The authors apologize for this correction in the original manuscript. Corrections are shown below.
1) Page 1661, abstract
Incorrect:
Methods and Results: In the OPTIVUS-Complex PCI study multivessel cohort enrolling 982 patients undergoing multivessel PCI, including left anterior descending coronary artery using intravascular ultrasound (IVUS), we conducted 90-day landmark analyses to compare shorter and longer DAPT. DAPT discontinuation was defined as withdrawal of P2Y12
inhibitors or aspirin for at least 2 months. The prevalence of acute coronary syndrome and high bleeding risk by the Bleeding Academic Research Consortium were 14.2% and 52.5%, respectively. The cumulative incidence of DAPT discontinuation was 22.6% at 90 days, and 68.8% at 1 year. In the 90-day landmark analyses, there were no differences in the incidences of a composite of death, myocardial infarction, stroke, or any coronary revascularization (5.9% vs. 9.2%, log-rank P=0.12; adjusted hazard ratio, 0.59; 95% confidence interval, 0.32–1.08; P=0.09) and BARC type 3 or 5 bleeding (1.4% vs. 1.9%, log-rank P=0.62) between the off- and on-DAPT groups at 90 days.
Correct:
Methods and Results: In the OPTIVUS-Complex PCI study multivessel cohort enrolling 978 patients undergoing multivessel PCI, including left anterior descending coronary artery using intravascular ultrasound (IVUS), we conducted 90-day landmark analyses to compare shorter and longer DAPT. DAPT discontinuation was defined as withdrawal of P2Y12
inhibitors or aspirin for at least 2 months. The prevalence of acute coronary syndrome and high bleeding risk by the Bleeding Academic Research Consortium were 14.1% and 52.5%, respectively. The cumulative incidence of DAPT discontinuation was 22.6% at 90 days, and 68.9% at 1 year. In the 90-day landmark analyses, there were no differences in the incidences of a composite of death, myocardial infarction, stroke, or any coronary revascularization (5.9% vs. 9.1%, log-rank P=0.13; adjusted hazard ratio, 0.60; 95% confidence interval, 0.35–1.15; P=0.10) and BARC type 3 or 5 bleeding (1.4% vs. 1.9%, log-rank P=0.62) between the off- and on-DAPT groups at 90 days.
2) Page 1663, left column, line 12–13
Incorrect:
the current study population for the 90-day landmark analyses consisted of 982 patients (Figure 1).
Correct:
the current study population for the 90-day landmark analyses consisted of 978 patients (Figure 1).
3) Pages 1663–1666, Results, “Antiplatelet Therapy and DAPT Discontinuation” section
Incorrect:
Antiplatelet Therapy and DAPT Discontinuation
In the entire study population, the cumulative incidence of DAPT discontinuation was 22.6% at 90 days, and 68.8% at 1 year (Figure 2A). The cumulative incidence of DAPT discontinuation was 90.2% at 90 days and 96.7% at 1 year in patients taking oral anticoagulants, and was 15.6% at 90 days and 65.9% at 1 year in patients not taking oral anticoagulants (Supplementary Figure 1). In the off-DAPT group, the cumulative incidence of DAPT discontinuation was 39.6% at 