Article ID: CJ-17-1084
Article ID: CJ-17-1084
Background: Minor ST-T changes are frequently observed on the electrocardiogram (ECG), but the risk of stroke associated with such changes is unclear.
Methods and Results: In 10,642 subjects from the Japanese general population, we evaluated minor and major ST-T changes (major ST depression ≥0.1 mV) on ECGs obtained at annual health examinations. At baseline, minor ST-T changes were found in 10.7% of the subjects and 0.5% had major ST-T changes. Minor ST-T changes were associated with older age, female gender, higher systolic blood pressure, presence of hyperlipidemia, and use of antihypertensive medication. There were 375 stroke events during the follow-up period (128.7±28.1 months). In all subjects, minor ST-T changes (HR, 2.10; 95% CI: 1.57–2.81) and major ST-T changes (HR, 8.64; 95% CI: 4.44–16.82) were associated with an increased risk of stroke, but the stroke risk associated with minor ST-T changes had borderline significance after adjustment for conventional risk factors (P=0.055). In subgroup analysis, the risk of stroke was significantly associated with minor ST-T changes in subjects who had hyperlipidemia (HR, 1.75; 95% CI: 1.15–2.67) compared to those without hyperlipidemia (HR, 1.01; 95% CI: 0.64–1.59; P for interaction=0.016), even after adjustment for ECG-diagnosed left ventricular hypertrophy.
Conclusions: Minor ST-T changes were particularly associated with a higher risk of stroke in subjects with hyperlipidemia and this association was independent of electrocardiographic left ventricular hypertrophy.
Left ventricular hypertrophy (LVH) can be diagnosed from an increased Sokolow-Lyon voltage (S in lead V1 and R in lead V5) and major ST-T changes (ST segment depression >0.1 mV in leads V5 or V6) on electrocardiogram (ECG). Major ST-T changes represent abnormal myocardial repolarization and are related to both anatomical LVH1,2 and diastolic dysfunction.3 It is often observed in patients with hypertension, and is a predictor of future cardiovascular risk4 and mortality.5
Minor ST-T changes (ST depression <0.1 mV with a flat or slightly negative T wave) are also observed in daily medical practice and at annual health examinations. An association has been reported between minor ST-T changes and cardiovascular disease,6–12 and Schillaci et al considered that minor ST-T changes were associated with an increased risk of ischemic heart disease in hypertensive subjects.13 In contrast, Vinyoles et al recently reported that minor ST-T changes were not associated with the risk of cardiovascular morbidity or mortality in hypertensive patients without diabetes.14 These reports suggested that the risks associated with minor ST-T changes could be influenced by the presence/absence of cardiovascular risk factors.
Although the incidence of stroke is higher than that of coronary artery disease in the general Japanese population, there has been only 1 study showing a relationship between minor ST-T changes and the risk of stroke.15 Therefore, we investigated whether minor ST-T changes were associated with an increased risk of stroke, and whether the level of risk related to minor ST-T changes was influenced by other clinical characteristics.
The Jichi Medical School (JMS) Cohort Study commenced in 1992 with the aim of clarifying the risk factors for cardiovascular and cerebrovascular disease in the general Japanese population. Details of the study protocol have been reported elsewhere.16 Baseline data were collected between April 1992 and July 1995 in 12 rural districts of Japan using a government-sponsored mass screening system. In each community, the local government office mailed letters to all potential subjects in accordance with the Health and Medical Service Law for the Aged. In 8 districts (Iwaizumi, Tako, Kuze, Sakuma, Sakugi, Okawa, Ainoshima, and Akaike), the individuals who participated in mass screening examinations were aged 40–69 years, while they were aged ≥30 years in 1 district (Wara) and belonged to other age groups in 3 districts (Hokudan, Yamato, and Takasu). At baseline, the total number of subjects enrolled in the JMS Cohort Study was 12,490 (4,911 men and 7,579 women). Exclusion criteria were as follows: no ECG, n=1,285; pacemaker implantation, n=7; atrial fibrillation, n=57; advanced atrioventricular block, n=1; complete atrioventricular block, n=1; dextrocardia, n=2; complete left bundle branch block, n=20; complete right bundle branch block, n=196; non-measurable QTc, n=27; heart rate >150 beats/min, n=1; incomplete data, n=5; no follow-up data, n=84; no Cornell product, n=7; previous stroke, n=104; previous myocardial infarction (MI), n=50; and unclear ST-T data, n=1. Hence, the final number of subjects analyzed in this study was 10,642.
