Article ID: CJ-17-0162
Article ID: CJ-17-0162
Heart transplantation (HTx) is the effective way to improve quality of life as well as survival in terminal heart failure (HF) patients. Since the first heart transplant in 1968 in Japan and in earnest in 1987 at Taiwan, HTx has been continuously increasing in Asia. Although the current percentage of heart transplants from Asia comprises only 5.7% of cases in the International Society of Heart and Lung Transplantation (ISHLT) registry, the values were under-reported and soon will be greatly increased. HTx in Asia shows comparable with or even better results compared with ISHLT registry data. Several endemic infections, including type B hepatitis, tuberculosis, and cytomegalovirus, are unique aspects of HTx in Asia, and need special attention in transplant care. Although cardiac allograft vasculopathy (CAV) is considered as a leading cause of death after HTx globally, multiple observations suggest less prevalence and benign nature of CAV among Asian populations. Although there are many obstacles such as religion, social taboo or legal process, Asian countries will keep overcoming obstacles and broaden the field of HTx.
The prevalence of heart failure (HF) is steadily growing worldwide because of aging populations and increased prevalence of risk factors such as ischemic heart disease, diabetes, and obesity. Also, medical and surgical treatment of cardiovascular disease has advanced tremendously and resulted in better initial survival from cardiovascular events, such as myocardial infarction; however, many survivors eventually suffer from HF following aging. It is estimated that 26 million adults worldwide are living with HF,1 costing roughly 1–2% of healthcare expenditures in Europe and North America.2 What is remarkable is the rapid growth of the elderly population and increasing prevalence of HF in Asia. In Japan, it is estimated that 1 million individuals have HF, and the number of Japanese outpatients with left ventricular dysfunction is predicted to gradually increase from 979,000 in 2005 to 1.3 million by 2030.3,4 In Korea also, HF prevalence was estimated to be 1.53% in 2013, but it is expected to increase by 2-fold, from 1.60% in 2015 to 3.35% in 2040. By 2040, more than 1.7 million Koreans are expected to have HF.5
Despite the remarkable advances in medical and device therapy in the treatment of chronic HF, approximately 5–7% of the HF population will progress to advanced HF.6 The associated mortality rate for endstage HF patients is dismal, with an estimated 1-year survival of 25–75% while receiving guideline-directed medical therapy.7–9 Heart transplantation (HTx) in carefully selected candidates with advanced HF remains the treatment of choice, with 1-year survival reported at 90% and a median survival of 14 years for those patients surviving the first year.10 Although controlled trials have never been conducted, there is a consensus that properly selected transplantation provides significantly increased survival, exercise capacity, quality of life and return to work compared with conventional treatment.6
In the 33rd Adult Heart Transplantation Registry report published by the International Society of Heart and Lung Transplantation (ISHLT) registry, a total of 4,746 heart transplants were performed in 2014 worldwide, but over 90% of the ISHLT data originated in North America and Europe.10 The ISHLT estimates 33% of heart transplant activity is not submitted to its global registry, which makes the registry unlikely to mirror actual heart transplant activity, especially in Asia.11 For example, only a few HTx centers in Australia (5), India (1: Fortis Malar hospital), Iran (2), Israel (3), Japan (1: Tohoku University Hospital), New Zealand (1), Korea (2: Seoul National University Hospital, Severance Hospital), Saudi Arabia (1), and Taiwan (1: Cheng-Hsin General Hospital) participated in the 2016 ISHLT registry.10
