2024 Volume 88 Issue 3 Pages 417-424
2024 Volume 88 Issue 3 Pages 417-424
Background: This study aimed to investigate the association between estimated pulse wave velocity (ePWV) and mortality outcomes among individuals with hypertension.
Methods and Results: Based on the National Health and Nutrition Examination Survey (NHANES) 1999–2018, a total of 14,396 eligible participants with hypertension were enrolled. The ePWV was calculated using the equation based on blood pressure and age. The mortality outcomes of included participants were directly acquired from the National Death Index database. The multivariable Cox regression analysis was used to examine the relationship between ePWV and mortality outcomes. Moreover, the restricted cubic spline (RCS) was also used to explore this relationship. Receiver operating characteristics curves (ROC) were adopted to evaluate the prognostic ability of ePWV for predicting mortality outcomes of patients with hypertension. The median follow-up duration was 10.8 years; individuals with higher an ePWV had higher risks of mortality from both all causes (HR: 2.79, 95% CI: 2.43–3.20) and cardiovascular diseases (HR: 3.41, 95% CI: 2.50–4.64). After adjusting for confounding factors, each 1 m/s increase in ePWV was associated with a 43% increase in all-cause mortality risk (HR: 1.43, 95% CI: 1.37–1.48) and a 54% increase in cardiovascular mortality risk (HR: 1.54, 95% CI: 1.43–1.66).
Conclusions: This study indicates that ePWV is a novel prognostic indicator for predicting the risks of mortality among patients with hypertension.
Hypertension is a significant global health problem, affecting millions of people worldwide; it is also a leading cause of death globally.1 Despite the availability of effective medications and lifestyle modifications, hypertension remains poorly controlled in many populations, leading to increased morbidity and mortality.2 Arterial stiffness is one of the major complications of hypertension, which can be measured through carotid-femoral pulse wave velocity (cf-PWV).3,4 cf-PWV is a measure of how quickly the pressure wave travels down the arterial tree; it is influenced by the elasticity and compliance of the arterial wall. However, due to the measurement of cf-PWV requiring specialized equipment and an experienced doctor, it is not widely used at present.5
Estimated PWV (ePWV), a novel non-invasive measurement for arterial stiffness, was calculated based on mean arterial blood pressure (MBP) and age; it has been shown to have a favorable prognostic value of cardiovascular disease (CVD) events and mortality outcomes in recent years.6–8 Although ePWV cannot replace cf-PWV, it has been confirmed that ePWV effectively detects arterial stiffness levels.9 Elevated ePWV levels signify stiffness of elastic arteries, which is linked to a higher likelihood of developing CVDs and mortality. The loss of arterial flexibility is a typical characteristic of aging in humans, and it is believed that vascular remodeling plays a crucial role in this process.10,11 Moreover, vascular remodeling is a process that is constantly changing and can be influenced by various factors such as lifestyle choices, genetic and epigenetic factors, as well as biological signals.12–14 Arterial stiffness is greater in patients with hypertension than in individuals without hypertension.9 However, the relationship between ePWV and mortality in people with hypertension remains uncertain.
As far as we know, there have been few studies examining the link between ePWV and mortality outcomes among individuals with hypertension. This study seeks to investigate how ePWV is linked to all-cause mortality and cardiovascular mortality in hypertensive patients through utilizing data from a diverse, large population who participated in the National Health and Nutrition Examination Survey (NHANES).
NHANES is an ongoing survey conducted every 2 years, which aims to evaluate the health and nutrition status of U.S. residents.15 Stratified multistage probability sampling is a method used in survey research to ensure representative and reliable data collection from a population of interest.16 This sampling technique involves multiple stages and incorporates stratification to enhance the precision of estimates and account for population heterogeneity. More information about the survey’s methods can be found on the NHANES website (http://www.cdc.gov/nchs/nhanes.htm). All participants from 10 consecutive NHANES cycles, conducted between 1999 and 2018, were initially enrolled. Individuals meeting any of the following criteria were classified as having hypertension: SBP ≥140 mmHg or DBP ≥90 mmHg, self-reported hypertension, or being prescribed antihypertensive medications.17,18 These criteria align with the guideline of the International Society of Hypertension.19 Of 101,316 NHANES participants, 24,039 were diagnosed with hypertension, and 14,396 adults with hypertension were finally included in this study after excluding ineligible individuals. The exclusion criteria included: (1) individuals aged <18 or ≥80 years; (2) an estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2; (3) participants lacking eligible follow-up data; and (4) pregnant individuals (Figure 1).