Questionnaire and Other MeasurementsInformation about each subject’s medical history and lifestyle was obtained at baseline using a questionnaire that included items about past illnesses, present illnesses, and any heart disease of the subject’s parents. The ages reported in this study are baseline data. Smoking status was classified as current smoker or not. Habitual alcohol drinking was defined as drinking ≥20 g alcohol daily. Body mass index (BMI) was calculated as weight (kg)/height (m)2. Systolic and diastolic blood pressures (SBP and DBP) were recorded at baseline using a fully automated sphygmomanometer (BP203RV-II Nippon Colin, Komaki, Japan), with a single reading being obtained after the subject had rested for ≥5 min in the sitting position. Hypertension was defined as SBP ≥140 mmHg and/or DBP ≥90 mmHg, or use of antihypertensive medication. Diabetes mellitus was defined as fasting glucose >7.0 mmol/L (126 mg/dL), random glucose >11.1 mmol/L (200 mg/dL), or use of oral hypoglycemic agents or insulin. Hyperlipidemia was defined as total cholesterol >5.7 mmol/L (220 mg/dL), triglycerides >1.7 mmol/L (150 mg/dL), or use of oral lipid-lowering agents, according to the Japan Atherosclerosis Society Guidelines for the Prevention of Atherosclerotic Cardiovascular Diseases.17
ECGThe ECG was recorded at a paper speed of 25 mm/s and a gain of 10 mm/mV (or 5 mm/mV), using the ECG devices of each institution. Initially, the first author evaluated ST-T changes according to reported criteria.13 Details of measurement of Sokolow-Lyon voltage, Cornell voltage, and Cornell product have been reported previously.18,19 Cornell product was the product of the Cornell voltage multiplied by QRS duration afterward. Sokolow-Lyon LVH was defined as ≥3.8 mV and Cornell product LVH was defined as ≥244 mV×ms according to the Losartan Intervention for Endpoint Reduction in Hypertension Study.20
Informed ConsentThe internal review board of Jichi Medical University School of Medicine approved this study. Written informed consent to participate in the study was obtained from each individual who underwent mass screening health examinations at baseline.
Follow-upThe mass screening examination system was used to assess all subjects every year for 10 years. During each examination, the subjects were asked directly whether a stroke or cardiovascular disease had occurred since enrollment in this study. If a subject did not attend a scheduled annual screening examination, the person or family was contacted by mail or telephone to confirm whether any cardiovascular events or death had occurred. If a subject visited a medical center due to a cardiovascular event or died at a medical center, a doctor or nurse associated with the JMS Cohort study visited the institution and checked the subject’s medical records. When an incident case was suspected, copies of brain computed tomography or magnetic resonance imaging (suspected cerebrovascular event) were obtained. If a subject died during the follow-up period and the family could not be contacted, death certificate data were collected from public health centers with the permission of the Agency of General Affairs and the Ministry of Health Labor and Welfare. Information regarding changes of residence that occurred during the study period was obtained annually from each municipal government.
