Article ID: CJ-15-0462
Article ID: CJ-15-0462
Background: To investigate the relationship between age and both short- and long-term outcomes of off-pump coronary bypass grafting (OPCAB).
Methods and Results: The 780 patients undergoing OPCAB were divided into 3 groups: 262 aged <65 years (young), 329 aged 65–74 years (early elderly), and 189 aged >75 years (late elderly), and retrospectively analyzed. The follow-up rate was 94.9%, and mean follow-up period was 5.6±3.4 years. In-hospital mortality rates were similar among the groups (0.8% in young, 1.2% in early elderly, and 1.1% in late elderly; P=0.862). In logistic regression analysis, the risk factor for predicting major complications was the New York Heart Association (NYHA) classification (odds ratio: 1.555, P=0.001), and not age. The 10-year estimated rates free from cardiac death (89.6±3.2, 95.0±2.1, and 96.5±2.1%, log rank, P=0.16) and cardiac events (71.8±3.8, 66.8±4.3, and 59.9±7.7%, P=0.61) were not significantly different among the groups. In multivariate Cox models, independent risk factors predicting cardiac events were the NYHA classification (hazard ratio (HR): 1.265, P=0.009), and ejection fraction (HR: 0.986, P=0.016), but not age (young HR: 1.0, early elderly HR: 1.276; P=0.210, late elderly HR: 0.910; P=0.707).
Conclusions: Both short- and long-term cardiac outcomes of OPCAB are not influenced by age at operation.
Rapid aging of the population results in increasing need to perform coronary artery bypass grafting (CABG) in elderly patients.1 Advanced age has been reported as a risk factor in cardiovascular surgery because of preoperative comorbidities such as chronic kidney disease, cerebrovascular disease, and impaired respiratory function.2,3 Among the elderly, those aged 65–74 are classified as the early elderly and those older than 75 as the late elderly. In general, the elderly require longer-term care in hospital than do younger people. In addition, the late elderly require more frequent long-term care than the early elderly, because they have multiple comorbidities.4 Off-pump CABG (OPCAB) is a less invasive technique without the need for cardiopulmonary bypass (CPB), and is expected to reduce morbidity and mortality in such high-risk patients.5–11 Japan is well-known for having one of the most rapidly aging populations in the world, where the rate of the elderly undergoing CABG is more than 50% in those aged over 70, and 12% are older than 80 years. The high rate of OPCAB is another characteristic of Japan. The rate was over 50% in 2003, and since 2004 it has been greater than 60% of isolated CABG cases.12 However, both the short- and long-term results of isolated OPCAB, especially for the elderly, remain unclear.13,14 The aim of this study was to compare the short- and long-term clinical outcomes of patients who underwent isolated OPCAB based on age stratification.
This study was approved by the Institutional Review Board of Kyoto Prefectural University of Medicine. Individual consent was obtained from each patient. Between July 1997 and December 2012, a total of 1,177 consecutive patients underwent isolated CABG performed by 2 surgeons (H.Y. and K.D.). Of these, 954 patients underwent OPCAB, and the 780 patients who had at least 2 distal anastomoses in the left coronary artery area were included in this study. Patients with double-vessel disease without 2 distal anastomoses in the left coronary area (52 cases), single-vessel disease (91 cases), or redo sternotomy (31 cases) were excluded from this study. The 262 patients younger than 65 years were defined as the young group, the 329 patients aged 65–74 were defined as the early elderly group, and the 189 patients older than 75 years were defined as the late elderly group. Since January 2000, we have performed OPCAB as the first choice for surgical revascularization regardless of the level of urgency.
Revascularization StrategyOur strategy for multivessel revascularization was to revascularize the LAD by in-situ internal thoracic artery (ITA) grafting, mostly achieved by the right ITA. The left circumflex artery was revascularized by another ITA or the great saphenous vein (SVG). The right coronary area (RCA) was revascularized by the SVG or gastroepiploic artery (GEA). The GEA was used in patients with a markedly calcified ascending aorta and severe stenosis (>90%) of the proximal RCA. We routinely performed head and neck MRI to assess the preoperative risk of cerebrovascular disease.15 In cases of severe carotid stenosis, we used intra-aortic balloon pumping (IABP) to avoid systemic low blood pressure during heart positioning and subsequent hemodynamic cerebral infarction. Computed tomography was carried out to preoperatively assess calcification of the aorta.