30 days, 74.8% at 60 days, and 100% at 90 days (Figure 2B), and the median interval from the index PCI to DAPT discontinuation was 36 (IQR: 0–61) days (Table 1). In the on-DAPT group, the cumulative incidence of DAPT discontinuation was 18.7% at 180 days, and 59.6% at 1 year (Figure 2B), and the median interval from the index PCI to DAPT discontinuation was 211 (IQR: 156–264) days (Table 1). At discharge from the index hospitalization for PCI, clopidogrel was more often selected as the P2Y12
inhibitor in the off-DAPT group than in the on-DAPT group (65.8% vs. 52.5%) (Table 1). In terms of the type of antiplatelet monotherapy after DAPT discontinuation, P2Y12
inhibitors were more often selected in the off-DAPT group than in the on-DAPT group (78.4% vs. 50.9%).
Correct:
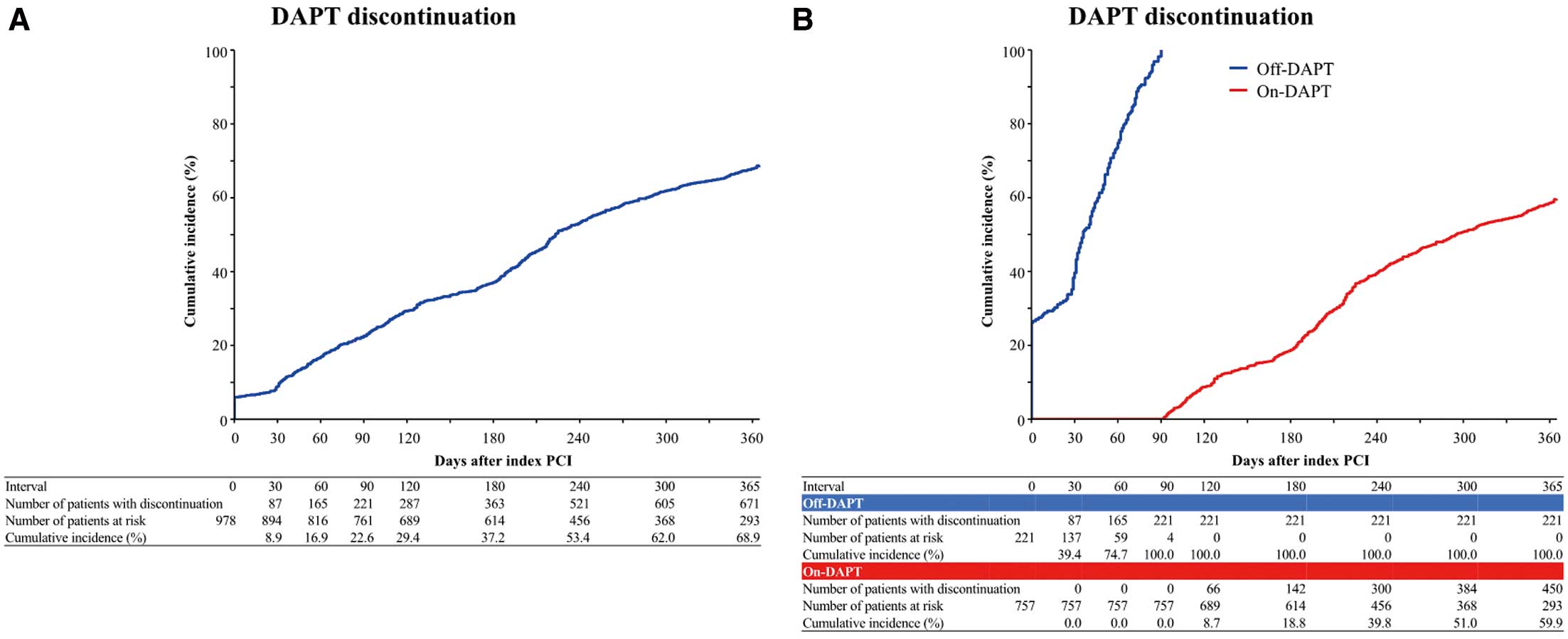
Antiplatelet Therapy and DAPT Discontinuation
In the entire study population, the cumulative incidence of DAPT discontinuation was 22.6% at 90 days, and 68.9% at 1 year (Figure 2A). The cumulative incidence of DAPT discontinuation was 90.2% at 90 days and 96.7% at 1 year in patients taking oral anticoagulants, and was 15.6% at 90 days and 65.9% at 1 year in patients not taking oral anticoagulants (Supplementary Figure 1). In the off-DAPT group, the cumulative incidence of DAPT discontinuation was 39.4% at 30 days, 74.7% at 60 days, and 100% at 90 days (Figure 2B), and the median interval from the index PCI to DAPT discontinuation was 36 (IQR: 0–61) days (Table 1). In the on-DAPT group, the cumulative incidence of DAPT discontinuation was 18.8% at 180 days, and 59.9% at 1 year (Figure 2B), and the median interval from the index PCI to DAPT discontinuation was 211 (IQR: 146–264) days (Table 1). At discharge from the index hospitalization for PCI, clopidogrel was more often selected as the P2Y12
inhibitor in the off-DAPT group than in the on-DAPT group (65.6% vs. 52.7%) (Table 1). In terms of the type of antiplatelet monotherapy after DAPT discontinuation, P2Y12
inhibitors were more often selected in the off-DAPT group than in the on-DAPT group (78.7% vs. 49.8%).
4) Page 1666, “Baseline Characteristics” section
Incorrect:
Baseline Characteristics
The mean age was 71.1 years, and 14.2% of the patients presented as acute coronary syndrome (Table 1). The prevalence of ARC-HBR and Japanese version HBR (J-HBR) was 52.5% and 63.2%, respectively. Patients in the off-DAPT group were older and more often had comorbidities such as heart failure, systolic left ventricular dysfunction, chronic kidney disease, and atrial fibrillation compared with the on-DAPT group (Table 1). The prevalence of ARC-HBR and J-HBR was higher in the off-DAPT group than in the on-DAPT group (68.0% vs. 48.0%, P<0.001 and 73.4% vs. 60.3%, P<0.001, respectively).
Correct:
Baseline Characteristics