Flowchart of the study population. eGFR, estimated glomerular filtration rate.
ePWV Measurement
Experienced examiners followed the blood pressure measurement protocol of the American Heart Association, and participants were required to rest quietly in a seated position for 5 min before measuring their blood pressure.17 The average SBP and DBP were obtained and reported as the average value of three consecutive measurements. Similar to previous studies,20–22 the mean arterial blood pressure (MBP) was measured using algorithm (1):
MBP = DBP + [0.4 × (SBP – DBP)] (1)
ePWV was algorithmically calculated as algorithm (2):
ePWV = 9.587 – (0.402 × age) + [4.560 × 0.001 × (age2)] – [2.621 × 0.00001 × (age2) × MBP] + (3.176 × 0.001 × age × MBP) – (1.832 × 0.01 × MBP) (2)
Mortality OutcomesAll participants in the present study were connected to the National Death Index (NDI) database; this allowed information to be obtained from death certificates and determined if they had passed away. Public death records were used from the beginning until December 31, 2019 (the most recent update of the NDI database). We determined the mortality outcomes in accordance with the International Statistical Classification of Diseases (ICD-10).23,24 In the ICD-10, various codes are assigned to signify cardiovascular death, such as heart failure (I50), strokes or cerebrovascular accidents (CVA) (I60-I69), and negative impacts of agents affecting the cardiovascular system (T46).
CovariatesThe NHANES survey collected information on various demographic factors including age, sex, race/ethnicity, education levels, and family income through questionnaires. Health questionnaires were also used to determine the participants’ alcohol consumption, smoking status, and status of other chronic diseases. The Charlson comorbidity index (CCI) was calculated following the processes used in previously published studies.25,26 Body mass index (BMI) was grouped into three categories: <25.0, 25.0–29.9, and >29.9 kg/m2 based on the definitions of obesity and overweight of the World Health Organization.17,27,28 Blood samples were collected after at least an 8-h overnight fast.
Statistical MethodsThis study adhered to analytic and reporting guidance of the NHANES group, which utilized stratified multistage probability sampling to minimize bias. Each participant was assigned a specific sampling weight based on the primary sampling unit to ensure representative estimates at the national level. All data were analyzed using the 20-year survey weight. Continuous variables were reported as weighted means with 95% confidence intervals (CI), whereas categorical variables were reported as proportions with 95% CIs. The adjusted Wald test was used for continuous variables, and the Rao-Scott χ2 test was used for categorical variables to compare baseline characteristics. The relationship between ePWV and mortality risks was visualized using a restricted cubic spline (RCS) with three knots. Weighted multivariable Cox regression was utilized to further examine the association between ePWV and mortality risks. We ultimately selected 10 m/s as the cut-off value by referring to previous relevant literature on ePWV and mortality.7 Moreover, it also advises the use of 10 m/s as new cut-off value for cfPWV in expert consensus.29 Significant multicollinearity existed between age, systolic blood pressure, and ePWV; therefore, age and SBP were not included in the adjusted model (Supplementary Table 1). Hazard ratios and 95% CI were reported in Cox regression analysis results. R software (version 4.1.6, Rsoftware core team, Vienna, Austria) was used to carry out all statistical analyses. A P value <0.05 considered statistically significant.
We eventually enrolled 14,396 participants with hypertension, which represents 56.6 million individuals with hypertension. The mean age of the population was 52.8 years, and the weighted mean level of ePWV was 9.00 m/s. The results presented in Table 1 show that individuals with a higher ePWV (ePWV ≥1.0 m/s) were generally older (with an average age of 66.2 years compared to 46.1 years), more likely to have quit smoking, suffer from diabetes (24.7% vs. 18.9%) and CVDs. Additionally, a significantly higher proportion of participants with a CCI score of 2 or more were found among those with elevated ePWV.