Surgical TechniquesAll surgical procedures were performed through a median sternotomy with an off-pump technique. The ITAs were harvested in a skeletonized fashion using a harmonic scalpel (Ethicon Endo-Surgery; Cincinnati, OH, USA).16 After systemic heparinization (1 mg/kg), the ITAs were transected distally at the bifurcation. All arterial conduits were dilated by papaverine hydrochloride (0.3 mg/ml). The SVG was harvested by direct exposure. Proximal anastomosis was performed using anastomotic devices, including the Novare Enclose device (Novare Surgical Systems; Cupertino, CA, USA) and the HEARTSTRING Proximal Seal System (Guidant Corporation; Santa Clara, CA, USA). Before proximal anastomosis, epi-aortic echocardiography was performed in all cases. If mobile plaque or calcification was detected, an aorta-non-touch technique was adopted with in-situ grafts. An intracoronary shunt tube (Anastaflow; Edwards Lifescience; Irvine, CA, USA) was routinely used. The ITA was anastomosed with 8-0 polypropylene. Distal anastomosis of other grafts was performed with 7-0 or 8-0 polypropylene. To evaluate the graft function, a transit time flow trace (MediStim VQ-1101, MediStim ASA, Oslo, Norway) was performed after each distal anastomosis. If the flow pattern was not favorable, the SPY system (Novadaq Technologies Inc, Toronto, Canada) was used to visualize the anastomotic site.
Endpoints and DefinitionsThe operative data and incidence of in-hospital complications were extracted from the hospital records. The duration of follow-up was calculated from the date of the operation to that of death or the last direct contact by telephone or personal interview. Follow-up was performed by direct patient contact or telephone and a postcard survey each year. The endpoints were overall death, cardiac death, and cardiac events. Cardiac events were a composite outcome and defined as: (1) cardiac death caused by arrhythmia, myocardial infarction (MI), heart failure, or sudden death, (2) any coronary re-intervention including CABG or percutaneous coronary intervention (PCI), (3) readmission for congestive heart failure, and (4) lethal ventricular arrhythmia requiring resuscitation. A respiratory complication was defined as prolonged ventilation longer than 72 h and re-intubation. Major in-hospital complications included reoperation, respiratory complications, newly required dialysis, mediastinitis, and stroke. Postoperative renal failure was defined as newly required hemodialysis, or a postoperative estimated glomerular filtration rate (eGFR) below 50% of preoperative level.17 Perioperative MI was defined as an elevation of creatinine kinase-MB to >100 IU/L and the appearance of new Q waves. Low output syndrome (LOS) was defined as the postoperative need for IABP, extracorporeal membrane oxygenator use, or >5 µg·kg–1·min–1 catecholamine for longer than 24 h. Incomplete revascularization was defined as the existence of any non-revascularized vessel with >1 mm diameter showing more than 50% stenosis. Mitral regurgitation (MR) was examined by transthoracic echocardiography and divided into 4 grades: none (0), mild (1+), moderate (2+), moderate to severe (3+), and severe (4+). The degree of MR was diagnosed by more than 2 in-house cardiologists. Preoperative diabetes mellitus (DM) was defined as receiving insulin, oral medications, diet therapy, or exercise therapy.
Statistical AnalysisContinuous variables are expressed as the mean±standard deviation. Comparisons of clinical characteristics and outcomes among groups were performed using the Kruskal-Wallis test for skewed variables, and the χ2 test for categorical variables. Kaplan-Meier survival curves were used to evaluate the long-term results. The log-rank test was used to compare survival curves. Predictors of peri- and postoperative outcome events were analyzed using uni- and multivariate logistic regression models. The odds ratios (OR) and 95% confidence intervals (CI) for the association between patients’ backgrounds and major complications were estimated. Independent predictors of overall survival and the freedom from cardiac events rate were determined using Cox proportional hazard models, to be expressed as hazard ratios (HR) and 95% CI. Multivariate analyses were performed with a stepwise downward selection model into which was entered each variable with a probability value of less than 0.20 in the univariate analysis. Trends in the associations of interest were evaluated by a linear regression model with ordinal scores (0, 1, and 2) assigned to the categories of respective covariates. Age groups were categorized by tertile. Multivariate regression analysis was then used to examine the independent association with each covariation on a continuous scale.18 Results were considered significant at P<0.05. All statistical calculations were performed using SPSS 22.0 software (SPSS Inc, Chicago, IL, USA).
Patients’ background and intraoperative details are summarized in Table 1. Higher rates of male sex (89.3% in the young group, 77.8% in the early elderly group, and 70.4% in the late elderly group), obesity, previous PCI (33.7, 25.7, and 21.9%, respectively; P=0.0015), hyperlipidemia (60.9, 55.8, and 43.7%, respectively; P=0.009), and smoking (62.8, 56.6, 38.5%, respectively; P<0.001) were found in the young group. On the other hand, a higher New York Heart Association (NYHA) classification (1.7±0.8, 1.7±0.8, and 1.9±0.9, respectively; P=0.011), higher rate of left main trunk stenosis (40.9%, 45.1%, and 53.4%, respectively; P<0.030), and lower eGFR (66.2±29.0, 59.9±24.0, and 57.9±27.4 ml/min/1.73 m2, respectively, P<0.001) were observed in the late elderly group. The higher rates of MR above a moderate severity, atrial fibrillation (AF), and lower rate of patients on hemodialysis were investigated in the late elderly group, but they were not significant. The rates of DM (51.9%, 56.7%, and 45.0%, respectively; P=0.036) and chronic lung disease, mean ejection fraction (EF) (59.4, 62.5±14.1, and 59.9±14.4, respectively; P<0.001), and the number of diseased vessels were higher in the early elderly group.