The mean age was 71.2 years, and 14.1% of the patients presented as acute coronary syndrome (Table 1). The prevalence of ARC-HBR and Japanese version HBR (J-HBR) was 52.5% and 63.2%, respectively. Patients in the off-DAPT group were older and more often had comorbidities such as heart failure, systolic left ventricular dysfunction, chronic kidney disease, and atrial fibrillation compared with the on-DAPT group (Table 1). The prevalence of ARC-HBR and J-HBR was higher in the off-DAPT group than in the on-DAPT group (68.3% vs. 47.8%, P<0.001 and 73.8% vs. 60.1%, P<0.001, respectively).
5) Page 1668, “Follow-up CAG” section
Incorrect:
Follow-up CAG
The cumulative incidence of follow-up CAG at 1 year was lower in the off-DAPT group than in the on-DAPT group (8.7% vs. 20.3%, log-rank P<0.001) (Supplementary Figure 2).
Correct:
Follow-up CAG
The cumulative incidence of follow-up CAG at 1 year was lower in the off-DAPT group than in the on-DAPT group (8.8% vs. 20.2%, log-rank P<0.001) (Supplementary Figure 2).
6) Page 1668, “Clinical Outcomes” section
Incorrect:
Clinical Outcomes
The cumulative 1-year incidence of the primary endpoint was not different between the off- and on-DAPT groups (5.9% vs. 9.2%, log-rank P=0.12) (Figure 3). After adjusting confounders, the effect of off-DAPT relative to on-DAPT was not significant for the primary endpoint (HR, 0.59; 95% CI, 0.32–1.08; P=0.09) (Table 3).
(an omission)
In the analyses after excluding patients who were on oral anticoagulants at discharge, the cumulative 1-year incidences of the primary endpoint and BARC type 3 or 5 bleeding were not different between groups (5.1% vs. 9.2%; HR, 0.54; 95% CI, 0.25–1.17; P=0.12; and 1.4% vs. 2.9%; HR, 0.49; 95% CI, 0.11–2.08; P=0.33) (Supplementary Table 2).
Correct:
Clinical Outcomes
The cumulative 1-year incidence of the primary endpoint was not different between the off- and on-DAPT groups (5.9% vs. 9.1%, log-rank P=0.13) (Figure 3). After adjusting confounders, the effect of off-DAPT relative to on-DAPT was not significant for the primary endpoint (HR, 0.60; 95% CI, 0.33–1.10; P=0.10) (Table 3).
(an omission)
In the analyses after excluding patients who were on oral anticoagulants at discharge, the cumulative 1-year incidences of the primary endpoint and BARC type 3 or 5 bleeding were not different between groups (5.1% vs. 9.1%; HR, 0.55; 95% CI, 0.25–1.19; P=0.13; and 0.7% vs. 1.9%; HR, 0.38; 95% CI, 0.05–2.92; P=0.35) (Supplementary Table 2).
7) Page 1669, right column, line 4–5
Incorrect:
The cumulative incidence of DAPT discontinuation was only 22.6% at 90 days and 68.8% at 1 year,
Correct:
The cumulative incidence of DAPT discontinuation was only 22.6% at 90 days and 68.9% at 1 year,
8) Page 1664, Table 1 (Corrected)

9) Page 1667, Table 2 (Corrected)

10) Page 1669, Table 3 (Corrected)

11) Page 1662, Figure 1 (Corrected)
12) Page 1666, Figure 2
Correct:
13) Page 1668, Figure 3
Correct:
14) Page 1670, Figure 4
Correct:
15) Supplementary File, Supplementary Table 1 (Corrected)

16) Supplementary File, Supplementary Table 2 (Corrected)

17) Supplementary File, Supplementary Figure 2
Correct:

18) Supplementary File, Supplementary Figure 3
Correct:

19) Supplementary File, Supplementary Figure 4
Correct: