2024 Volume 88 Issue 5 Pages 642-648
2024 Volume 88 Issue 5 Pages 642-648
Background: Permanent pacemaker (PPM) implantation has been identified as a risk factor for morbidity and mortality after Fontan operation. This study investigated the factors associated with outcomes in patients with Fontan physiology who underwent PPM implantation.
Methods and Results: We retrospectively reviewed 508 patients who underwent Fontan surgery at Asan Medical Center between September 1992 and August 2022. Of these patients, 37 (7.3%) received PPM implantation. Five patients were excluded, leaving 32 patients, of whom 11 were categorized into the poor outcome group. Poor outcomes comprised death, heart transplantation, and “Fontan failure”. Clinical, Fontan procedure-related, and PPM-related factors were compared between the poor and good outcome groups. Ventricular morphology, Fontan procedure-associated factors, pacing mode, high ventricular pacing rate, and time from first arrhythmia to PPM implantation did not differ significantly between the 2 groups. However, the poor outcome group exhibited a significantly longer mean paced QRS duration (P=0.044). Receiver operating characteristic curve analysis revealed a paced QRS duration cut-off value of 153 ms with an area under the curve of 0.73 (P=0.035).
Conclusions: A longer paced QRS duration was associated with poor outcomes, indicating its potential to predict adverse outcomes among Fontan patients.
Patients with a single ventricle generally undergo staged operations, including neonatal palliative operation, bidirectional cavopulmonary shunt placement, and the Fontan procedure. Although the Fontan procedure significantly improves outcomes in these patients,1–4 it can cause various problems, including rhythm abnormalities such as sinus node dysfunction, atrioventricular (AV) block, and atrial tachyarrhythmia. These rhythm abnormalities can stem from several factors, such as congenital abnormalities of the conduction system,5 damage to the sinus node and conduction pathway after serial surgeries,6 and increased right atrial pressure.7 Depending on their symptoms, some patients with bradyarrhythmia may require permanent pacemaker (PPM) implantation.
Editorial p 649
PPM implantation is required in 8–38% of Fontan patients and is a risk factor for post-Fontan morbidity and mortality. In recent studies, a higher ventricular pacing ratio, non-apical pacing, and a higher QRS z-score were identified as possible risk factors for mortality and heart transplantation in these patients.8–13
In this study, we retrospectively analyzed Fontan patients who underwent PPM implantation at Asan Medical Center between September 1992 and August 2022. Our objective was to investigate the pacemaker-related factors associated with poor outcomes among patients with Fontan physiology who underwent PPM implantation.
We identified Fontan patients who underwent PPM implantation at Asan Medical Center between September 1992 and August 2022. The medical records were reviewed to extract data on sex; anatomical cardiac diagnosis; surgical procedure; surgical timing; pre- and post- Fontan hemodynamic data, including ventricular end-diastolic pressure, mean pulmonary arterial pressure (PAP), pulmonary vascular resistance index, AV valvar regurgitation, ventricular function and New York Heart Association (NYHA) functional class at follow-up; and electrocardiography (ECG) results, such as paced QRS duration. Systolic ventricular function was graded as preserved at a ventricular ejection fraction (EF) >50%, mild dysfunction at an EF of 40–49%, and moderate/severe dysfunction at an EF of <40%.14–17 Cardiac catheterization was not routinely performed after the Fontan operation and post-Fontan hemodynamic data were collected for only 14 of 32 patients. We further collected PPM-related data, including the primary indication for PPM implantation, age at implantation, timing of implantation, PPM type, and lower heart rate setting. The poor outcome variables included death, heart transplantation, or Fontan failure, including the requirement for heart transplantation, protein-losing enteropathy, plastic bronchitis, or NYHA Class III or IV at follow-up.2,18,19
To ensure accuracy, we reviewed the most recently available data for each patient; for those who died, underwent heart transplantation, or received cardiac resynchronization therapy (CRT), we selected data recorded immediately before the corresponding event.
Based on their outcomes, patients were classified into good (Group I) and poor (Group II) outcome groups. The poor outcome group comprised patients who died, required heart transplantation, or experienced “Fontan failure”; the good outcome group consisted of the remaining patients.