The first heart transplant in Asia was performed in 1968 by Dr. Juro Wada at Sapporo Medical University, Japan.11 However, initial experience met with poor outcomes until cyclosporine was used in 1980. Also, cultural taboos surrounding organ donation (believing that organ donation might mean removing organs from a body after death) and incomplete legislation regarding brain death retarded widespread HTx in Asia. However, eventually, the heart transplant era began again in Asia in 1987 in Taiwan12 and Thailand,13 in 1992 in Korea14 and Hong Kong,15 and in 1999 in Japan.16 The first survey of heart transplants in Asia was published in 1999.17 That initial survey reported the HTx activity from 1987 to 1996 with a total of 380 cases from 8 countries: China (7 cases), Hong Kong (8 cases), India (12 cases), Philippines (3 cases), Singapore (12 cases), South Korea (65 cases), Thailand (95 cases), and Taiwan (178 cases). A follow-up survey in 2004 reported that HTx was performed in 10 countries including Hong Kong, India, Japan, Korea, Malaysia, PR China, Saudi Arabia, Singapore, Taiwan, and Thailand. Then, the annual number decreased from 133 in 1997 to 104 in 2001, and 3 countries, Taiwan, Korea and PR China, comprise 73.6% of the total number of HTxs in Asia.18 At present, there are reports of heart transplant activity from other countries, including Japan, Malaysia, Saudi Arabia, Iran, Bangladesh, and Vietnam. Grossly, the majority of the total heart transplants in Asia were done in Taiwan and Korea. In Taiwan, 1,354 hearts transplants have been performed between 1987 and 2012,19 and in Korea 1,319 cases have been performed between 1992 and 2016. Among other countries, the numbers of cases since the initiation of the program are as follows: Saudi Arabia, 249; Japan, 266; Iran, 122; Thailand, 97; Hong Kong, 77; and Singapore, 40.11
In general, the candidate selection criteria are similar to those in Western countries. For example, in Korea, criteria for candidates include cardiogenic shock dependent on continuous inotropic support or mechanical circulatory support, persistent NYHA class IV HF refractory to maximal medical therapy, intractable or severe angina patients not amenable to percutaneous or surgical revascularization, and intractable life-threatening arrhythmias unresponsive to medical therapy, catheter ablation, and/or implantation of intracardiac defibrillator. Similar to Western countries, the waiting list is stratified according to urgency status and waiting time.
Developed countries such as Taiwan, Hong Kong, Singapore, Korea, and Japan have an average recipient age of 49, 47, 45, 50, and 38 years, respectively, which is older than those in Iran, Saudi Arabia, and Thailand (average recipient age of 29, 35, and 35 years, respectively). Overall, recipients in Asia are younger when compared with data from the ISHLT registry (median recipient age of 54 years).11 Recipients in Asia are more commonly male and have less proportion of pretransplant coronary disease.
