Article ID: CJ-18-0136
Article ID: CJ-18-0136
Background: Fulminant myocarditis (FM) presents various abnormal findings on ECG, the prognostic impact of which has not been not fully elucidated. The aim of this study was therefore to clarify the prognostic value of ECG data in FM patients supported by venoarterial extracorporeal membrane oxygenation (VA-ECMO).
Methods and Results: In this multicenter chart review, we investigated 99 patients with FM supported by VA-ECMO. The final cohort consisted of 87 patients (mean age, 52±16 years; female, 42%) after 12 patients who required conversion to other forms of mechanical circulatory support were excluded. The median LVEF was 14.5%. At the time of VA-ECMO initiation, 38 patients (44%) had arrhythmias including atrial fibrillation (6%), complete atrioventricular block (CAVB; 17%), and ventricular tachycardia or fibrillation (VT/VF; 15%). Of the 49 patients with sinus rhythm (SR), 26 had QRS duration ≥120 ms (wide QRS). On logistic regression analysis, wide QRS predicted in-hospital death in patients with SR (OR, 3.6; 95% CI: 1.07–13.61, P=0.04). Compared with SR with narrow QRS (QRS duration <120 ms), CAVB and VT/VF had a higher risk of in-hospital death (CAVB: OR, 7.20; 95% CI: 1.78–34.15, P=0.005; VT/VF: OR, 8.10; 95% CI: 1.86–42.31, P=0.005).
Conclusions: In patients with FM, CAVB and VT/VF carried a higher risk of in-hospital death. Wide QRS also predicted a higher risk of in-hospital death in patients with SR.
Some patients with acute myocarditis have a fulminant course (fulminant myocarditis [FM]), characterized by rapid circulatory collapse.1,2 These patients often require mechanical circulatory support (MCS) to stabilize their hemodynamic status.3 Percutaneous venoarterial extracorporeal membrane oxygenation (VA-ECMO) is often used as first-line MCS because it can be introduced more easily and quickly and is less invasive than other surgical MCS.4–6
The management of FM in patients on VA-ECMO support is challenging. Previous studies have reported an in-hospital mortality of 30–50% in these patients.7–9 In addition, it is difficult to predict outcome at the early stage of disease. In this regard we previously reported on an early prediction model for FM patients on VA-ECMO support.10 That model, however, focused on the recovery of cardiac function and changes in biochemical markers. From a clinical standpoint, distinguishing abnormalities on electrocardiogram (ECG) is also important for the daily practice and management of FM patients.
According to the current Japanese Society of Cardiology guidelines, abnormality on ECG constitutes one of the main components in the diagnosis of acute myocarditis.11 A total of 50–80% of patients with FM have arrhythmia during hospitalization,4,8,12 but little is known about the details of the clinical impact of ECG data on prognosis in such situations. The purpose of this study was to investigate the prognostic value of the in patients with FM on VA-ECMO.
This was a multicenter retrospective study of FM patients on VA-ECMO, using data from the Chart Review of In-hospital Prognosis in Patients with Fulminant Myocarditis on Percutaneous Cardiopulmonary Support (CHANGE PUMP) Study. The data from patients with FM who required percutaneous VA-ECMO from January 2000 to August 2016 were obtained from their medical records at 26 high-volume cardiovascular centers in the Tokai area of Japan. The study protocol was approved by the Ethics Review Board of Nagoya University (approval no. 2016-0002).
PatientsWe performed a review of medical records to collect the data of 99 patients with FM who were supported by percutaneous VA-ECMO. Patients with comorbid critical complications ≤24 h after the initiation of percutaneous VA-ECMO, such as irreversible leg ischemia, stroke, major bleeding, and massive systemic thromboembolism, were not included in the study. Twelve patients who required conversion to other forms of MCS, that is, bi-ventricular assist device (VAD; n=5), left-VAD with VA-ECMO (n=4), left-VAD alone (n=2), and add-on left ventricular (LV) drainage to VA-ECMO (n=1) were excluded from the total of 99 because we focused on in-hospital mortality while under management with VA-ECMO. We defined 46 patients who achieved removal of percutaneous VA-ECMO and subsequent discharge as survivors. The remaining 41 patients who died while in hospital were defined as non-survivors (Figure 1). The medical record review was performed by the expert cardiologists in each institute.
