Abstract
Background:
This study investigated the safety and outcome of endovascular therapy for steno-occlusive subclavian or innominate artery disease at a single center over a long period of more than 2 decades.
Methods and Results:
We retrospectively analyzed all endovascular procedures of stenosis or occlusion of the subclavian or innominate artery between January 1990 and October 2013. During the observation period, a total of 130 procedures were attempted in 127 mostly symptomatic patients with stenosis (n=108; 83%) or occlusion (n=22; 17%) of the subclavian (n=119; 92%) and innominate (n=11; 8%) artery. The overall technical success rate was 97.7% (n=127/130). Accounting for the type of lesion, the success rate for stenosis was 100% (n=108/108) and for total occlusion, 86% (n=19/22). The periprocedural complication rate was low and included stroke, transient ischemic attack, and access site complications of 0.8%, 1.5%, and 3.8%, respectively. During a mean follow-up of 28 months the rate of restenosis (>70%) was 12%. Due to the overall low event rate no significant lesion or procedural risk factor for the development of restenosis could be identified.
Conclusions:
Stenosis and occlusion of the subclavian and innominate artery can be treated safely and successfully by endovascular therapy with excellent long-term patency.
The subclavian artery and brachiocephalic trunk are the most common locations for stenotic lesions in the upper extremities.1,2
Steno-occlusive disease in that region occurs in up to 2.7% in the general population and its prevalence increases up to 11.5% in patients with concomitant manifestation of atherosclerosis such as peripheral artery or coronary artery disease.3,4
According to the literature, atherosclerosis is by far the main reason for upper extremity artery stenosis or occlusion besides inflammatory diseases such as Takayasu’s arteritis or radiation-induced vascular disease.3,5–7