In general, survival after HTx in Asia has been comparable with or slightly inferior to the results reported from the ISHLT registry.11 Overall results until 2015 are excellently reported in the review article by Krittayaphong et al.11 However, in countries where the HTx procedure is standardized and there is adequate annual surgical experience, >12 cases/year in a majority of transplantation centers, including Taiwan, Hong Kong, Singapore, Korea, and Japan, showed even better survival compared with the ISHLT registry data. For example, in Korea, the survival rates at 1, 5, and 10 years are 88%, 78%, and 67%, respectively.14,20 Remarkably, in Japan, the survival rates at 5 and 10 years are 92.7% and 89.6% (Figure 1). This excellent result may be related to the special donor evaluation and management system in Japan. Because of the limited number of donors, Japan uses a 2-stage screening process for registering for a heart transplant with the Japan Organ Transplant Network (JOTNW) to maximize suitable organs from donors and the authorization to permit heart transplant procedures is only in authorized institutions.21
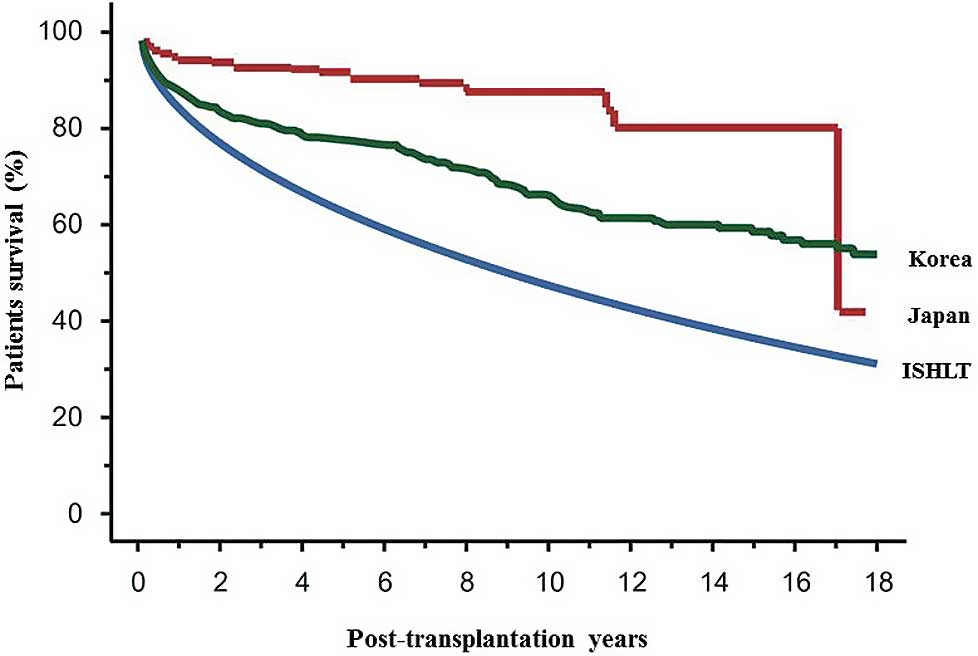
Cumulative survival rate of heart transplant recipients in Japan and Korea.16,24 Korean data presented at Japanese Heart Failure Society meeting 2016 (unpublished data). ISHLT, International Society for Heart and Lung Transplantation. Adapted with permission from Fukushima et al16 and Cha et al.24
The percentage of heart transplants from Asia compared with the rest of the world was reported in the 2012 ISHLT registry.22 According to that, North America, which comprises 7.5% of the world population, accounted for 55.8% of cases, whereas Asia, with 62.5% of the world population, accounted for 5.7% of cases. The data on the optimal number of potential candidates for HTx in Asia are unavailable, but can be estimated based on the number of HTx required in Singapore (3 per 1 million population), yielding the number required for the Asian population of 4.4 billion in 2015 as 13,200, which might far exceed the entire cases in the annual ISHLT registry.23
In contrast to the common belief that donor shortage is the main limiting factor of HTx, most donor hearts are still be under-utilized in Korea. For example, the annual number of brain-death donors is continuously increasing, up to 573 cases in 2016. Although HTx cases are continuously increasing, the ratio of HTx to total brain-death donors has paradoxically decreased from 41.1% in 2001 to 20.6% in 2006, 24.9% in 2009, and 29% (156/573) in 201624 (Korean Network for Organ Sharing, https://www.konos.go.kr/konosis/common/bizlogic.jsp#). As a result, the most urgent HTx candidates, defined as status 0, undergo transplantation within 10 days, while status 1 patients wait approximately 1 month, which is shorter than in the USA data, reported to be at least 2 months for status 1A patients.25 The donor selection criteria are too strict. For example, donors aged over 50 account for only 6.2% of total cases. Female donor hearts are utilized less than male donor hearts and the utilization rate of donor hearts with minor echocardiography abnormalities was only 15.2%, even though clinical outcomes of marginal donor hearts were not different from non-marginal donor hearts.24
In contrast, in Japan, the mean waiting period under status 1 exceeded 1,150 days at the end of June 2016 because of a rapid increase in newly registered patients on the waiting list.16 Therefore, bridge-to-transplantation using a left ventricular assist device plays a greater role, being used in most status 1 recipients (93%). Also because of the severe organ shortage, more marginal donor hearts are being transplanted than in other developed countries. In China, donor shortage has not been a serious problem. However, in 2006, China initiated a citizen organ donation program with the goal of gradually eliminating its old, and to some extent, inappropriate organ procurement system.26 By the end of 2014, China announced the completion of ceasing the use of organs from executed prisoners.27 Considering the rapid expansion of organ transplantation in China, there must be a shortage in organs for HTx in the near future.