Baseline Characteristics of the Study Population
| Overall (n=14,396) |
ePWV <10 m/s (n=8,476) |
ePWV ≥10 m/s (n=5,920) |
P value | |
|---|---|---|---|---|
| Age, years | 52.8 [52.3, 53.2] | 46.1 [45.6, 46.6] | 66.2 [65.9, 66.6] | <0.001* |
| Male, % | 52.5 [49.4, 55.6] | 54.5 [52.9, 56.2] | 48.4 [46.7, 50.2] | <0.001* |
| Race/ethnicity | <0.001* | |||
| White | 13.0 [11.7, 14.4] | 13.9 [12.2, 15.7] | 11.3 [9.6, 13.0] | |
| Black | 6.2 [5.2, 7.1] | 6.9 [5.7, 8.0] | 4.7 [3.7, 5.8] | |
| Mexican | 10.6 [9.4, 11.9] | 11.1 [9.7, 12.6] | 9.6 [8.1, 11.2] | |
| Others | 70.2 [64.4, 75.9] | 68.1 [65.3, 70.8] | 74.4 [71.7, 77.1] | |
| BMI, kg/m2 | <0.001* | |||
| Normal weight (<25.0) | 17.8 [16.7, 19.0] | 16.1 [14.9, 17.2] | 22.1 [20.7, 23.5] | |
| Over weight (25.0–29.9) | 48.0 [45.2, 50.8] | 51.9 [50.1, 53.6] | 42.1 [40.4, 43.8] | |
| Obesity (≥30.0) | 32.8 [30.7, 35.0] | 32.1 [30.5, 33.7] | 35.8 [34.1, 37.5] | |
| Drinking status | <0.001* | |||
| Non-drinker | 17.4 [16.0, 18.8] | 21.5 [20.0, 23.0] | 9.1 [7.7, 10.5] | |
| Low to moderate drinker | 48.9 [46.0, 51.7] | 48.0 [45.8, 50.2] | 50.7 [48.1, 53.3] | |
| Heavy drinker | 28.8 [26.4, 31.2] | 25.0 [23.1, 26.9] | 36.4 [33.9, 38.9] | |
| Not recorded | 5.0 [4.4, 5.6] | 5.5 [4.8, 6.3] | 3.9 [3.2, 4.5] | |
| Smoking status | <0.001* | |||
| Never smoker | 21.5 [19.8, 23.3] | 25.6 [24.0, 27.1] | 13.4 [12.4, 14.5] | |
| Ever smoker | 30.3 [28.1, 32.4] | 25.4 [24.1, 26.8] | 39.9 [37.6, 42.3] | |
| Current smoker | 47.5 [45.3, 50.0] | 48.0 [46.3, 49.8] | 46.5 [44.2, 48.8] | |
| Not recorded | 0.7 [0.4, 1.0] | 1.0 [0.6, 1.4] | 0.1 [0.0, 0.3] | |
| Education levels | <0.001* | |||
| Less than high school | 0.0 [0.0, 0.1] | 0.1 [0.0, 0.1] | 0.0 [0.0, 0.0] | |
| High school or equivalent | 54.2 [51.3, 57.1] | 56.0 [53.6, 58.4] | 50.6 [48.4, 52.7] | |
| College or above | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | |
| Not recorded | 39.1 [35.9, 42.3] | 39.0 [36.7, 41.4] | 39.3 [37.3, 41.3] | |
| Family income | 0.004** | |||
| <2,000$ | 19.7 [18.0, 21.4] | 18.6 [17.1, 20.1] | 22.0 [20.1, 23.9] | |
| ≥2,000$ | 77.0 [73.0, 81.1] | 78.5 [77.0, 80.1] | 74.0 [71.9, 76.0] | |
| Not recorded | 3.3 [2.6, 3.9] | 2.9 [2.2, 3.6] | 4.0 [2.7, 5.3] | |
| SBP, mmHg | 132.9 [132.3, 133.4] | 126.6 [126.1, 127.2] | 145.4 [144.6, 146.2] | <0.001* |
| DBP, mmHg | 75.8 [75.4, 76.3] | 75.5 [75.0, 76.0] | 76.5 [75.9, 77.1] | 0.004** |
| DM, % | 20.9 [19.5, 22.2] | 18.9 [17.7, 20.1] | 24.7 [23.1, 26.4] | <0.001* |
| CVD, % | 12.9 [11.9, 14.0] | 9.8 [8.9, 10.6] | 19.5 [18.0, 21.1] | <0.001* |
| CCI | <0.001* | |||
| ≥3 | 17.0 [15.8, 18.2] | 14.0 [13.0, 15.0] | 23.0 [21.3, 24.7] | |
| 0 | 44.5 [41.9, 47.0] | 51.0 [49.3, 52.7] | 31.3 [29.3, 33.3] | |
| 1 | 25.3 [23.5, 27.2] | 22.6 [21.0, 24.2] | 30.8 [29.0, 32.6] | |
| 2 | 13.3 [12.1, 14.4] | 12.5 [11.2, 13.7] | 14.9 [13.6, 16.1] |
Continuous variables are presented as the mean and 95% CI; category variables are presented as the proportion and 95% CI. BMI, body mass index; CCI, Charlson comorbidity index; CI, confidence interval; CVD, cardiovascular disease; DBP, diastolic blood pressure; DM, diabetes mellitus; ePWV, estimated pulse wave velocity; SBP, systolic blood pressure. *P value <0.001, **P value <0.01.