Although the majority of patients are asymptomatic,8
affected individuals can develop serious complications such as subclavian steal syndrome, ischemic events in the vertebro-basilary territory or myocardial ischemia (in patients with an internal mammary artery bypass graft).9
Current guidelines recommend the endovascular-first strategy in patients with atherosclerotic lesions of the upper extremities.2
But, given that no randomized data are available and the guideline recommendation is derived only from expert opinion and smaller retrospective analyses, further evidence is of importance to emphasize the current concept.
In this study we analyzed all endovascular procedures of subclavian and innominate artery lesions performed at both sites of our angiology/cardiology institutions since 1990 with respect to safety, efficacy and long-term outcome. Moreover, we assessed the endovascular success rate in revascularization of chronic total occlusions and analyzed potential factors contributing to the development of restenosis.
Methods
Patients
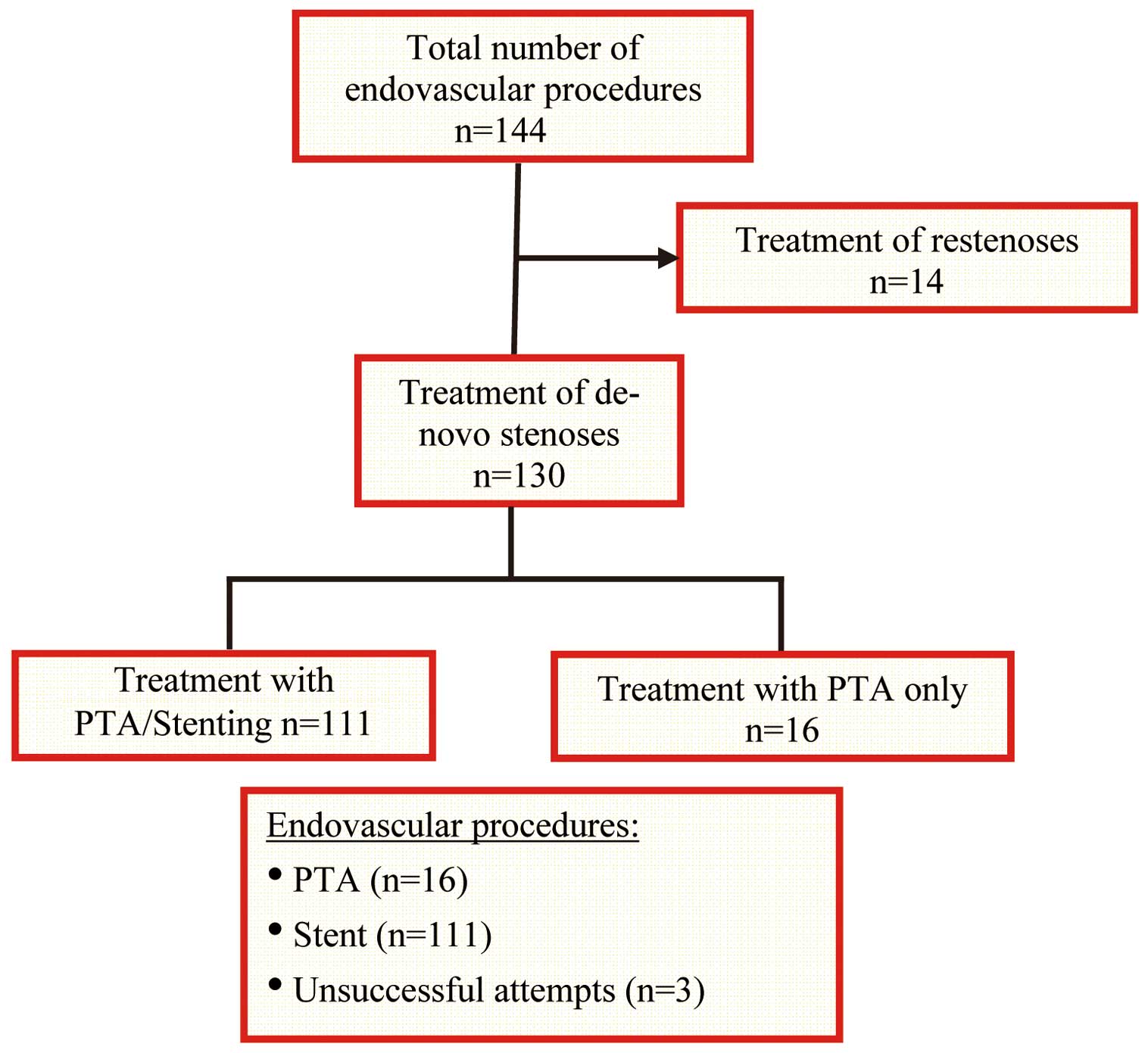
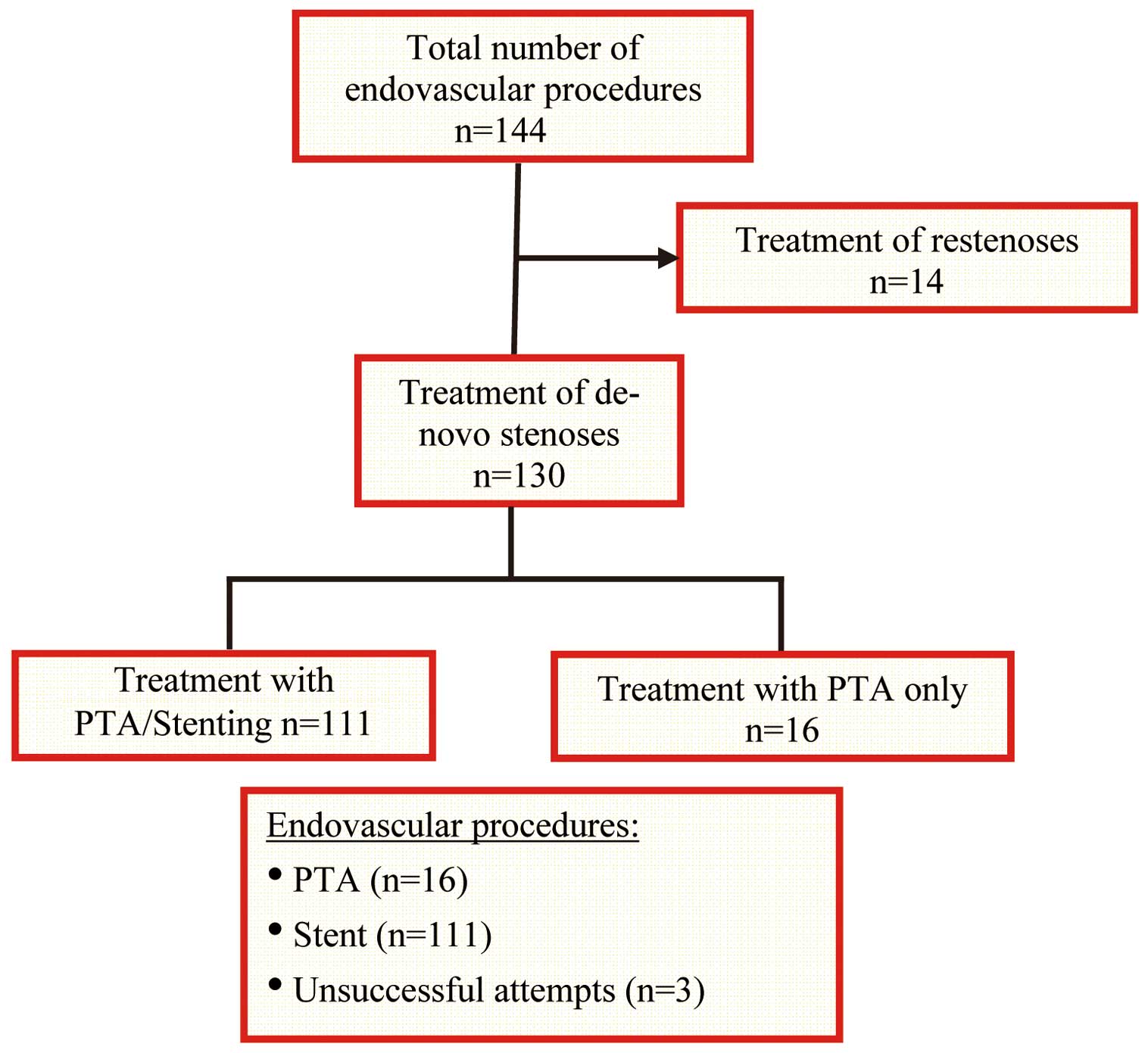
We retrospectively evaluated all patients who underwent endovascular treatment for stenosis or occlusion of the subclavian or innominate artery between January 1990 and October 2013. During the observation period, a total of 144 endovascular procedures was performed (Figure 1). After exclusion of 14 cases due to restenosis, the study finally included a total of 130 interventions of de novo subclavian or innominate artery lesions, which were carried out in 127 patients. Three patients had bilateral interventions, which were undertaken as staged procedures and were considered as independent of each other.