Legal process can greatly influence the transplantation process. For example, in Korea in 2000, KONOS (Korean Network for Organ Sharing) was established and abruptly removed the organ allocation authority from individual hospitals to KONOS. That change resulted in the loss of the driving force to locate brain-death donors from the hospital and a decline in HTx from 2-digit annual numbers to limited cases for more than 6 years until the KONOS system was stabilized. In contrast, in Japan revision of the transplant law in July 2010 resulted in a sharp increase in HTx (Figure 2).

Effect of legal policy on heart transplantation. (A) In Korea in 2000, KONOS (Korean Network for Organ Sharing) abruptly removed organ allocation authority from each hospital and centralized it to KONOS. That change resulted in the loss of the driving force finding brain-death donors and a decline in heart transplantation from 2-digit annual numbers to limited cases for more than 6 years until the KONOS system was stabilized. (B) In Japan, revision of the transplant law in July 2010 resulted in a sharp increase in heart transplantation. (Blue bar) Newly referred patients. (Red bar) Transplant patients.
Type B hepatitis (HBV) and tuberculosis (TB) are endemic in Asia. Also, seropositivity of cytomegalovirus (CMV) among Asian countries is much higher, even reaching 90–100% in southern America, Africa and Asia compared with 40–80% in the USA and Western Europe.28 Such chronic infections cause substantial morbidity and mortality after transplantation, not only by infection per se but also by increasing the risk of acute and chronic allograft rejection, including allograft vasculopathy after HTx.29
Asia is endemic for HBV infection. In Korea, the prevalence of HBV in people older than 30 years is still as high as 3.7%. The risk of infection after solid organ transplantation from persons with isolated anti-HBc is low. In particular, recipients with immunity to HBV before HTx can receive a heart from HBV-seropositive donors without any liver-related events. HBV-seropositive recipients have comparable perioperative results and long-term survival rates as HBV-seronegative recipients. However, absence or cessation of antiviral prophylaxis can indiscriminately reactivate HBV, with rapidly progression to hepatic failure and death. In contrast, HBV-seropositive hearts transplanted to HBV immune recipients are maintained without hepatitis reactivation. Therefore, lifelong antiviral prophylaxis is mandatory for HBV-seropositive recipients.30
The development of TB is a well-known infectious complication in solid organ transplantation and the risk of active TB is higher than in the general population. One study in Korea reported that the incidence density of TB in solid organ transplantation was 372 cases per 100,000 patient-years, which is 4-fold higher than for the general Korean population.31 And the overall frequency of TB is reported as 1.59–1.67% in solid organ transplantation,32 which is higher than the results from the RESITRA cohort in Spain.33 Interestingly, the use of cyclosporin was an independent risk factor for subsequent TB in kidney transplantation recipients, whereas the risk was lower in recipients using tacrolimus and mycophenolate mofetil.34 Because of highly endemic nature of TB in Korea, we routinely survey, using tuberculin skin test and/or interferon-gamma release assay, all recipients pre-transplantation and if positive, adopt universal prophylaxis with isoniazid 300 mg daily for 9 months combined with vitamin B6 50 mg after transplantation.
CMV infection is a major infectious complication following solid organ transplantation and also hematopoietic stem cell transplantation.35 Although its prevalence decreased in Japan from 1996 to 2014,36 most of the population in Korea,37 China,38,39 and Taiwan40 are CMV seropositive. As a result, in most HTx cases both the donor and recipient are CMV seropositive, which has a remarkably lower risk of CMV infection than donor (+)/recipient (−) cases. However, CMV reactivation can occur with the immunosuppressive treatment. Therefore, recipient seropositive cases are considered moderate risk, being higher risk than donor (−)/recipient (−) cases.41 The 2 major approaches to CMV prevention are prophylaxis and preemptive treatment. Prophylaxis is further categorized as universal or targeted. With universal prophylaxis, all at-risk patients receive antiviral therapy for a defined post-transplantation period. With targeted or selective prophylaxis, only high-risk patients, such as lymphocyte-depleting induction therapy, are indicated. Preemptive therapy entails monitoring the patient’s CMV antigenemic status regularly and administering antiviral drugs to those with laboratory evidence of CMV replication to prevent the development of symptomatic CMV disease.42 There is still controversy regarding which of the strategies is superior, but there have been very few head-to-head comparisons of them, and each has advantages and disadvantages. If a prophylaxis strategy is used for prevention in seropositive recipients, 3 months of antiviral medication might be acceptable for HTx.42 In Korea, most hospitals use the preemptive strategy, which requires regularly monitoring CMV antigenemic status.