Associations of ePWV With Mortality Outcomes in a Population With Hypertension
The median follow-up time was 10.8 years. Overall, 2,587 (18.0%) of 8,916 patients with hypertension died, including 657 (4.6%) cardiovascular deaths. We observed a positive linear correlation between ePWV and all-cause and cardiovascular mortality, as shown in Figure 2. The risks of all-cause and cardiovascular mortality were higher in patients with higher ePWV, as demonstrated by the weighted Kaplan-Meier (KM) plots in Figure 3A and Figure 3B, respectively (P<0.001). We also found that every 1 m/s increase in ePWV was associated with a 43% and 54% increased risk of all-cause (HR: 1.43, 95% CI: 1.37–1.48) and cardiovascular mortality (HR: 1.54, 95% CI: 1.43–1.66), respectively. Participants with an ePWV ≥10 m/s had higher risks of mortality from both all causes (HR: 2.79, 95% CI: 2.43–3.20) and CVDs (HR: 3.41, 95% CI: 2.50–4.64). Despite adjusting for covariates, individuals with higher ePWV tend to have a higher prevalence of pre-existing CVD, as the characteristics of ePWV that are strongly associated with age contribute to this association. Subgroup analysis showed a favorable prognostic outcome regardless of whether patients had pre-existing CVD, as shown in Figure 4. Besides, we conducted an unweighted Cox regression analysis in sensitive analysis to further validate our conclusion (Table 2, Supplementary Table 2).
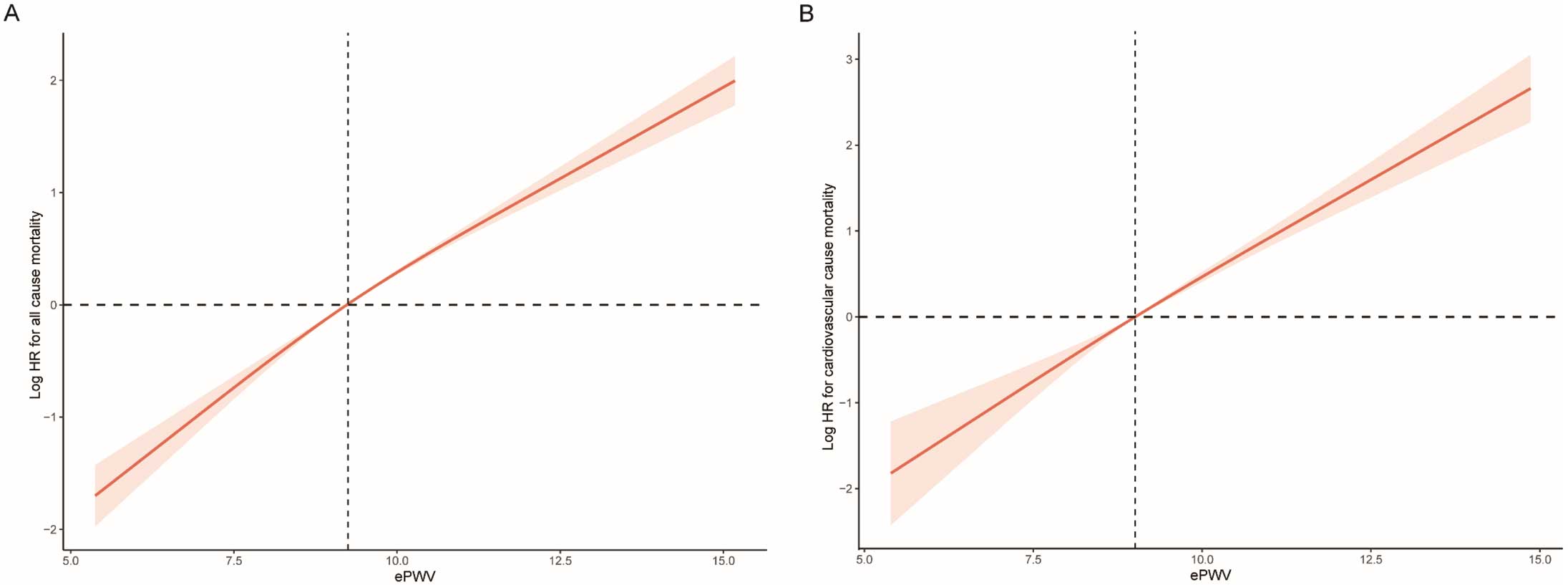
Association of ePWV with all-cause (A) and cardiovascular mortality (B) among participants with hypertension, visualized by the restricted cubic spline. Hazard ratios (HRs) were adjusted for sex, race/ethnicity, study circle, education levels, BMI, smoking, drinking, diabetes, hyperlipemia, eGFR, CVDs, and CCI. Both P value for linearity <0.001. BMI, body mass index; CVD, cardiovascular diseases; CCI, Charlson comorbidity index; eGFR, estimated glomerular filtration rate; ePWV, estimated pulse wave velocity.