Statistical analyses were performed using SPSS Statistics for Windows version 27.0 (IBM Corp., Armonk, NY, USA) and R Studio version 4.2.3 (PBC, Boston, MA, USA). Data are presented as frequencies, the mean±SD, or as the median with interquartile range. Intergroup comparisons were performed using the Mann–Whitney U test and Fisher’s exact probability test. Two-sided P<0.05 was considered significant. A receiver operating characteristic (ROC) curve analysis was performed to assess diagnostic accuracy and identify the optimal cut-off value. A Kaplan-Meier analysis was performed to compare the incidence of poor outcomes between patients with and without a prolonged paced QRS duration. The date of PPM implantation was considered time zero.
All retrieved data were reviewed and analyzed. This study was approved by the Institutional Review Board of Asan Medical Center (No. 2022-1366), which waived the requirement for informed consent owing to the retrospective nature of the study.
Overall, 508 patients with a single-ventricle heart underwent the Fontan procedure during the study period. During the follow-up period (16.8±9.1 years), 37 (7.3%) patients underwent PPM implantation. Of these patients, 5 were excluded from the present study because of loss to follow-up (n=3) or because they primarily received CRT (n=2; Figure 1). The baseline characteristics, factors associated with the Fontan operations and PPM implantation, and ECG findings for the remaining 32 patients are listed in Table 1.

Study population. CRT, cardiac resynchronization therapy; PPM, permanent pacemaker.
Demographic Characteristics
| All patients (n=32) |
Group I: good outcome (n=21; 65.6%) |
Group II: poor outcome (n=11; 34.4%) |
P value | |
|---|---|---|---|---|
| Sex | 0.397 | |||
| Male | 24 (75.0) | 17 (53.1) | 7 (21.9) | |
| Female | 8 (25.0) | 4 (12.5) | 4 (12.5) | |
| Anatomical diagnosis | 0.667 | |||
| DILV | 7 (21.9) | 5 (15.6) | 2 (6.3) | |
| DORV | 7 (21.9) | 6 (18.8) | 1 (3.1) | |
| RAI | 1 | |||
| LAI | 3 | |||
| ccTGA | 4 (12.5) | 2 (6.3) | 2 (6.3) | |
| Ebstein anomaly | 3 (9.4) | 1 (3.1) | 2 (6.3) | |
| PA/IVS | 3 (9.4) | 2 (6.3) | 1 (3.1) | |
| d-TGA PA(PS) | 2 (6.3) | 1 (3.1) | 1 (3.1) | |
| TA | 2 (6.3) | 2 (6.3) | 0 (0) | |
| Criss-cross heart | 2 (6.3) | 1 (3.1) | 1 (3.1) | |
| AVSD | 1 (3.1) | 0 (0) | 1 (3.1) | |
| HLHS | 1 (3.1) | 1 (3.1) | 0 (0) | |
| Ventricular morphology | 0.301 | |||
| Dominant RV | 7 (21.9) | 6 (18.8) | 1 (3.1) | |
| Dominant LV | 16 (50.0) | 10 (31.3) | 6 (18.8) | |
| Intermediate | 9 (28.1) | 5 (15.6) | 4 (12.5) | |
| Age at Fontan procedure (months) | 0.022 | |||
| Mean±SD | 48.7±20.7 | 42.7±11.3 | 60.0±29.2 | |
| Median [IQR] | 42.5 [37–56] | 41.0 [36.5–51.5] | 42.5 [42–70] | |
| Type of Fontan procedure | 0.122 | |||
| EC | 24 (75.0) | 14 (43.8) | 10 (31.3) | |
| LT | 4 (12.5) | 3 (9.4) | 1 (3.1) | |
| AP connection | 4 (12.5) | 4 (12.5) | 0 (0) | |
| Fenestration | 7 (21.9) | 4 (12.5) | 3 (9.4) | 0.667 |
| Fontan conversion | 7 (21.9) | 6 (18.8) | 1 (3.1) | 0.374 |
| Maze operation | 0.223 | |||
| Before PPM insertion | 5 (15.6) | 3 (9.4) | 2 (6.3) | |
| After PPM insertion | 5 (15.6) | 2 (6.3) | 3 (9.4) | |
| Pre-Fontan hemodynamics | ||||
| Mean PAP (mmHg; n=27) | 12.0±3.9 | 10.6±3.6 | 14.3±3.6 | 0.015 |
| VEDP (mmHg; n=27) | 6.6±3.6 | 5.9±3.4 | 7.9±3.7 | 0.173 |
