Article ID: CJ-14-1098
Article ID: CJ-14-1098
Background: Wearable cardioverter-defibrillators (WCD) have been available in Japan since April 2014, but their application is still limited.
Methods and Results: We report 9 patients with a WCD applied between April and September 2014. All patients were at high risk of life-threatening ventricular arrhythmias. During WCD use, 1 patient had sustained ventricular tachycardia and successful shock delivery; 6 (67%) subsequently underwent implantable cardioverter-defibrillator (ICD) therapy, while 2 had no requirement because of reduced risk, and 1 died of heart failure during WCD use.
Conclusions: WCD is useful during acute-phase care of high-risk patients, and may help to avoid unnecessary ICD implantation.
The wearable cardioverter-defibrillator (WCD; LifeVest 4000, ZOLL, PA, USA) is a vest-type device that is capable of continuous ECG monitoring, and automatic detection and defibrillation of ventricular tachycardia/fibrillation (VT/VF).1,2 It has been in use worldwide, especially in the USA and Germany, and its efficacy in detecting and treating VT/VF has been demonstrated in patients at high risk of sudden cardiac death (SCD) who are not clearly indicative of implantable cardioverter-defibrillator (ICD) therapy or are at temporary high-risk of SCD until ICD implantation.3,4
Editorial p ????
The WCD has been available in Japan since April 2014, but information on its usefulness and efficacy is limited. Here, we report our primary experience of WCD use describing its indication, patient compliance, and clinical efficacy.
Nine consecutive patients treated with a WCD between April and September 2014 were studied. Details of the WCD and the algorithm of arrhythmia detection have been described elsewhere.1,2 Daily WCD wearing time and ECG recordings were collected from the WCD monitoring system. In the present cases, the threshold heart rate for both the VT and VF zones was set at 200 beats/min. Time from VT detection to shock delivery was 60 s for VT and 25 s for VF. Shock energy was set to biphasic 150 J for both VT and VF. The study was approved by the institutional ethics committee.
Data are expressed as median (25–75th percentile) or n (%). Statistical analyses were performed using JMP 10 software (SAS, Cary, NC, USA).
The clinical characteristics of the patients are summarized in Table. The median age was 56 (51–63) years, and 7 (78%) were male. The median left ventricular ejection fraction (LVEF), evaluated by echocardiography, was 35.3 (29.9–61.2) %. The underlying heart diseases were prior myocardial infarction (MI: 3 recent, 2 previous MI), and 1 case each of variant angina, fulminant myocarditis, cardiac amyloidosis, and idiopathic VF. In all, 8 patients (89%) had experienced a recent sudden cardiac arrest from VT or VF, and 1 had reduced LVEF (29.8%) and heart failure (HF), but not VT/VF, after recent MI. All were considered to be potentially indicative of ICD.
| All patients (n=9) | |
|---|---|
| Age (years) | 56 (51–63) |
| Male sex | 7 (78%) |
| Body mass index (kg/m2) | 25.2 (19.9–29.5) |
| Baseline heart disease | |
| Myocardial infarction | |
| Recent | 3 (33%) |
| Previous | 2 (22%) |
| Variant angina | 1 (11%) |
| Fulminant myocarditis | 1 (11%) |
| Cardiac amyloidosis | 1 (11%) |
| Idiopathic VF | 1 (11%) |
| LVEF (%) | 35.3 (29.9–61.2) |
| History of VT/VF | 8 (89%) |
| WCD wearing time (h/day) | 23.7 (23.6–23.9) |
| Duration of WCD use (days) | 21 (7–31) |
| Shock delivery during WCD use | 1 (11%) |
| ICD implantation | 6 (67%) |
Data are shown as median (25–75th percentile) or n (%).
ICD, implantable cardioverter-defibrillator; LVEF, left ventricular ejection fraction; VF, ventricular fibrillation; VT, ventricular tachycardia; WCD, wearable cardioverter-defibrillator.