Standard institutional criteria for revascularization included hemodynamic significant stenosis ≥75% or occlusion. The indication for revascularization of the subclavian or innominate artery was made for every patient individually and decision-making was based on the presence of symptoms, concomitant diseases, life expectancy, general surgical risk, progression of severity of the lesion during serial imaging, consideration of the vascular access route, and finally patient wish. One hundred and six patients (84%) presented with symptomatic lesions. Twenty-one patients (16%) were asymptomatic, 7 (6%) of whom were treated due to progression of severity on serial ultrasound imaging, and 13 (10%) due to the patients’ wish.
Patients were considered to have symptomatic lesions when presenting with previous symptoms consistent with subclavian steal including vertigo, syncope, ipsilateral upper extremity paresthesia or claudication, or evidence of cardiac ischemia caused by flow limitation due to the presence of an internal mammary bypass graft, respectively. The degree of stenosis was generally evaluated on duplex ultrasound imaging, which was available in 85% of the patients, according to established criteria.10
The other patients were diagnosed either on magnetic resonance imaging, computed tomography or angiography. Written informed consent was obtained prior to the endovascular procedure and the local ethics committee approved the study.
Follow-up
Clinical and duplex ultrasound follow-up visits to the outpatient department were routinely scheduled 3–6 months, 12 months and annually after the index procedure. The follow-up visits included an interview, clinical examination with blood pressure measurements on both arms and duplex ultrasound of the subclavian artery or innominate artery including the stented segment. Death, transient ischemic attack (TIA)/stroke, vertigo, syncope, claudication as well as restenosis were recorded. The respective data were obtained from charts and outpatient reports and were supplemented with data from follow-up telephone calls. For assessment of in-stent restenosis, duplex ultrasound and blood pressure difference were considered. When clinically relevant, angiography was performed. In-stent restenosis was defined as blood pressure difference >20 mmHg and/or peak velocity ratio >3 on duplex ultrasound as previously described.11
Angiographic restenosis was defined as stenosis in the stented vessel ≥70%.
Angiography
Subclavian and innominate angiograms, which were available in 72% of the study population, were digitally recorded and assessed off-line at the quantitative coronary angiography (QCA) core laboratory (ISAR-RESEARCH Center, Munich, Germany) with an automated edge-detection system (CMS version 7.1, Medis Medical Imaging Systems) by experienced personnel. Qualitative morphological lesion characteristics such as calcification score, degree of stenosis (based on diameter of the vessel, lesion length and diameter of the remaining lumen), access strategy (brachial or femoral) and localization of the lesion (proximal, medial, distal) were evaluated before and after the intervention. Lesion localization was defined as follows: proximal segment, origin of the subclavian artery from the aortic arch reaching to the origin of the vertebral artery; medial segment, segment of the vertebral artery; distal segment, vertebral artery origin up to the axillary artery.
Statistical Analysis
Symmetrically distributed quantitative data are given as mean±SD, and skewed data as median (minimum–maximum). For qualitative data absolute and relative frequencies are presented. Event time analysis was used for time from first procedure to restenosis. In order to avoid violation of the assumption of independence between censoring times and event times, only the first 3 years of follow-up, which can be regarded as the time of routine follow-up, were considered. Later events are described, but were not included in the time-to-event analyses. The Kaplan-Meier method was applied to estimate freedom from restenosis. Kaplan-Meier curves and 95% confidence intervals (CI) are given for the whole study cohort. Log-rank test was used to test for differences in event time distributions between relevant groups. Cox regression models were fitted to the data to investigate the influence of quantitative parameters on the risk of restenosis. Due to the low number of events in the first 3 years, the power for detection of true effects was low.
Results
Patient Characteristics
The patient characteristics are listed in
Table 1. We performed a total number of 130 endovascular procedures in 127 patients with de novo lesions of the subclavian or innominate artery. The mean patient age was 68±11 years (range, 34–87 years). More than half of the procedures were performed in women and were unilateral. Bilateral interventions were undertaken in approximately 2% of cases. The subjects had typical cardiovascular risk factors, most commonly arterial hypertension, followed by hyperlipidemia and smoking. Cardiovascular comorbidities were present in the majority, whereas two-thirds had coronary artery disease and approximately one-third, lower extremity peripheral or carotid artery disease.
Table 1.
Patient Characteristics
| No. interventions |
130 |
| No. patients |
127 |
| Age (years) |
68±11 |
| Sex |
| Male |
58 (46) |
| Female |
69 (54) |
| Risk factors† |
| Hypertension |
109 (86) |
| Hypercholesterolemia |
95 (75) |
| (Ex-)smoker |
68 (54) |
| Family history |
37 (29) |
| Diabetes mellitus |
29 (23) |
| Comorbidity† |
| CAD |
75 (59) |
| Previous MI |
21 (17) |
| Carotid stenosis |
42 (33) |
| Renal artery stenosis |
14 (11) |
| Lower extremity PAD |
43 (34) |
| Previous cardiovascular therapy |
| Coronary intervention |
71 (56) |
| Coronary bypass |
25 (20) |
| Carotid intervention |
21 (17) |
| Carotid endarterectomy |
5 (4) |
| Lower extremity bypass |
7 (6) |
| Lower extremity intervention |
35 (28) |
| Symptoms† |
| Any |
106 (84) |
| Vertigo |
54 (43) |
| Syncope |
15 (12) |
| Arm claudication |
36 (28) |
| Paresthesia |
31 (24) |
| Angina pectoris |
2 (2) |
Data given as mean±SD or n (%). †Based on 127 patients. CAD, coronary artery disease; MI, myocardial infarction; PAD, peripheral artery disease.
