Abstract
Background:
Little is known about the clinical outcomes of patients with different types of coronary bifurcation lesions. We sought to compare long-term clinical outcomes of patients with true or non-true bifurcation lesions who underwent percutaneous coronary intervention.
Methods and Results:
We compared major adverse cardiac events (MACE: cardiac death, myocardial infarction [MI], or target lesion revascularization) between 1,502 patients with true bifurcation lesions (51.8%) and 1,395 with non-true bifurcation lesions (48.2%). True bifurcation lesions were defined as Medina classification (1.1.1), (1.0.1), or (0.1.1) lesions. During a median follow-up of 36 months, MACE occurred in 296 (10.2%) patients. Patients with true bifurcation lesions had a significantly higher risk of MACE than those with non-true bifurcation lesions (HR 1.39; 95% CI 1.08–1.80; P=0.01). Among true bifurcation lesions, Medina (1.1.1) and (0.1.1) were associated with a higher risk of cardiac death or MI than Medina (1.0.1) (HR 4.15; 95% CI 1.01–17.1; P=0.05). During the procedure, side branch occlusion occurred more frequently in Medina (1.1.1) and (1.0.1) than Medina (0.1.1) lesions (11.5% vs. 7.4%, P=0.03).
Conclusions:
Patients with true bifurcation lesions had worse clinical outcomes than those with non-true bifurcation lesions. Procedural and long-term clinical outcomes differed according to the type of bifurcation lesion. These findings should be considered in future bifurcation studies.
The treatment of coronary bifurcation lesions is challenging for interventional cardiologists, even in the era of drug-eluting stent (DES). Several randomized trials have been carried out to determine the most effective strategies for percutaneous coronary intervention (PCI) for coronary bifurcation lesions.1–3
As a result, the provisional approach is now accepted as the standard strategy for coronary bifurcation lesions.4–6
However, little is known about the clinical outcomes of patients with different bifurcation types, especially when comparing true and non-true bifurcation lesions. Therefore, we sought to investigate the long-term clinical outcomes according to true vs. non-true bifurcation lesions in patients undergoing PCI for bifurcation lesions on the basis of a large bifurcation registry.
Methods
Study Population
The COronary BIfurcation Stent (COBIS) II registry is an observational, multicenter, real-world registry of patients treated with DES for coronary bifurcation lesions. From 18 major coronary intervention centers in Korea, consecutive patients were enrolled between January 2003 and December 2009. The inclusion criteria were (1) coronary bifurcation lesions treated with DES alone, and (2) main vessel (MV) diameter ≥2.5 mm and side branch (SB) diameter ≥2.3 mm. The exclusion criteria were (1) presence of cardiogenic shock or cardiopulmonary resuscitation and (2) protected left main disease. This registry was sponsored by the Korean Society of Interventional Cardiology. The local institutional review board at each hospital approved this study and waived the requirement for informed consent for access to each institutional PCI registry.
All bifurcation lesions were classified according to the Medina classification, in which the proximal MV, distal MV, and SB components of the bifurcation are respectively allocated a score of 1 or 0 depending on the presence or absence of >50% diameter stenosis.7
Medina classification was based on the operator’s visual inspection. True bifurcation lesions were defined as lesions significantly involved in both the MV and the ostium of the SB.8
Accordingly, lesions with Medina classifications (1.1.1), (1.0.1), and (0.1.1) were included in the true bifurcation group.9,10
All other lesions were included in the non-true bifurcation group.
PCI
PCI was performed according to current practice guidelines. All patients received loading doses of aspirin (300 mg) and clopidogrel (300–600 mg) before PCI unless antiplatelet medications had previously been prescribed. Unfractionated heparin was administered during PCI in order to achieve an activated clotting time of 250–300 s. The treatment strategy, stenting techniques, final kissing balloon (FKB) inflation, type of DES, and use of intravascular ultrasound (IVUS) were determined by the operator. Following PCI, aspirin was continued indefinitely. The duration of clopidogrel treatment was also at the operator’s discretion.
Data Collection and Angiographic Analysis
Clinical, laboratory, angiographic, procedural, and outcome data were obtained using a web-based reporting system. Additional information was collected by medical record review or telephone interview. Using standard qualitative and quantitative angiographic methods,11
baseline and procedural coronary angiograms were analyzed at the angiographic core laboratory (Heart Vascular Stroke Institute, Samsung Medical Center, Seoul, Korea) with an automated edge-detection system (Centricity CA1000, GE, Waukesha, WI, USA). Bifurcation lesions were divided into 3 segments for quantitative coronary angiographic analysis: proximal MV, distal MV, and SB ostium.12
We determined the minimum luminal diameter (MLD) and reference diameter (RD) for each segment. In the distal MV and SB ostium, MLDs were measured <5 mm distal to the SB take-off. The MV RD was the average of the proximal and distal MV RD, and the MV MLD was the minimum of the proximal and distal MV MLDs. Percent diameter stenosis was calculated as 100×(RD–MLD)/RD. Bifurcation angle was defined as the angle between the distal MV and the SB at its origin using the angiographic projection with the widest separation of the 2 branches.13
Study Endpoints and Definitions
Major adverse cardiac events (MACE) were defined as a composite of cardiac death, myocardial infarction (MI), or target lesion revascularization (TLR) during follow-up. All deaths were considered cardiac unless a definite non-cardiac cause was established. MI was defined as elevated cardiac enzymes (troponin or MB fraction of creatine kinase) greater than the upper limit of the normal value, with ischemic symptoms or ECG findings indicative of ischemia that was not related to the index procedure. TLR was defined as repeat PCI of the lesion within 5 mm of stent deployment or bypass graft surgery of the target vessel. Definite or probable stent thrombosis (ST) was assessed according to the definitions of the Academic Research Consortium.14
Remote site intervention was defined as PCI of any lesion outside the bifurcation lesion at index admission. SB occlusion and MV occlusion were defined as development of a Thrombolysis in Myocardial Infarction (TIMI) flow grade <3 during the procedure. Angiographic success was defined as a TIMI flow grade 3, <30% residual stenosis in MV, and <50% residual stenosis in SB by visual estimation.15
All outcome data were identified by the patient’s physician and confirmed by the principle investigator of each hospital. For validation, information about vital status was obtained from the National Population Registry of the Korea National Statistical Office using a unique personal identification number.