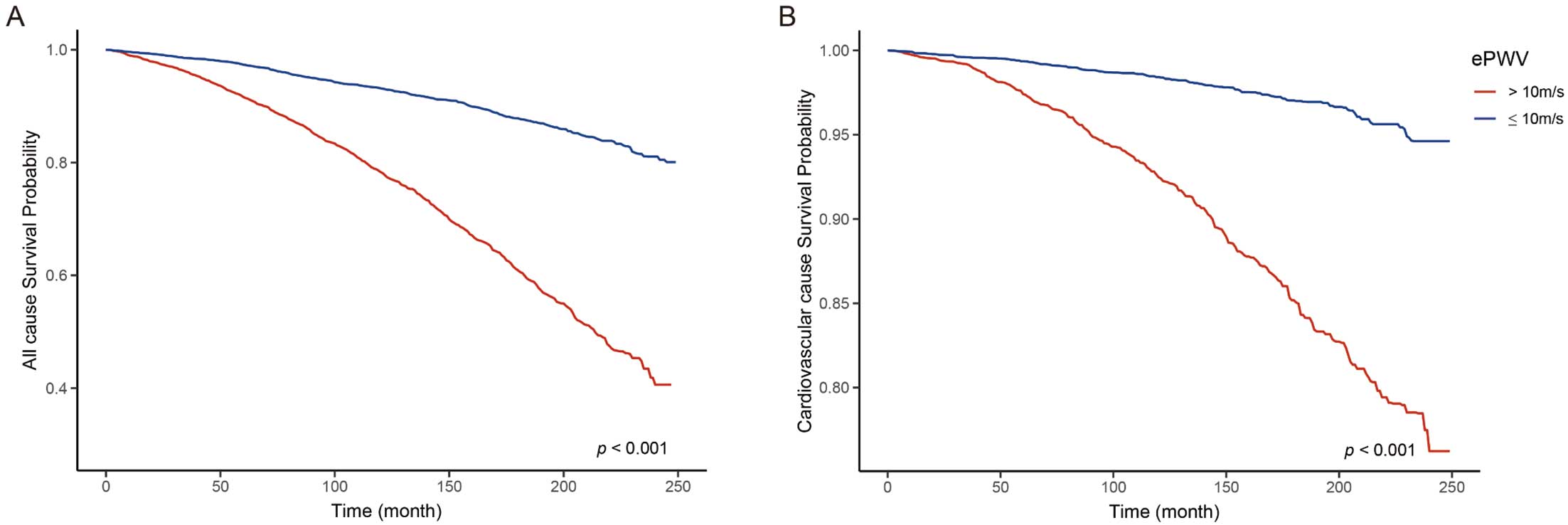
Kaplan-Meier survival curve of patients with normal (<10 m/s) ePWV and elevated (≥10 m/s) ePWV. ePWV, estimated pulse wave velocity. All-cause survival probability (A) and cardiovascular cause survival probability (B).

Subgroup analysis of the association between ePWV with all-cause (A) and cardiovascular mortality (B) among participants with hypertension. Hazard ratios (HRs) were adjusted for sex, race/ethnicity, study circle, education levels, BMI, smoking, drinking, diabetes, hyperlipemia, eGFR, CVDs, and CCI. BMI, body mass index; CCI, Charlson comorbidity index; CVD, cardiovascular diseases; eGFR, estimated glomerular filtration rate; ePWV, estimated pulse wave velocity; OR, odds ratio.