The majority of patients were symptomatic and had reverse (58%) or oscillatory (17%) flow in the vertebral artery, mostly leading to subclavian-steal phenomenon with symptoms such as vertigo or syncope. Further symptoms were ipsilateral arm claudication, paresthesia or angina pectoris due to an insufficient perfusion of an internal mammary bypass graft. The mean blood pressure difference in the whole group between the affected and the contralateral upper limb prior to the intervention was 45±20 mmHg. The mean peak velocity as measured on duplex ultrasound within stenotic but not occluded lesions averaged 305±90 cm/s.
Lesion Characteristics
More than two-thirds of the lesions were on the left side within the subclavian artery (Table 2). Of the right-sided lesions, 69% were within the subclavian artery and 31% were located within the innominate artery. The majority of lesions were stenotic or included flow-limiting dissections (2 lesions), which occurred during diagnostic angiography of the left internal mammary artery, whereas 17% of the treated lesions were total occlusions. On angiography, mean percentage of lesions prior to intervention was >80%, and the mean lesion length and diameter were >20 mm and >8 mm, respectively. The majority of lesions were located within the proximal part of the subclavian artery close to the vessel origin and only a few lesions were located in the medial area or distal to the vertebral artery origin.
Table 2.
Lesion Characteristics
| Subclavian artery |
119/130 (92) |
| Innominate artery |
11/130 (8) |
| Side |
| Left |
94 (72) |
| Right |
36 (28) |
| Occlusion |
22 (17) |
| Ultrasound† |
| Blood pressure difference (mmHg) |
45±21 |
| Peak velocity (cm/s) |
305±90 |
| Retrograde flow in vertebral artery |
67/116 (58) |
| QCA† (before intervention) |
| Lesion length (mm) |
22.8±18.7 |
| Vessel diameter (mm) |
8.8±3.8 |
| Mean stenosis (%) |
83.4±14 |
| Calcification |
| Little |
54 (56) |
| Moderate |
27 (28) |
| Severe |
15 (16) |
| Localization† |
| Proximal |
83 (86) |
| Medial |
12 (13) |
| Distal |
1 (1) |
Data given as mean±SD or n (%). †Data not available for every lesion. QCA, quantitative coronary angiography.
Endovascular procedure was successful in 127/130 cases, resulting in an overall technical success rate of 97.7% (Table 3). Given that 3 chronic total occlusions could not be crossed with the wire, the technical success rate for stenotic lesions was 100% (108/108) and for total occlusions 86% (19/22).
Table 3.
Procedural Characteristics
| Success rate (overall) |
127/130 (97.7) |
| Success rate (stenosis) |
108/108 (100) |
| Success rate (occlusion) |
19/22 (86) |
| Residual stenosis (QCA data) (%)† |
6.7 (0–55) |
| Stent |
111/127 (87) |
| PTA only |
16/127 (13) |
| Stent type |
| Balloon-expandable |
96/111 (86) |
| Self-expandable |
15/111 (14) |
| Stent length† (mm) |
31.1±12.2 |
| Stent diameter† (mm) |
8.1±1.4 |
| Balloon-size† (mm) |
7.9±1.3 |
| Max. pressure† (bar) |
12.8±3.2 |
| X-ray† (min) |
11.7 (2.8–61.0) |
| Contrast agent† (ml) |
240 (40–717) |
| Area-dose product† (cGy/cm2) |
3,830 (400–24,434) |
Data given as mean±SD, n (%) or median (min–max). †Data not available for every lesion. PTA, percutaneous transluminal angioplasty. Other abbreviation as in Table 2.
Mere balloon angioplasty was performed in 12.6% (16/127) of the cases. These cases were predominantly undertaken at the beginning of the observation period during the early 1990 s. Stent placement was performed in 111/127 successfully treated lesions (87.4%), whereas the majority of stents were balloon-expandable. The following stent types were used: Omnilink®
(62%), Herculink®
(18%), Palmaz®Blue®
(6%), Acculink®
(5%), Smart®
(4%), Protégé®
(1%), Xact®
(1%), WallStent®
(1%), Precise®
(1%), and Sinus-SuperFlex®
(1%). On average 1.2±0.5 stents were implanted per lesion and the median postprocedural residual stenosis as measured on QCA was 6.7% (range, 0–55%). A small proportion of lesions (13%) was located in the mid-section of the subclavian artery, of which 10 lesions needed additional treatment of the vertebral artery ostium including plain angioplasty or bifurcational T-stenting, while none of these patients had significant plaque shifting into the mammary artery. The overall periprocedural complication rate was low. One patient (0.8%) with complete occlusion of the right subclavian artery developed a minor stroke, presenting with complete left-sided hemiparesis during intervention, which almost completely dissolved at discharge 6 days later. Two patients (1.5%), who underwent intervention of the left subclavian artery, one with a high-grade stenosis and the other with a total thrombotic occlusion, had symptoms consistent with TIA. One patient had vertigo and nystagmus and the other suffered from a short-term 1-sided arm weakness. There was complete resolution of symptoms in both patients within 1 day. Vascular complications at the puncture site were present in 5 patients (3.8%) who developed false aneurysm. In 3 the location was the brachial artery and in 2 it was the right femoral artery, and treatment with ultrasound-guided manual compression or thrombin injection, respectively, was successful. No relevant access site bleeding requiring blood transfusion occurred.
