2024 Volume 88 Issue 9 Pages 1472-1477
2024 Volume 88 Issue 9 Pages 1472-1477
Background: The incidence and prognostic predictors of heart failure (HF) without left ventricular systolic dysfunction (LVSD) in hypertrophic cardiomyopathy (HCM), particularly their differences in terms of developing LVSD (progression to end-stage) or sudden cardiac death (SCD), are not fully elucidated.
Methods and Results: This study included 330 consecutive HCM patients with left ventricular ejection fraction (LVEF) ≥50%. HF hospitalization without LVSD and development of LVSD were evaluated as main outcomes. During a median follow-up of 7.3 years, the incidence of HF hospitalization without LVSD was 18.8%, which was higher than the incidence of developing LVSD (10.9%) or SCD (8.8%). Among patients who developed LVSD, only 19.4% experienced HF hospitalization without LVSD before developing LVSD. Multivariable analysis showed that predictors for HF hospitalization without LVSD (higher age, atrial fibrillation, history of HF hospitalization, and higher B-type natriuretic peptide concentrations) were different from those of developing LVSD (male sex, lower LVEF, lower left ventricular outflow tract gradient, and higher tricuspid regurgitation pressure gradient). Known risk factors for SCD did not predict either HF without LVSD or developing LVSD.
Conclusions: In HCM with LVEF ≥50%, HF hospitalization without LVSD was more frequently observed than development of LVSD or SCD during mid-term follow-up. The overlap between HF without LVSD and developing LVSD was small (19.4%), and these 2 HF events had different predictors.
Although the development of left ventricular systolic dysfunction (LVSD) in hypertrophic cardiomyopathy (HCM), known as end-stage HCM or formerly the “dilated phase”, has been reported to occur in 5–10% of patients during disease progression of HCM.1–8 Heart failure (HF) events without LVSD (i.e., preserved ejection fraction [EF]) in HCM was underrecognized,9,10 but is now recognized as one of the phenotypes of HF with preserved EF (HFpEF).11–14
However, the incidence and predictors of HF hospitalization without LVSD, particularly their difference from those of developing LVSD (progression to end-stage) or sudden cardiac death (SCD), as well as the extent of their overlap, are not fully understood. The aim of this study was to investigate the incidence, predictors, and overlap of HF hospitalization without LVSD compared with developing LVSD (progression to end-stage) and SCD, in HCM with preserved EF.
Of 450 consecutive HCM patients aged over 16 years evaluated at the National Cerebral and Cardiovascular Center, a tertiary referral center, between January 1, 2009 and December 31, 2013, 330 patients with left ventricular (LV) EF ≥50% were studied. The characteristics of the cohort have been published previously.15 Consecutive patients who were hospitalized for thorough diagnostic and risk evaluation of newly diagnosed HCM, as per our standard practice, or those previously diagnosed with HCM who were hospitalized during the specified period were enrolled in this cohort. A diagnosis of HCM was made using the standard definition based on identification by 2-dimensional echocardiography or cardiovascular magnetic resonance imaging (CMR) of a hypertrophied non-dilated LV, in the absence of another cardiac or systemic disease capable of producing the magnitude of hypertrophy evident.16–18 Patients with HCM linked to Noonan syndrome, Fabry disease, mitochondrial disease, or congenital heart defects were not included. Variables at the time of enrollment were used as baseline patient characteristics.
Left ventricular outflow tract (LVOT) obstruction was defined as estimated peak instantaneous pressure gradient ≥30 mmHg caused by systolic anterior motion of the anterior mitral leaflet.19–21 The risk of SCD was calculated using the European Society of Cardiology 2014 Risk-SCD model.22
This study complies with the Declaration of Helsinki and was approved by the Institutional Review Board of the National Cerebral and Cardiovascular Center (R19017).
