Article ID: CJ-16-0602
Article ID: CJ-16-0602
Background: Ventricular fibrillation (VF) is a life-threatening disease that can be remedied by prompt defibrillation. However, data regarding such risk in a general population remain limited. This general population study was to explore the epidemiological profile of VF.
Methods and Results: We investigated patients with VF younger than 60 years (average population, 19,725,031) using a national database spanning the period 2000–2010. We identified 3,971 (68.4% male) patients with VF (crude incidence rate: 1.83/100,000). Incidence rates were low in patients younger than 10 years and increased steadily after adolescence. Comorbidities were noted in 2,766 (69.7%) patients, with 2,431 (61%) having cardiac diseases. Over half of the adolescent and young adult patients did not have comorbidities. Among the 838 deaths (mortality rate 21.1%), approximately half (381/838, 45.5%) occurred after arrival at emergency services (ES). The proportion of deaths after arrival at ES relative to total deaths increased sharply to a peak in the 15–19-years age group and thereafter remained stationary.
Conclusions: VF patients, with a male dominance, increased after adolescence and were likely to die at presentation to ES. Approximately half of young adults, with high mortality, did not have comorbidities, suggesting underdiagnosis of underlying primary electrical diseases and the need for implementing automated external defibrillator programs.
Ventricular fibrillation (VF) is a very rare but life-threatening rhythm disturbance of the heart. It may be the first manifestation of an underlying primary electrical disease, particularly in the young.1–3 In adults, it more likely occurs as a complication of coexisting coronary artery disease (CAD) or other cardiac disease. It can also serve as a sign of poor prognosis in patients with cardiac diseases. Prompt resuscitation using a defibrillator may improve an affected patient’s prognosis, promoting efforts to make automated external defibrillator (AEDs) accessible to the public.4–6 However, epidemiological data on VF, particularly for young populations, are still limited.
The population of Taiwan is approximately 23 million. The National Health Insurance (NHI) program, implemented in 1995, covers more than 99% of the general population. We hypothesized that the number of patients with VF in Taiwan, a country with comprehensive and easily accessible medical care, would reflect the clinical spectrum and subsequent medical needs of the disease. Therefore, this study, based on a national database spanning 11 years, explored the current epidemiological profile of VF.
All healthcare records logged between January 1, 2000 and December 31, 2010 were retrieved from the NHI database. Each health record had a scrambled identification number and contained information such as the patient’s date of birth, date of hospital visit, sex, type of visit, diagnosis, and treatment codes. On the basis of the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code, we selected patients who met the criteria listed for VF (ICD 427.4). The comorbidities were also identified by the respective ICD-9-CM codes. To avoid errors from tentative diagnoses, only the data from those who required attention at outpatient clinics more than twice, or emergency services (ES) or were admitted under a VF-specific diagnosis were used. To avoid confounding from other diseases commonly encountered in old age, we used only the data of those aged younger than 60 years at first VF diagnosis. The population sizes between 2000 and 2010 were adopted from the Statistical Yearbook of the Department of Statistics, Ministry of the Interior. The average general population younger than 60 years during the study period was 19,725,031.
The NHI program initiated reimbursement for implantable cardioverter-defibrillator (ICD) therapy in 2003. The reimbursement rates were identified from the reimbursement code for the devices. The patient’s survival status was determined by the event of death reported at discharge and confirmed by the final insurance status in the NHI database. Survival patients comprised those with confirmed survival. Death at admission and death at ES included patients who died on the same dates as discharge from admission and ES, respectively.
Statistical AnalysisWe used the Statistical Package for Social Sciences statistical software (SPSS, Version 15.0, SPSS Inc, Chicago, IL, USA) for analysis. We used the independent t test to draw comparisons of the means among continuous variables and analyzed the associations among categorical variables by using the chi-squared test. Multivariate logistic regression was then applied to identify the predictors. Those with a P value <0.05 were included for analysis, while those with a P value >0.1 were excluded. A P value <0.05 was considered statistically significant. We used the World Health Organization’s World Standard Population (2000–2025) for age adjustment of incidence rate. Poisson regression was adopted for analyzing the differences in incidence rates between male and female groups.