Clinical Follow-up
Follow-up data were available in 79% of the cases. The median follow-up time was 12 months (range, 1–207 months). Evaluation of restenosis was performed in 82% of the patients on ultrasound only, and diagnostic angiography was performed in 18% additionally, and in 3% exclusively. The overall rate of restenosis ≥70% was 12% (12/100;
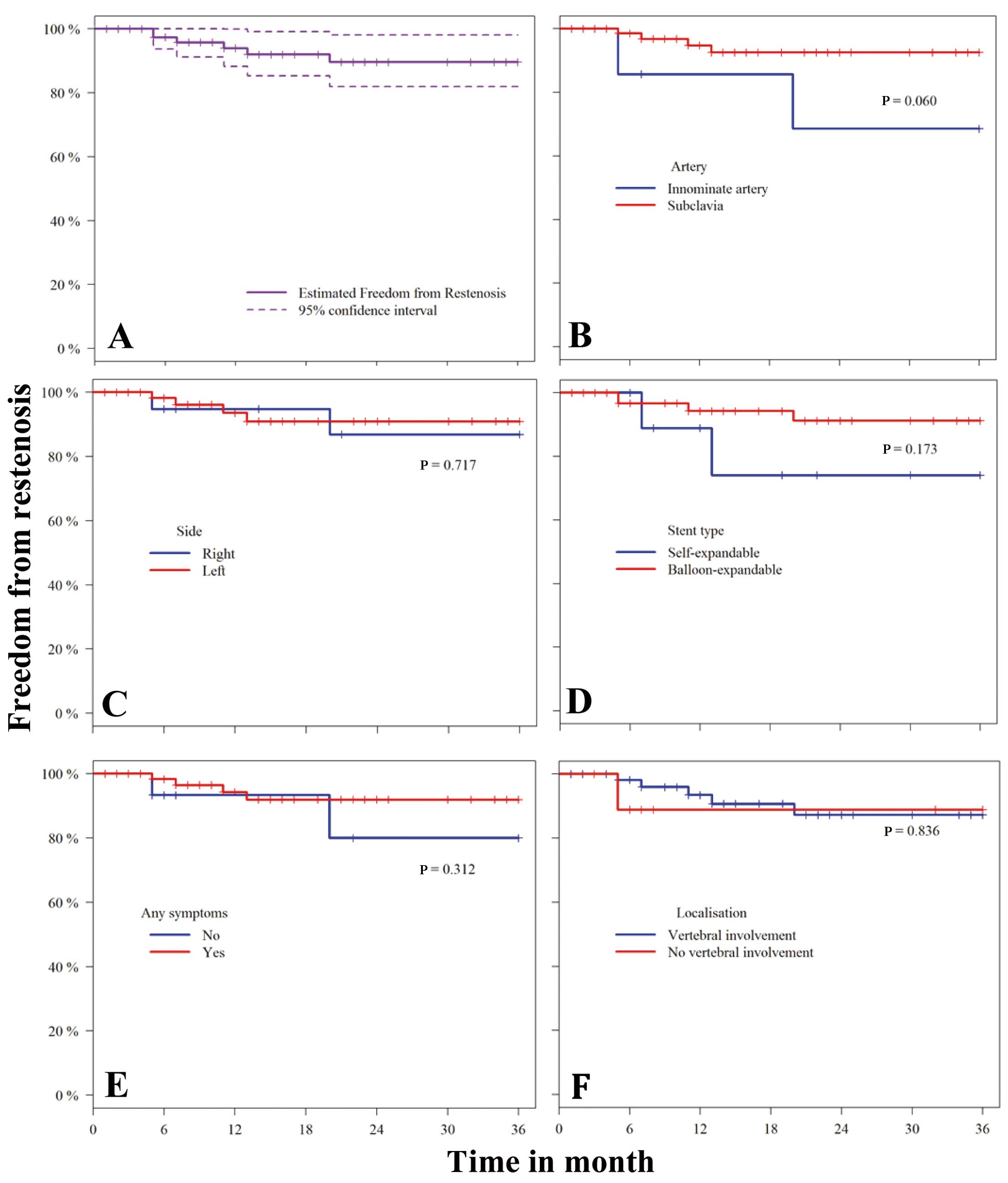
Table 4). The estimated probability of freedom of restenosis was 94% (95%CI: 88–>99%) after 1 year and still 90% (95%CI: 82–98%) after 3 years (Figure 2).
Table 4.
Follow-up
| FU completed |
100/127 (79) |
| Mean FU (months) |
28±38 |
| Median FU (months) |
12 (1–207) |
| Restenosis n (%) |
12/100 (12) |
| BP difference (mmHg)† |
10 (0–60) |
| Peak velocity (cm/s)† |
170 (5–560) |
| Diagnostic at FU |
| Ultrasound only |
82 (82) |
| Angiography alone |
3 (3) |
| Both |
15 (15) |
| Symptomatic at FU |
7 (7) |
Data given as mean±SD, n (%) or median (min–max). †Data not available for every lesion. BP, blood pressure; FU, follow-up.
