Article ID: CJ-17-1334
Article ID: CJ-17-1334
Background: We investigated the prevalence and prognostic significance of functional mitral regurgitation (MR) and tricuspid regurgitation (TR) in patients with atrial fibrillation (AF) and preserved left ventricular ejection fraction (LVEF).
Methods and Results: We retrospectively studied the cases of 11,021 consecutive patients who had undergone transthoracic echocardiography. AF appeared in 1,194 patients, and we selected 298 with AF and LVEF ≥50% but without other underlying heart diseases. Moderate or greater (significant) degree of functional MR and of TR was seen in 24 (8.1%) and in 44 (15%) patients, respectively (P=0.0045). In contrast, significant MR and TR were more frequently seen in patients with AF duration >10 years (28% vs. 25%, respectively). During the follow-up period of 24±17 months, 35 patients (12%) met the composite endpoint defined as cardiac death, admission due to heart failure, or mitral and/or tricuspid valve surgery. On Cox proportional hazard ratio analysis, both MR and TR grading predicted the endpoint, independently of other echocardiographic parameters. On Kaplan-Meyer analysis, presence of both significant functional MR and TR was associated with poor prognosis, with an event-free rate of only 21% at the mean follow-up period of 24 months.
Conclusions: Significant functional MR and TR are seen in a substantial proportion of patients with longstanding AF, despite preserved LVEF. This MR/TR combination predicts poor outcome for AF patients, who may have to be treated more intensively.
The incidence of atrial fibrillation (AF) increases with age,1–3 and heart failure (HF) is the most important cause of mortality in elderly AF patients.4–6 AF can develop after HF, but it can also precede HF with reduced left ventricular ejection fraction (LVEF) or HF with preserved LVEF.7–9 Patients with AF and subsequent HF have a poor prognosis, but the determinants that generate HF in AF patients are still uncertain.
Secondary (functional) mitral regurgitation (MR) and tricuspid regurgitation (TR) can occur as a result of atrial dilatation in AF patients, despite having preserved left ventricular (LV) systolic function.10–16 These can be termed “atrial functional MR” and “atrial functional TR,” respectively. Both atrial functional MR and TR resulting from atrial dilatation have recently received much attention, but little information is available regarding the disease characteristics of these valvular regurgitations and their impacts on HF. In addition, very few descriptions are available for the MR and TR secondary to AF in the current guidelines for valvular heart disease.17,18 The aim of the present retrospective analysis was therefore to investigate the prevalence and the prognostic significance of the occurrence of functional MR and TR despite preserved LV systolic function in patients with AF.
We retrospectively analyzed the echocardiography laboratory database and the medical records at Osaka City General Hospital, Osaka, Japan. We selected patients with AF and preserved LVEF (≥50%) who underwent transthoracic echocardiography (TTE) in the echocardiography laboratory over a period of 2 consecutive years (June 2012–May 2014). We excluded patients with acute decompensated HF (ADHF), a moderate or greater degree of organic valvular heart disease, apparent degenerative changes in mitral or tricuspid valve complex, a history of coronary artery disease or regional LV wall motion abnormality suggesting myocardial ischemia or infarction, or a definite diagnosis of cardiomyopathy. Patients who had undergone cardiac device implantation or cardiac surgery, patients with AF spontaneously or therapeutically defibrillated within 1 week after TTE, and patients with <1 week of follow-up data were also excluded. In patients who underwent repeated TTE for the 2 years, the earliest TTE was considered as the entry point into the study, and the repeated TTE were excluded.