In the study period 2000–2010, 3,971 patients (68.4% male) aged younger than 60 years received medical care for VF. The crude incidence rate was 1.83 per 100,000 person-years, and the incidence rate age-adjusted using the World Health Organization’s World Standard Population (2000–2025) was 1.55 per 100,000 person-years. The crude incidence rates of males and females were 2.46 and 1.18 per 100,000 person-years, respectively. The age-adjusted incidence rates were 2.11 and 0.99 per 100,000 person-years in the male and female groups, respectively. The crude incidence rates vs. age in different sex groups are shown in Figure 1. Few patients were younger than 10 years; however, the numbers increased steadily after adolescence. The incidence rate increased with age. Male predominance was observed in almost all age groups except for the 1–4-years group. The differences in incidence rates between sexes increased with ages. The male-to-female ratio of crude incidence rates was 1.48–1.67 in the 15–39-years age group, increasing to more than 2.28 in the 40–59-years age group (Table 1). The Poisson regression showed that the incidence rate of the male group was 2.16-fold higher than that of the female group (P<0.0001).

Crude incidence rate over age.
| Crude incidence rates (per 100,000 person-years) |
Age at 1 st diagnosis of VF (years) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1–4 | 5–9 | 10–14 | 15–19 | 20–24 | 25–29 | 30–34 | 35–39 | 40–44 | 45–49 | 50–54 | 55–59 | Total | |
| Total | 0.520 | 0.083 | 0.069 | 0.183 | 0.307 | 0.439 | 0.642 | 1.058 | 1.464 | 2.462 | 3.606 | 5.248 | 8.047 | 1.829 |
| Female | 0.454 | 0.097 | 0.039 | 0.179 | 0.228 | 0.328 | 0.508 | 0.802 | 1.177 | 1.495 | 2.165 | 2.909 | 4.868 | 1.175 |
| Male | 0.580 | 0.071 | 0.096 | 0.186 | 0.381 | 0.545 | 0.772 | 1.309 | 1.746 | 3.411 | 5.033 | 7.597 | 11.297 | 2.459 |
| Male-to-female ratio | 1.279 | 0.732 | 2.450 | 1.042 | 1.673 | 1.660 | 1.520 | 1.632 | 1.483 | 2.282 | 2.325 | 2.612 | 2.320 | 2.1 |
VF, ventricular fibrillation and flutter.
Comorbidities were noted in 2,766 (69.7%) patients (Table 2). Cardiac comorbidities were noted in 2,431 (61%) of the patients with VF. The adolescent and young adult patients (the 15–19, 20–24, and 25–29-years age groups) were less likely to have comorbidities, and over half of the patients in the 15–19, 20–24, and 25–29-years age groups did not have comorbidities. By contrast, in the infant (age <1 years) and older adults (aged ≥35 years) groups, over half of the patients had cardiac comorbidities.
| Age at 1 st diagnosis of VF (years) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1–4 | 5–9 | 10–14 | 15–19 | 20–24 | 25–29 | 30–34 | 35–39 | 40–44 | 45–49 | 50–54 | 55–59 | Total | |
| None, n (%) | 4 (33) | 5 (56) | 5 (45) | 12 (38) | 35 (63) | 52 (59) | 70 (51) | 85 (39) | 110 (36) | 153 (30) | 198 (28) | 228 (26) | 248 (25) | 1,205 (30) |
| Cardiac comorbidities, n (%) | 7 (58) | 3 (33) | 5 (45) | 14 (44) | 18 (32) | 22 (25) | 54 (40) | 106 (49) | 160 (53) | 314 (61) | 460 (64) | 596 (67) | 672 (68) | 2,431 (61) |
| Ao dissection | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 2 | 4 |
| Bradycardia | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 2 | 0 | 1 | 0 | 0 | 2 | 7 |
| CAD | 0 | 0 | 0 | 0 | 1 | 6 | 23 | 47 | 104 | 207 | 313 | 430 | 450 | 1,581 |