Statistical Analysis
Categorical variables are summarized as frequency with percentage and were compared using the chi-square test or Fisher’s exact test. The linear-by-linear association test was used to test trend among the binomial proportions. Continuous variables are presented as median with interquartile range (IQR) and were compared using the Mann-Whitney U test. The event-free survival curves were constructed using Kaplan-Meier estimates and were compared with the log-rank test. Cox regression analysis was performed to identify the hazard rates of true bifurcation compared with non-true bifurcation. Covariates that were statistically significant on univariate analysis and/or those that were clinically relevant were included in the multivariate models. To avoid the overfitting problem caused by a limited number of events, we restricted the number of covariates to include age, sex, acute coronary syndrome (ACS), diabetes mellitus, left ventricular dysfunction, left main bifurcation, type of stent used, 2-stent technique, FKB, use of IVUS, remote site intervention, MV stent length, RDs of the MV and SB, and the angle between the MV and SB. Interactions between true bifurcation and covariates were tested by incorporation of formal interaction terms in multivariate Cox models. All tests were 2-tailed, and P values <0.05 were considered significant. SPSS version 20 (IBM, Armonk, NY, USA) was used for statistical analysis.
Results
Clinical, Angiographic, and Procedural Characteristics
From January 2003 through December 2009, 2,897 consecutive patients were enrolled from 18 major coronary intervention centers in Korea: 1,502 patients (51.8%) had true bifurcation lesions and 1,395 (48.2%) had non-true bifurcation lesions. The baseline clinical characteristics of the 2 groups are shown in
Table 1. Patients with true bifurcation lesions had a higher prevalence of ACS at admission and left ventricular systolic dysfunction than those with non-true bifurcation lesions.
Table 1.
Baseline Clinical Characteristics of Patients With True or Non-True Bifurcation Lesions Who Underwent PCI in COBIS II
| |
True bifurcation
(n=1,502) |
Non-true bifurcation
(n=1,395) |
P value |
| Age, years |
63 (55–70) |
63 (55–69) |
0.49 |
| Male |
1,084 (72.2) |
999 (71.6) |
0.74 |
| Acute coronary syndrome |
960 (63.9) |
838 (60.1) |
0.03 |
| Current smoker |
376 (25.0) |
357 (25.6) |
0.73 |
| Diabetes mellitus |
437 (29.1) |
403 (28.9) |
0.90 |
| Hypertension |
882 (58.7) |
793 (56.8) |
0.31 |
| Dyslipidemia |
489 (32.6) |
417 (29.9) |
0.12 |
| Chronic kidney disease |
46 (3.1) |
35 (2.5) |
0.37 |
| Prior MI |
93 (6.2) |
80 (5.7) |
0.60 |
| Prior revascularization |
216 (14.4) |
198 (14.2) |
0.89 |
| LV ejection fraction, %* |
60.0 (52.0–65.0) |
60.0 (54.7–66.0) |
0.03 |
Data are presented as median (interquartile range) or n (%). *Available in 1,267 patients (84.4%) with true bifurcation and 1,130 patients (81.0%) with non-true bifurcation lesions. MI, myocardial infarction; PCI, percutaneous coronary intervention.
Angiographic and procedural characteristics are shown in
Table 2. Left main bifurcation lesions were more prevalent in patients with non-true bifurcation lesions than in those with true bifurcation lesions. In patients with true bifurcation lesions, the 2-stent technique, FKB, and remote site intervention were performed more frequently, but IVUS was used less frequently. The MV stents implanted in true bifurcation lesions were longer and narrower than those used for non-true bifurcation lesions. The SB stents implanted in true bifurcation lesions were shorter and narrower than those used for non-true bifurcation lesions.
Table 2.