The clinical, electrocardiographic (ECG), and echocardiographic data at TTE were retrospectively collected. Clinical data included demographics, presenting symptoms, cardiovascular risk factors, and medical treatment at TTE. The clinical information parameters are listed in Table 1. The duration of AF was estimated if the ECG data or other specific information in the medical record were available. The echocardiographic data were collected from the TTE database. The occurrence of cardiac events after TTE was also recorded, and the primary composite endpoint was defined as cardiac death that included sudden death with an unknown cause, hospitalization due to worsening HF, or mitral valve and/or tricuspid valve repair. According to the consensus of the Department of Cardiology and Department of Cardiovascular Surgery, Osaka City General Hospital, we usually performed mitral valve repair and concomitant tricuspid valve repair in patients who had permanent AF that had persisted for >1 year, chronic moderate or severe MR with at least mild TR, chronic HF symptoms of at least New York Heart Association (NYHA) functional class II, and at least 1 prior admission for ADHF complicated by severe MR.12
| Significant (≥moderate) MR and TR | A priori P-value |
||||
|---|---|---|---|---|---|
| Neither MR nor TR (n=241) |
Only TR (n=33) |
Only MR (n=13) |
Both MR and TR (n=11) |
||
| Age (years) | 71±10 | 78±9*,† | 69±13*,‡ | 80±7*,†,§ | <0.001 |
| Men | 155 (64) | 12 (36)*,† | 6 (46) | 5 (45) | 0.009 |
| NYHA functional class | 1.2±0.4 | 1.5±0.6*,† | 1.6±0.8*,† | 1.8±0.6*,† | <0.001 |
| Prior HF admission | 27 (11) | 7 (21) | 6 (46)*,† | 7 (64)*,†,‡ | <0.001 |
| Hypertension | 125 (52) | 17 (52) | 7 (54) | 5 (45) | 0.98 |
| Diabetes mellitus | 68 (28) | 4 (12) | 1 (8) | 1 (9) | 0.050 |
| Dyslipidemia | 71 (29) | 10 (30) | 1 (8) | 2 (18) | 0.32 |
| Digitalis | 61 (25) | 15 (45) | 6 (46) | 5 (45) | 0.030 |
| ACEI or ARB | 91 (38) | 11 (33) | 5 (38) | 7 (64) | 0.35 |
| β-blocker | 86 (36) | 11 (33) | 7 (54) | 4 (36) | 0.60 |
| Aldosterone antagonist | 32 (13) | 10 (30) | 2 (15) | 5 (45) | 0.005 |
| Other diuretics | 78 (32) | 17 (52) | 9 (69)*,† | 8 (73)*,† | <0.001 |
| Anticoagulant agents | 170 (70) | 27 (82) | 10 (77) | 10 (91) | 0.25 |
| Statins | 48 (20) | 9 (27) | 0 (0) | 0 (0) | 0.067 |
Data given as mean±SD or n (%). *P<0.05 vs. †patients with neither MR nor TR, ‡patients with only TR, or §patients with only MR (post-hoc test). ACEI, angiotensin-converting enzyme inhibitor; AF, atrial fibrillation; ARB, angiotensin receptor blocker; HF, heart failure; LVEF, left ventricular ejection fraction; MR, mitral regurgitation; NYHA, New York Heart Association; TR, tricuspid regurgitation.
This study was approved by the institutional review board, with a waiver of individual consent.
EchocardiographyAll TTE was performed by expert level 3 sonographers according to the American Society of Echocardiography definition,19 and the results were interpreted by experienced attending doctors in the echocardiography laboratory. Any disagreements were resolved on consensus reading.
For all measurements of systolic parameters in AF patients, 1 beat occurring after 2 serial beats with average RR interval was carefully selected.20 For all measurements of diastolic Doppler parameters in AF patients, 1 beat with an average Doppler-wave contour with an average velocity was visually, but carefully, selected. The LV end-diastolic dimension, LV end-systolic dimension, LVEF, LV mass, and left atrial (LA) dimension were measured according to the guidelines.21 We indexed these parameters by dividing them by the body surface area. The severity of the MR was defined using a multiparametric approach, including an assessment of the color Doppler-derived jet area, the effective regurgitant orifice area using the proximal isovelocity surface area method, the MR volume and fraction using the Doppler-derived volumetric method, and the pulmonary vein flow velocity pattern.22 TR grade was also defined using a multiparametric approach, including an assessment of the color Doppler-derived jet area, the continuous wave Doppler-derived jet density and contour, and the hepatic vein flow velocity pattern.22 The methods for the assessments of these valvular regurgitations were selected per patient under the careful consideration of the methodological advantages and