| All (n=780) |
Young (n=262) |
Early elderly (n=329) |
Late elderly (n=189) |
P value | |
|---|---|---|---|---|---|
| Age, years | 67.5±9.0 | 57.4±5.9 | 69.3±2.7 | 78.5±3.2 | <0.001 |
| Male | 623 (79.9) | 234 (89.3) | 256 (77.8) | 133 (70.4) | <0.001 |
| BMI, kg/m2 | 23.4±3.4 | 24.3±3.9 | 23.1±3.1 | 22.8±3.1 | <0.001 |
| EF, % | 60.9±14.0 | 59.4±13.4 | 62.5±14.1 | 59.9±14.4 | 0.033 |
| EF <35% | 33 (4.3) | 13 (5.0) | 10 (3.1) | 10 (5.4) | 0.367 |
| Diseased vessels | 2.4±0.8 | 2.4±0.8 | 2.5±0.8 | 2.3±0.8 | 0.037 |
| LMT ≥50% | 355 (45.7) | 106 (40.9) | 148 (45.1) | 101 (53.4) | 0.030 |
| NYHA class, mean | 1.8±0.8 | 1.7±0.8 | 1.7±0.8 | 1.9±0.9 | 0.011 |
| Previous PCI | 208 (27.5) | 86 (33.7) | 82 (25.7) | 40 (21.9) | 0.015 |
| Previous MI | 314 (42.8) | 114 (45.4) | 122 (40.3) | 78 (43.6) | 0.463 |
| Acute MI | 15 (2.0) | 2 (0.8) | 10 (3.9) | 3 (1.7) | 0.110 |
| MR ≥2 | 63 (8.1) | 16 (6.1) | 25 (7.6) | 22 (11.6) | 0.095 |
| AS ≥mild | 20 (2.6) | 2 (0.8) | 10 (3.0) | 8 (4.2) | 0.023 |
| Diabetes mellitus | 407 (52.3) | 136 (51.9) | 186 (56.7) | 85 (45.0) | 0.036 |
| Hypertension | 534 (70.4) | 172 (67.2) | 230 (72.1) | 132 (72.1) | 0.373 |
| Hyperlipidemia | 414 (54.6) | 156 (60.9) | 178 (55.8) | 80 (43.7) | 0.009 |
| Smoking | 408 (54.3) | 159 (62.8) | 179 (56.6) | 70 (38.5) | <0.001 |
| COPD | 27 (3.6) | 3 (1.2) | 17 (5.3) | 7 (3.8) | 0.027 |
| eGFR, ml/min/1.73 m2 | 61.5±26.8 | 66.2±29.0 | 59.9±24.0 | 57.9±27.4 | <0.001 |
| eGFR ≤40 ml/min/1.73 m2 | 138 (17.7) | 40 (15.3) | 59 (17.9) | 39 (20.6) | 0.344 |
| Cre, mg/dl | 1.3±1.6 | 1.5±1.9 | 1.3±1.5 | 1.2±1.1 | 0.880 |
| Cre ≥1.5 mg/dl | 116 (14.9) | 39 (14.9) | 52 (15.8) | 25 (13.2) | 0.730 |
| Hemodialysis | 57 (7.3) | 23 (8.8) | 27 (8.2) | 7 (3.7) | 0.087 |
| PAD | 95 (12.5) | 28 (10.9) | 44 (13.8) | 23 (12.6) | 0.590 |
| Stroke | 79 (10.1) | 21 (8.0) | 41 (12.5) | 17 (9.0) | 0.172 |
| AF | 36 (4.9) | 7 (2.8) | 16 (5.2) | 13 (7.3) | 0.100 |
Data are number (%) or mean±standard deviation. AF, atrial fibrillation; AS, aortic stenosis; BMI, body mass index; CABG, coronary artery bypass grafting; COPD, chronic obstructive pulmonary disease; Cre, creatinine; EF, ejection fraction; eGFR, estimated glomerular filtration rate; LMT, left main trunk; MI, myocardial infarction; MR, mitral regurgitation; NYHA, New York Heart Association; PAD, peripheral arterial disease; PCI, percutaneous coronary intervention.
The average number of distal anastomoses (3.6±1.1, 3.5±1.0, and 3.1±0.8, respectively; P<0.001), rate of BITA grafting (86.6%, 81.8%, and 67.7%, respectively; P<0.001), and rate of GEA grafting (27.1%, 10.6%, and 1.6%, respectively; P<0.001) were significantly higher in the young group. The rates of complete revascularization were not significantly different among the groups (93.9%, 89.4%, and 89.4%, respectively; P=0.118). The rates of SVG grafting (46.9%, 53.9%, and 72.0%, respectively; P<0.001) and intraoperative IABP usage (14.9%, 12.2%, and 25.1%, respectively; P<0.001) were significantly higher in the late elderly group. The rate of using proximal anastomotic devices was 78.3% in total, being significantly higher in the young group.