Cox Regression Analysis on the Association Between ePWV and All-Cause Mortality and Cardiovascular Mortality
| Non-adjusted model | Model I | Model II | ||||
|---|---|---|---|---|---|---|
| HR [95% CI] | P value | HR [95% CI] | P value | HR [95% CI] | P value | |
| All-cause mortality | ||||||
| Continuous ePWV | 1.48 [1.44, 1.51] | <0.001* | 1.49 [1.45, 1.53] | <0.001* | 1.43 [1.37, 1.48] | <0.001* |
| Normal ePWV | Reference | – | Reference | – | Reference | – |
| Elevated ePWV | 3.73 [3.35, 4.15] | <0.001* | 3.79 [3.39, 4.23] | <0.001* | 2.79 [2.43, 3.20] | <0.001* |
| Cardiovascular mortality | ||||||
| Continuous ePWV | 1.61 [1.53, 1.71] | <0.001* | 1.64 [1.55, 1.74] | <0.001* | 1.54 [1.43, 1.66] | <0.001* |
| Normal ePWV | Reference | – | Reference | – | Reference | – |
| Elevated ePWV | 4.91 [3.83, 6.29] | <0.001* | 5.14 [3.99, 6.62] | <0.001* | 3.41 [2.50, 4.64} | <0.001* |
Continuous ePWV represents HR per 1 m/s increase in ePWV with 95% CIs. Normal ePWV represents ePWV <10 m/s, elevated ePWV represents ePWV ≥10 m/s. Model I adjusted for sex, race/ethnicity, and study circle. Model II adjusted for sex, race/ethnicity, study circle, education levels, BMI, smoking, drinking, diabetes, hyperlipemia, eGFR, CVDs, and CCI. eGFR, estimated glomerular filtration rate; ePWV, estimated pulse wave velocity; HR, hazard ratio. Other abbreviations as in Table 1. *P value <0.001.
Evaluation of Predicting the Value of ePWV for Mortality Outcomes in a Population With Hypertension
We conducted time-dependent ROC curve analysis to assess the predictive value of ePWV for all-cause mortality and cardiovascular mortality. The findings demonstrated that ePWV exhibited good predictive accuracy for all-cause mortality in the short-term (AUC: 66.5%), medium-term (AUC: 67.9%), and long-term (AUC: 69.6%) (Figure 5A,B). For cardiovascular-caused mortality, ePWV also had a favorable prognostic value, with an AUC of 67.0%, 70.4% and 72.9% in 3, 5, and 10 years, respectively (Figure 5C,D).
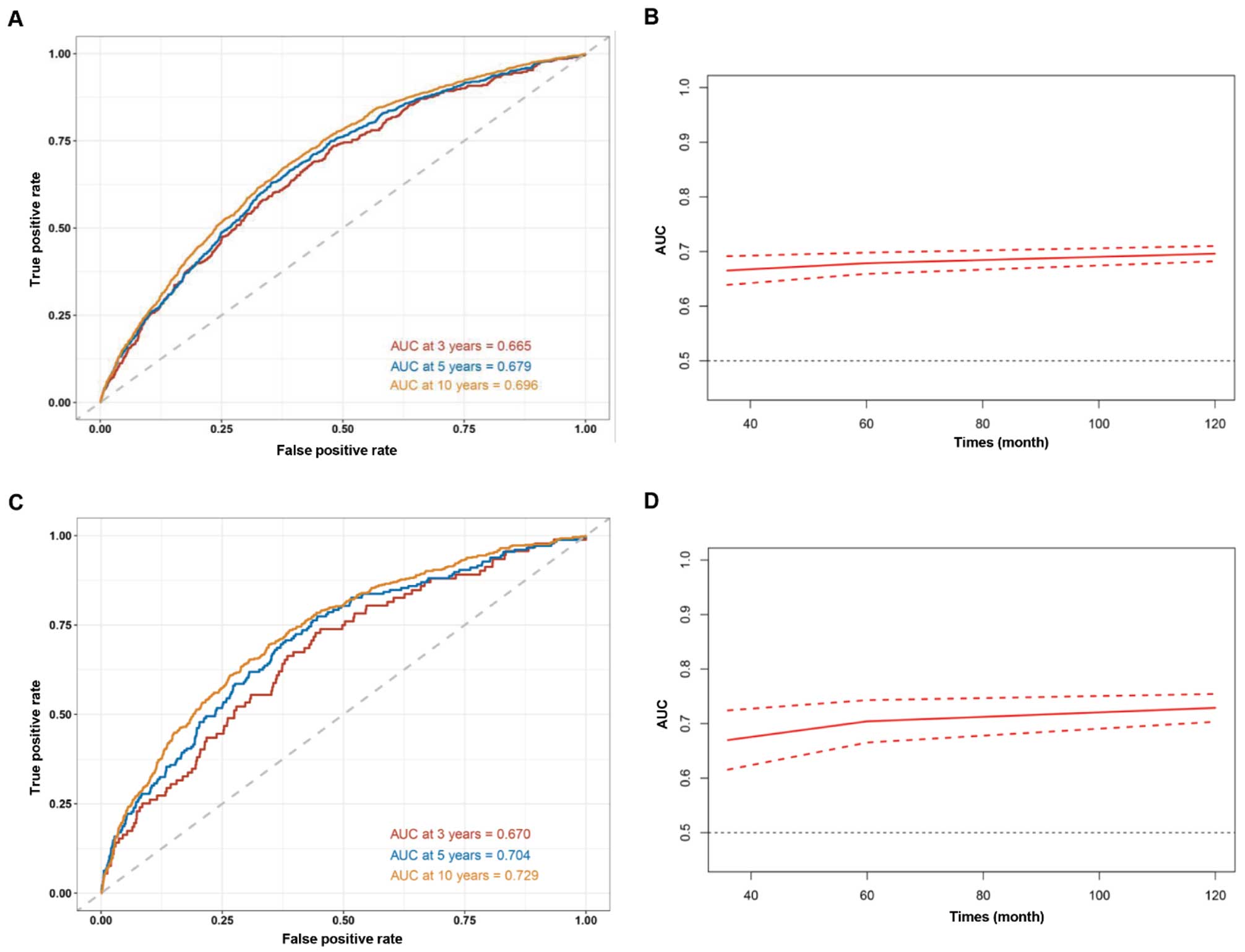
Time-dependent ROC curves (A) and time-dependent AUC values (B) of ePWV predicting all-cause mortality, and time-dependent ROC curves (C) and time-dependent AUC values (D) of ePWV predicting cardiovascular mortality. ePWV, estimated pulse wave velocity; ROC, receiver operating characteristic.
Arterial stiffness refers to the decreased ability of arteries to expand and contract, whereas hypertension is a condition characterized by high blood pressure levels.30,31 Stiffness is determined by the composition of the arterial wall, which is composed of smooth muscle cells, elastin fibers, and collagen fibers.32–34 With aging, the elastin fibers in the arterial wall become less elastic, leading to an increase in arterial stiffness. In addition, arterial stiffness can also result from inflammation, oxidative stress, and genetic factors.35,36 Hypertension can contribute to arterial stiffness, and increased pressure within the arteries can lead to structural changes in the arterial walls, causing them to become stiffer over time. Arterial stiffness, in turn, exacerbates hypertension by impairing the ability of arteries to accommodate the flow of blood, resulting in higher blood pressure levels. In contrast, hypertension can lead to arterial stiffness by causing remodeling of the arterial wall, leading to an increase in collagen content and a decrease in elastin content.37,38 Also in contrast, arterial stiffness can contribute to the development of hypertension by increasing pulse pressure, leading to endothelial dysfunction, and promoting atherosclerosis.38,39
