Article ID: CJ-14-1374
Article ID: CJ-14-1374
A 53-year-old woman was referred to hospital for cardiac screening to evaluate cardiomegaly on chest X-ray. Electrocardiogram showed normal sinus rhythm and negative T in V4–V6. The patient had no symptoms and no history of cardiac disease or Kawasaki disease. Transthoracic echocardiography showed dilated left atrium (end-systolic volume, 108 ml) and left ventricle (end-diastolic volume, 154 ml) with left ventricular ejection fraction of 62%. No regional motion abnormality was found. The entire left coronary artery (LCA), from the left main to the left anterior descending coronary artery (LAD) and circumflex branch, was markedly dilated. In addition, the right coronary artery (RCA) was dilated as well. The vessel diameters of the proximal site of the LAD and RCA were 23 mm and 12 mm, respectively. Color Doppler imaging showed turbulent coronary blood flow around the heart (Figure 1A; Movie S1). The blood flow of the septal branch was shown in red (Figure 1B; Movie S2), indicating collateral connection from RCA to LAD via septal branches, and it had high flow velocity of 2.3 m/s (Figure 1C). Normally, blood flow of the septal branch is shown in blue with a speed of 0.10–0.30 m/s. A jet flow draining from the left main coronary artery (LMCA) to the main pulmonary artery was also visualized (Figure 1D). The ostium of the RCA was visualized, but neither the ostium of the LCA in 2-D mode nor blood flow running from the ascending aorta into the LCA in color mode, were detected. No significant valvular disease was found. Aortic valve was tricuspid and coronary sinus was not dilated.
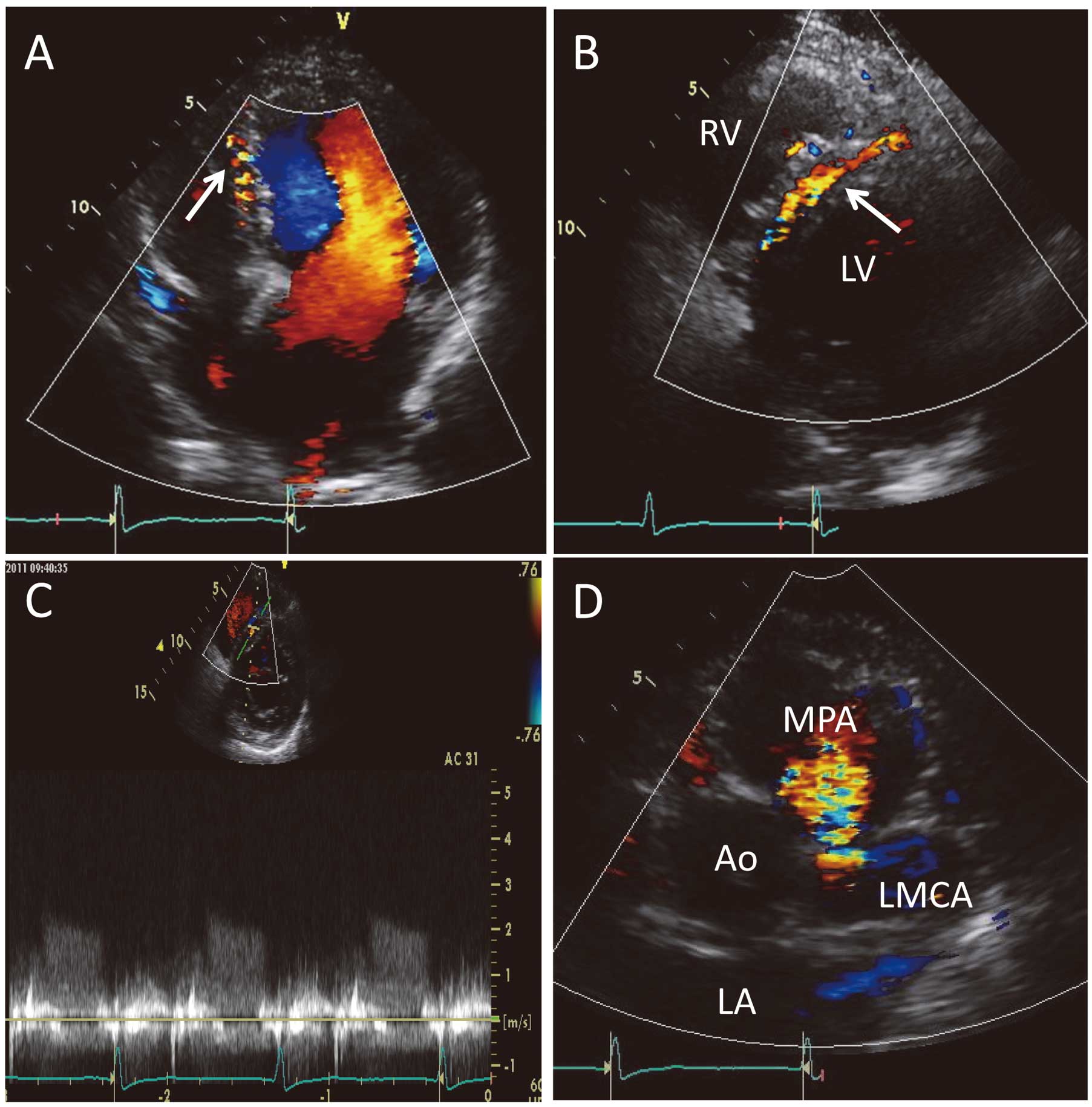
(A,B) Color Doppler transthoracic echocardiography (arrow, blood flow of septal branch). (C) Doppler flow velocity profile of septal branch. (D) Color Doppler transthoracic echocardiography showing the jet flow from left main coronary artery (LMCA) to main pulmonary artery (MPA). Ao, ascending aorta; LA, left atrium; LV, left ventricle; RV, right ventricle.