In-Hospital OutcomeThe postoperative results are summarized in Table 2. In the early results, there were a total of 8 in-hospital deaths (1.0%), but the rate of in-hospital mortality was not significantly different among the groups (0.8%, 1.2%, and 1.1%, respectively; P=0.862). The late elderly group required more frequent transfusion (26.3%, 43.3%, and 55.0%, respectively; P<0.001), and prolonged ventilation (1.9%, 1.5%, and 5.3%, respectively; P=0.024). No significant difference was noted in the incidence of re-exploration for bleeding (1.6%, 1.9%, and 1.1%, respectively; P=0.797), perioperative stroke (0.8%, 1.8%, and 1.1%, respectively; P=0.498), renal failure (4.3% vs. 3.0% vs. 3.4%, P=0.712), perioperative MI (3.1% vs. 4.3% vs. 3.7%, P=0.745), LOS (6.5%, 4.3%, and 5.8%, respectively; P=0.468), or mediastinitis (2.7%, 1.8%, and 0.5%, respectively; P=0.239). A shorter hospital stay (17.8±15.2, 21.4±32.6, and 21.5±15.5, respectively; P=0.961) was observed in the young group. The incidence of postoperative AF was lower in the young group, but there was no difference between the early elderly and elderly groups. In the subgroup analysis, patients aged over 80 years showed excellent early outcomes (Table S1). Complete revascularization was achieved in more than 90% of the patients. The rates of hypertension, peripheral artery disease, MR, and using intraoperative IABP were relatively high. However, there were no cases of hospital death, stroke, or mediastinitis.
| All (n=780) |
Young (n=262) |
Early elderly (n=329) |
Late elderly (n=189) |
P value | |
|---|---|---|---|---|---|
| Off-pump | 780 (100) | 262 (100) | 329 (100) | 189 (100) | 1.000 |
| Emergency | 37 (4.7) | 10 (3.8) | 14 (4.3) | 13 (6.9) | 0.276 |
| No. of distal anastomoses | 3.4±1.0 | 3.6 ±1.1 | 3.5±1.0 | 3.1±0.8 | <0.001 |
| Bilateral ITA | 624 (80.0) | 227 (86.6) | 269 (81.8) | 128 (67.7) | <0.001 |
| LITA | 748 (95.9) | 255 (97.3) | 312 (94.8) | 181 (95.8) | 0.314 |
| RITA | 650 (83.3) | 232 (88.5) | 284 (86.3) | 135 (52.6) | <0.001 |
| SVG | 455 (58.3) | 123 (46.9) | 196 (53.9) | 136 (72.0) | <0.001 |
| GEA | 109 (14.0) | 71 (27.1) | 35 (10.6) | 3 (1.6) | <0.001 |
| Complete revascularization | 709 (90.9) | 246 (93.9) | 294 (89.4) | 169 (89.4) | 0.118 |
| Proximal suture device | 611 (78.3) | 222 (84.7) | 251 (76.3) | 138 (73.0) | 0.006 |
| IABP | 126 (16.3) | 39 (14.9) | 40 (12.2) | 47 (25.1) | <0.001 |
| Transfusion | 315 (40.4) | 59 (26.3) | 142 (43.2) | 104 (55.0) | <0.001 |
| AF | 163 (22.2) | 40 (16.1) | 81 (26.1) | 42 (23.7) | 0.015 |
| Stroke | 10 (1.3) | 2 (0.8) | 6 (1.8) | 2 (1.1) | 0.498 |
| Renal failure | 63 (8.1) | 22 (8.4) | 24 (7.3) | 17 (9.0) | 0.770 |
| Perioperative MI | 29 (3.7) | 8 (3.1) | 14 (4.3) | 7 (3.7) | 0.745 |
| LOS | 42 (5.4) | 17 (6.5) | 14 (4.3) | 11 (5.8) | 0.468 |
| Mediastinitis | 14 (1.8) | 7 (2.7) | 6 (1.8) | 1 (0.5) | 0.239 |
| Hospital stay, days | 20.2±24.2 | 17.8±15.2 | 21.4±32.6 | 21.5±15.5 | <0.001 |
| Major complications | 95 (12.2) | 24 (9.2) | 41 (12.5) | 30 (15.9) | 0.097 |
| In-hospital mortality | 8 (1.0) | 2 (0.8) | 4 (1.2) | 2 (1.1) | 0.862 |
Data are number (%) or mean±standard deviation. GEA, gastroepiploic artery; IABP, intra-aortic balloon pump; ITA, internal thoracic artery; LITA, left ITA; LOS, low output syndrome; RITA, right ITA; SVG, saphenous vein graft. Other abbreviations as in Table 1.