Angiographic and Procedural Characteristics of Patients With True or Non-True Bifurcation Lesions Who Underwent PCI in COBIS II
| |
True bifurcation
(n=1,502) |
Non-true bifurcation
(n=1,395) |
P value |
| Bifurcation location |
|
|
<0.001 |
| Left main |
358 (23.8) |
495 (35.5) |
|
| LAD/diagonal |
907 (60.4) |
644 (46.2) |
|
| LCX/OM |
153 (10.2) |
196 (14.1) |
|
| RCA bifurcation |
84 (5.6) |
60 (4.3) |
|
| Medina classification |
|
|
– |
| True bifurcation |
|
|
– |
| 1.1.1 |
938 (62.5) |
– |
|
| 0.1.1 |
353 (23.5) |
– |
|
| 1.0.1 |
211 (14.0) |
– |
|
| Non-true bifurcation |
|
|
– |
| 1.1.0 |
– |
427 (30.6) |
|
| 1.0.0 |
– |
346 (24.8) |
|
| 0.1.0 |
– |
508 (36.4) |
|
| 0.0.1 |
– |
114 (8.2) |
|
| No. of diseased vessels |
|
|
<0.001 |
| 1 |
601 (40.0) |
666 (47.7) |
|
| 2 |
404 (26.9) |
394 (28.2) |
|
| 3 |
497 (33.1) |
335 (24.0) |
|
| Stent type |
|
|
0.05 |
| Sirolimus-eluting |
753 (50.1) |
661 (47.4) |
|
| Paclitaxel-eluting |
437 (29.1) |
385 (27.6) |
|
| Everolimus-eluting |
159 (10.6) |
189 (13.5) |
|
| Zotarolimus-eluting |
150 (10.0) |
159 (11.4) |
|
| Other |
3 (0.2) |
1 (0.1) |
|
| 2-stent technique |
574 (38.2) |
196 (14.1) |
<0.001 |
| Crush |
265 (17.6) |
107 (7.7) |
|
| T-stenting |
212 (14.1) |
67 (4.8) |
|
| Kissing or V-stenting |
78 (5.2) |
19 (1.4) |
|
| Culottes |
19 (1.3) |
3 (0.2) |
|
| FKB |
853 (56.8) |
496 (35.6) |
<0.001 |
| Guidance of IVUS |
549 (36.6) |
574 (41.1) |
0.01 |
| Remote site intervention |
440 (29.3) |
359 (25.7) |
0.03 |
| MV |
| Total stent length (mm) |
28 (23–33) |
24 (20–33) |
<0.001 |
| Maximal stent diameter (mm) |
3.0 (3.0–3.5) |
3.5 (3.0–3.5) |
<0.001 |
| SB |
(n=575) |
(n=260) |
|
| Total stent length (mm) |
20 (16–28) |
23 (18–28) |
0.03 |
| Maximal stent diameter (mm) |
2.75 (2.5–3.0) |
3.0 (2.75–3.5) |
0.005 |
| Procedural outcome |
| MV occlusion during procedure |
73 (4.9) |
50 (3.6) |
0.09 |
| SB occlusion during procedure |
158 (10.5) |
54 (3.9) |
<0.001 |
| Final TIMI flow grade <3 in MV |
10 (0.7) |
7 (0.5) |
0.56 |
| Final TIMI flow grade <3 in SB |
49 (3.3) |
14 (1.0) |
<0.001 |
| Angiographic success in MV* |
1,479 (98.5) |
1,380 (98.9) |
0.36 |
| Angiographic success in SB† |
1,022 (68.0) |
1,165 (83.5) |
<0.001 |
Data are presented as median (interquartile range) or n (%). All patients had 1 bifurcation lesion. *Defined as TIMI 3 flow and <30% residual stenosis. †Defined as TIMI 3 flow and <50% residual stenosis. FKB, final kissing balloon inflation; IVUS, intravascular ultrasound; LAD, left anterior descending; LCX, left circumflex; MV, main vessel; OM, obtuse marginal; RCA, right coronary artery; SB, side branch; TIMI, Thrombolysis in Myocardial Infarction. Other abbreviations as in Table 1.
During the procedure, MV occlusion occurred at a similar rate in the 2 groups, but SB occlusion occurred more frequently in patients with true bifurcation lesions than in those with non-true bifurcation lesions. To remedy SB occlusion, balloon angioplasty was performed in 127 lesions (59.9%), and a stent was implanted in 32 lesions (15.1%). Although there was no significant difference in the angiographic success in the MV between the groups, angiographic success in the SB was lower in patients with true bifurcation lesions than in those with non-true bifurcation lesions.
Quantitative Coronary Angiographic Analysis
Quantitative coronary angiographic data are presented in
Table 3. In patients with true bifurcation lesions, the angle between the MV and SB was more acute, the RD and MLD of each segment were smaller, the percent diameter stenosis of each segment was greater, and the lesion length of the MV was longer than in patients with non-true bifurcation lesions.
Table 3.
Quantitative Coronary Angiographic Analysis of Patients With True or Non-True Bifurcation Lesions Who Underwent PCI in COBIS II
| |
True bifurcation
(n=1,502) |
Non-true bifurcation
(n=1,395) |
P value |
| Pre-intervention |
| MV RD, mm |
3.0 (2.7–3.3) |
3.1 (2.8–3.4) |
<0.001 |
| SB RD, mm |
2.4 (2.3–2.6) |
2.5 (2.3–2.8) |
<0.001 |
| MV MLD, mm |
0.9 (0.6–1.3) |
1.0 (0.7–1.4) |
<0.001 |
| SB MLD, mm |
1.0 (0.7–1.2) |
1.8 (1.5–2.2) |
<0.001 |
| MV DS, % |
68.8 (59.0–79.6) |
66.1 (56.7–76.5) |
<0.001 |
| SB DS, % |
60.2 (51.7–71.0) |
27.5 (15.0–40.0) |
<0.001 |
| MV lesion length, mm |
17.8 (11.3–27.1) |
13.7 (8.4–22.3) |
<0.001 |
| SB lesion length, mm |
6.5 (3.4–12.3) |
– |
– |
| Bifurcation angle (°) |
57.8 (44.7–74.8) |
61.0 (46.9–80.0) |
<0.001 |
| Post-intervention |
| MV RD, mm |
3.0 (2.8–3.4) |
3.1 (2.8–3.5) |
0.001 |
| SB RD, mm |
2.4 (2.3–2.6) |
2.5 (2.3–2.8) |
<0.001 |
| MV MLD, mm |
2.6 (2.3–2.9) |
2.7 (2.4–3.0) |
<0.001 |
| SB MLD, mm |
1.7 (1.0–2.3) |
1.9 (1.4–2.3) |
<0.001 |
| MV DS, % |
13.8 (6.3–21.6) |
12.7 (5.4–21.2) |
0.04 |
| SB DS, % |
30.7 (9.5–56.4) |
27.8 (13.2–42.3) |
<0.001 |
Data are presented as median (interquartile range) or n (%). DS, diameter stenosis; MLD, minimum luminal diameter; RD, reference diameter. Other abbreviations as in Tables 1,2.