| CHD | 3 | 2 | 3 | 6 | 4 | 6 | 5 | 6 | 14 | 12 | 5 | 2 | 9 | 77 |
| Hypertension | 0 | 0 | 0 | 1 | 0 | 0 | 3 | 11 | 14 | 36 | 65 | 74 | 116 | 320 |
| Myocardial disease | 3 | 1 | 1 | 3 | 6 | 5 | 11 | 18 | 22 | 41 | 52 | 68 | 73 | 304 |
| Myocarditis | 0 | 0 | 1 | 2 | 1 | 1 | 5 | 0 | 4 | 3 | 2 | 0 | 0 | 19 |
| Other | 0 | 0 | 0 | 0 | 1 | 0 | 4 | 4 | 1 | 3 | 7 | 3 | 5 | 28 |
| VHD | 0 | 0 | 0 | 1 | 2 | 2 | 1 | 14 | 1 | 9 | 15 | 16 | 15 | 76 |
| WPW | 0 | 0 | 0 | 1 | 2 | 2 | 2 | 4 | 0 | 1 | 1 | 2 | 0 | 15 |
| Noncardiac comorbidities, n (%) |
1 (8) | 1 (11) | 1 (9) | 5 (16) | 2 (4) | 10 (11) | 12 (9) | 22 (10) | 30 (10) | 44 (9) | 54 (8) | 60 (7) | 69 (7) | 311 (8) |
| Trauma, n (%) | 0 | 0 | 0 | 1 (3) | 1 (2) | 4 (5) | 0 | 5 (2) | 2 (1) | 1 (0.2) | 2 (0.3) | 2 (0.2) | 6 (1) | 24 (1) |
| Total | 12 | 9 | 11 | 32 | 56 | 88 | 136 | 218 | 302 | 512 | 714 | 886 | 995 | 3,971 |
Ao, aortic; CAD, coronary artery disease; CHD, congenital heart disease; VF, ventricular fibrillation and flutter; VHD, valvular heart disease; WPW, Wolff-Parkinson-White syndrome.
The cardiac comorbidities identified were CAD in 1,581 (65%), hypertension in 320 (13.2%), myocardial disease (cardiomyopathy) in 304 (12.5%), congenital heart disease (CHD) in 77 (3.2%), valvular heart disease in 76 (3.1%), myocarditis in 19 (0.8%), Wolff-Parkinson-White syndrome (WPW syndrome) in 15 (0.6%), and bradycardia (such as sick sinus syndrome or atrioventricular block) in 7 (0.3%). The spectrum of associated cardiac disease and ailments was distinct among the different age groups (Figure 2). In the pediatric population (<20 years), few patients had CAD, with the majority of cardiac comorbidities being CHD, followed by myocardial disease and myocarditis. By contrast, in the adult age groups, CAD was the most common associated cardiac disease, followed by hypertension and myocardial disease. Nevertheless, patients with CHD continued to also present as VF in all adult age groups. In addition, WPW syndrome was found to be especially prevalent in the 15–19- and 25–29-years age groups (3.6% and 1.5%, respectively).

Percentages of cardiac comorbidities and no comorbidities. Ao, aortic; CAD, coronary artery disease; CHD, congenital heart disease; VHD, valvular heart disease; WPW syndrome, Wolff-Parkinson-White syndrome; None, no comorbidities.
There were 838 (72.4% male) deaths, accounting for a mortality rate of 21.1%, with approximately half (381/838, 45.5%) of them occurring after arrival at ES. The proportion of deaths after arrival at ES relative to total deaths was extremely low in children, increased sharply to a peak (83.3%) in the 15–19-years age group, and thereafter remained at approximately 50% in the adult age groups (Figure 3). In the pediatric age groups, the mortality rate varied widely. It was high in the age groups younger than 15 years (21.9–66.7%), with most of the patients having cardiac comorbidities (20/23). By contrast, the mortality rate in the 15–19-year-olds was relatively low (10.7%), with most deaths (5/6) occurring after arrival at ES and all of the patients who died not having comorbidities identified. In the adult population, the mortality rate ranged from 16.2% to 23.8%, with approximately half of the group having cardiac comorbidities.