limitations, according to the American Society of Echocardiography guidelines.22 MR and TR were graded as none, mild, moderate, or severe. When a considerable discrepancy was evident in the grading between the multiple methods or between the different beats in AF patients, we used the following 3 levels of borderline grading: none-mild; mild-moderate; and moderate-severe. For the statistical analysis, the grading was scored as follows: none, 0; none-mild, 0.5; mild, 1; mild-moderate, 1.5; moderate, 2; moderate-severe, 2.5; and severe, 3. A ≥moderate degree of MR or TR (i.e., 2, 2.5, or 3) was defined as significant in the present study. Continuous wave Doppler was used to obtain the TR peak velocity (v, m/s) and the transtricuspid systolic pressure gradient (mmHg), which was calculated as 4×v2. The right ventricular systolic pressure (RVSP) was then estimated as the sum of the estimated transtricuspid systolic pressure gradient and right atrial (RA) pressure. The RA pressure was estimated as follows: an inferior vena cava (IVC) diameter ≤2.1 cm that collapsed by ≥50% with a sniff was considered to indicate a normal RA pressure of 3 mmHg, whereas an IVC diameter >2.1 cm that collapsed <50% with a sniff was considered to indicate a high RA pressure of 15 mmHg. In scenarios in which the IVC diameter and collapse did not fit this paradigm, an intermediate value of 8 mmHg was assigned.23 The transmitral flow velocity curves in diastole and the mitral annular tissue Doppler imaging signals were obtained as previously described.24 The peak velocity of early diastolic flow across the mitral valve (E) and the deceleration time were measured. The peak early diastolic tissue Doppler velocity of the medial mitral annulus (e’) on apical 4-chamber view was measured, and the E/e’ ratio was calculated.
Statistical AnalysisThe categorical variables are expressed as absolute values and percentages and were compared using chi-squared test, McNemar test, or Kruskal-Wallis test followed by post-hoc pairwise test. The continuous variables are expressed as mean±SD and were compared using 1-way analysis of variance followed by the post-hoc Tukey-Kramer test, or Kruskal-Wallis test followed by the post-hoc pairwise test. The significant predictors of the primary endpoint were identified on univariate Cox proportional hazards regression analysis. We then performed a multivariate Cox proportional hazards regression analysis based on stepwise selection with a model using significant clinical predictors and a model using significant echocardiographic predictors to determine the independent predictors of the primary endpoint. The Kaplan-Meier method was used to evaluate event-free survival. Statistical analysis was performed using MedCalc (version 15.8, MedCalc Software, Ostend, Belgium). P<0.05 was considered statistically significant.
Subject selection is shown in Figure 1. Of a total of 11,021 patients who underwent TTE in the echocardiography laboratory for the 2 years, 1,194 (11%) had AF at TTE. We excluded 580 patients who met the exclusion criteria and 245 TTE repeated in the same patients. Of the remaining patients, 298 (2.7% of the total cohort) had LVEF ≥50%, and constituted the final study cohort. All data for the clinical and echocardiographic parameters were collected with missing values <5%, except for AF duration, E/e’, and estimated RVSP, which had missing values of 56%, 6% and 24%, respectively. Therefore, we excluded AF duration, E/e’, and estimated RVSP from the subsequent Cox hazard proportional hazards regression analysis.

Flow diagram of subject selection. AF, atrial fibrillation; CAD, coronary artery disease; LVEF, left ventricular ejection fraction; TTE, transthoracic echocardiography; VHD, valvular heart disease.
Of the 298 patients, 241 (81%) were referred from the outpatient departments. The remaining 57 (19%) were referred from the wards, whereas all of them had stable conditions before discharge. The mean age of the 298 patients was 72±10 years, and 178 (60%) were male. In these patients, significant MR and TR, defined as ≥moderate MR and TR, were seen in 24 (8.1%) patients and in 44 (15%) patients, respectively (P=0.0045; Figure 2). Only 11 (3.7%) had both significant MR and significant TR.

Distribution of the severity of mitral and tricuspid regurgitations (MR and TR). Significant, defined as moderate or greater.