The following 9 variables with a probability value of less than 0.20 in the univariate analysis were entered into logistic regression models: group (young, early elderly, and late elderly), emergency status, preoperative EF, preoperative eGFR, hyperlipidemia, NYHA classification, acute MI, complete revascularization, and preoperative stroke. In the multivariate logistic regression analysis of developing major in-hospital complications, the NYHA classification at operation was an independent risk factor (OR: 1.571, P<0.001) (Table 3). The OR of age stratification increased with aging, but showed a borderline significance (young group: reference; early elderly group: OR: 1.473, P=0.143; late elderly group: OR: 1.649, P=0.076). In addition, the trend P-value for age stratification was calculated and showed a near-significant trend (P=0.076) (Table 3; bottom-most line).
| β coefficient | Adjusted OR | (95% CI) | P value | |
|---|---|---|---|---|
| NYHA | 0.451 | 1.571 | 1.253–1.968 | <0.001 |
| Age group (years) | – | – | – | 0.185 |
| <65 | – | 1 | – | – |
| 65–74 | 0.387 | 1.473 | 0.877–2.473 | 0.143 |
| ≥75 | 0.500 | 1.649 | 0.949–2.867 | 0.076 |
| Trend P=0.076 | ||||
Trend P value shows the trend of the association with ordinal scores (0, 1, and 2) assigned to categories of the factor. CI, confidence interval; OR, odds ratio. Other abbreviations as in Table 1.
The follow-up rate was 94.9%, and the mean follow-time period was 5.6±3.4 years. Long-term causes of death are summarized in Table 4. In young patients, cardiac death was the main cause of mortality (42.4%). However, the rate of cardiac death was 18.6% in the early elderly group and 18.2% in the late elderly group. The rate of freedom from cardiac events was not significantly different among the groups (Figure 1). The 5- and 10-year estimated cardiac event-free rates were 79.7±2.9% in the young group, 79.1±2.5% in the early elderly group, and 82.4±3.4% in the old elderly group, and 71.8±3.8, 66.8±4.3, and 59.9±7.7%, respectively (P=0.61). The 5- and 10-year estimated cardiac death-free rates (Figure 2) were 95.3±1.4%, 97.7±0.9%, and 98.3±1.2%, and 89.6±3.2%, 95.0±2.1%, and 96.5±2.1%, respectively (P=0.16). The overall survival was significantly reduced with aging (Figure 3). The 5- and 10-year estimated survival rates were 88.6, 87.4±2.0%, and 80.3±3.5%, and 75.7±4.2%, 62.7±4.2%, and 51.3±6.5%, respectively (P<0.001).
| All (n=780) | <65 (n=262) | 65–74 (n=329) | ≥75 (n=189) | |
|---|---|---|---|---|
| No. of deaths | 153 | 33 | 70 | 50 |
| Cause of death | ||||
| Cardiac death | 36 (23.5) | 14 (42.4) | 13 (18.6) | 9 (18.2) |
| Cancer | 30 (19.6) | 8 (24.2) | 13 (18.6) | 9 (18.2) |
| Pneumonia | 23 (15.0) | 4 (12.1) | 12 (17.1) | 7 (14.0) |
| Stroke | 11 (7.2) | 1 (3.0) | 3 (4.3) | 7 (14.0) |
| Renal failure | 12 (7.8) | 1 (3.0) | 7 (10.0) | 4 (8.0) |
| Other | 41 (30.1) | 5 (15.2) | 22 (31.4) | 14 (28.0) |