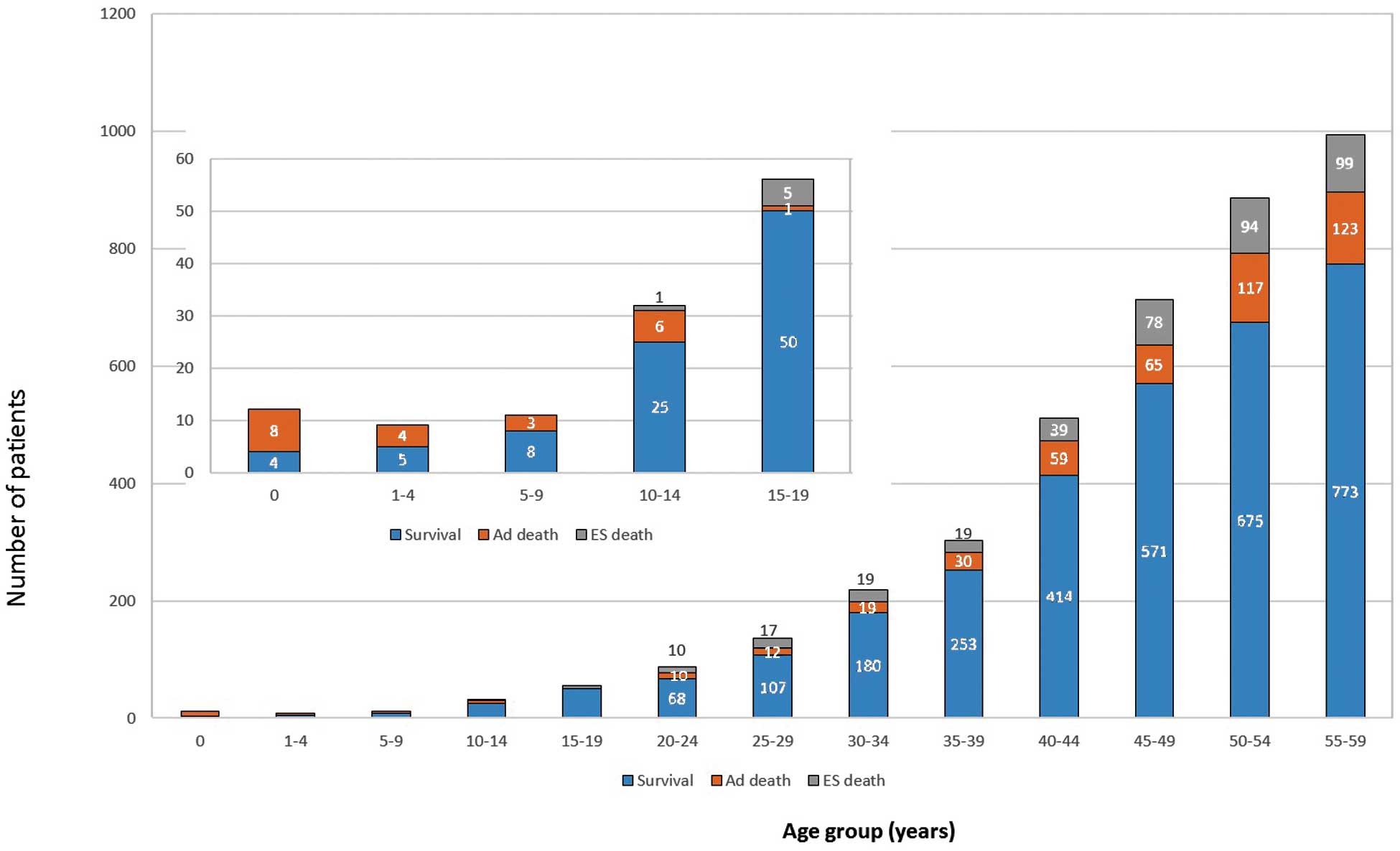
Proportion of deaths at emergency services and the inpatient department. Ad death, death at admission; ES death, death at emergency services.