Diagnostic CriteriaDiagnoses were determined independently by a diagnosis committee composed of radiologists, neurologists, and cardiologists. Questionnaire responses and copies of each subject’s medical records were used to assess whether any of the following events had occurred: cardiac death, vascular death, stroke death, sudden cardiac death, non-fatal MI, or non-fatal stroke. The detailed definitions of stroke events have been reported previously.21
Statistical AnalysisResults are shown as mean±SD or as percentages. One-way analysis of variance was performed to evaluate overall differences in continuous measures in subjects with (1) no ST-T changes; (2) minor ST-T changes; and (3) major ST change, while Tukey’s honestly significant difference test was used for comparison of means between these groups. Chi-squared test was used to detect intergroup differences in the frequencies of categorical measures. Logistic regression analysis was performed to identify the strongest demographic and clinical predictors of minor and major ST-T changes. Kaplan-Meier failure curves for the 3 groups are presented and the log-rank test is used to test the difference in these unadjusted survival curves. Adjusted hazard ratios (HR) and 95% CI for stroke events were obtained from a Cox proportional hazards regression analysis that included the following covariates (conventional cardiovascular risk factors that could be related to the risk of LVH):18,19,22,23 age, sex, BMI (as a continuous variable), current smoking, alcohol intake >20 g/day, SBP (as a continuous variable), antihypertensive medication, heart rate, hyperlipidemia, and diabetes in model 1. In model 2, presence of LVH by Cornell product was added to model 1, because LVH diagnosed on Cornell product has been shown to be more strongly related to stroke risk than LVH diagnosed on Sokolow-Lyon voltage.18 P<0.05 was considered statistically significant. SPSS version 18.0 (SPSS, Chicago, IL, USA) was used for all analyses.
The characteristics of the total sample (n=10,642) and according to ST-T change status are listed in Table 1. At baseline, the mean age was 55.4±11.2 years and 37.6% of them were men. In this study of the general Japanese population, the prevalence of minor ST-T change was 10.7% and that of major ST-T change was 0.5% (female, 13.7% and 0.5%; male, 5.4% and 0.6%, respectively).
| All subjects (n=10,642) |
ST-T change | P-value | |||
|---|---|---|---|---|---|
| None (n=9,462) | Minor (n=1,124) | Major (n=56) | |||
| Age (years) | 55.4±11.2 | 54.9±11.2 | 59.2±10.0***,§ | 64.0±7.3***,§,**,¶ | <0.001† |
| Male | 37.6 | 39.8 | 19.2 | 42.9 | <0.001‡ |
| BMI (kg/m2) | 23.1±3.1 | 23.0±3.1 | 23.7±3.2***,§ | 23.7±4.3 | <0.001† |
| Current smoking | 22.5 | 23.8 | 11.3 | 32.7 | <0.001‡ |
| Habitual alcohol drinking | 31.9 | 31.6 | 34.4 | 45.2 | 0.034‡ |
| SBP (mmHg) | 129.4±21.0 | 127.9±20.3 | 140.5±22.2***,§ | 151.1±27.0***,§,**,¶ | <0.001† |
| DBP (mmHg) | 77.5±12.3 | 76.8±12.1 | 82.9±12.4***,§ | 85.8±14.4***,§ | <0.001† |
| Hypertension | 33.9 | 31.0 | 56.2 | 78.6 | <0.001‡ |
| Antihypertensive drugs | 11.1 | 9.7 | 20.9 | 40.0 | <0.001‡ |
| Diabetes | 3.6 | 3.4 | 4.9 | 7.1 | 0.014‡ |
| Hyperlipidemia | 35.9 | 34.9 | 43.4 | 42.9 | <0.001‡ |
| Total cholesterol (mg/dL) | 192.6±35.0 | 191.8±34.9 | 199.6±34.8***,§ | 198.8±38.9 | <0.001† |
| Triglyceride (mg/dL) | 117.3±76.4 | 116.5±75.9 | 123.7±80.6**,§ | 126.4±71.4 | 0.008† |
| HDL-C (mg/dL) | 51.2±13.0 | 51.2±13.0 | 50.9±13.1 | 50.8±12.7 | 0.680† |
| SL voltage (mV) | 26.8±8.3 | 26.5±8.1 | 28.2±9.2***,§ | 39.6±11.5***,§,¶ | <0.001† |
| LVH on SL voltage | 9.5 | 8.6 | 14.4 | 48.2 | <0.001‡ |
| CP (mV×ms) | 150.7±58.2 | 148.0±56.6 | 169.0±63.0***,§ | 236.8±90.3***,§,¶ | <0.001† |
| LVH on CP | 6.3 | 5.6 | 10.5 | 37.5 | <0.001‡ |
Data given as mean±SD or %. †ANOVA; ‡chi-squared test. **P<0.01, ***P<0.001 §vs. no ST-T change, ¶vs. minor ST-T change (Tukey’s honestly significant differences test). BMI, body mass index; CP, Cornell product; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; LVH, left ventricular hypertrophy; SBP, systolic blood pressure; SL, Sokolow-Lyon.