Recurrence of symptoms, which was present in 7 of 12 patients with proven restenosis, was significantly associated with restenosis (P<0.001), but no significant lesion or procedural risk factor contributing to restenosis could be identified (Table 5).
Table 5.
Univariate Predictors of Restenosis
| Parameters |
Groups |
3-year probability of freedom
from restenosis (%) |
HR |
95% CI |
P-value† |
| Age‡ |
– |
– |
0.95 |
0.88–1.03 |
0.192 |
| Diabetes mellitus |
Yes (n=21) |
90.0±9.5 |
0.95 |
0.11–8.15 |
0.960 |
| No (n=79) |
89.8±4.5 |
| Artery |
Subclavian artery (n=92) |
92.5±3.6 |
0.23 |
0.04–1.24 |
0.060 |
| Innominate artery (n=8) |
68.6±18.6 |
| Side |
Left (n=74) |
90.9±4.4 |
0.73 |
0.13–4.00 |
0.717 |
| Right (n=26) |
86.8±8.9 |
| Stenosis vs. occlusion* |
Stenosis (n=82) |
87.0±5.1 |
– |
– |
0.210 |
| Occlusion (n=18) |
100 |
| Stent length (mm)‡ |
– |
– |
1.00 |
0.95–1.07 |
0.851 |
| Stent diameter (mm)‡ |
– |
– |
1.26 |
0.70–2.28 |
0.435 |
| Localization |
Medial/Distal (n=12) |
90.0±9.5 |
0.95 |
0.11–8.15 |
0.963 |
| Proximal (n=72) |
86.8±5.7 |
| Stent vs. PTA* |
Stent (n=93) |
88.7±4.5 |
– |
– |
0.451 |
| PTA (n=7) |
100 |
| Stent type |
Balloon-expandable (n=81) |
91.2±4.4 |
0.33 |
0.06–1.79 |
0.173 |
| Self-expandable (n=12) |
74.1±16.1 |
†Log-rank test for categorical variables and Cox regression for quantitative measures. ‡Quantitative variable. *No event observed for 1 group, no HR estimable. HR, hazard ratio. Other abbreviation as in Table 3.
Discussion
The major findings of this study are that endovascular treatment of subclavian and innominate artery disease is a safe procedure, which can be accomplished with an excellent clinical success rate and is associated with a good long-term patency rate.
In this study the majority of patients were symptomatic, and approximately 16% were asymptomatic. Most procedures in asymptomatic patients were performed in the 1990 s prior to the introduction of dedicated guidelines. Current recommendations clearly state that symptoms should be present if revascularization of subclavian and innominate artery lesions are considered.2
The technical success rate in the present cohort was 100% for stenotic lesions and 98% including total occlusions, which underlines the feasibility of the endovascular approach in experienced hands and compares well with recently published data.11–15
Even in the beginning of the endovascular treatment era of subclavian and innominate artery disease in the early 1980 s, a high technical success rate ranging from 73% to 100% was reported.16–18
Within the last decade, however, the technical success rates increased, ranging from 97% to 100%, which may be due to the more widespread use of endovascular therapy and an increase in operator experience as well as improvements in materials.11,15,19–21
Although endovascular techniques and facilities have improved over the last 3 decades, interventional treatment of chronic total occlusions remains challenging. Aziz et al reported a mean technical success rate of 64% for occluded lesions from 26 studies dating from 1985 until 2008.22
The wide range of success (0–90.5%) reported in the literature might be due to the high variation in experience of interventionalists with regard to complete occlusions.22,23
This is emphasized by the very high success rate of 86% in the present study and 90% in the Patel et al study, both of which represent the largest available studies at centers with considerable experience in that field.23
Given that no randomized trials are available to date, there is currently insufficient evidence to determine whether stent-supported angioplasty is favorable over plain angioplasty without stenting.24
While some studies showed at least a trend towards an advantage of stenting over plain angioplasty,25
others reported no significant difference between the treatment strategies.20,26
All these observational studies, however, were small, and did not allow for sound statistical conclusions. In the present study, plain angioplasty was a treatment option in the 1990 s. Since that time stenting of the lesion has always been preferred, mainly in order to avoid recoil, which substantially may contribute to recurrence of stenosis, particularly in highly calcified and ostial lesions, as well as to cover potential vascular dissections. There was no significant difference in the present cohort, however, with respect to restenosis in the stent, or the percutaneous transluminal angioplasty (PTA) group. The overall complication rate in the present study was low, with only one minor stroke and two TIA. Similar to the present observation, the risk of cerebral or limb embolization has been consistently low in the literature, ranging from 0 to 5.7%.11,15,27,28
Besides the small number of embolic events, access-site complications are the most common adverse events. As reported previously, there is a higher incidence of complications when using the brachial artery.21
In this context we found a significant increase of local adverse events when the brachial but not the femoral artery served as the access site. The radial approach, which is commonly used in coronary angiography, is an alternative option with a lower access site complication rate.29
Our Department of Cardiology in Munich, however, does not have a large amount of operating experience with regard to the radial approach in supraaortic interventions so far. Femoral access allowing an antegrade procedure is still favorable in the majority of cases, and is used as the primary approach, whereas a combined approach with additional retrograde access allowing double injection technique and guidewire usage in both directions might be crucial for technical success in some cases, especially in the setting of total chronic occlusions.30
During follow-up, the overall rate of restenosis in the present cohort was low, with an excellent 1-year patency rate of 94%. This finding is consistent with previous observational studies reporting primary patency rates between 70% and 90% after 2 years.11,15,21,23,25
These patency rates are similar to those reported after surgery, and underlines that endovascular therapy is an effective and durable alternative to surgery.