The mortality rate was higher in those without comorbidities (387/1,205, 32.1%, P<0.001), than in those with cardiac comorbidities (356/2,431, 14.6%), those with trauma (6/24, 25%), and those with noncardiac comorbidities (89/311, 28.6%). We summarized the probability of death for each subgroup in the different age groups in Table 3. Among those with cardiac comorbidities, the highest mortality rate was noted in those with myocarditis.
| Age group (years) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1–4 | 5–9 | 10–14 | 15–19 | 20–24 | 25–29 | 30–34 | 35–39 | 40–44 | 45–49 | 50–54 | 55–59 | Total | |
| None (%) | 25 | 20 | 0.0 | 8.3 | 17.1 | 23.1 | 25.7 | 29.4 | 20.0 | 25.5 | 37.9 | 39.5 | 39.1 | 32.1 |
| Comorbidities (%) | ||||||||||||||
| Cardiac comorbidities | 85.7 | 100.0 | 60.0 | 21.4 | 0.0 | 13.6 | 16.7 | 8.5 | 12.5 | 15.0 | 11.7 | 16.3 | 15.2 | 14.6 |
| Aortic dissection | – | – | – | – | – | – | – | – | – | 0.0 | – | 0.0 | 0.0 | 0.0 |
| Bradycardia | 0.0 | – | – | – | 0.0 | – | – | 0.0 | – | 0.0 | – | – | 0.0 | 0.0 |
| CAD | – | – | – | – | 0.0 | 0.0 | 4.3 | 8.5 | 9.6 | 12.1 | 10.5 | 15.8 | 15.6 | 13.3 |
| CHD | 100.0 | 100.0 | 33.3 | 16.7 | 0.0 | 0.0 | 0.0 | 0.0 | 14.3 | 16.7 | 20.0 | 0.0 | 0.0 | 15.6 |
| Hypertension | – | – | – | 0.0 | – | – | 0.0 | 0.0 | 7.1 | 8.3 | 7.7 | 8.1 | 8.6 | 7.8 |
| Myocardial diseases | 100.0 | 100.0 | 100.0 | 0.0 | 0.0 | 40.0 | 45.5 | 16.7 | 22.7 | 34.1 | 23.1 | 27.9 | 24.7 | 27.3 |
| Myocarditis | – | – | 100.0 | 100.0 | 0.0 | 100.0 | 40.0 | – | 50.0 | 66.7 | 50.0 | – | – | 57.9 |
| Other | – | – | – | – | 0.0 | – | 0.0 | 25.0 | 0.0 | 0.0 | 0.0 | 0.0 | 20.0 | 7.1 |
| VHD | – | – | – | 0.0 | 0.0 | 0.0 | 100.0 | 7.1 | 0.0 | 11.1 | 13.3 | 18.8 | 20.0 | 14.5 |
| WPW syndrome | – | – | – | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | – | 0.0 | 0.0 | 50.0 | – | 6.7 |
| Noncardiac comorbidities | 100.0 | 0.0 | 0.0 | 40.0 | 0.0 | 30.0 | 16.7 | 18.2 | 20.0 | 27.3 | 25.9 | 38.3 | 31.9 | 28.6 |
| Trauma | – | – | – | 100.0 | 0.0 | 50.0 | – | 0.0 | 50.0 | 0.0 | 0.0 | 50.0 | 16.7 | 25.0 |
| Total | 66.7 | 44.4 | 27.3 | 21.9 | 10.7 | 22.7 | 21.3 | 17.4 | 16.2 | 19.1 | 20.0 | 23.8 | 22.3 | 21.1 |
–: Not shown, because no patients in the group. Abbreviations as in Table 2.
During a total of 16,187 patient-years of follow-up, 201 patients received intracardiac defibrillator therapy at ages ranging from 11 to 50 (median, 43) years. The probability of ICD therapy in the population of patients with VF was 1.24% per person-years. Excluding 381 patients who died after arriving at ES and patients who received only outpatient department follow-up, ICD therapy was administered in 6.45% (201/3,118) of the patients with VF.
VF is a rare but life-threatening arrhythmia. In this national cohort study, we obtained 3 main findings: (1) low incidence rate in patients younger than 10 years, but a steady increase after adolescence, with an age-adjusted incidence rate of 1.55 per 100,000 person-years (the crude incidence rate was 1.83 per 100,000 person-years); (2) predominance of males in most age groups, but male sex did not increase the risk of death; and (3) comorbidities were common in the adolescent and young adult age groups, but over half of the patients did not have comorbidities. In addition, the mortality rate was significantly higher in those with no comorbidities.