The subjects with minor or major ST-T change were older than those without ST-T change and had higher SBP and DBP, as well as a higher prevalence of hypertension, use of antihypertensive medication, diabetes, hyperlipidemia, and electrocardiographic LVH. The subjects with minor ST-T change were much more likely to be female and less likely to be current smokers than those without ST-T change, while the opposite associations were observed between the subjects with major ST-T change and those without ST-T change (Table 1).
Determinants of ST-T ChangeOlder age, SBP, and antihypertensive medication use were strong predictors of both minor and major ST-T change. In addition, female sex and hyperlipidemia were strong predictors of minor ST-T change, and current smoking was a strong predictor of major ST-T change (Table 2).
| Minor ST-T change | Major ST change | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | |||
| Age (per 1 year) | 1.02 | 1.01 | 1.03 | <0.001 | 1.08 | 1.04 | 1.13 | <0.001 |
| Male | 0.33 | 0.27 | 0.40 | <0.001 | 0.78 | 0.36 | 1.69 | 0.523 |
| BMI (per 1 kg/m2) | 0.99 | 0.97 | 1.01 | 0.426 | 1.02 | 0.92 | 1.14 | 0.646 |
| Current smokers | 0.81 | 0.62 | 1.04 | 0.095 | 3.34 | 1.49 | 7.48 | 0.003 |
| Alcohol drinking habit | 1.15 | 0.98 | 1.33 | 0.079 | 1.75 | 0.93 | 3.29 | 0.081 |
| SBP (per 1 mmHg) | 1.03 | 1.02 | 1.03 | <0.001 | 1.03 | 1.01 | 1.04 | <0.001 |
| Antihypertensive medication use | 1.23 | 1.01 | 1.51 | 0.040 | 2.34 | 1.16 | 4.68 | 0.017 |
| Hyperlipidemia | 1.18 | 1.01 | 1.37 | 0.036 | 1.18 | 0.61 | 2.29 | 0.622 |
| Diabetes | 1.36 | 0.96 | 1.92 | 0.081 | 0.78 | 0.18 | 3.30 | 0.734 |
†Multivariable logistic regression analysis. BMI, body mass index; SBP, systolic blood pressure.
During the mean follow-up period of 128.7±28.1 months (114,132 total person-years), there were a total of 375 stroke events (85 cerebral hemorrhages, 242 ischemic strokes, 47 subarachnoid hemorrhages, and 1 stroke event of unknown etiology). During the follow-up period, there were 292 incident stroke events in the 9,462 subjects without ST-T change (101,776 person-years); 70 stroke events in the 1,124 subjects with minor ST-T change (11,872 person-years); and 13 events in the 56 subjects with major ST-T change (484 person-years) at baseline. On Kaplan-Meier analysis, the cumulative 10-year incidence of stroke was 2.6% in those without ST-T change; 5.6% in those with minor ST change; and 21.4% in those with major ST change (P<0.001, log-rank test of group differences in failure curves) (Figure 1). On unadjusted Cox regression analysis, the risk of stroke in subjects with minor ST-T change was more than double (2.10-fold as great) that for those without ST-T change. The adjusted risk associated with minor ST-T change, however, was only 1.35-fold as great (marginally significant) after adjustment for conventional cardiovascular risk factors, including age, gender, BMI, smoking status, alcohol intake, SBP, antihypertensive medication, diabetes, and hyperlipidemia, but the increase in adjusted risk (51% increase) for ischemic stroke in those with minor ST-T change remained significant (Table 3). Subjects with major ST-T change had a significantly higher risk of stroke than those without ST-T change, both before and after adjustment for conventional cardiovascular risk factors and LVH diagnosed by the Cornell product.