Clinical follow-up data were available for 96.3% of all patients. The median follow-up was 36 months (IQR, 24–52) in the non-true bifurcation group and 36 months (IQR, 25–51) in the true bifurcation group. Observed clinical outcomes according to the true bifurcation lesions are shown in
Figure 1
and
Table 4. The cumulative incidence of MACE was significantly higher in patients with true bifurcation lesions than in those with non-true bifurcation lesions (12.1% vs. 8.2%, P<0.001,
Figure 1A). The true bifurcation group had a significantly higher incidence of the composite of cardiac death or MI (3.8% vs. 2.4%, P=0.02,
Figure 1B), death (5.0 vs. 3.1%, P=0.01), definite or probable ST (1.4% vs. 0.4%, P=0.007,
Figure 1C), and TLR (9.1% vs. 6.7%, P=0.01,
Figure 1D). Definite ST occurred in 17 patients: 12 in the true bifurcation group and 5 in the non-true bifurcation group (Figure S1). All definite ST occurred in the sites of bifurcation stenting. In the multivariate analysis, the adjusted risks for MACE were significantly higher in patients with true bifurcation lesions than in those with non-true bifurcation lesions (adjusted hazard ratio [HR], 1.39; 95% confidence interval [CI], 1.08–1.80, P=0.01). True bifurcation lesions were also associated with a higher risk of the composite of cardiac death or MI (adjusted HR, 1.66; 95% CI, 1.03–2.67; P=0.04), death (adjusted HR, 1.56; 95% CI, 1.03–2.36, P=0.04), and definite or probable ST (adjusted HR, 2.82; 95% CI, 1.03–7.67; P=0.04).

Table 4.
Clinical Outcomes at the End of Follow-up of Patients With True or Non-True Bifurcation Lesions Who Underwent PCI in COBIS II
| |
True bifurcation
(n=1,502) |
Non-true bifurcation
(n=1,395) |
Unadjusted HR
(95% CI) |
P value |
Adjusted HR†
(95% CI) |
P value |
| MACE* |
181 (12.1) |
115 (8.2) |
1.52 (1.20–1.92) |
<0.001 |
1.39 (1.08–1.80) |
0.01 |
| Cardiac death or MI |
57 (3.8) |
33 (2.4) |
1.63 (1.06–2.50) |
0.03 |
1.66 (1.03–2.67) |
0.04 |
| Death |
75 (5.0) |
43 (3.1) |
1.63 (1.12–2.37) |
0.01 |
1.56 (1.03–2.36) |
0.04 |
| Cardiac death |
28 (1.9) |
14 (1.0) |
1.87 (0.98–3.55) |
0.06 |
2.08 (0.98–4.39) |
0.06 |
| MI |
31 (2.1) |
22 (1.6) |
1.33 (0.77–2.30) |
0.31 |
1.26 (0.69–2.32) |
0.46 |
| Definite or probable ST |
21 (1.4) |
6 (0.4) |
3.27 (1.32–8.10) |
0.01 |
2.82 (1.03–7.67) |
0.04 |
| TLR |
136 (9.1) |
94 (6.7) |
1.39 (1.07–1.81) |
0.02 |
1.24 (0.93–1.65) |
0.14 |
*MACE defined as a composite of cardiac death, MI, or TLR during follow-up. †Adjusted covariates included age, sex, acute coronary syndrome, diabetes mellitus, left ventricular dysfunction, left main bifurcation, type of stent used, 2-stent technique, FKB, use of IVUS, remote site intervention, MV stent length, RD of the MV, RD of the SB, and angle between the main branch and SB. CI, confidence interval; HR, hazard ratio; MACE, major adverse cardiac events; ST, stent thrombosis; TLR, target lesion revascularization. Other abbreviations as in Tables 1–3.
Independent predictors of MACE are presented in
Table 5. The 2-stent technique, left main bifurcation lesions, diabetes mellitus, as well as true bifurcation lesions were independently associated with an increased risk of MACE. Among components of the Medina classification, distal MV stenosis was the independent predictor of MACE, while proximal MV and SB stenosis were not significant factors of MACE. Conversely, use of FKB or second-generation DES was associated with lower risk of MACE.
Table 5.
Independent Predictors of MACE in Patients With True or Non-True Bifurcation Lesions Who Underwent PCI in COBIS II
| Variable |
Model 1* |
Model 2* |
| Adjusted HR† (95% CI) |
P value |
Adjusted HR† (95% CI) |
P value |
| True bifurcation (vs. non-true bifurcation) |
1.39 (1.08–1.80) |
0.01 |
|
|
| Pre-procedural %DS of the proximal MV ≥50% |
|
|
0.97 (0.76–1.23) |
0.79 |
| Pre-procedural %DS of the distal MV ≥50% |
|
|
2.16 (1.05–4.43) |
0.04 |
| Pre-procedural %DS of the SB ≥50% |
|
|
1.03 (0.80–1.33) |
0.81 |
| 2-stent technique (vs. 1-stent technique) |
2.06 (1.53–2.76) |
<0.001 |
2.27 (1.68–3.07) |
<0.001 |
| Left main lesions (vs. non-left main lesions) |
1.78 (1.29–2.45) |
<0.001 |
1.69 (1.21–2.36) |
0.002 |
| Diabetes mellitus |
1.33 (1.04–1.69) |
0.02 |
1.31 (1.03–1.67) |
0.03 |
| FKB |
0.69 (0.52–0.91) |
0.009 |
0.72 (0.55–0.95) |
0.02 |
| 2nd generation DES (vs. 1st generation DES) |
0.64 (0.41–0.99) |
0.05 |
0.64 (0.41–0.99) |
0.04 |
*Model 1 or 2 included the variables related to Medina classification: true bifurcation (vs. non-true bifurcation) or each component of the Medina classification, respectively. †Adjusted covariates included age, sex, acute coronary syndrome, left ventricular dysfunction, use of IVUS, remote site intervention, MV stent length, RD of the MV and SB, and the angle between the MV and SB. DES, drug-eluting stent. Other abbreviations as in Tables 1–4.