Arterial stiffness is a strong predictor of cardiovascular risk, independent of traditional cardiovascular risk factors; therefore, the measurement of arterial stiffness could be used as a tool for the identification of individuals at high risk of CVD.40,41 It is crucial to assess arterial stiffness, particularly in high-risk individuals.42 However, cf-PWV is not commonly used in clinical practice.43,44 Brachial-ankle pulse wave velocity (baPWV) is a non-invasive measure used to assess arterial stiffness, which is calculated by measuring the time it takes for the pulse wave to travel from the brachial artery in the arm to the ankle artery in the leg. This measurement is simple and widely used in clinical practice because it requires less specialized equipment and expertise. baPWV has been shown to be a useful tool for evaluating cardiovascular risk and is often utilized to assess arterial health and predict future cardiovascular events.45,46 In 2010, ePWV was first introduced as a novel index to determine the level of arterial stiffness based on age and MBP. The use of ePWV has improved awareness of the hazards of arterial stiffness and aided physicians in clinical practice. This non-invasive measurement technique has played a crucial role in raising awareness among healthcare professionals regarding the potential hazards associated with arterial stiffness.47 By assessing ePWV, physicians can obtain valuable insights into the elastic properties of arteries and their ability to respond to changes in blood pressure. This information enables a more comprehensive evaluation of cardiovascular health and helps identify individuals at higher risk for various cardiovascular conditions. ePWV provides objective measurements of arterial stiffness, allowing for early detection and monitoring of this important risk factor. With this information, physicians can make informed decisions regarding treatment strategies, lifestyle modifications, and interventions to manage arterial stiffness and mitigate associated risks. Therefore, by incorporating this technology into routine clinical assessments, physicians can tailor individualized treatment plans and interventions to improve patient outcomes and overall cardiovascular health. The 2018 guideline from the European Society of Hypertension/European Society of Cardiology (ESH/ESC) suggests using PWV as an indicator of target organ damage for better prediction of cardiovascular risk.48 In the present study, ePWV was both analyzed as a continuous variable and divided into 2 groups using a clinical cut-off point advised by expert consensus and adopted in previously published studies, where the elevated ePWV group had ePWV values of at least 10 m/s and the normal ePWV group had values <10 m/s.29
Actually, researchers have extensively studied the clinical usefulness of ePWV before. Vishram-Nielsen et al conducted a substantial prospective study involving a low-risk European cohort and discovered that ePWV has the ability to forecast cardiovascular outcomes in the overall population.49 Similarly, an analysis of NHANES data revealed that higher ePWV levels strongly correlated with increased risks of cardiovascular and all-cause mortality in the general population.6 Heffernan et al also used NHANES data and discovered that ePWV has a predictive value for specific mortality.7 However, further research is needed to determine the effectiveness of ePWV in high-risk populations. Hametner et al found a correlation between ePWV and mortality in patients with suspected coronary artery disease