OutcomesAs the main outcomes for this study, we evaluated: (1) HF hospitalization without LVSD (LVEF ≥50% at hospitalization); and (2) the development of LVSD, defined as documentation of LVEF <50% by echocardiography during follow-up. HF hospitalization was defined as unplanned hospitalization due to worsening HF symptoms and physical findings requiring hospitalization, diagnosed based on the Framingham criteria by an experienced cardiologist. Also evaluated were other clinical events, including HF hospitalization after development of LVSD, all-cause death, cardiovascular death, SCD equivalent event, and heart transplantation or implantation of an LV assist device. An SCD equivalent event was defined as instant and unexpected death occurring within the first hour of the onset of symptoms or an equivalent event (appropriate implantable cardioverter defibrillator therapy or successful resuscitation after cardiac arrest). Events were collected by reviewing electronic medical records, and the collection of follow-up data was completed on May 31, 2021.
Statistical AnalysisNormally distributed variables are presented as the mean±SD; non-normally distributed variables are presented as the median with interquartile range (IQR). The Shapiro-Wilk test was used to assess whether data were normally distributed. All tests were 2-sided, and P<0.05 was considered statistically significant.
Cox proportional hazard analysis was performed to evaluate the influence of baseline variables on events. Variables for univariable and multivariable analysis were selected based on clinical relevance and established prognostic risk factors for HF. Stepwise selection with P<0.2 for forward selection was used to select the best predictive model. Multicollinearity among the variables in the model was assessed by calculation of the variance inflation factor. No variable in the model had an associated variance inflation factor greater than 10.0, demonstrating that there were no significant multicollinearities. CMR variables were available for a limited subgroup of patients, and so were considered only in the univariable analysis.
All statistical analyses were performed using JMP 12 (SAS Institute, Inc., Cary, NC, USA) and SPSS version 22 (SPSS Inc., Chicago, IL, USA).
For the 330 patients studied, the median age was 67 years (IQR 56–74 years), 175 (53%) were male, and 123 (37%) had LVOT obstruction (Table 1). The median ESC 2014 Risk-SCD score was 1.85%/5 years (IQR 1.05–3.48%/5 years). On echocardiography, median interventricular septal thickness was 14 mm (IQR 11–17 mm) and the mean LVEF was 60.5±4.5% (Table 2). In a subgroup of 149 patients for whom CMR variables were available, the median LVEF by CMR was 56% (IQR 52–61%). Results for other variables are presented in Tables 1 and 2.
Patient Characteristics (n=330)
| Age (years) | 67 [56–74] |
| Male sex | 175 (53) |
| Body mass index (kg/m2) | 23.6 [21.1–26.0] |
| LVOT obstruction/non-LVOT obstruction | 123 (37)/207 (63) |
| History of sustained VT/VF | 44 (13) |
| Non-sustained VT | 111 (34) |
| Family history of SCD | 42 (13) |
| Family history of HCM | 46 (14) |
| Unexplained syncope | 67 (20) |
| Risk-SCD score (%/5 years) | 1.85 [1.05–3.48] |
| LV apical aneurysm | 19 (6) |
| Atrial fibrillation | |
| None | 195 (59) |
| Paroxysmal | 83 (25) |
| Persistent/chronic | 52 (16) |
| History of HF hospitalization | 75 (23) |
| NYHA functional class | |
| I | 93 (29) |
| II | 190 (57) |
| III | 36 (11) |
| IV | 11 (3) |
| Systolic blood pressure (mmHg) | 120 [108–133] |
| Diastolic blood pressure (mmHg) | 67 [60–75] |
| Heart rate (beats/min) | 64 [57–72] |
| Medications | |
| β-blocker | 235 (71) |
| ACEi/ARB | 106 (32) |
| Diuretic | 82 (25) |
| Class I anti-arrhythmic drugs | 89 (27) |
| Class III anti-arrhythmic drugs | 55 (17) |
| Laboratory data | |
| BNP (pg/mL) | 212 [82–432] |
| eGFR (mL/min/1.73 m2) | 61 [52–71] |
| Creatinine (mg/dL) | 0.86 [0.72–1.02] |
| Blood urea nitrogen (mg/dL) | 15 [13–19] |
| Sodium (mEq/L) | 141 [139–142] |
| Albumin (g/dL) | 4.1 [3.9–4.3] |
| Total bilirubin (mg/d ) | 0.6 [0.5–0.8] |
| Hemoglobin (g/dL) | 13.1±1.7 |
Data are presented as n (%), median [interquartile range], or mean±SD. ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; BNP, B-type natriuretic peptide; eGFR, estimated glomerular filtration rate; HCM, hypertrophic cardiomyopathy; HF, heart failure; LV, left ventricle; LVOT, left ventricular outflow tract; NYHA, New York Heart Association; SCD, sudden cardiac death; VF, ventricular fibrillation; VT, ventricular tachycardia.