Incidence of VF EventsIn Taiwan, bystander cardiopulmonary resuscitation rates in out-of-hospital cardiac arrest patients increased from 2% in 2001 to 17.3% in 2009.7,8 However, laws regarding public-access AED were not promulgated until 2013. To allocate limited medical resources in order to effectively disseminate AEDs, a precise epidemiological profile of sudden cardiac death (SCD) and relevant cardiac conduction disturbances is required.4–6 An exact understanding of both the incidence of VF and the demographics of affected patients can facilitate determining the social burden associated with heart rhythm disturbances. Data regarding the epidemiology of VF are still limited. Most relevant studies have examined the epidemiology of SCD and explored the characteristics of VF subgroups using databases created by emergency medical system personnel.9–11 The reported annual incidence of SCD ranges from 50 to 100 per 100,000 person-years in the general population in Europe and North America and from 37 to 43 per 100,000 person-years in Asia.12–14 Primary electric disorders related to channelopathies, such as long QT syndrome, Brugada syndrome, catecholaminergic polymorphic ventricular tachycardia, short QT syndrome and idiopathic VF, are estimated to be responsible for approximately 10% of SCDs. They also play a critical role in the development of VF.14,15 Currently suggested placements of AEDs in public locations are guided by site-specific incidences, the availability of emergency medical service, and the presence of subjects who are thought to be at a high risk for SCD.4,5,16 Our study was a nationwide, population-based cohort study and thoroughly describes the age-specific incidence, mortality rates, and patient characteristics of VF. The main reason that incidence rates in the present study were lower than those estimated from the previous literature was because we used the data of those aged younger than 60 years at first VF diagnosis. However, by providing information about age-specific incidences of, and death probabilities associated with, different comorbidities, our study will facilitate clarification of the costs and benefits of secondary prevention strategies such as the indications for ICD implantation, screening programs for cardiac conduction disturbances, and promotion of public-access AED programs. The results of our comorbidity analysis, especially concerning the percentage of cardiac comorbidities in different age groups, revealed the different manifestations of rhythm disturbance in different age groups. In pediatric populations, the majority of cardiac comorbidities were CHD, followed by myocardial disease and myocarditis. In adult groups, however, CAD was the most common associated cardiac disease, followed by hypertension and myocardial disease. Our study revealed that incidence rates of VF gradually increased with age after the age of 10 years. This phenomenon may be related to epidemiological changes in the underlying diseases in the general population, because prevalence rates of CAD, hypertension and myocardial disease also increase with age. Although we could not ascertain a causal relationship between VF and comorbidities, the changes in the spectrum of comorbidities may provide guidance for future research into these fatal diseases in different age groups.
Sex Differences in VF EventsNumerous epidemiologic studies have examined the sex differences in clinical arrhythmia.17–20 However, few studies have focused on the rhythm disturbances of VF.21 According to our review of relevant literature, the present study has the largest population-based data to provide references on sex differences in VF. According to the literature, at the ventricular level, women are more susceptible to long QT-associated arrhythmias, whereas men are at a higher risk of early repolarization, idiopathic VF, and Brugada syndrome.17 However, in prepubertal children, sex differences in ventricular arrhythmias are not observed.17 In the present study, male predominance in the incidence rate was noted in all age groups except for the 1–4-years age group. There were 2 sharp increases in the trend of the male-to-female ratio (Table 1). The first increase occurred in the 15–19-years age group, and the second occurred in the 40–44-years age group. These trends correspond with the stages of puberty and menopause, respectively. The trend of increasing differences implies that VF might be associated with biological differences, including changes in hormone regulation during different stages of life and variance in the basic electrophysiological properties of cardiomyocytes. However, further investigation is still required to determine the precise causes of the differences. In general, men have a higher incidence of SCD than women, which generally reflects the higher incidence of CAD in men.14,22–24 Regarding the underlying rhythm related to SCD, women experience VF less often than men.25,26 In our study, the incidence of VF was higher in males in almost all age groups. However, the mortality rate was not increased in the male sex group. Therefore, the epidemiological data in the present study are an important reference about sex differences in VF critical for organizing prevention strategies of SCD.