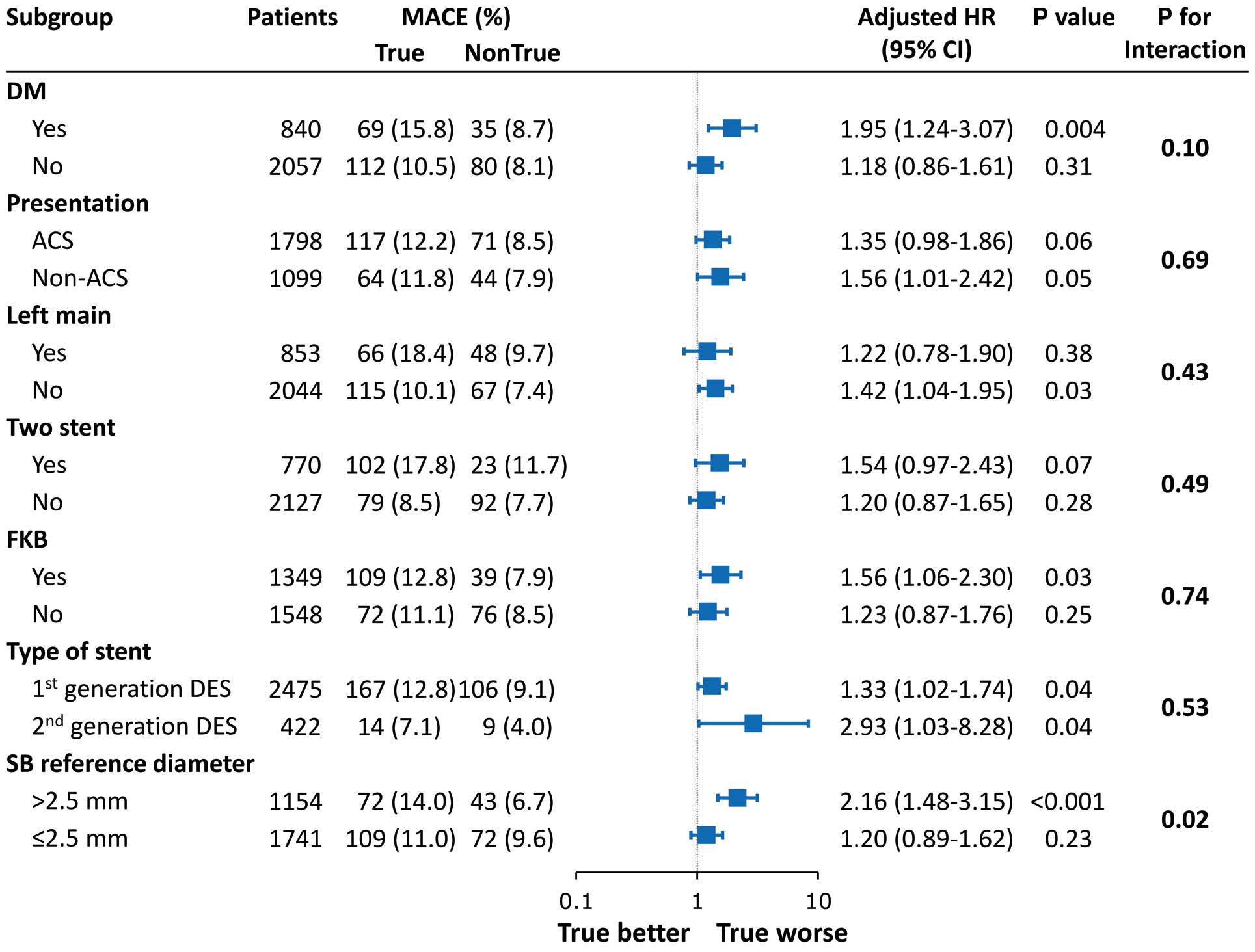
The adjusted risk of MACE was consistently higher in patients with true bifurcation lesions than in those with non-true bifurcation lesions across subgroups, regardless of diabetes, ACS, left main bifurcation, 2-stent technique, FKB, and stent type (Figure 2). There was significant interaction on the MACE rate according to SB RD (P for interaction=0.02). Although the MACE rate was not significantly different among patients with small SB RD, the MACE rate was higher in the true bifurcation group than in the non-true bifurcation group among patients with large SB RD.
Clinical Outcomes According to Medina Classification
The distribution, procedural events, and long-term clinical outcomes according to Medina classification in patients with bifurcation lesions are shown in
Table 6. The most common types of true and non-true bifurcation lesions were Medina (1.1.1) and Medina (0.1.0), respectively. The rarest type of coronary bifurcation lesion was Medina (0.0.1). During the procedure, SB occlusion occurred most frequently in patients with Medina (1.1.1). Among true bifurcation lesions, patients with Medina (1.1.1) and (1.0.1) had a higher prevalence of SB occlusion during the procedure than those with Medina (0.1.1) (11.5% vs. 7.4%, P=0.03).
Table 6.