Kaplan-Meier cumulative incidence of stroke vs. ST-T change status.
| Total stroke | Cerebral hemorrhage | Ischemic stroke | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | P-value† | HR | 95% CI | P-value† | HR | 95% CI | P-value† | |
| Unadjusted model | |||||||||
| No ST-T change | 1.00 | 1.00 | 1.00 | ||||||
| Minor ST-T change | 2.10 | 1.57–2.81 | <0.001 | 2.00 | 1.07–3.75 | 0.030 | 2.32 | 2.32–1.63 | <0.001 |
| Major ST-T change | 8.64 | 4.44–16.82 | <0.001 | 8.61 | 2.10–35.34 | 0.003 | 10.91 | 10.91–5.11 | <0.001 |
| Model 1: adjusted for conventional risk factors | |||||||||
| No ST-T change | 1.00 | 1.00 | 1.00 | ||||||
| Minor ST-T change | 1.35 | 0.99–1.83 | 0.055 | 1.31 | 0.68–2.52 | 0.424 | 1.51 | 1.04–2.19 | 0.032 |
| Major ST-T change | 3.41 | 1.73–6.73 | <0.001 | 3.72 | 0.88–15.79 | 0.075 | 4.37 | 2.01–9.47 | <0.001 |
| Model 2: adjusted for CP LVH in addition to model 1 | |||||||||
| No ST-T change | 1.00 | 1.00 | 1.00 | ||||||
| Minor ST-T change | 1.32 | 0.97–1.78 | 0.078 | 1.28 | 0.66–2.47 | 0.459 | 1.47 | 1.01–2.14 | 0.042 |
| Major ST-T change | 3.07 | 1.55–6.06 | 0.001 | 3.34 | 0.78–14.29 | 0.103 | 4.04 | 1.85–8.82 | <0.001 |
†Cox hazard model. Age, sex, body mass index, systolic blood pressure, presence of diabetes, presence of hyperlipidemia, current smoking, and hyperlipidemia were included in model 1. CP, Cornell product; LVH, left ventricular hypertrophy.
On exploratory analysis of possible effect modifications, the risk of stroke associated with minor ST-T change differed significantly according to presence of hyperlipidemia (P for interaction=0.016) in the model adjusted for conventional cardiovascular risk factors and LVH diagnosed by the Cornell product (Figure 2). In contrast, the risk of stroke associated with major ST-T change did not differ significantly according to any of the conventional risk factors (Figure 3). Kaplan-Meier plots of the cumulative incidence of stroke according to hyperlipidemia and ST change status are shown in Figure 4.

Cox hazard ratios for the incidence of stroke associated with minor ST-T changes according to conventional cardiovascular risk factors. BMI, body mass index; CP LVH, Cornell product left ventricular hypertrophy; SBP, systolic blood pressure.