Echocardiography and Cardiac Magnetic Resonance Imaging Results
| Echocardiography (n=330) | |
| LV end-diastolic dimension (mm) | 44 [40–48] |
| LV end-systolic dimension (mm) | 27 [23–30] |
| LVEF (%) | 60.5±4.5 |
| Interventricular septal thickness (mm) | 14 [11–17] |
| Posterior wall thickness (mm) | 11 [9–12] |
| Maximum LV wall thickness (mm) | 15 [13–19] |
| Peak LVOT gradient (mmHg) | 8 [0–41] |
| LA dimension (mm) | 45 [41–49] |
| LA volume index (mL/m2) | 56 [41–73] |
| MR moderate/severe | 26 (8) |
| TR pressure gradient (mmHg) | 25 [21–31] |
| e′ (septal; cm/s) | 4.5 [3.3–5.6] |
| E/e′ (septal) | 15.8 [11.4–21.9] |
| Cardiac magnetic resonance imaging (n=149) | |
| LV ejection fraction (%) | 56 [52–61] |
| LV end-diastolic volume (mL) | 136 [106–165] |
| LV end-systolic volume (mL) | 59 [46–75] |
| LV mass (g) | 129 [104–169] |
| RV ejection fraction (%) | 49 [45–54] |
| RV end-systolic volume (mL) | 106 [88–132] |
| RV end-systolic volume (mL) | 56 [42–69] |
Data are presented as n (%), median [interquartile range], or mean±SD. LA, left atrium; LVEF, left ventricular ejection fraction; MR, mitral regurgitation; RV, right ventricle; TR, tricuspid regurgitation. Other abbreviations as in Table 1.
Incidence of Events and Overlap Between the 2 HF Events
During a median follow up of 7.3 years (IQR 3.9–9.3 years), HF hospitalization without LVSD was observed in 62 (18.8%) patients, and this rate was higher than that of developing LVSD (36 [10.9%]) or SCD in (29 [8.8%]; Table 3; Figure A). Kaplan-Meier curves for each clinical event are shown in the Supplementary Figure. HF hospitalization without LVSD was due to LV diastolic dysfunction (55%), LVOT obstruction (23%), and mitral regurgitation (3%; Supplementary Table 1).
Events During Follow-up (n=330)
| HF events | |
| HF hospitalization without LVSD (LVEF ≥50% at hospitalization) | 62 (18.8) |
| Development of LVSD (progression to LVEF <50%) | 36 (10.9) |
| HF hospitalization after development of LVSD (LVEF <50%) | 19 (5.8) |
| Other events | |
| All-cause death | 39 (11.8) |
| Cardiovascular death | 20 (6.1) |
| Sudden cardiac death (or equivalent) | 29 (8.8) |
| Heart transplantation or LVAD implantation | 2 (0.6) |
Data are presented as n (%). HF, heart failure; LVAD, left ventricular assist device; LVEF, left ventricular ejection fraction; LVSD, left ventricular systolic dysfunction.