Abbreviation as in Table 1.

Freedom from cardiac events among elderly Japanese patients undergoing off-pump CABG.
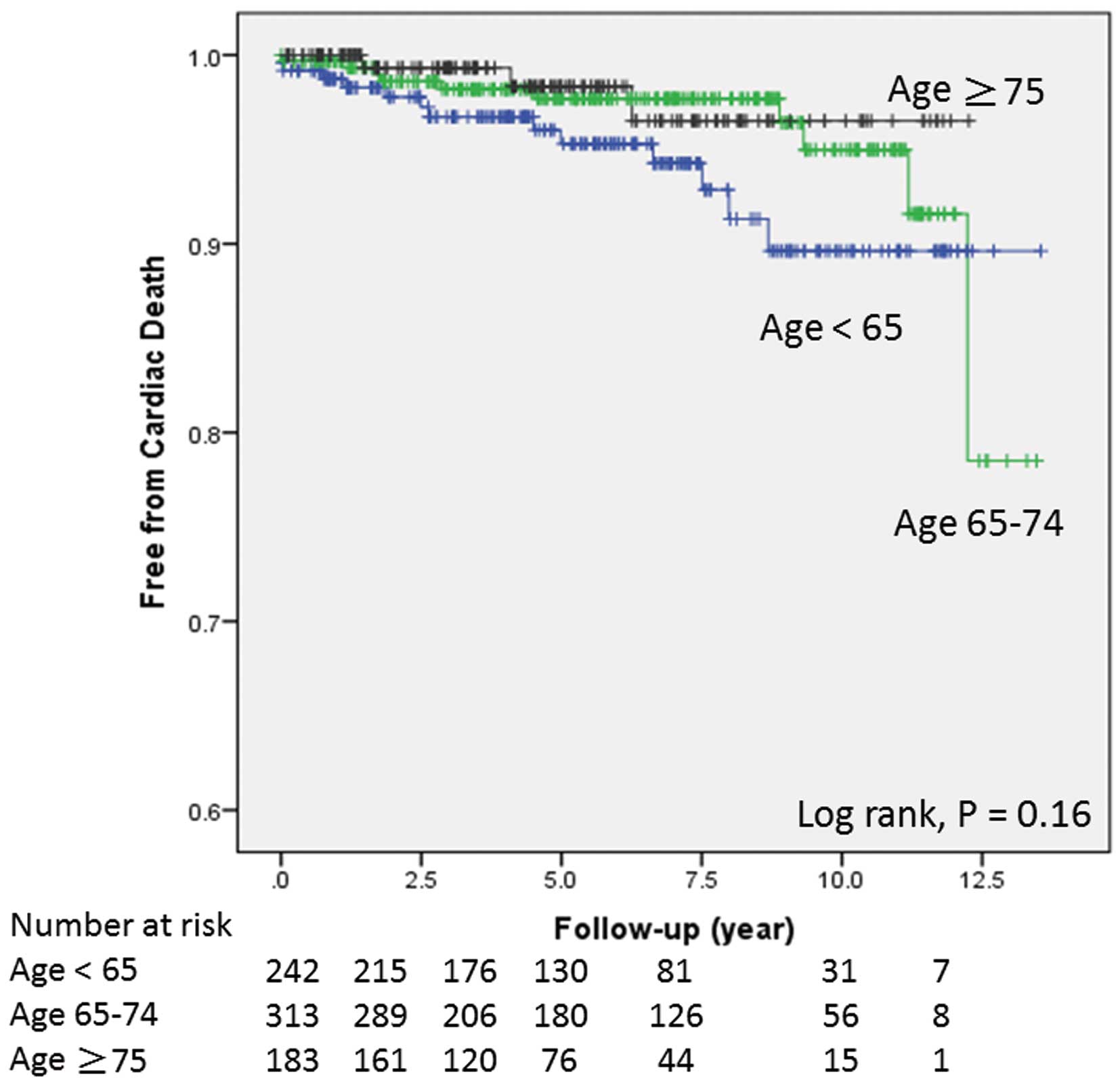
Survival free from cardiac death among elderly Japanese patients undergoing off-pump CABG.

Survival free from overall death among elderly Japanese patients undergoing off-pump CABG.
In a subgroup analysis of patients aged over 80 years, the 5-year estimated cardiac event-free and overall survival rate were 85.6±6.1% and 78.8±6.2%, respectively (Figure S1). As for reoperation, there were 4 cases and all of them involved CABG. The total reoperation-free rate at 10 years after the operation was 99.4±0.3% (Figure S2).
Multivariate Cox Hazard ModelThe results of the Cox hazard models and entered variables are summarized in Table 5. The independent risk factors predicting cardiac events were preoperative NYHA classification (HR: 1.265, P=0.009), and preoperative EF (HR: 0.987, P=0.16). Age at operation was not an independent risk factor for predicting long-term cardiac events (P=0.261). The risk factors affecting overall survival were age at operation, preoperative EF (HR: 0.980, P<0.001), preoperative eGFR (HR: 0.974, P<0.001), and peripheral artery disease (HR: 2.098, P=0.007). Bilateral ITA grafting was an independent preventive factor improving overall survival (HR: 0.646, P=0.029).
| β coefficient | Adjusted HR | 95% CI | P value | |
|---|---|---|---|---|
| Cardiac events | ||||
| Age group (years) | – | – | – | 0.261 |
| <65 | – | 1 | – | – |
| 65–74 | 0.183 | 1.201 | 0.826–1.746 | 0.337 |
| ≥75 | −0.173 | 0.841 | 0.520–1.363 | 0.483 |
| NYHA | 0.250 | 1.265 | 1.065–1.510 | 0.009 |
| Pre EF | −0.014 | 0.986 | 0.975–0.997 | 0.016 |
| Overall survival | ||||
| Age group (years) | <0.001 | |||
| <65 | – | 1 | – | – |
| 65–74 | 0.528 | 1.696 | 1.249–3.059 | 0.029 |
| ≥75 | 0.953 | 2.595 | 1.927–5.155 | <0.001 |
| Pre EF | −0.020 | 0.980 | 0.967–0.990 | <0.001 |
| Pre eGFR | −0.026 | 0.974 | 0.967–0.981 | <0.001 |
| PAD | 0.594 | 2.098 | 1.175–2.796 | 0.007 |
| Bilateral ITA | −0.437 | 0.646 | 0.437–0.956 | 0.029 |
The following variables with a probability value of less than 0.20 in the univariate analysis were entered as adjustors: group, male sex, preoperative eGFR, preoperative EF, MR ≥2, diabetes mellitus, COPD, PAD, hyperlipidemia, NYHA classification, previous PCI, acute MI, bilateral ITA, and complete revascularization. HR, hazard ratio. Other abbreviations as in Tables 1,2.
In the present study, we compared the short- and long-term results of OPCAB based on age stratification. There were 2 major findings. Firstly, despite the high rate of postoperative respiratory complications in the elderly groups, in-hospital mortality was excellent regardless of age at operation. Secondly, age at operation did not affect the long-term cardiac outcomes in patients undergoing OPCAB.