Consequent coronary computed tomography (CT) showed that the jet flow drained from dilated LMCA into the main pulmonary artery (Figure 2A), similar to the echocardiographic finding. All coronary arteries were ectatic and serpiginous, having diameters 6-fold that of healthy vasculature. No significant coronary stenosis was detected. Volume-rendered 3-D reconstruction showed that huge tortuous coronary arteries were connected to each other through collateral vessels, forming a vascular basket (Figures 2B,C). The RCA originated from the ascending aorta, but the LCA was not connected to the ascending aorta, only to the main pulmonary artery (Figure 2D). Considering the echocardiographic and coronary CT information, we reached a diagnosis of complex anomaly of Bland-White-Garland syndrome, known as anomalous LCA from the pulmonary artery (ALCAPA) syndrome. We recommended reparative surgery but the patient refused because she had no symptoms.
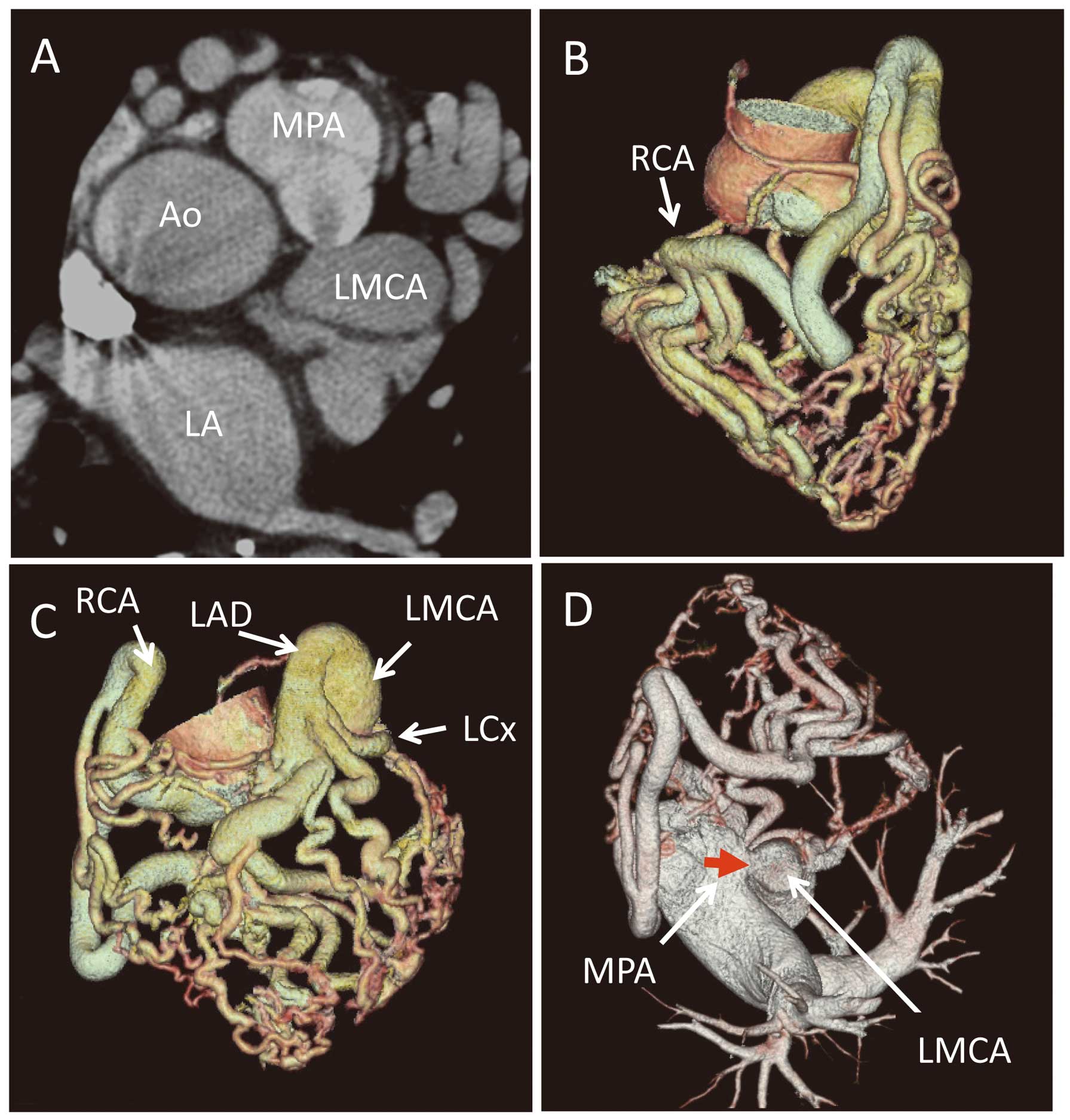
(A) Coronary computed tomography showing the jet flow from left main coronary artery (LMCA) to main pulmonary artery (MPA). (B–D) Volume-rendered 3-D coronary computed tomography. (D) Red arrow, ostial site of the LMCA. Ao, ascending aorta; LA, left atrium; LAD, left anterior descending artery; LCx, left circumflex branch; RCA, right coronary artery.
Owing to recent developments in echocardiography, flow direction and velocity in the coronary artery can now be determined.1–3 In the clinical setting, reversed direction of coronary flow suggests the existence of collateral blood flow to feed occluded coronary artery;4 in particular, reversed septal flow indicates total occlusion of the LAD.5 In the present case, the dilated septal branch had reversed blood flow with high velocity, meaning that a large blood volume ran into the LAD through the septal branch from the RCA. LMCA was assumed to be occluded at the ostial site. Considering the jet flow from the LMCA to main pulmonary artery, this patient was suspected to have coronary to pulmonary artery fistula with coronary ectasia accompanied by ostial occlusion of LMCA on echocardiography. Consequent coronary CT provided anatomical