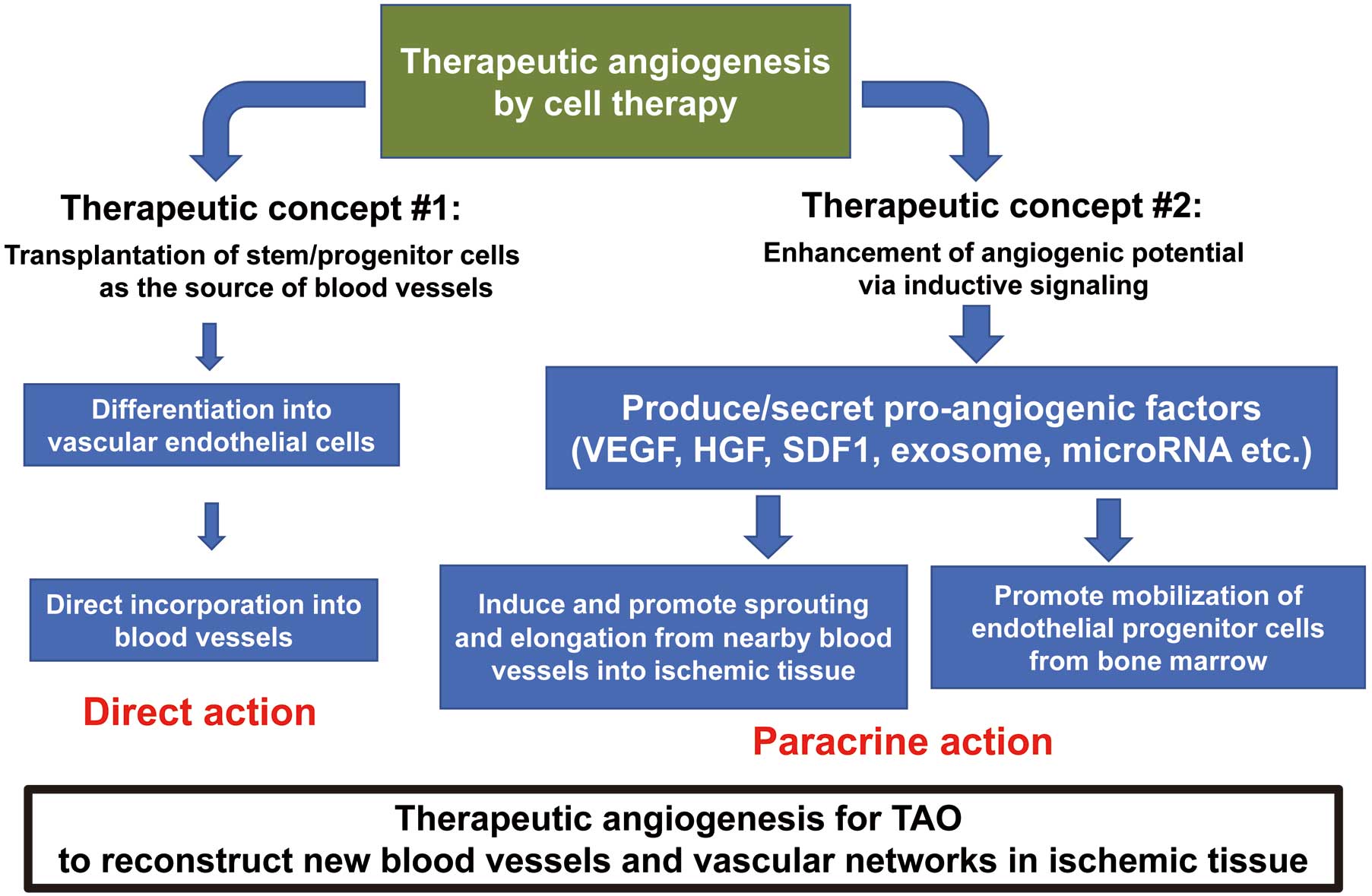
Schema for potential mechanisms of therapeutic angiogenesis for thromboangiitis obliterans (TAO). HGF, hematopoietic growth factor; VEGF, vascular endothelial growth factor.
Supported by a grant from the Ministry of Education, Culture, Sports, Science and Technology of Japan (No. 22K08201) to Y.S.
T.M. is a member of Circulation Journal’s Editorial Team.