Procedural and Clinical Outcomes According to Medina Classification of Bifurcation Lesion in Patients Undergoing PCI in COBIS II
| |
All |
1.1.1 |
0.1.1 |
1.0.1 |
1.1.0 |
1.0.0 |
0.1.0 |
0.0.1 |
P for trend |
| |
 |
|
| Frequency |
2,897 |
938 (32.4) |
353 (12.2) |
211 (7.3) |
427 (14.7) |
346 (11.9) |
508 (17.5) |
114 (3.9) |
|
| Procedural outcome |
| 2-stent technique |
770 (26.6) |
357 (38.1) |
159 (45.0) |
58 (27.5) |
59 (13.8) |
16 (4.6) |
48 (9.4) |
73 (64.0) |
<0.001 |
| FKB inflation |
1,349 (46.6) |
551 (58.7) |
197 (55.8) |
105 (49.8) |
167 (39.1) |
81 (23.4) |
165 (32.5) |
83 (72.8) |
<0.001 |
MV occlusion during
procedure |
123 (4.2) |
51 (5.4) |
15 (4.2) |
7 (3.3) |
27 (6.3) |
12 (3.5) |
10 (2.0) |
1 (0.9) |
0.002 |
SB occlusion during
procedure |
212 (7.3) |
111 (11.8) |
26 (7.4) |
21 (10.0) |
29 (6.8) |
18 (5.2) |
5 (1.0) |
2 (1.8) |
<0.001 |
Final TIMI flow grade
<3 in MV |
17 (0.6) |
9 (1.0) |
– |
1 (0.5) |
4 (0.9) |
2 (0.6) |
1 (0.2) |
– |
0.15 |
Final TIMI flow grade
<3 in SB |
63 (2.2) |
32 (3.4) |
7 (2.0) |
10 (4.7) |
7 (1.6) |
6 (1.7) |
1 (0.2) |
– |
<0.001 |
| Long-term outcome |
| Cardiac death or MI |
90 (3.1) |
42 (4.5) |
13 (3.7) |
2 (0.9) |
10 (2.3) |
6 (1.7) |
15 (3.0) |
2 (1.8) |
0.01 |
| Definite or probable ST |
27 (0.9) |
14 (1.5) |
7 (2.0) |
– |
2 (0.5) |
– |
4 (0.8) |
– |
0.006 |
| TLR |
230 (7.9) |
80 (8.5) |
41 (11.6) |
15 (7.1) |
35 (8.2) |
15 (4.3) |
35 (6.9) |
9 (7.9) |
0.03 |
| MACE |
296 (10.2) |
116 (12.4) |
49 (13.9) |
16 (7.6) |
42 (9.8) |
19 (5.5) |
44 (8.7) |
10 (8.8) |
<0.001 |
Abbreviations as in Tables 1,2,4.
Long-term clinical outcomes of patients with true bifurcation lesions showed different trends according to Medina classification (Figure S2). After adjustment of covariates, Medina (1.1.1) and (0.1.1) were associated with a higher risk of cardiac death or MI than Medina (1.0.1) (adjusted HR, 4.15; 95% CI, 1.01–17.1; P=0.05,
Table S1). However, patients with Medina (1.0.1) had similar long-term clinical outcomes compared with those with non-true bifurcation lesions (Table S2).
Discussion
In the present study, we compared the long-term clinical outcomes of patients with bifurcation lesions of 2 types, true vs. non-true, using data from a large, multicenter bifurcation registry. The main findings of this study are as follows: (1) compared with non-true bifurcation lesions, true bifurcation lesions were associated with unfavorable long-term clinical outcomes; (2) procedural and long-term clinical outcomes differed according to the type of bifurcation lesions; (3) true bifurcation, or especially distal MV stenosis, was the independent predictor of long-term clinical outcome; and (4) use of FKB and second-generation DES was associated with favorable clinical outcomes.
True Bifurcation vs. Non-True Bifurcation
Although several classifications of bifurcation lesions have been proposed, none has gained full acceptance. The Medina classification is a straightforward system that has been popularly received.8
However, prior randomized studies have included small to medium sample sizes and inadequately evaluated clinical outcomes according to angiographic distribution in patients with coronary bifurcation lesions, especially comparing true and non-true bifurcations.1–3
Although some studies have evaluated the value of the angiographic distribution of bifurcation lesions, these have had small sample sizes or contained results with mixed use of bare-metal stents and DES.16,17
Therefore, we sought to investigate procedural and long-term clinical outcomes according to angiographic distribution in patients with coronary bifurcation lesions using data from the COBIS II registry.
It is well-known that patients with true bifurcation lesions are at higher risk for procedural complications than patients with other types of bifurcation lesions.18
However, no trial has demonstrated that patients with true bifurcation lesions actually have unfavorable long-term outcomes compared with patients with non-true bifurcation lesions. In the Arterial Revascularization Therapies Study part II, there was no difference in any of the endpoints between the true bifurcation group and the non-true bifurcation group.17
In the present study, we report that patients with true bifurcation lesions had worse long-term clinical outcomes than those with non-true bifurcation lesions. The patients with true bifurcation lesions had a higher prevalence of unfavorable factors, including left ventricular systolic dysfunction, ACS at presentation,19
and nonuse of IVUS.20
After adjustment for statistically significant covariates, the risks for MACE and the composite of cardiac death or MI were significantly higher in patients with true bifurcation lesions. Notably, the risk of ST was significantly higher in patients with true bifurcation lesions. The exact cause of the higher risk of ST in true bifurcation lesions is unknown, although ST is a complex process that may be a culmination of device, patient, lesion, and procedural factors.21
True bifurcation lesions were more complex and had inferior results after intervention than non-true bifurcation lesions. In the post-intervention results from quantitative coronary angiographic analysis, the true bifurcation lesions had smaller diameter, longer lesion length, and more severe percent diameter stenosis than non-true bifurcation lesions.
Within True Bifurcation Lesions
During the procedure, SB occlusion occurred more frequently in patients with Medina (1.1.1) and (1.0.1) than those with Medina (0.1.1) lesions. Proximal MV stenosis combined with SB ostial stenosis might be more important for SB occlusion than distal MV stenosis combined with SB ostial stenosis. This hypothesis was well-supported by our recently published study.12
Among true bifurcation lesions, Medina (1.1.1) and (0.1.1) were associated with a higher risk of cardiac death or MI than Medina (1.0.1). Although Medina (1.0.1) was classified with the true bifurcation lesions and had a high prevalence of SB occlusion, patients with Medina (1.0.1) lesions had similar long-term clinical outcomes to those with non-true bifurcation lesions. These findings are consistent with the results of a previous study regarding outcomes according to bifurcation lesion type.22
One possible explanation is carina shift, which is influenced by distal MV lumen expansion, may cause SB narrowing after MV stent implantation, and might be followed by worse outcomes.23
On multivariable analysis of our registry, distal MV stenosis was the independent predictor of long-term outcome. In addition, the 2-stent technique was used less frequently compared with the other true bifurcation lesions. Therefore, it is possible that patients with Medina (1.0.1) showed favorable long-term outcomes as a result of lack of distal MV stenosis and less use of the 2-stent technique.