Interestingly none of the 19 patients with total occlusion developed restenosis in the present cohort, of whom 18 were treated with stenting and only one with angioplasty alone. Similar observations were also described by de Vries et al, who reported that all of their patients with occlusive lesions were free of restenosis at follow-up.15
Sixt et al noted a 1-year primary patency rate of 33% (1/3) after recanalization of occluded lesions with plain angioplasty, but 82% (18/22) for occlusions treated with stenting,25
which may support stent usage especially in this type of lesion.
There are smaller studies, none of them randomized, showing significant predictors of restenosis such as stent-length, diameter of stents, PTA alone or residual stenosis.31
Due to the overall low number of events in the present study we could not identify a significant predictor of restenosis, but it was clear that at least recurrence of symptoms was associated with restenosis, which emphasizes the importance of accurate selection of patients for subclavian and innominate artery intervention.
Randomized data comparing surgical treatment with the endovascular therapy are lacking. In contemporary surgical studies of the 2000 s there is still a relevant rate of mortality and stroke of 0–11% and 0–7%, respectively, although good long-term patency is documented.22
Current guidelines state that when revascularization is indicated, an endovascular-first strategy is recommended in patients with atherosclerotic lesions of the upper extremities.2
This recommendation, however, is derived from expert opinion and small, retrospective studies and registries. The present high success and low complication rates are in line with the guideline recommendations and further support the endovascular-first strategy.
In our opinion surgery should be reserved only for a complex vascular setting lacking adequate endovascular access site, for lesions with a high thrombotic burden or for symptomatic patients after failed endovascular procedure when conservative, medical treatment is not an option.
This was a single-center retrospective analysis that has all known limitations of such studies. The median follow-up was relatively short at 12 months. Procedural outcome was assessed only until hospital discharge and follow-up data were missing in approximately one-fifth of the cases, due to the very long time period of >20 years, with some data inaccessible, especially from the early 1990 s. Also, due to that fact, some data on procedural characteristics, ultrasound, as well as QCA and localization are incomplete. Finally, due to the overall low rate of restenosis the study was not powered to detect significant predictors for restenosis.
Conclusions
In the present observational single-center study, comprising patients with subclavian and innominate artery obstruction and occlusion, endovascular treatment was safe, effective, and associated with excellent long-term patency rates similar to those for surgery. Thus, the present data, which are in line with previous reports, further support the notion that percutaneous revascularization performed in experienced hands and centers should be regarded as first-line therapy.
Disclosures
The authors declare that they have no conflict of interest.
References
- 1.
Contorni L. The vertebro-vertebral collateral circulation in obliteration of the subclavian artery at its origin. Minerva Chir 1960; 15: 268–271.
- 2.
Brogneaux C, Sprynger M, Magnée M, Lancellotti P; European Society for Cardiology. 2011 ESC guidelines on the diagnosis and treatment of peripheral artery diseases. Rev Med Liege 2012; 67: 560–565 (in French).
- 3.
Shadman R, Criqui MH, Bundens WP, Fronek A, Denenberg JO, Gamst AC, et al. Subclavian artery stenosis: Prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol 2004; 44: 618–623.
- 4.
English JA, Carell ES, Guidera SA, Tripp HF. Angiographic prevalence and clinical predictors of left subclavian stenosis in patients undergoing diagnostic cardiac catheterization. Catheter Cardiovasc Interv 2001; 54: 8–11.
- 5.
Ishihara T, Haraguchi G, Tezuka D, Kamiishi T, Inagaki H, Isobe M. Diagnosis and assessment of Takayasu arteritis by multiple biomarkers. Circ J 2013; 77: 477–483.
- 6.
Ohigashi H, Haraguchi G, Konishi M, Tezuka D, Kamiishi T, Ishihara T, et al. Improved prognosis of Takayasu arteritis over the past decade: Comprehensive analysis of 106 patients. Circ J 2012; 76: 1004–1011.
- 7.
Ishida T, Ishida M, Tashiro S, Yoshizumi M, Kihara Y. Role of DNA damage in cardiovascular disease. Circ J 2014; 78: 42–50.
- 8.
Criqui MH, Fronek A, Barrett-Connor E, Klauber MR, Gabriel S, Goodman D. The prevalence of peripheral arterial disease in a defined population. Circulation 1985; 71: 510–515.
- 9.
Anegawa T, Kai H, Fukuda K, Iwamoto Y, Tsuru T, Itaya N, et al. Respiratory variation of vertebral arterial flow in a patient scheduled for coronary artery bypass graft surgery: Lesson from atypical subclavian steal phenomenon. Circ J 2013; 77: 2412–2414.
- 10.