| PVR index (Wood units·m2; n=16) | 1.31±0.7 | 1.1±0.4 | 1.6±0.9 | 0.261 |
| Moderate to severe AVVR | 2 | 1 | 1 | 1.00 |
| Ventricular function | 0.178 | |||
| Preserved | 28 (87.5) | 19 (59.4) | 9 (28.1) | |
| Mild dysfunction | 2 (6.3) | 2 (6.3) | 0 (0) | |
| Moderate/severe dysfunction | 2 (6.3) | 0 (0) | 2 (6.3) | |
| Post-Fontan hemodynamics | ||||
| Mean PAP (mmHg; n=15) | 13.9±3.4 | 12.6±2.3 | 16.4±4.2 | 0.113 |
| VEDP (mmHg; n=14) | 9.1±2.4 | 8.6±2.7 | 10.2±1.6 | 0.236 |
| PVR index (Wood units·m2; n=9) | 1.8±1.1 | 1.6±0.8 | 2.3±1.6 | 0.391 |
| Moderate to severe AVVR | 1 | 0 (0) | 1 (3.1) | 0.344 |
| Ventricular function | 0.004 | |||
| Preserved | 22 (68.8) | 18 (56.3) | 4 (12.5) | |
| Mild dysfunction | 5 (15.6) | 2 (6.3) | 3 (9.4) | |
| Moderate/severe dysfunction | 5 (15.6) | 1 (3.1) | 4 (12.5) | |
| Primary indication for PPM | 0.324 | |||
| Congenital AV block | 6 (18.8) | 4 (12.5) | 2 (6.3) | |
| Postoperative AV block | 14 (43.8) | 7 (21.9) | 7 (21.9) | |
| Sinus node dysfunction | 12 (37.5) | 10 (31.3) | 2 (6.3) | |
| Time from first arrhythmia to PPM implantation (days) | 472.3±630.8 | 437.5±629.3 | 538.6±658.7 | 0.674 |
Unless indicated otherwise, data are given as the mean±SD, n (%), or n. AP, atriopulmonary; AVSD, atrioventricular septal defect; AVVR, atrioventricular valve regurgitation; ccTGA, congenitally corrected transposition of the great arteries; DILV, double inlet left ventricle; DORV, double outlet right ventricle; d-TGA, D-transposition of the great arteries; EC, extracardiac conduit; HLHS, hypoplastic left heart syndrome; IQR, interquartile range; LAI, left atrial isomerism; LT, lateral tunnel; LV, left ventricle; PA/IVS, pulmonary atresia with intact ventricular septum; PAP, pulmonary artery pressure; PPM, permanent pacemaker; PVR, pulmonary vascular resistance; RAI, right atrial isomerism; RV, right ventricle; TA, tricuspid atresia; VEDP, ventricular end-diastolic pressure.
Twenty-four of the 32 patients were male (75%). The most common anatomical diagnoses were double inlet left ventricle (n=7) and double outlet right ventricle (n=7). Most patients underwent the Fontan operation with an extracardiac conduit (EC; 24/32 [75%]); however, an intra-atrial lateral tunnel was used in 4 patients, and an atriopulmonary connection was used in the remaining 4 patients. Seven of these 8 patients underwent a reoperation for conversion to EC. The median age at the Fontan operation was 42.5 months. Arrhythmia surgery was performed in 10 patients: before PPM implantation in 5 and after PPM implantation in 5. The most common indications for PPM implantation were high-degree or complete postoperative AV block (14/32 [43.8%]), sinus node dysfunction (12/32 [37.5%]), and congenital AV block (6/32 [18.8%]).
Fontan Failure and Death or Requirement for Heart TransplantationAmong the 32 patients with PPM, 11 (34.4%) exhibited a poor outcome (Group II). Among these patients, 6 (16.2%) died, 1 (2.7%) required heart transplantation, and 4 (12.5%) experienced Fontan failure (Supplementary Table 1). Of the 6 patients who died, the deaths of 2 were confirmed through the insurance system; however, the cause of death was unknown owing to a loss to follow-up. Another 2 patients died in the immediate postoperative period, and the remaining 2 patients died of multiorgan failure. The detailed causes of death are presented in Supplementary Table 2.