Patient characteristics according to significant MR and TR status are listed in Table 1. The patients with both significant MR and significant TR had the highest age (80±7 years old), the highest NYHA functional class (1.8±0.6), and the most frequent history of prior admission due to HF (64%). The echocardiographic data according to significant MR and TR status are listed in Table 2. The patients with both significant MR and significant TR had the largest LV diastolic dimension index (35±5 mm/m2), LV systolic dimension index (23±5 mm/m2), LA dimension index (37±8 mm/m2), and estimated RVSP (42±12 mmHg). In contrast, LVEF was similar regardless of the presence or absence of significant MR and TR.
| Significant (≥moderate) MR and TR | A priori P-value |
||||
|---|---|---|---|---|---|
| Neither MR nor TR (n=241) |
Only TR (n=33) |
Only MR (n=13) |
Both MR and TR (n=11) |
||
| LV mass index (g/m2) | 88±23 | 88±19 | 122±56*,†,‡ | 116±38*,†,‡ | 0.007 |
| LVDd index (mm/m2) | 27±4 | 29±4*,† | 33±5*,†,‡ | 35±5*,†,‡ | <0.001 |
| LVDs index (mm/m2) | 17±3 | 19±3*,† | 21±4*,† | 23±5*,†,‡ | <0.001 |
| LVEF (%) | 66±7 | 64±8 | 64±6 | 64±7 | 0.49 |
| LA dimension index (mm/m2) | 26±5 | 30±6*,† | 35±5*,†,‡ | 37±8*,†,‡ | <0.001 |
| E wave velocity (cm/s) | 85±20 | 96±28*,† | 117±41*,† | 110±24*,† | <0.001 |
| DT (ms) | 179±47 | 174±37 | 175±47 | 171±58 | 0.90 |
| e’ (cm/s) | 8.2±2.4 | 7.9±2.1 | 7.3±2.8 | 8.6±2.1 | 0.60 |
| E/e’ | 11.4±4.7 | 12.9±6.2 | 17.3±6.9*,† | 13.6±5.0 | 0.001 |
| Estimated RVSP (mmHg) | 28±7 | 37±13*,† | 34±10*,† | 42±12*,† | <0.001 |
Data given as mean±SD. *P<0.05 vs. †patients with neither MR nor TR, and ‡patients with only TR, and (post-hoc test). Dd, diastolic dimension; Ds, systolic dimension; DT, deceleration time; LA, left atrial; LV, left ventricular; RVSP, right ventricular systolic pressure. Other abbreviations as in Table 1.
The duration of AF was retrospectively confirmed on ECG or on the description in the medical records in 131 (44%) of the 298 patients. The relationship between AF duration and the prevalence of significant (≥moderate) MR or TR is shown in Figure 3. Of the patients with AF duration ≤1 year, 3% and none had significant MR and significant TR, respectively. In contrast, of the patients with AF duration >10 years, approximately one-fourth (28% and 25%) had significant MR and significant TR, respectively.

Prevalence of significant (i.e., moderate or greater) mitral or tricuspid regurgitation (MR or TR) vs. duration of atrial fibrillation (AF). Blue, not significant; orange, significant.