who undergo invasive angiography.50 Arterial stiffness plays a major role in hypertension and can worsen the condition, leading to a harmful cycle. Vlachopoulos et al studied individuals from the Systolic Blood Pressure Intervention Trial (SPRINT) trial and found that ePWV was linked to increased risk of all-cause mortality and cardiovascular events in hypertensive patients after a follow-up period of 3.26 years.20 Our study differs from the SPRINT cohort study in several aspects: (1) we had a significantly longer follow-up period (a median of 10 years), compared to their median of 3.26 years; (2) we included a larger participant pool of 14,396 individuals, whereas they had 9,361 participants; (3) additionally, we accounted for more comprehensive confounding factors, such as the CCI. However, it is worth noting that in the multivariable Cox regression model, we found that there was multicollinearity between ePWV and age and blood pressure, as ePWV is calculated based on age and MBP. Adjusting for age and blood pressure would affect the model fit;51,52 therefore, we did not include these two covariates in the adjustment.
There are several strengths of our study. First, the long follow-up duration and large-scale sample size allowed for reliable conclusions. Second, the inclusion of participants from the NHANES survey minimized selection bias that can arise from including only specific hospitals and health insurance systems. Finally, the NDI database provided high-quality nationwide registers and direct follow-up and mortality information until death.
There were also several limitations to our study. First, cf-PWV was not available in the NHANES database, and further investigation is necessary to compare its prognostic potential with ePWV. Second, self-reported covariates from the NHANES database might have caused subjective bias. Finally, the generalizability of our findings to other populations outside the US needs further exploration in future studies.
In total, 14,396 adult participants with hypertension were enrolled in the prospective study, over a long-term follow-up period, and it was found that ePWV is associated with the increased risks of all-cause and cardiovascular mortality. As such, ePWV can be used as a prognostic indicator for patients with hypertension. Additionally, our findings highlight the potential benefits of earlier prevention strategies aimed at reducing arterial stiffness and decreasing the burden of hypertension.
We acknowledge the NHANES database for their contributors and providing their platforms for uploading meaningful datasets.
This research is funded by the National Natural Science Foundation of China (Grant No. 81970309 and No. 82170350).
The authors declare no competing interests.
S.-L.C., J.-X.Z. and Z.-Y.L. were involved in the experiment design. Y.S., L.-D.W. and X.-H.F. performed the data analysis. Y.S., L.-D.W. and J.-Y.K. wrote the manuscript. C.-H.K. reviewed the manuscript and provided critical suggestions.
The NCHS Ethics Review Board protects the rights and welfare of NHANES participants. The NHANES protocol complies with the U.S. Department of Health and Human Services Policy for the Protection of Human Research Subjects. NCHS IRB/ERC Protocol number: 2011–2017. Ethical review and approval were waived for this study as it solely used publicly available data for research and publication.
Publicly available datasets were analyzed in this study. These data can be found here: https://www.cdc.gov/nchs/nhanes/index.htm.
Please find supplementary file(s);
https://doi.org/10.1253/circj.CJ-23-0674