Surgical intervention for the elderly remains challenging because of the presence of multiple comorbidities.1,19 One of the main aims in adopting the OPCAB technique is to overcome the side effects of using CPB, including stroke and serious adverse outcomes.15,20,21 These complications result from aortic manipulation, embolic complications, non-physiological circulation, cardiac arrest, coagulation disturbances, and systemic inflammation.9–11,14,22 Stamou et al demonstrated that the benefits of OPCAB are more evident in high-risk patients based on short- and long-term results.9 The report from The Society of Thoracic Surgeons National Clinical Database demonstrated that OPCAB significantly reduces the risk of death, stroke, and acute renal failure. Sarin et al demonstrated, based on propensity-score matching, that in-hospital mortality was reduced in patients with vs. without OPCAB (2.8% and 9.3%, respectively).5
In the early results of our study, in-hospital mortality of 1.1%, even in the late elderly patients (>75 years), was excellent as compared with previous studies.3,5,20 The relatively high mortality in elderly patients undergoing conventional CABG is considered to result from high rates of perioperative stroke and complications related to CPB.5,6,9,20 A recent meta-analysis of 14 studies of OPCAB in octogenarians demonstrated lower incidences of stroke and respiratory failure in patients receiving OPCAB.20 The reported in-hospital mortality in the OPCAB group was 3.8% and that in the conventional CABG was 6.0% in patients older than 80 years, and the OR for mortality was 0.54. Saito et al reported the short-term results in 13,488 cases of isolated CABG with the same age stratification as in the present study.3 They reported that 30-day mortality was 1.7% (<65 years old), 2.3% (65–75 years old), and 4.3% (≥75 years old), respectively. Their in-hospital mortality of the elderly was higher than in our results. One of the possible reasons for these differences is that their study included approximately 40% of on-pump CABG cases. Indeed, they reported that bleeding requiring reoperation, postoperative stroke, renal failure, gastrointestinal complications, and LOS were significantly increased with aging. However, the occurrence of these complications was not significantly different among the 3 groups in the present study. As for renal protection, we tried to maintain systolic blood pressure at more than 80 mmHg to preserve blood flow to the kidney during heart positioning. The target was raised to 100 mmHg in patients with advanced age, or impaired kidney function. In the case of impaired renal function, we started to administer intravenous fluids from the day prior to the operation to prevent prerenal failure. A combination of these strategies with an off-pump technique may minimize the differences in the incidence of postoperative renal failure among groups. Therefore, our results suggest that OPCAB could prevent the potential complications that can occur in patients undergoing CABG with CPB. However, the rate of respiratory complications was significantly higher in the elderly groups, which contributed to the increase in major complications with aging in the present study (borderline significance). In the elderly, respiratory complications are common and contribute to a higher mortality rate after conventional CABG.20 However, the in-hospital mortality did not increase with aging in this study, possibly because these respiratory complications were not as severe as those observed with conventional CPB, such as pulmonary edema or acute respiratory disorder syndrome, but rather those caused by weakened expectoration of sputum or weakened respiration after general anesthesia. Indeed, Nagpal et al reported favorable results with the shorter postoperative ventilation time in OPCAB patients as compared with those receiving conventional CABG (5.3% and 13.3%, respectively).23
Stroke occurred in 10 patients (1.3%) postoperatively, being similar to the rates in previous reports on OPCAB.12,15,20 Our meticulous pre- and intraoperative risk assessment of cerebrovascular disease and the aorta may have contributed to the absence of differences in the stroke rate among groups. In fact, there was no case of intraoperative stroke in the present study. However, patients showed delayed cerebral infarction related to AF, carotid stenosis, or coagulation disturbance caused by infection. This type of stroke occurred even in cases of aorta-non-touch technique (4 cases, 2.4% of aorta-non-touch technique group) as compared with 6 cases of aortic manipulation (1.0% of patients with proximal anastomosis). This suggests that OPCAB with or without the aorta-non-touch technique does not significantly reduce the incidence of delayed stroke, despite it being effective at preventing intraoperative stroke.24 In addition to carotid stenosis and a past history of stroke, we previously reported that perioperative delayed stroke was associated with postoperative AF, LOS, and MI.25 Heart positioning is a concern during OPCAB. We have adopted the use of IABP in patients with severe carotid stenosis to prevent hemodynamic cerebral infarction during heart positioning. Therefore, the rate of IABP usage might be significantly higher in the late elderly group. The incidence of AF was slightly higher in the early elderly group, but not significantly different and may have been related to the higher rates of preoperative DM and hyperlipidemia in the early elderly group than in the other groups. In this study, transfusion was more frequently required in the late elderly group, possibly because preoperative anemia of various etiologies is usually more frequent with advanced age. However, data on the preoperative hemoglobin levels were not available.
Our subgroup analysis demonstrated excellent early outcomes of patients aged older than 80 years. Not using CPB certainly contributed to these favorable results; however, a potential selection bias may have existed. For example, more high-risk patients received catheter intervention, or hemodynamically unstable patients underwent an on-pump procedure from the beginning.