During the follow-up period of 24±17 months (median, 32 months; range, 0.3–54 months), 35 patients (12%) met the primary endpoint, consisting of 5 cardiac deaths, 23 hospitalizations due to ADHF, and 7 mitral valve and tricuspid valve repairs. In contrast, only 7 patients (2.3%) had cerebral infarction, and only 4 (1.3%) had major hemorrhagic events, including 3 intracranial hemorrhages and 1 traumatic intramuscular hematoma at the shoulder. Table 3 lists the results of the Cox proportional hazards regression analysis to identify the predictors of the primary endpoint. In the model using clinical data, the factors of age, NYHA functional class, history of prior admission due to HF, and absence of dyslipidemia could independently predict the endpoint. In the model using echocardiographic data, both the MR grade and the TR grade could predict the endpoint independently of each other and independently of other echocardiographic parameters. The hazard ratios per 1-grade increase in MR and TR were 4.0 (95% CI: 2.3–7.0) and 1.8 (95% CI: 1.1–2.9), respectively.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | |
| Model using clinical data | ||||||
| Age (per 10-year increase) | 2.2 | 1.4–3.5 | 0.0005 | 1.8 | 1.1–2.9 | 0.011 |
| NYHA functional class | 3.0 | 1.8–4.8 | <0.0001 | 2.2 | 1.4–3.6 | 0.0015 |
| Prior HF admission | 4.4 | 2.3–8.6 | <0.0001 | 4.1 | 2.1–8.2 | <0.0001 |
| Dyslipidemia | 0.31 | 0.11–0.88 | 0.027 | 0.32 | 0.11–0.92 | 0.034 |
| Aldosterone antagonist | 2.1 | 1.02–4.5 | 0.043 | – | – | – |
| Other diuretics | 2.3 | 1.2–4.6 | 0.015 | – | – | – |
| Model using echocardiographic data | ||||||
| LV mass index (g/m2) (per 10-g/m2 increase) | 1.2 | 1.1–1.3 | <0.0001 | – | – | – |
| LVDd index (mm/m2) | 1.2 | 1.1–1.3 | <0.0001 | – | – | – |
| LVDs index (mm/m2) | 1.2 | 1.1–1.3 | <0.0001 | – | – | – |
| LA dimension index (mm/m2) | 1.13 | 1.09–1.2 | <0.0001 | – | – | – |
| MR grade (per 1-grade increase) | 5.0 | 3.3–7.5 | <0.0001 | 4.0 | 2.3–7.0 | <0.0001 |
| TR grade (per 1-grade increase) | 3.3 | 2.3–4.8 | <0.0001 | 1.8 | 1.1–2.9 | 0.0012 |
| E wave velocity (cm/s) (per 10-cm/s increase) | 1.3 | 1.2–1.5 | <0.0001 | – | – | – |
†Cardiac death, hospitalization due to worsening heart failure, or mitral valve and/or tricuspid valve repair. Abbreviations as in Tables 1,2.
On Kaplan-Meyer analysis, patients with significant functional MR had poorer prognosis than patients without significant functional MR: the event-free rate was 39% with the standard error of 11%, vs. 94% with the standard error of 2%, respectively, at mean follow-up of 24 months (log rank P<0.0001; Figure 4A). As well, the patients with significant functional TR had poorer prognosis than patients without significant functional TR: the event-free rate was 69% with the standard error of 8% vs. 93% with the