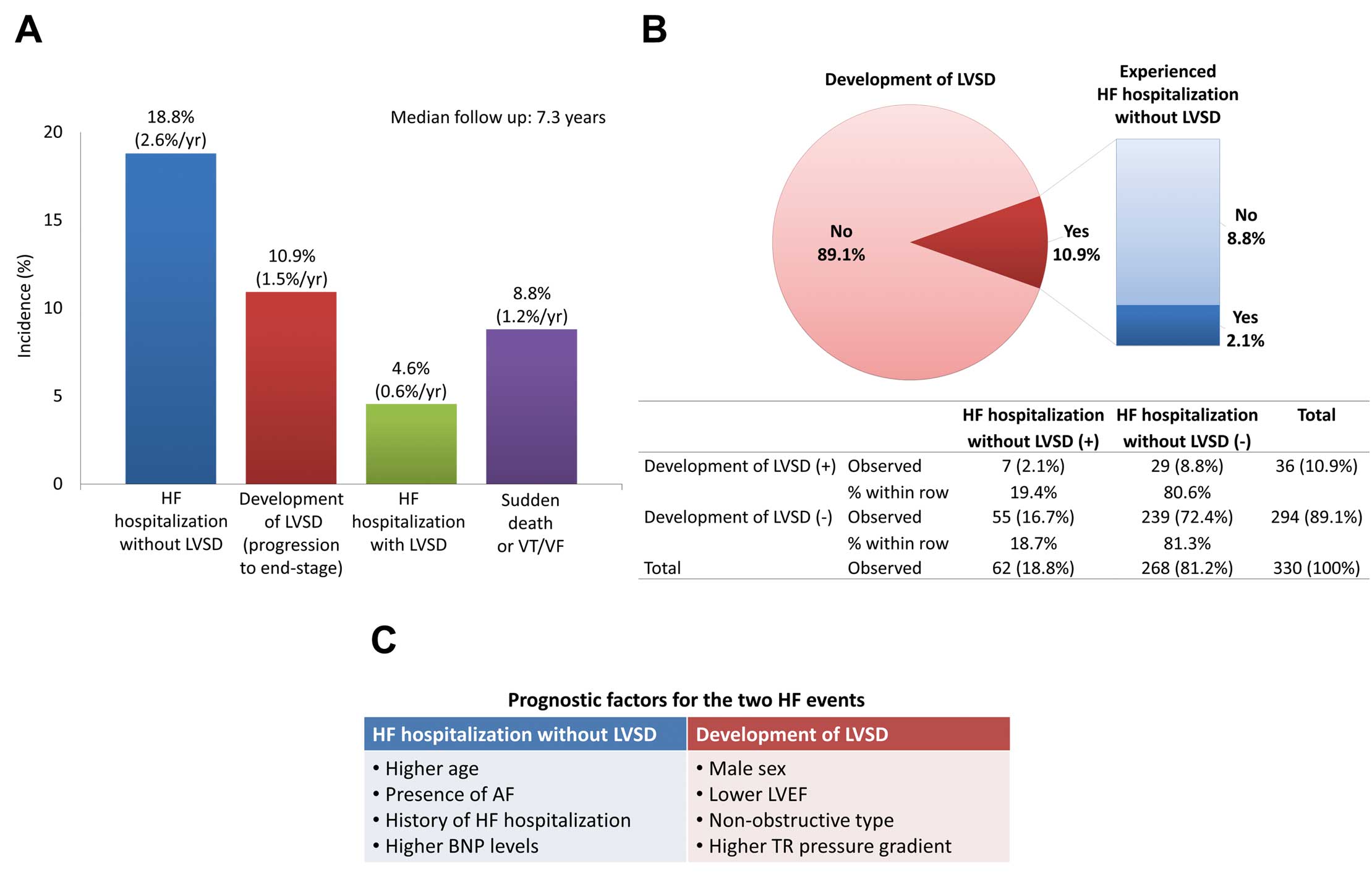
Summary of the study results. (A) Incidence of clinical events. Heart failure (HF) hospitalization without left ventricular systolic dysfunction (LVSD) was observed in 18.8% of patients, with this rate being higher than the development of LVSD (10.9%) and sudden cardiac death (8.8%). VF, ventricular fibrillation; VT, ventricular tachycardia; yr, year. (B) Overlap between the development of LVSD and HF without LVSD. Of the 10.9% of patients who developed LVSD, only one-fifth (2.1% of 10.9%) experienced HF hospitalization without LVSD before developing LVSD. (C) Differences in the prognostic factors associated with the 2 HF events. The factors were associated with HF hospitalization without LVSD and the development of LVSD (progression to end-stage) were different. AF, atrial fibrillation; BNP, B-type natriuretic peptide; LVEF, left ventricular ejection fraction; TR, tricuspid regurgitation.