In our multivariate analysis, the preoperative NYHA classification was the only risk factor predicting the occurrence of major in-hospital complications, and not age. Argenziano et al reported in their randomized trial that the preoperative NYHA classification is a significant risk factor in predicting in-hospital mortality in patients undergoing CABG.26
In our long-term results, the rates free from cardiac events and cardiac deaths were not significant, and advanced age was not an independent risk factor for cardiac events. However, the overall survival significantly decreased with aging, and advanced age was an independent risk factor predicting all-cause mortality. In general, normal life expectancy is usually shorter in the more elderly group. In the present study, more than 40% of the deaths in the young group were cardiac, while the majority of deaths in the elderly groups were non-cardiac, such as cancer, infection, stroke, or renal failure.
Therefore, our results suggest that age at operation does not affect long-term outcomes in patients undergoing OPCAB with regard to cardiac complications.
Controversies remain regarding the long-term outcomes of OPCAB, because of concerns over incomplete revascularization or the quality of the anastomosis.27–29 Propensity-score matching involving a large cohort from Korea28 showed that OPCAB significantly reduced the long-term survival compared with on-pump CABG. However, in the quintile stratification analysis of that report, the long-term results improved with an increasing rate of OPCAB, which suggests that even in a high-volume center with well-experienced surgeons and staff, there is a learning curve to performing OPCAB. In the present study, our rate of adopting OPCAB was 81.0%, and that over the last 5 years was 96.4% (data not shown), which means that the off-pump procedure is our routine technique for surgical revascularization. A recent meta-analysis showed that analysis of only randomized controlled trials and propensity-matched studies demonstrates comparable long-term mortality between OPCAB and on-pump CABG.30 One of the largest randomized studies demonstrated similar 1-year outcomes between OPCAB and on-pump CABG with regard to overall mortality, stroke, MI, and renal failure.31 One feature of this study was specifying the qualification of surgeons performing OPCAB and on-pump CABG, which was neglected in previously unfavorable reports on OPCAB.27,32 In the long-term, a recent study demonstrated that the 15-year survival between on- and off-pump groups was not different (72.8% and 76.5% for bilateral ITA and 61.8% and 67.2% for single ITA, respectively), and the pump status did not influence long-term survival.33 They also reported that bilateral ITA grafting and complete revascularization were independent factors improving overall survival. In the present study, the mean number of distal anastomoses was 3.4±1.0 in the entire cohort, and the rate of complete revascularization was not significant in each group. Therefore, optimal revascularization was achieved. We think that OPCAB should be performed throughout the world, but multivessel OPCAB requires a different skill set and is technically demanding. Therefore, OPCAB should not be readily performed by all surgeons, as presented by the ROOBY trial.31 However, it is not so difficult for surgeons experienced in conventional CABG to perform high-quality OPCAB after having treated 50–100 cases with the off-pump technique. There is a learning curve, but it can be mastered with a step-by-step approach, such as starting with simple cases, or on-pump beating CABG.
One of the features of the present study was the high rate of bilateral ITA grafting even in the late elderly (67.7% in the late elderly and 81.8% in the early elderly). We showed that using bilateral ITA grafting was an independent predictor of improved overall survival, consistent with many previous reports.34–36 However, it was not an independent preventive factor for cardiac events, possibly because cardiac events comprise relatively soft endpoints, such as congestive heart failure caused by rapid AF or afterload mismatch, or coronary intervention for a progressed lesion that did not show significant stenosis at surgery. To eliminate the potential observer bias, we defined all of the above as cardiac events.
Study LimitationsFirstly, it was a single center, nonrandomized, retrospective study. Secondly, the patients’ backgrounds were intrinsically different in some respects between groups. However, the aim of this study was to investigate the influence of age on both short- and long-term outcomes. This type of comparison is not suitable for propensity-matched models. Thirdly, there might be some bias in choosing an elderly patient as a candidate to undergo OPCAB at referral. Therefore, there is a possibility that more high-risk patients would undergo PCI or receive medical treatment only. Fourthly, we did not directly compare OPCAB and CABG+CPB. Finally, we did not examine the relationship between graft patency and long-term outcomes.
OPCAB was performed safely in elderly patients, despite a higher rate of postoperative respiratory complications and transfusion. In addition to favorable short-term results, long-term cardiac outcomes of OPCAB were not influenced by age at operation.
The authors thank Professor Satoshi Teramukai (Department of Biostatics, Kyoto Prefectural University of Medicine, Kyoto, Japan), for providing statistical discussion and valuable comments about this study.
None declared.
Supplementary File 1
Table S1. Baseline characteristics and operative results in Japanese patients older than 80 years undergoing off-pump CABG
Figure S1. Freedom from cardiac events and overall death in Japanese patients older than 80 years undergoing off-pump CABG.
Figure S2. Freedom from reoperation in each age group of elderly Japanese patients undergoing off-pump CABG.
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-15-0462