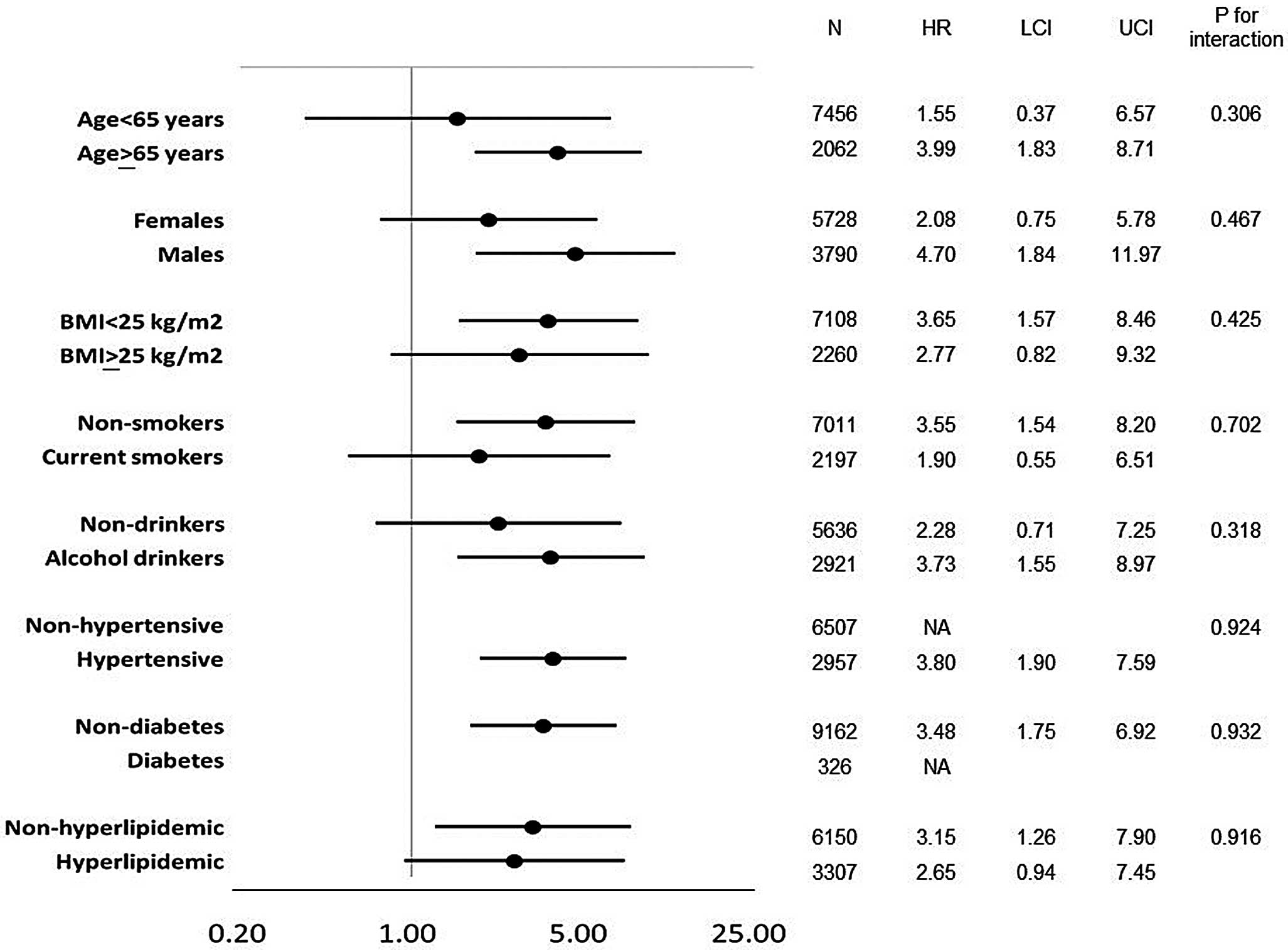
Cox hazard ratios for the incidence of stroke associated with major ST-T according to conventional cardiovascular risk factors. Abbreviations as in Figure 2.

Kaplan-Meier cumulative incidence of stroke according to ST-T change, in patients (A) without or (B) with hyperlipidemia.
Minor ST-T change was observed on ECG in approximately 10% of Japanese subjects undergoing annual health screening. The risk of stroke associated with minor ST-T change was influenced only by the presence or absence of hyperlipidemia (effect modification); the risk of stroke itself was influenced by conventional cardiovascular risk factors. Because of the association of minor ST-T change with conventional CV risk factors, the estimated risk due to minor ST-T change depends on whether or not the conventional CV risk factors are controlled for. This study showed that minor ST changes were associated with an increased risk of stroke even after adjustment for ECG LVH and conventional cardiovascular risk factors, in subjects with hyperlipidemia.