standard error of 2%, respectively, at mean follow-up of 24 months (log rank P<0.0001; Figure 4B). We excluded mitral and tricuspid valve repairs from the endpoint to avoid possible intentional bias in surgical indication, but prognosis was still poorer for patients with significant functional MR than without significant functional MR: the event-free rate was 53% with the standard error of 13% vs. 95% with the standard error of 2%, respectively, at mean follow-up of 24 months (log rank P<0.0001; Figure 4C). As well, prognosis was poorer for the patients with significant functional TR than without significant functional TR, even after the exclusion of surgical valve repairs from the endpoint: the event-free rate was 74% with the standard error of 8% vs. 95% with the standard error of 2%, respectively, at mean follow-up of 24 months (log rank P<0.0001; Figure 4D).
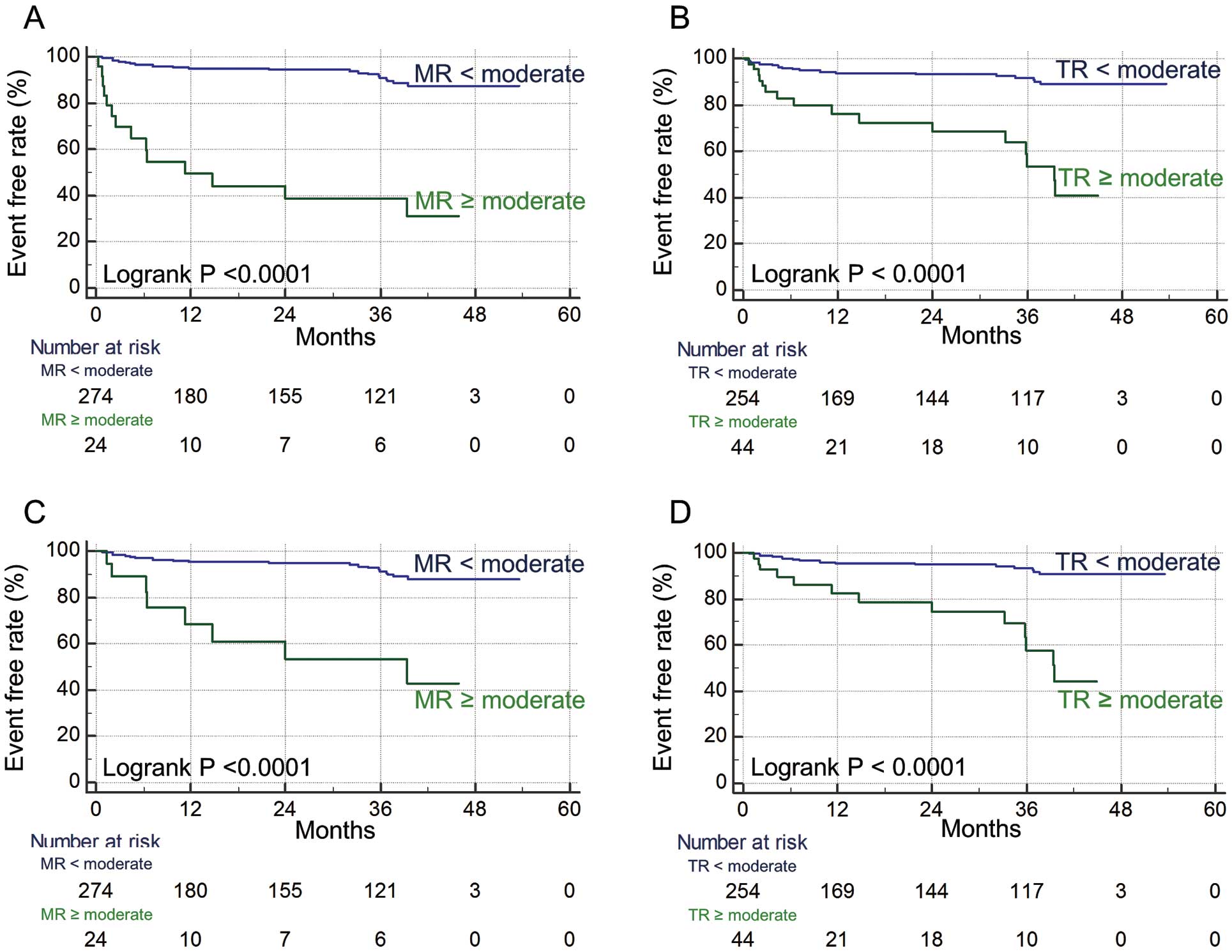
Kaplan-Meier event-free rates of (A,B) cardiac death, hospitalization due to worsening heart failure, or mitral valve and/or tricuspid valve repair or (C,D) cardiac death, hospitalization due to worsening heart failure (i.e., excluding valve repair) vs. the presence of significant (i.e., moderate or greater) mitral or tricuspid regurgitations (MR or TR).
In addition, the patients with both significant functional MR and TR had the poorest prognosis, with an event-free rate of 21% and a standard error of 13% at mean follow-up of 24 months (Figure 5A). Even after we excluded the surgical repairs from the endpoint, the event-free rate at mean follow-up of 24 months was still low in patients with both significant MR and significant TR (27% with the standard error of 16%; Figure 5B).

Kaplan-Meier event-free rates of (A) cardiac death, hospitalization due to worsening heart failure, or mitral valve and/or tricuspid valve repair or (B) cardiac death, hospitalization due to worsening heart failure (i.e., excluding valve repair) vs. the combinations of significant (i.e., moderate or greater) mitral and tricuspid regurgitations (MR and TR).
The present study has described the prevalence and prognostic significance of functional MR and TR in AF patients despite having preserved LVEF. Overall, (1) functional MR and TR were rarely seen in patients with AF duration ≤1 year; (2) functional MR and TR were seen in one-fourth of patients with longstanding AF >10 years; (3) both MR and TR were independent predictors of the primary endpoint defined as cardiac death, admission due to worsening HF, or surgical mitral and tricuspid repair; and (4) the concomitance of MR and TR carried the worst prognosis, with an event-free rate of only 21% at the mean follow-up of 2 years.