PPM-Related CharacteristicsThe PPM-related characteristics are summarized in Table 2. All PPM systems were epicardial. The mean age at PPM implantation was 7.4±7.5 years. The most common timing for PPM implantation was after the Fontan operation (15/32 [46.9%]). The mean interval from the first arrhythmia episode to PPM insertion was 15.1±20.7 months. The mean time that elapsed after the first PPM implantation was 108.1±67.4 months. The most commonly used PPM type was dual-chamber (22/32 [68.8%]), followed by single-chamber ventricular pacing (8/32 [25%]) and single-chamber atrial pacing (2/32 [6.3%]). Twenty-one patients received high ventricular pacing for >50% of the time. The ventricular lead was located apically in 10 (31.3%) patients and non-apically and 20 (62.5%). The mean PPM lower rate setting was 65.6±10.7 beats/min, whereas the mean paced QRS duration was 136.4±34.1 ms.
Pacemaker-Related Characteristics
| All patients (n=32) |
Group I: good outcome (n=21; 65.6%) |
Group II: poor outcome (n=11; 34.4%) |
P value | |
|---|---|---|---|---|
| Age at PPM implantation (years) | 0.224 | |||
| Mean±SD | 7.4±7.5 | 8.5±8.2 | 5.4±5.8 | |
| Median [IQR] | 4.5 [0–11.75] | 9.0 [0–17] | 4.0 [2–7] | |
| Timing of PPM implantation | 1.000 | |||
| Before first palliation operation | 1 (3.1) | 1 (3.1) | 0 (0) | |
| After first palliation operation | 7 (21.9) | 6 (18.8) | 1 (3.1) | |
| After BCPS | 9 (28.1) | 3 (9.4) | 6 (18.8) | |
| After Fontan procedure | 15 (46.9) | 11 (34.4) | 4 (12.5) | |
| Time from the first arrhythmia to PPM implantation (months) | 15.1±20.7 | 14.0±20.7 | 17.2±21.5 | 0.686 |
| PPM duration (months) | 108.1±67.4 | 123.4±71.6 | 79.0±48.9 | 0.076 |
| PPM mode | 1.000 | |||
| DDD | 22 (68.8) | 15 (46.9) | 7 (21.9) | |
| VVI | 8 (25.0) | 4 (12.5) | 4 (12.5) | |
| AAI | 2 (6.3) | 2 (6.3) | 0 (0) | |
| Ventricular lead position (n=30) | 0.246 | |||
| Apical | 10 (31.3) | 8 (25.0) | 2 (6.3) | |
| Non-apical | 20 (62.5) | 11 (34.4) | 9 (28.1) | |
| Paced QRS duration (ms) | 136.4±34.1 | 127.7±28.8 | 153.1±38.6 | 0.044 |
| Ventricular pacing >50% | 21 (65.6) | 12 (37.5) | 9 (28.1) | 0.248 |
| PPM lower rate setting (beats/min) | 65.6±10.7 | 63.0±9.1 | 69.1±12.2 | 0.125 |
Unless indicated otherwise, data are given as the mean±SD, n (%), or n. BCPS, bidirectional cavopulmonary shunt; ECG, electrocardiography; IQR, interquartile range; LBBB, left bundle branch block; PPM, permanent pacemaker; RBBB, right bundle branch block.
Predictors of Adverse Outcomes
Among the demographic variables, intergroup differences were observed in age at Fontan operation, pre-Fontan mean PAP, and the presence of ventricular dysfunction after Fontan operation. The mean age at the Fontan operation was older in Group II than in Group I (P=0.022). The pre-Fontan mean PAP was higher in Group II than in Group I (P=0.015). Ventricular dysfunction was more common in Group II (P=0.004).
Among pacemaker-related variables, no intergroup differences were observed in PPM mode, ventricular lead position, or percentage of ventricular pacing. The only significantly different factor was mean paced QRS duration, which was wider in Group II than in Group I (153.1±38.6 vs. 127.7±28.8 ms, respectively; P=0.044).
Outcomes According to Paced QRS DurationAn ROC curve analysis was performed to determine whether paced QRS duration could predict a poor outcome. The area under the ROC curve was 0.73 (P=0.035). The optimal cut-off value was 153 ms, with a sensitivity and specificity of 63.6% and 85.7%, respectively. When divided into 2 groups based on paced QRS duration (≥153 and <153 ms), patients with a paced QRS duration of ≥153 ms tended to have worse Fontan failure-free survival, although the difference was not statistically significant (Figure 2A; P=0.074). Moreover, mortality and transplant-free survival rates were worse in the group with a paced QRS duration of ≥153 ms (Figure 2B; P=0.012).