The present study cannot elucidate the mechanism by which hyperlipidemia influences the risk of stroke associated with minor ST-T change. Hyperlipidemic subjects might have occult coronary artery disease, although we carefully excluded all subjects who had a history of heart disease or apparent ECG abnormalities suggestive of previous MI (e.g., a QS pattern in the anterior chest leads). It is possible that the subjects with hyperlipidemia had both cerebral atherosclerosis and subtle hypertensive target organ damage in the heart causing minor ST-T change. The subjects with hyperlipidemia might have pericardial fat and intramyocardial fat deposition, leading to endocardial ischemia. Thus, careful observation may be required in persons with both hyperlipidemia and minor ST-T change. Atorvastatin has been reported to improve late cardiac remodeling by altering collagen metabolism in a rat model of MI,24 and statins have been reported to reduce the incidence of stroke in hypertensive patients.25
ST-T abnormalities might reflect the cumulative effect of long-term hypertension. Aging and higher SBP were determinants of both minor and major ST-T change. In a Spanish ambulatory blood pressure registry for 24,351 hypertensive patients,26 dyslipidemia was related to poor control of both office and ambulatory blood pressure, and it was also associated with LVH. Ohira et al reported that 46% of minor ST-T abnormalities at baseline had reverted to normal ST-T; 45% remained abnormal; and 9% changed to major ST-T abnormalities during the 15.4-year follow-up period: age-adjusted relative risks of total stroke tended to be higher for men with 2 recorded occurrences of minor ST-T abnormalities than for men with only 1 recorded occurrence.15 Additionally, progression from minor ST-T change to major ST-T change was associated with an increased risk of cardiovascular disease.27 This suggests that subjects with major ST-T change had more advanced hypertensive target organ damage in the heart, compared with those with minor ST-T change.
In contrast, there were some differences in the determinants of minor and major ST-T change (i.e., presence of hyperlipidemia and being female for minor ST-T change; and current smoking for major ST-T change). Hyperlipidemia might induce fat deposition in the heart and atherosclerosis in the coronary artery (i.e., minor ST-T change). After having hypertensive target organ damage (i.e., major ST-T change), aging and increased SBP would be more important risk markers of incident stroke events than hyperlipidemia. Major ST-T change was associated with an increased risk of stroke regardless of the presence or absence of hyperlipidemia. Both minor and major ST-T change were markers of LVH, but there might be a different stage in pathophysiology for incidence of stroke.
There were some limitations of this study: (1) we evaluated ST depression as a categorical variable; (2) diagnosis of ST-T change was not obtained by Minnesota code, because most of the ECG devices did not have the automatic analysis system between 1992 and 1995; but it is reassuring that the prevalence of minor ST-T change did not differ from a previous report in a general Japanese population;15 (3) follow-up ECG data were not obtained; therefore, data on the occurrence of atrial fibrillation during the follow-up period were not available; (4) hyperlipidemia was defined by total cholesterol and triglycerides, and follow-up assessment of hyperlipidemia was not systematically collected from all subjects; (5) although use of lipid-lowering drugs was assessed, patient adherence to statins was not; (6) we could not exclude subjects who had hypertrophic cardiomyopathy because we did not obtain echocardiographic data, but we excluded subjects with giant negative T wave suggestive of hypertrophic cardiomyopathy; and (7) there were no data on antiplatelet or anticoagulant drug use in this cohort.
Minor ST-T change on ECG was associated with an increased risk of stroke, especially in subjects with hyperlipidemia, but this interaction was not observed for major ST-T changes. Careful observation may be required in those persons with minor ST-T change and also hyperlipidemia.
This study was supported by a Grant-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology, Japan, and grants from the Foundation for the Development of the Community, Tochigi, Japan.
Members of the diagnostic committee are as follows: Makoto Furuse, former radiologist; Shinichi Muramatsu, Division of Neurology, Department of Medicine, Jichi Medical University; Tadataka Kawakami, Department of Neurology, Shin-Oyama City Hospital; Yoshihito Ando, Division of Neurology, Department of Medicine, Jichi Medical University; Takeshi Mitsuhashi, Division of Cardiovascular Medicine, Department of Medicine, Jichi Medical University.
The authors declare no conflicts of interest.