Importantly, of the 36 patients who developed LVSD, only 7 (19.4%) experienced HF hospitalization without LVSD before developing LVSD (Figure B).
Comparison of Factors Associated With the 2 HF EventsPrognostic predictors of HF hospitalization without LVSD and the development of LVSD were compared using Cox proportional hazard analysis. Significant predictors by univariable analysis for HF hospitalization without LVSD were higher age, lower body mass index, the presence of atrial fibrillation (AF), a history of HF hospitalization, a higher New York Heart Association (NYHA) functional class, higher B-type natriuretic peptide (BNP) concentration, lower estimated glomerular filtration rate, larger left atrial (LA) volume index, higher tricuspid regurgitation (TR) pressure gradient, and higher E/e′. Predictors for the development of LVSD were male sex, non-LVOT obstruction, the presence of apical aneurysm, a larger LV dimension, lower LVEF, lower LVOT gradient, larger LA, and higher TR pressure gradient (Supplementary Table 2). In a subgroup of patients for whom CMR variables were available, reduced LVEF and right ventricular EF and larger LV and right ventricular volumes were predictors of the development of LVSD, but none of the variables was a significant predictor for HF hospitalization without LVSD (Supplementary Table 2).
Of note, risk factors currently considered for primary prevention of SCD in HCM, including the ESC 2014 Risk-SCD score, non-sustained ventricular tachycardia, a family history of SCD, and unexplained syncope, did not predict either HF hospitalization without LVSD or the development of LVSD.
Multivariable analyses showed that significant predictors for HF hospitalization without LVSD were higher age, the presence of AF, a history of HF hospitalization, and higher BNP levels. The predictors for developing LVSD were different: male sex, lower LVEF, lower LVOT gradient, and higher TR pressure gradient (Table 4; Figure C).
Multivariable Analysis of the 2 HF Events
| HR (95% CI) | P value | |
|---|---|---|
| HF hospitalization without LVSD | ||
| Age, per 1-year increase | 1.035 (1.013–1.059) | 0.001 |
| Atrial fibrillation | 1.987 (1.176–3.439) | 0.012 |
| History of HF hospitalization | 2.475 (1.456–4.158) | 0.001 |
| Log BNP, per 1 increase | 1.611 (1.220–2.156) | 0.001 |
| Development of LVSD | ||
| Male sex | 6.463 (1.555–46.59) | 0.008 |
| LVEF, per 1% increase | 0.842 (0.737–0.957) | 0.009 |
| Peak LVOT gradient, per 1-mmHg increase | 0.948 (0.865–0.993) | 0.012 |
| TR pressure gradient, per 1-mmHg increase | 1.073 (1.003–1.155) | 0.041 |
CI, confidence interval; HR, hazard ratio. Other abbreviations as in Tables 1–3.
We report 4 main findings of the present analysis of HCM with LVEF ≥50% at a tertiary referral center with a median follow up of 7.3 years, as detailed below.
• The incidence of HF hospitalization without LVSD was 18.8% and was higher than the incidence of developing LVSD (10.9%) or SCD (8.8%).
• Among patients who developed LVSD, only 19.4% experienced HF hospitalization without LVSD before developing LVSD, demonstrating the small overlap between these 2 HF events.