Annular dilatation in lone AF patients does not usually cause functional MR, but functional TR is relatively easily induced.25,26 In contrast, some other studies have shown that functional MR can occur in patients with AF and an enlarged LA, despite having preserved LV systolic function; this MR is known as atrial functional MR.10–13,15,16 In our previous study using 3-D transesophageal echocardiography (TEE), AF patients with atrial functional MR had dilated LA, dilated mitral annulus, flattened anterior mitral leaflet along the mitral annular plane, and posterior mitral leaflet bending toward the LV cavity, traditionally referred as the “hamstringing” phenomenon of the posterior mitral leaflet.13 Utsunomiya et al also used 3-D TEE and showed that AF patients with atrial functional TR had dilated RA and tricuspid annulus without valvular tenting.14 The present study has shown that the prevalence of atrial functional MR and TR depends on AF duration, which may relate to the degree of LA and RA dilatation. The differences in the prevalence of atrial functional MR and TR between the previous studies and the present study might result from differences in AF duration between the various cohorts. We suppose that the prevalence of functional MR and TR is growing due to the increased number of senior patients with longstanding AF in today’s aging population.1–3 According to some previous studies, however, regurgitation-induced secondary ventricular dilatation or the lack of leaflet remodeling can be added to other known factors (i.e., AF duration, atrial dilatation, and annular dilatation) as possible causes of the occurrence or the worsening of atrial functional MR and TR.13,27 The exact determinants of atrial functional MR and TR remain uncertain, therefore further studies are needed to address this issue.
AF can lead to HF with preserved LVEF, and their association brings a poor prognosis.7 In fact, cardiac death is more frequent than stroke-related death in AF patients, and a substantial proportion of the cardiac death results from HF.4–6 Consequently, interventions beyond anticoagulation are needed to further reduce mortality in AF. The present study confirmed the high probability of future HF events in AF patients who had both significant functional MR and significant functional TR, thereby suggesting that more intensive therapy may be required for these regurgitations to prevent HF events in AF patients. Gertz et al showed that atrial functional MR improved if the sinus rhythm was restored by AF ablation.11 The initial LA size, however, was not particularly large in their patients who had significant atrial functional MR: the LA dimension was 4.4±0.6 cm. Our previous study showed that surgical mitral annuloplasty with concomitant tricuspid annuloplasty may be an effective treatment strategy for reducing MR, HF symptoms, LA size, and HF admissions in patients with a significant degree of atrial functional MR with more dilated LA: the initial LA dimension was 5.2±0.9 cm.12 Surgical intervention for atrial functional MR and TR could be the best option for HF issues in AF patients with dilated atriums with preserved LVEF.
Study LimitationsThe present study has several limitations. It was a retrospective study based on the medical records of Osaka City General Hospital, and the echocardiography laboratory database. Consequently, MR and TR were graded using various qualification or quantification methods selected at the sonographer’s discretion, therefore grading might not be consistent. In our opinion, however, this may be a strength of the present study, rather than a limitation, because these data represent real-world clinical data. In the clinical setting, discrepancy in the grading of MR and TR in AF patients can easily arise with method-by-method and beat-by-beat assessments. Accordingly, we usually use a multiparametric approach with multiple qualification and quantification methods for assessing MR and TR in AF patients, and we finally grade the regurgitations from a comprehensive standpoint under the careful consideration of the advantages and limitations of each method, as done in the present study. We avoided inaccuracy as much as possible by carefully selecting 1 beat occurring after 2 serial beats with average RR interval for the measurement of the systolic parameters.20 In addition, we used 3 levels of borderline grades (none-mild, mild-moderate, and moderate-severe) when a considerable discrepancy existed in the grading between the multiple methods or between the different beats.
A further challenge is obtaining an accurate evaluation of LV diastolic dysfunction as a possible cause of HF with preserved LVEF in AF patients.28 We did not assess LV diastolic parameters from the calculation of the average at multiple beats; instead, we used the measurements at a single representative beat, although the single-beat measurement is not recommended in the assessment of diastolic parameters in AF patients.29 Consequently, the present single-beat measurements might disturb an accurate evaluation of the relationship between diastolic parameters and HF events. Future prospective studies using the recommended methods for echocardiographic measurements are needed to address this issue.
Significant functional MR and TR were seen in a substantial proportion of patients with longstanding AF despite having preserved LVEF. The combination of these regurgitations, termed “atrial functional MR and TR”, is associated with poor prognosis in AF patients with preserved LVEF and may have to be treated more intensively.
The authors declare no conflicts of interest.