information on the whole coronary tree. According to coronary CT, LMCA originated from the main pulmonary trunk, not from the ascending aorta. After combined non-invasive imaging, which provided physiological information via echocardiography and anatomical information via coronary CT, a diagnosis of ALCAPA syndrome was reached.
ALCAPA syndrome is a rare congenital cardiac anomaly occurring in one of 300,000 live births and is usually isolated.6,7 ALCAPA does not cause any negative effects prenatally because of the favorable fetal physiology that includes equivalent pressures and oxygen concentrations in the main pulmonary artery and aorta. This results in no stimulus for collateral vessel formation between the RCA and LCA systems. Shortly after birth, decrease in pressure, resistance and oxygen content of pulmonary artery leads to hypoperfusion of myocardium by desaturated blood under low pressure. Left untreated, the mortality rate in the first year of life is 90% secondary to broad myocardial ischemia, infarction and heart failure.8 Sudden death occurs because of inadequate collateral circulation between the LCA and RCA systems. As collateral circulation between the RCA and LCA systems develops, LCA flow reverses and enters the pulmonary trunk due to the low pulmonary vascular resistance (coronary steal phenomenon). Approximately 10% are diagnosed in adulthood due to exertional chest pain and dyspnea caused by inadequate myocardial perfusion. In extremely rare cases, ALCAPA without symptoms is accidentally detected on cardiac screening in adults,9 and most have left-to-right shunting from RCA via LCA to main pulmonary artery through highly developed collateral vessels, as in the present case. Currently, the prognosis of ALCAPA is dramatically improved as a result of early diagnosis due to developments in Doppler echocardiography and improvement of surgical technique.10–12
Conflict of Interest: The authors declare no conflicts of interest.
Supplementary File 1
Movie S1. Turbulent coronary blood flow around the heart.
Supplementary File 2
Movie S2. The blood flow of the septal branch.
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-14-1374