Hua Y, Jia L, Li L, Ling C, Miao Z, Jiao L. Evaluation of severe subclavian artery stenosis by color Doppler flow imaging. Ultrasound Med Biol 2011; 37: 358–363.
- 11.
Sixt S, Rastan A, Schwarzwalder U, Burgelin K, Noory E, Schwarz T, et al. Results after balloon angioplasty or stenting of atherosclerotic subclavian artery obstruction. Catheter Cardiovasc Interv 2009; 73: 395–403.
- 12.
Miyakoshi A, Hatano T, Tsukahara T, Murakami M, Arai D, Yamaguchi S. Percutaneous transluminal angioplasty for atherosclerotic stenosis of the subclavian or innominate artery: Angiographic and clinical outcomes in 36 patients. Neurosurg Rev 2012; 35: 121–125, discussion 125–126.
- 13.
Brountzos EN, Malagari K, Kelekis DA. Endovascular treatment of occlusive lesions of the subclavian and innominate arteries. Cardiovasc Intervent Radiol 2006; 29: 503–510.
- 14.
Brountzos EN, Petersen B, Binkert C, Panagiotou I, Kaufman JA. Primary stenting of subclavian and innominate artery occlusive disease: A single center’s experience. Cardiovasc Intervent Radiol 2004; 27: 616–623.
- 15.
De Vries JP, Jager LC, Van den Berg JC, Overtoom TT, Ackerstaff RG, Van de Pavoordt ED, et al. Durability of percutaneous transluminal angioplasty for obstructive lesions of proximal subclavian artery: Long-term results. J Vasc Surg 2005; 41: 19–23.
- 16.
Motarjeme A, Keifer JW, Zuska AJ, Nabawi P. Percutaneous transluminal angioplasty for treatment of subclavian steal. Radiology 1985; 155: 611–613.
- 17.
Theron J, Melancon D, Ethier R. “Pre” subclavian steal syndromes and their treatment by angioplasty: Hemodynamic classification of subclavian artery stenoses. Neuroradiology 1985; 27: 265–270.
- 18.
Dorros G, Lewin RF, Jamnadas P, Mathiak LM. Peripheral transluminal angioplasty of the subclavian and innominate arteries utilizing the brachial approach: Acute outcome and follow-up. Cathet Cardiovasc Diagn 1990; 19: 71–76.
- 19.
Przewlocki T, Kablak-Ziembicka A, Pieniazek P, Musialek P, Kadzielski A, Zalewski J, et al. Determinants of immediate and long-term results of subclavian and innominate artery angioplasty. Catheter Cardiovasc Interv 2006; 67: 519–526.
- 20.
Bates MC, Broce M, Lavigne PS, Stone P. Subclavian artery stenting: Factors influencing long-term outcome. Catheter Cardiovasc Interv 2004; 61: 5–11.
- 21.
Berger L, Bouziane Z, Felisaz A, Coffin O, Dugue A, Maiza D. Long-term results of 81 prevertebral subclavian artery angioplasties: A 26-year experience. Ann Vasc Surg 2011; 25: 1043–1049.
- 22.
Aziz F, Gravett MH, Comerota AJ. Endovascular and open surgical treatment of brachiocephalic arteries. Ann Vasc Surg 2011; 25: 569–581.
- 23.
Patel SN, White CJ, Collins TJ, Daniel GA, Jenkins JS, Reilly JP, et al. Catheter-based treatment of the subclavian and innominate arteries. Catheter Cardiovasc Interv 2008; 71: 963–968.
- 24.
Burihan E, Soma F, Iared W. Angioplasty versus stenting for subclavian artery stenosis. Cochrane Database Syst Rev 2011; (10): CD008461, doi:10.1002/14651858.CD008461.pub2.
- 25.
Sixt S, Rastan A, Schwarzwalder U, Schwarz T, Norry E, Frank U, et al. Long term outcome after balloon angioplasty and stenting of subclavian artery obstruction: A single centre experience. Vasa 2008; 37: 174–182.
- 26.
Henry M, Amor M, Henry I, Ethevenot G, Tzvetanov K, Chati Z. Percutaneous transluminal angioplasty of the subclavian arteries. J Endovasc Surg 1999; 6: 33–41.
- 27.
Mordasini P, Gralla J, Do DD, Schmidli J, Keseru B, Arnold M, et al. Percutaneous and open retrograde endovascular stenting of symptomatic high-grade innominate artery stenosis: Technique and follow-up. AJNR Am J Neuroradiol 2011; 32: 1726–1731.
- 28.
Rodriguez-Lopez JA, Werner A, Martinez R, Torruella LJ, Ray LI, Diethrich EB. Stenting for atherosclerotic occlusive disease of the subclavian artery. Ann Vasc Surg 1999; 13: 254–260.
- 29.
Brueck M, Bandorski D, Kramer W, Wieczorek M, Holtgen R, Tillmanns H. A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc Interv 2009; 2: 1047–1054.
- 30.
Higashimori A, Morioka N, Shiotani S, Fujihara M, Fukuda K, Yokoi Y. Long-term results of primary stenting for subclavian artery disease. Catheter Cardiovasc Interv 2013; 82: 696–700.
- 31.
Schillinger M, Haumer M, Schillinger S, Ahmadi R, Minar E. Risk stratification for subclavian artery angioplasty: Is there an increased rate of restenosis after stent implantation? J Endovasc Ther 2001; 8: 550–557.