Mean daily WCD wearing time was 23.7 (23.6–23.9) h/day and none of the patients complained about wearing the device. All patients were able to manage the battery system of the WCD by themselves. Median duration of WCD use was 21 (7–31) days. During WCD use, 1 patient with cardiac amyloidosis died of HF and the patient with reduced LVEF (29.8%) and without prior VT/VF had a sustained VT at 18 days after MI, for which lifesaving shock therapy was delivered (Figure). He lost consciousness during VT and therefore did not feel any pain on shock delivery. After this event, nifekalant was administered intravenously, and then amiodarone orally, with no further recurrence of VT. Because he was being treated for a testicular abscess at that time, ICD implantation was delayed, but finally was undergone at 27 days after WCD shock delivery. The other 7 patients had neither VT/VF nor shock therapy. Notably, 6 patients (6/9, 67%) subsequently underwent ICD implantation following WCD use and 2 (variant angina and fulminant myocarditis) had no requirement for it because of reduced risk of VT/VF after optimal pharmacological therapy and improvement in cardiac function.
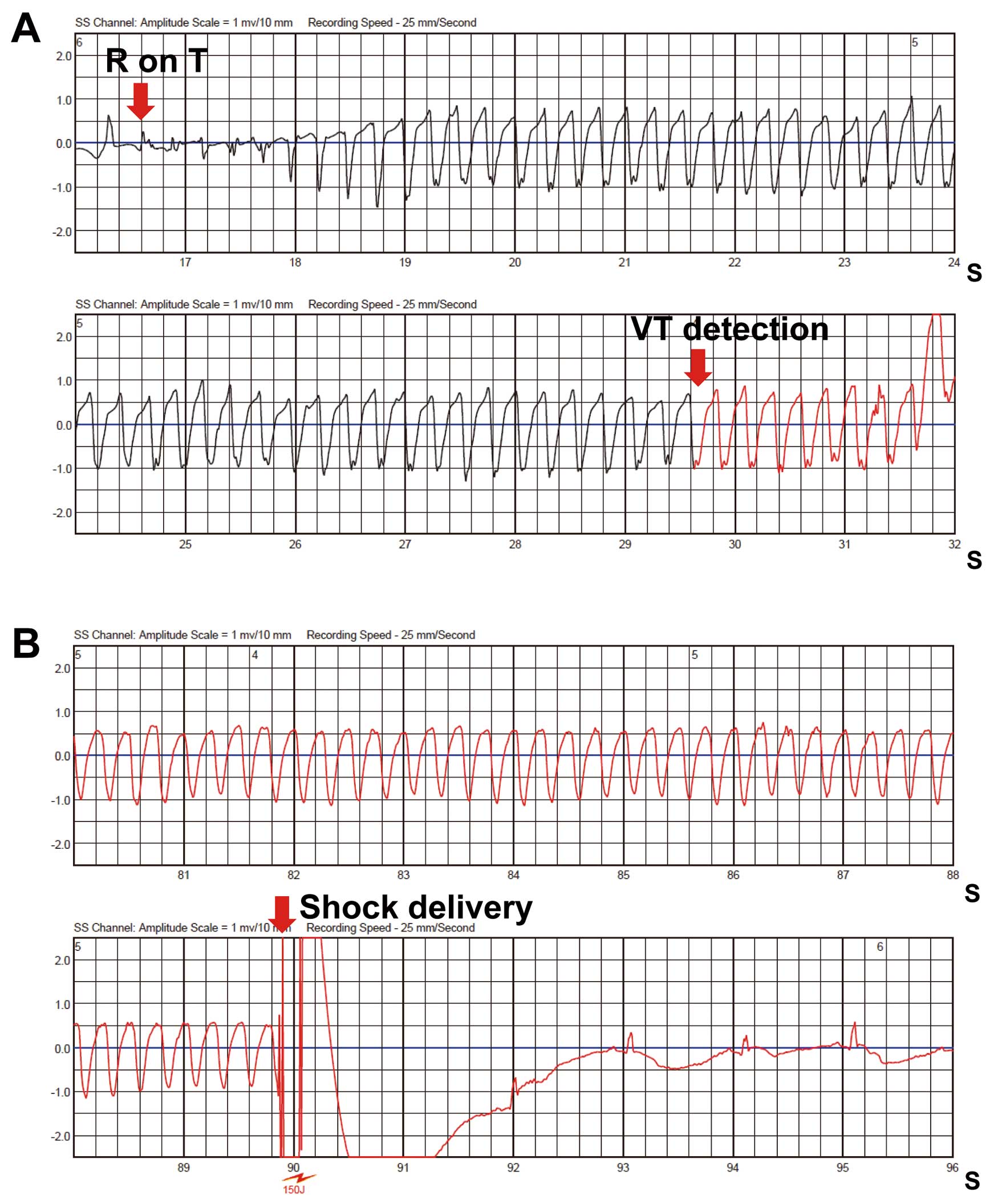
ECG recordings from a patient with a wearable cardioverter-defibrillator (WCD). (A) First red arrow indicates R on T followed by ventricular tachycardia (VT). Second arrow indicates starting point of VT detection by the WCD. (B) Shock (150 J) delivery at 60 s after VT detection by WCD and VT termination are shown.
We provide the first experience of WCD use in 9 Japanese patients at high risk for SCD from VT/VF, all of whom were potentially indicative of ICD implantation. One patient for primary prevention had successful shock therapy and 2 needed only temporary WCD use without subsequent ICD implantation. All patients showed excellent compliance. Despite the small number of patients, our findings indicate that WCD is useful and tolerable in the acute phase of care of high-risk patients, and may help to avoid unnecessary ICD implantation.