Predictors of MACE: Comparing the COBIS I and II Registries
The present study based on the COBIS II registry and our previous report from the COBIS I registry show conflicting results in terms of the independent predictors of MACE.15
First, true bifurcation lesions were not independent predictors of MACE in the COBIS I registry, whereas patients with true bifurcation lesions were associated with worse clinical outcomes in the COBIS II registry. It is possible that these findings result from different inclusion criteria. The COBIS II registry included a larger size of SB compared with the COBIS I registry. In the subgroup analysis, there was significant interaction on the MACE rate according to SB RD (P for interaction=0.02). As a result, true bifurcation lesions were independent predictor of MACE in the COBIS II registry, which included a larger size of SB than the COBIS I registry. Second, FKB was a risk factor of MACE in the COBIS I registry, but was associated with favorable clinical outcomes in the COBIS II registry. The benefit of FKB during the 1-stent technique has not been established.24–27
The possible explanation for the different effect of FKB during the 1-stent technique between the COBIS I and II registries was proposed in a recently published report; favorable outcomes of patients were mainly driven by the reduction of TLR in MV, as a result of an increase in the MLD of MV acquired by FKB during the 1-stent technique. Finally, the use of second-generation DES was associated with favorable outcomes in multivariable models.28
Therefore, it is possible that meticulous FKB and use of second-generation DES might improve the clinical outcomes of patients with true bifurcation lesions. Further randomized study regarding the appropriate treatment for true bifurcation lesions is required.
Study Limitations
First, this was a non-randomized, observational study, which may have significantly affected the results because of confounding factors. The treatment strategies and stent types were selected by the operator. Some baseline and angiographic characteristics were unfavorable in the true bifurcation group compared with the non-true bifurcation group, which may have contributed to the differences in adverse outcomes between the 2 groups. Therefore, we tried to reduce potential confounding using adjusted Cox regression analysis. In addition, tests for interaction based on multivariate Cox models were used to assess the heterogeneity of effects of true bifurcation lesions across different subgroups. Because we conducted a multivariate analysis using the same covariates for all outcomes, the overfitting problems of a Cox hazard model could not be avoided for rare outcomes, such as definite or probable ST. Another limitation is that large numbers of patients were treated with first-generation DES, which are associated with a higher incidence of adverse clinical events compared with the newer-generation DES. Adequately powered registries or randomized trials using newer-generation DES are needed to compare the effect of stent type. Finally, IVUS data for evaluating vessel size, plaque distribution, stent underexpansion, stent malapposition, or incomplete stent coverage of SB ostium bifurcation stenting were not available in the COBIS II registry.
Conclusions
In a large, multicenter, real-world registry, true bifurcation lesions were associated with higher risks of cardiovascular events compared with non-true bifurcation lesions. Procedural and long-term clinical outcomes differed according to the type of bifurcation lesion. True bifurcation, especially distal MV stenosis, was an independent predictor of long-term clinical outcome, but the use of FKB and second-generation DES was associated with favorable clinical outcome. These findings should be considered in future bifurcation studies.
Disclosures
None declared.
Grant Support
This work was supported by the Korean Society of Interventional Cardiology, Seoul, Republic of Korea.
Supplementary Files
Supplementary File 1
Figure S1.
Kaplan-Meier curve for definite or probable stent thrombosis for median 3-year follow-up.
Figure S2.
Kaplan-Meier curves for clinical outcomes according to Medina classification among true bifurcation lesions.
Table S1.
Clinical outcomes for Medina (1.1.1)/(0.1.1) and Medina (1.0.1) bifurcation lesions in patients undergoing PCI in COBIS II
Table S2.
Clinical outcomes between Medina (1.0.1) and non-true bifurcation lesions in patients undergoing PCI in COBIS II
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-15-0264
References
- 1.
Colombo A, Bramucci E, Sacca S, Violini R, Lettieri C, Zanini R, et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: The CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) Study. Circulation 2009; 119: 71–78.
- 2.
Hildick-Smith D, de Belder AJ, Cooter N, Curzen NP, Clayton TC, Oldroyd KG, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: The British Bifurcation Coronary Study: Old, new, and evolving strategies. Circulation 2010; 121: 1235–1243.
- 3.
Maeng M, Holm NR, Erglis A, Kumsars I, Niemela M, Kervinen K, et al. Long-term results after simple versus complex stenting of coronary artery bifurcation lesions: Nordic Bifurcation Study 5-year follow-up results. J Am Coll Cardiol 2013; 62: 30–34.
- 4.
Niccoli G, Ferrante G, Porto I, Burzotta F, Leone AM, Mongiardo R, et al. Coronary bifurcation lesions: To stent one branch or both? A meta-analysis of patients treated with drug eluting stents. Int J Cardiol 2010; 139: 80–91.
- 5.
Behan MW, Holm NR, Curzen NP, Erglis A, Stables RH, de Belder AJ, et al. Simple or complex stenting for bifurcation coronary lesions: A patient-level pooled-analysis of the Nordic Bifurcation Study and the British Bifurcation Coronary Study. Circ Cardiovasc Interv 2011; 4: 57–64.
- 6.
Gao XF, Zhang YJ, Tian NL, Wu W, Li MH, Bourantas CV, et al. Stenting strategy for coronary artery bifurcation with drug-eluting stents: A meta-analysis of nine randomised trials and systematic review. EuroIntervention 2014; 10: 561–569.