• Predictors for HF hospitalization without LVSD (higher age, the presence of AF, a history of HF hospitalization, and higher BNP concentrations) were different from the predictors for the development of LVSD (male sex, lower LVEF, lower LVOT gradient [non-LVOT obstruction], and higher TR pressure gradient).
• The risk factors currently used for the primary prevention of SCD in HCM did not predict either HF hospitalization without LVSD or the development of LVSD.
Our findings demonstrate that there are multiple clinical pictures of HF in the disease course of HCM with different predictors and a small overlap, as well as different risk factors from SCD. Our study is the first study to evaluate prognostic predictors specifically for HF hospitalization without LVSD (i.e., considering LVEF at hospitalization as part of the outcome) and to compare 2 different HF outcomes (HF hospitalization without LVSD and the development of LVSD) simultaneously in a single cohort. Several previous studies have reported predictors of HF hospitalization in HCM; however, no study has focused on LVEF at hospitalization, or other studies considered HF hospitalization as a part of a composite endpoint.23–30 Some studies have reported progression of NYHA functional class as an outcome,3,27,31–33 but we used HF hospitalization, which is more objective than changes in NYHA functional class.
Revisiting HF Events in the Disease Progression of HCMOur results show that the incidence of HF hospitalization without LVSD was 2.6%/year and was higher than that of developing LVSD (1.5%/year) or SCD (1.2%/year). The incidence and predictors of HF events without LVSD in HCM patients have not been fully elucidated, but our results show that HF events without LVSD are frequently observed in the disease course of HCM.
Of the patients who developed LVSD, only 19.4% experienced HF hospitalization without LVSD before developing LVSD, demonstrating the small overlap between these 2 HF events. Another novel finding of our study is that the predictors of HF hospitalization without LVSD differ from those of developing LVSD. These findings support the notion that there are multiple clinical pictures of HF in the disease course of HCM. It is also worth mentioning that risk factors currently used for primary prevention of SCD in HCM did not predict either of the HF events (HF hospitalization without LVSD or the development of LVSD). Although risk factors for SCD in HCM have been studied for decades, including the development of a risk prediction calculator,22 risk prediction models for HF events in HCM have not been developed.
Our results suggest that it may be beneficial to consider HF hospitalization without LVSD and the development of LVSD as distinct endpoints, rather than combining them into a single clinical endpoint, in future studies evaluating HF outcomes in HCM.
HF without LVSD in HCM is now recognized as one of the phenotypes of HFpEF.11–14 New promising medical treatments for HFpEF and HCM, including sodium-glucose cotransporter 2 inhibitors34–37 and mavacamten,38–40 have recently been introduced and future studies are warranted to evaluate the effectiveness of these novel treatments on HF events in HCM with preserved EF.
Study LimitationsThis study has some limitations. First, the study was a single-center retrospective study conducted at a national referral center. Thus, our cohort may be biased towards patients with advanced and severe cases of HCM. Second, the relatively limited number of events may have limited the statistical power of our analysis. Third, results from CMR were available only for a limited subgroup of patients, thus precluding their consideration in multivariable analysis. Fourth, genetic analysis was only available for a limited number of patients and was not included in our assessment. Therefore, the results of the present study require further evaluation in a larger prospective study.
In HCM with LVEF ≥50%, the incidence of HF hospitalization without LVSD was higher than that of developing LVSD or SCD. Among patients who developed LVSD, only 19.4% experienced HF hospitalization without LVSD before developing LVSD, demonstrating the small overlap between the 2 HF events. Prognostic predictors of HF hospitalization without LVSD were different from the predictors of developing LVSD. These findings support multiple clinical pictures of HF in the disease progression of HCM.
None.
T.N. and C.I. are members of Circulation Journal’s Editorial Team. The remaining authors have no conflicts of interest to declare.
This study was approved by the Institutional Review Board of the National Cerebral and Cardiovascular Center (R19017).
Please find supplementary file(s);
https://doi.org/10.1253/circj.CJ-24-0049