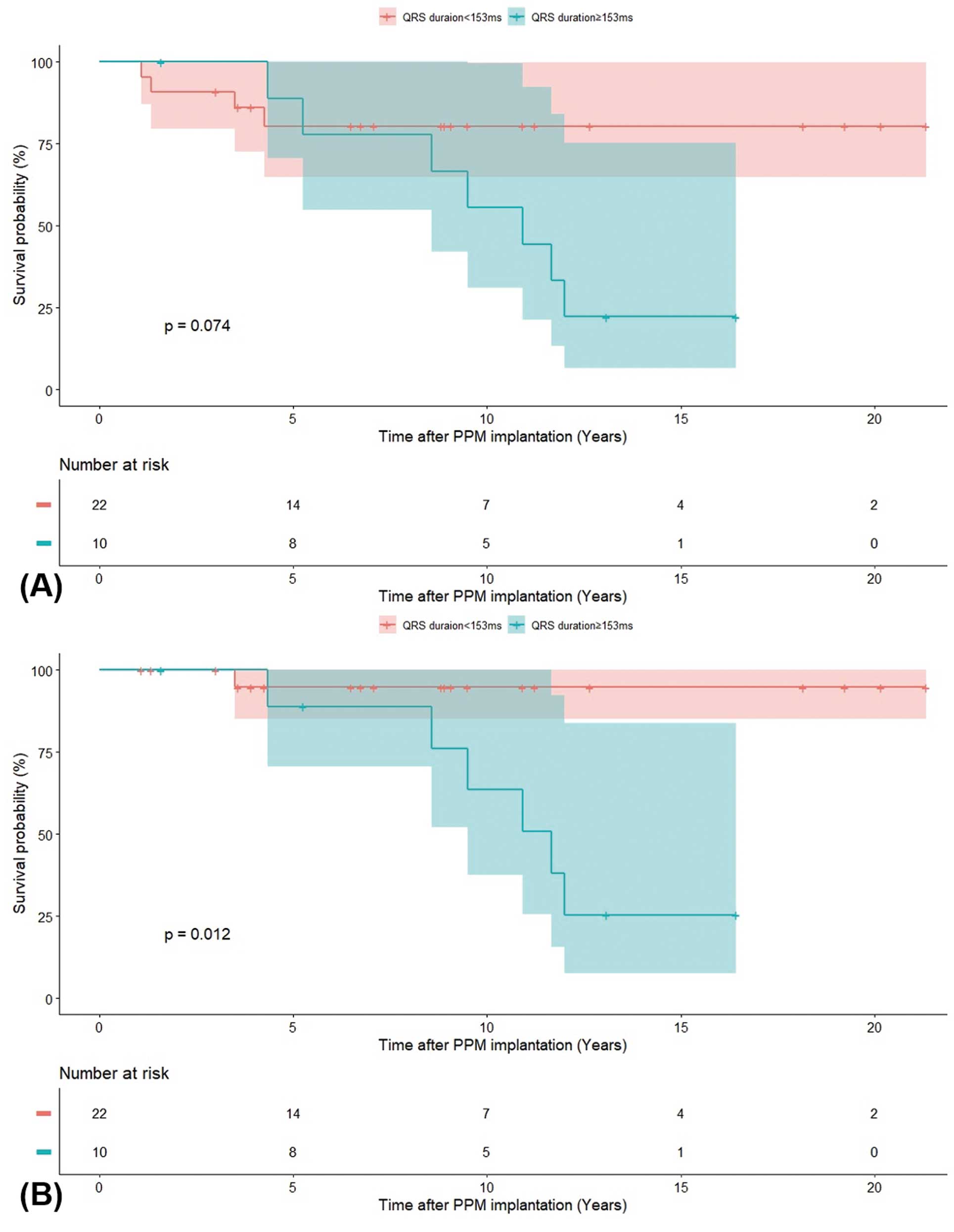
Kaplan-Meier survival curves according to paced QRS duration (≥153 and <153 ms). (A) Fontan failure-free survival and (B) death/transplant-free survival. PPM, permanent pacemaker.
The present retrospective study analyzed the outcomes of Fontan patients who underwent PPM implantation; 34.4% of these patients experienced Fontan failure during follow-up. In our study, older age at Fontan completion, an elevated mean PAP, and ventricular dysfunction (established risk factors associated with a poor outcome) differed significantly between the 2 outcome groups. Factors such as anatomical cardiac diagnosis and surgical procedure type did not differ significantly between the 2 groups. Among the PPM-associated factors, only paced QRS duration differed significantly, with a longer paced QRS duration in the poor outcome group (Group II).