- 7.
Medina A, Suarez de Lezo J, Pan M. A new classification of coronary bifurcation lesions. Rev Esp Cardiol 2006; 59: 183 (in Spanish).
- 8.
Thomas M, Hildick-Smith D, Louvard Y, Albiero R, Darremont O, Stankovic G, et al. Percutaneous coronary intervention for bifurcation disease: A consensus view from the first meeting of the European Bifurcation Club. EuroIntervention 2006; 2: 149–153.
- 9.
Zlotnick DM, Ramanath VS, Brown JR, Kaplan AV. Classification and treatment of coronary artery bifurcation lesions: Putting the Medina classification to the test. Cardiovasc Revasc Med 2012; 13: 228–233.
- 10.
Latib A, Colombo A. Bifurcation disease: What do we know, what should we do? JACC Cardiovasc Interv 2008; 1: 218–226.
- 11.
Lansky AJ, Dangas G, Mehran R, Desai KJ, Mintz GS, Wu H, et al. Quantitative angiographic methods for appropriate end-point analysis, edge-effect evaluation, and prediction of recurrent restenosis after coronary brachytherapy with gamma irradiation. J Am Coll Cardiol 2002; 39: 274–280.
- 12.
Hahn JY, Chun WJ, Kim JH, Song YB, Oh JH, Koo BK, et al. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: Results from the COBIS II Registry (COronary BIfurcation Stenting). J Am Coll Cardiol 2013; 62: 1654–1659.
- 13.
Yang JH, Song YB, Song PS, Hahn JY, Choi SH, Choi JH, et al. Impact of coronary bifurcation angle on clinical outcomes after percutaneous coronary intervention in real-world practice: Results from the COBIS registry. Cardiology 2012; 122: 216–224.
- 14.
Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 2007; 115: 2344–2351.
- 15.
Gwon HC, Choi SH, Song YB, Hahn JY, Jeong MH, Seong IW, et al. Long-term clinical results and predictors of adverse outcomes after drug-eluting stent implantation for bifurcation lesions in a real-world practice: The COBIS (Coronary Bifurcation Stenting) registry. Circ J 2010; 74: 2322–2328.
- 16.
Todaro D, Burzotta F, Trani C, Brugaletta S, De Vita M, Talarico GP, et al. Evaluation of a strategy for treating bifurcated lesions by single or double stenting based on the Medina classification. Rev Esp Cardiol 2009; 62: 606–614.
- 17.
Tsuchida K, Colombo A, Lefevre T, Oldroyd KG, Guetta V, Guagliumi G, et al. The clinical outcome of percutaneous treatment of bifurcation lesions in multivessel coronary artery disease with the sirolimus-eluting stent: Insights from the Arterial Revascularization Therapies Study part II (ARTS II). Eur Heart J 2007; 28: 433–442.
- 18.
Al Suwaidi J, Berger PB, Rihal CS, Garratt KN, Bell MR, Ting HH, et al. Immediate and long-term outcome of intracoronary stent implantation for true bifurcation lesions. J Am Coll Cardiol 2000; 35: 929–936.
- 19.
Sang Song P, Ryeol Ryu D, Choi SH, Yang JH, Song YB, Hahn JY, et al. Impact of acute coronary syndrome classification and procedural technique on clinical outcomes in patients with coronary bifurcation lesions treated with drug-eluting stents. Clin Cardiol 2012; 35: 610–618.
- 20.
Kim JS, Hong MK, Ko YG, Choi D, Yoon JH, Choi SH, et al. Impact of intravascular ultrasound guidance on long-term clinical outcomes in patients treated with drug-eluting stent for bifurcation lesions: Data from a Korean multicenter bifurcation registry. Am Heart J 2011; 161: 180–187.
- 21.
Honda Y, Fitzgerald PJ. Stent thrombosis: An issue revisited in a changing world. Circulation 2003; 108: 2–5.
- 22.
Lefevre T, Louvard Y, Morice MC, Dumas P, Loubeyre C, Benslimane A, et al. Stenting of bifurcation lesions: Classification, treatments, and results. Cathet Cardiovasc Interv 2000; 49: 274–283.
- 23.
Xu J, Hahn JY, Song YB, Choi SH, Choi JH, Lu C, et al. Carina shift versus plaque shift for aggravation of side branch ostial stenosis in bifurcation lesions: Volumetric intravascular ultrasound analysis of both branches. Circ Cardiovasc Interv 2012; 5: 657–662.
- 24.
Hariki H, Shinke T, Otake H, Shite J, Nakagawa M, Inoue T, et al. Potential benefit of final kissing balloon inflation after single stenting for the treatment of bifurcation lesions: Insights from optical coherence tomography observations. Circ J 2013; 77: 1193–1201.
- 25.
Yamawaki M, Muramatsu T, Kozuma K, Ito Y, Kawaguchi R, Kotani J, et al. Long-term clinical outcome of a single stent approach with and without a final kissing balloon technique for coronary bifurcation. Circ J 2014; 78: 110–121.
- 26.
Niemela M, Kervinen K, Erglis A, Holm NR, Maeng M, Christiansen EH, et al. Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: The Nordic-Baltic Bifurcation Study III. Circulation 2011; 123: 79–86.
- 27.
Gwon HC, Hahn JY, Koo BK, Song YB, Choi SH, Choi JH, et al. Final kissing ballooning and long-term clinical outcomes in coronary bifurcation lesions treated with 1-stent technique: Results from the COBIS registry. Heart 2012; 98: 225–231.
- 28.
Cho Y, Koo BK, Song YB, Hahn JY, Choi SH, Gwon HC, et al. Comparison of the first- and second-generation limus-eluting stents for bifurcation lesions from a Korean multicenter registry. Circ J 2015; 79: 544–552.