WCD is indicated for patients who are at high risk for SCD from VT/VF, but still need to be evaluated for subsequent ICD implantation, or who meet the criteria for ICD implantation, but need more time because of conditions such as infection. In the present cases, 5 of 6 patients subsequently undergoing ICD implantation met the criteria for ICD prior to WCD use because of their secondary prevention indication.5 However, ICD implantation for these patients was delayed, mainly because of infection, and therefore WCD was used temporarily until the day of ICD implantation. The other ICD patient with successful WCD shock therapy, the first case in Japan, was not a clear candidate for ICD implantation prior to WCD use, but was at high risk for SCD.6 Indeed, recent studies demonstrate that WCD use may benefit patients at high risk for SCD with reduced LVEF (<35%) early after MI onset or after coronary revascularization.7,8 Attention should be paid to the 2 patients (variant angina and fulminant myocarditis) without subsequent ICD implantation. They had VF in the acute phase, but did not meet the criteria for ICD implantation at that time, because their risk might possibly be reduced by optimal pharmacological or mechanical support therapy. As expected, risk reduction in these 2 patients was achieved after optimal therapies, and therefore they had no requirement for ICD implantation. Thus, WCD is useful for patients at temporary high risk for SCD from VT/VF if such a risk can be relieved by optimal therapy in the short term.
In all cases, WCD use was in the hospital ward and all patients showed excellent compliance, as evaluated by daily WCD wearing time. Only the patient with variant angina wore the WCD for 10 days in the ward and then continued for an additional 67 days at home after discharge, with excellent self-management. Further studies on WCD use as outpatients are required. Moreover, from the risk management point of view, the WCD is particularly useful in managing high-risk patients in the general ward of the hospital.
In conclusion, we had a first experience of successful WCD shock therapy in Japan. WCD is useful in the acute phase of care of high-risk patients, and its temporary use may help to avoid unnecessary ICD implantation.
We thank Mr Takeshi Goto and Mr Eiichi Tomita in the Department of Clinical Engineering, Hirosaki University Hospital, for excellent technical support.
None of the authors has disclosures.
There was no financial support for this study.