Previous studies identified certain PPM-associated risk factors in the Fontan population. A multicenter study of 236 patients with a single-ventricle heart and PPM and their matched controls without PPM found that a higher ventricular pacing ratio, higher QRS z-score, and non-apical lead position were associated with an increased risk of mortality and requirement for transplantation.13 Consistent with these findings, we also observed a longer mean paced QRS duration in the poor outcome group. It is unclear whether this longer paced QRS complex in the poor outcome group is solely attributable to ventricular dysfunction secondary to pacemaker-associated ventricular dyssynchrony or whether it is indicative of underlying ventricular dysfunction and remodeling resulting from other factors. Nevertheless, when Fontan patients with PPM have a prolonged paced QRS duration, further investigations and management (e.g., PPM modification or heart failure management) may be necessary.
Theoretically, multisite pacing may be more beneficial for the prevention and management of heart failure caused by ventricular dyssynchrony. Although the effectiveness of CRT in patients with a single ventricle remains debatable,20,21 Fontan patients treated with a conventional PPM and with a prolonged paced QRS duration may be candidates for CRT.
We identified a cut-off value of 153 ms as indicative of a prolonged paced QRS duration in Fontan patients. This value is closely aligned with the recommended criterion for CRT in individuals with a structurally normal heart. CRT is recommended for patients with ventricular dysfunction and a QRS duration of ≥150 ms.22 However, owing to the limited size of our cohort, future studies with larger sample sizes must validate our findings and establish a more definitive threshold for defining a long paced QRS duration in the single-ventricle patient population.
In addition, although not statistically significant, the Fontan failure-free survival rate according to paced QRS duration tended to be worse in the longer-paced QRS group (poor outcome group). This result was more pronounced for mortality and transplant-free survival (Figure 2). Previous studies of patients with heart failure and normally structured hearts observed an increasing divergence in outcomes over time between patients with a longer vs. shorter QRS duration.23,24 This suggests the presence of a cumulative effect over time.
Finally, we investigated a relationship between high ventricular pacing and adverse outcomes. Several previous studies suggested that high ventricular pacing is an adverse risk factor for long-term survival and ventricular function. In a study of a Fontan population using data from the Australia and New Zealand Fontan Registry, 126 patients underwent PPM implantation, and a higher risk of mortality or transplantation in the PPM group was confirmed using propensity score matching. Furthermore, ventricular pacing >50% of the time was associated with a high risk of late mortality or requirement for transplantation.8 Kodama et al reported that higher proportions of ventricular and non-apical pacing were associated with poor outcomes.25 Similarly, a study of patients with a single ventricle who required chronic ventricular pacing found moderate to severe ventricular dysfunction and AV valve regurgitation on echocardiography, along with an increased risk of mortality and transplantation compared with the control group.26
In our study, the mean ventricular pacing ratio did not differ significantly between the outcome groups. The small size of our cohort may have limited the ability of our analysis to achieve statistical significance. In addition, it is possible that other dominant factors contributing to the increased risk of adverse events in Fontan patients may have influenced this observation. Moreover, modifying risk factors, such as achieving a shorter paced QRS duration through optimal lead positioning, could potentially reduce the impact of high ventricular pacing on adverse outcomes.
Study LimitationsOur study has some limitations. First, it had a retrospective single-center design and a small sample size. Second, it included patients with different observation periods, which made determining risk factors using survival analysis challenging. Furthermore, the study was difficult to standardize owing to heterogeneity in the patients’ ages, cardiac anatomy, and Fontan surgery-related factors. Extracardiac status may also be a risk factor, but its impact did not seem significant. Two patients had epilepsy due to hypoxic-ischemic encephalopathy, and 3 patients had liver cirrhosis. However, none of the patients experienced renal failure.
In this single-center cohort of Fontan patients with PPM, a prolonged paced QRS duration, along with other known risk factors, was associated with poor outcomes, including death, requirement for heart transplantation, and Fontan failure. These findings suggest that when Fontan patients with PPM exhibit a prolonged paced QRS duration, hemodynamic evaluations and interventions (e.g., medication or PPM modification) may be necessary.
None.
This research received no external funding.
The authors declare that there are no conflicts of interest.
This study was approved by the Institutional Review Board of Asan Medical Center (No. 2022-1366), which waived the requirement for informed consent.
The deidentified participant data will be shared on a request basis. Please contact the corresponding author directly to request data sharing.
Please find supplementary file(s);
https://doi.org/10.1253/circj.CJ-23-0491