SCD PreventionVF can be the first manifestation of a myocardial disease or channelopathy that causes SCD in those previously thought to be healthy. SCD in young people brings great grief to the whole family and causes substantial loss of potential social productivity.1–3,27–31 Developing prevention strategies for early diagnosis of underlying electrical diseases, increasing the availability of public-accessed defibrillators and increasing use of ICD in VF survivors, especially in the adolescent and young adult populations, are thus high-priority public health issues.13,28,29 Chiu et al detected cardiac conduction disturbances in a pediatric population through a school survey program involving simplified 4-lead electrocardiography, phonocardiography, and physical examination.32 Fifteen high-risk patients were found among 432,166 students through the program. In our study, more than half of the VF patients did not have documented comorbidities in the 15–19-, 20–24-, and 25–29-years age groups. Furthermore, diseases that could be diagnosed through an electrocardiography screening program, such as WPW syndrome and myocardial diseases, occupied a more significant percentage of the cardiac comorbidities compared with other age groups.33,34 Further study should therefore be designed to determine whether a screening strategy could be effectively applied to detect diseases correlated with VF earlier. Allowing laypersons to use an AED in community units with a relatively higher incidence of SCD has been proven to be safe and to increase the survival rate of patients who experience out-of-hospital cardiac arrest; moreover, several studies have suggested increasing the availability of school-based AEDs.2,16,27,30,31,35,36 Current guidelines recommend a layperson AED program if (1) sudden cardiac arrest is likely to occur every few years and to be witnessed, (2) there are students or staff who are at increased risk of SCD, or (3) the likelihood that emergency medical services can arrive at the scene within 5 min of collapse is low. Nishiuchi et al2 reported a high percentage of pediatric cardiac arrests at schools (approximately 40%). Cardiac diseases were observed in the majority of their patients. The authors suggested the importance of identifying people with cardiac diseases that potentially predispose them to cardiac arrest.2 In the present study, more than half of the VF patients in the 15–19-years age group did not have documented comorbidities. Although the mortality rate was relatively low in this group (10.7%), most of those without comorbidities died after arriving at the ES (5 of 6 deaths), indicating that VF might be the first and lethal manifestation of an underdiagnosed condition. In the 20–24- and 25–29-years age groups, similar results were found. These results created 2 important considerations. (1) Underlying primary electrical diseases might be underdiagnosed in adolescent and young adult populations in Taiwan. Efficient and reliable prevention strategies (eg, ECG screening) should be developed for facilitating early diagnosis and preventing those who are asymptomatic from experiencing lethal events. (2) AED programs must be implemented at schools with people who are known to have cardiopulmonary disease. AED programs in high school and college settings should be encouraged because those who died at ES would have had a greater chance of survival if a defibrillator had been available at the scene. Prevention of SCD by ICD implantation is also validated. Its role in primary prevention in certain patients and evaluation of the difference in clinical outcomes through the upper limit of vulnerability test are well reported.37–39 ICD therapy in Taiwan is still underused (6.45% of the patients with VF) because, at least in part, the NHI program did not initiate the reimbursement until 2003. Future studies should be designed to monitor changes in the epidemiology of VF and SCD in the ICD era.
Study LimitationsFirst, because we could not directly review the ECG results and medical records, we could not confirm the accuracy of the diagnosis of the rhythm disturbance, the location of VF occurrence, the status of cardiac function, the severity of comorbidities and the relation between comorbidities and outcome. Second, there is the possibility that some patients with VF were not included. The initial rhythm of SCD might degenerate from VF to another rhythm, such as asystole or pulseless electric activity, because of delayed arrival of emergency medical services or other reasons. Therefore, those who have been rescued from cardiac arrest caused by VF may not be coded as that rhythm disturbance in the medical records. Third, the study design did not enable us to distinguish between idiopathic VF and secondary VF. Further risk stratification for different underlying electrical diseases or predisposing diseases should be performed in future studies.
Male predominance was noted in patients with VF, in whom the incidence increased after adolescence. The mortality rate was still high and likely to occur after arrival at ES. Mortality rates were higher in young adults without comorbidities, suggesting an underdiagnosis of underlying primary electrical diseases and the need to increase AED programs targeted at the adolescent and young adult subgroups.
We acknowledge the National Science Council, Taiwan, for the funding (NSC 102-2628-B-002-017-MY3, 103-2314-B-002-054-MY3).
This study was in part supported by grants from National Science Council, Taiwan (ROC), (102-2628-B-002-017-MY3, 103-2314-B-002-054-MY3). No author has conflicts to declare.