Cardiac allograft vasculopathy (CAV), accelerated atherosclerosis of the transplanted heart, is a leading cause of death after HTx. The prevalence of CAV diagnosed by angiography in the ISHLT registry was high at 29% and 40% at 5 and 8 years, respectively, post-transplant.43 Also, CAV is a leading cause of long-term death, accounting for up to 1 in 8 deaths beyond 1 year post-transplant.43 However, the prevalence and the severity might be less in Asian populations.11
In Korea, among 297 survivors out of 399 patients who underwent HTX between 1992 and 2014, CAV was detected in 1%, 17.6% and 39.7% overall at 1, 5, and 10 years, respectively.44 Interestingly, most cases (83%) were grade 1 and the disease showed a stationary course and only 7.4% of CAV cases showed progression over 4.8±2.1 years’ follow-up. Also, the presence of CAV did not affect long-term survival.
Similar observations were reported in Taiwan45 and Hong Kong.15 In the earlier period of HTx in 1999, among 50 Chinese patients reviewed, the cumulative incidence of CAV was 2% at 1, 2, and 4 years after transplantation.45 In Hong Kong, of the 110 patients who survived at least 1 year and underwent annual coronary angiographic assessment, the prevalence rate of CAV was 19.2%, 20.8%, and 36.6% at 2 years, 5 years and 10 years, respectively, after HTx.15 Moreover, the prevalence rate of severe CAV, defined as ≥grade 2, was only 1.9%, 5.5%, and 12% at 2 years, 5 years and 10 years, respectively, and CAV accounts for 28% of all deaths in heart transplant recipients surviving more than 1 year after transplantation.
What factors can explain this low incidence of CAV in Asian countries? Older donor age, male donor, and pretransplant coronary disease in recipients have been suggested as major risk factors for CAV.46 Also, a longer cold ischemic time was shown to cause adverse outcomes following HTx.25 In this regard, much younger recipient age and smaller proportion of pretransplant coronary disease might be the main reasons. Also, the smaller portion of remote transplantations could shorten the cold ischemic time. Whether there are race and ethnic differences in CAV incidence is still in debate,47 and warrants further study.
In some Asian countries (Taiwan, Korea, and Japan), HTx has settled, with more than 30 cases annually, and other countries are in various developmental stages. Religious conditions and legal structures are continuously exerting an influence on HTX programs. The number cases increased rapidly after settlement of the national organ procurement system in Korea, and increased rapidly in Japan after revision of organ transplant act.
Long-term survival after HTx is even better in some Asian countries than that in global registry data. A low incidence of CAV could be the main reason of better survival. This will be a main driving force for further expansion of HTx in Asia. Although there are arguments that a conservative strategy including younger donor/recipient age and less proportion of pretransplant coronary disease is merely the reason of better survival in Asia, transplantation in elderly populations48 and multi-organ transplantation cases49 also suggest better results among Asian populations.
For further expansion of HTx, more aggressive donor/recipient criteria and maximizing donor heart utilization will be necessary. In particular, aged and female donor hearts with minor echocardiographic abnormalities are less utilized, and pretransplant coronary disease patients are less benefited by HTx.
In conclusion, early and long-term results of HTx in Asian countries are similar to global registry data. Although there are many obstacles, such as religion, social taboo or legal process, Asian countries keep overcoming these and broadening the field of HTx.