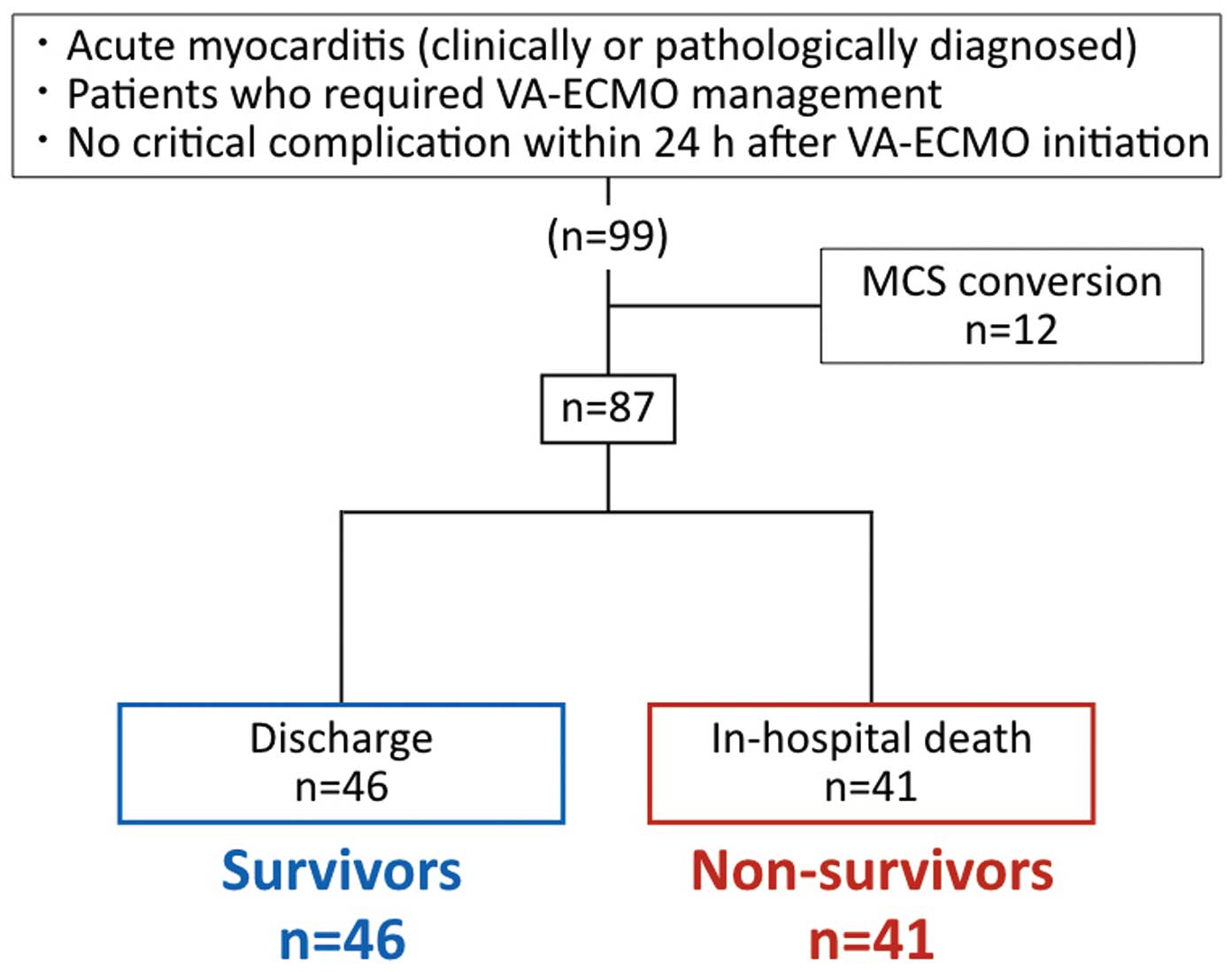
Schematic diagram of prognostic classification. MCS, mechanical circulatory support; VA-ECMO, venoarterial extracorporeal membrane oxygenation.
In this study, patients with a diagnosis of acute myocarditis who required percutaneous VA-ECMO because of circulatory collapse were considered to have FM. The diagnosis of acute myocarditis was based on the endomyocardial biopsy or autopsy histology13 or on the clinical findings according to the Japanese Circulation Society guideline for the diagnosis and treatment of myocarditis.11
ElectrocardiographyThe standard 12-lead ECG at the time of VA-ECMO initiation (0 h) was obtained for all patients. In addition, ECG at the time of VA-ECMO removal (in survivors) or immediately before cardiac arrest (in non-survivors) was obtained. An expert cardiologist in each institution investigated the ECG data according to the AHA/ACCF/HRS recommendations for the standardization and interpretation of ECG.14,15 We gathered information on QRS duration and type of rhythm including sinus rhythm (SR), atrial fibrillation (AF), atrial flutter (AFL), paroxysmal supraventricular tachycardia (PSVT), accelerated idioventricular rhythm (AIVR), ventricular tachycardia or fibrillation (VT/VF), sick sinus syndrome (SSS), and high-degree or complete atrioventricular block (CAVB). Duration of QRS complex ≥120 ms and <120 ms was defined as wide QRS and narrow QRS, respectively.
Statistical AnalysisContinuous variables are presented as mean±SD or median (IQR), and the distributions of these variables between 2 groups were compared using 2-sample t-test or Wilcoxon rank-sum test. Categorical variables are presented as number and percentage, and the distribution of these variables between 2 groups was compared using chi-squared test. The changes in serum creatine kinase (CK) from VA-ECMO initiation were analyzed using the Wilcoxon signed-rank test. Univariable logistic analysis was used to evaluate OR and 95% CI for the prediction of in-hospital mortality. All statistical analysis was performed using JMP Pro version 13.0 (SAS Institute, Cary, NC, USA). P<0.05 was considered to indicate statistical significance.
Baseline characteristics are listed in Table 1. The median time from symptom onset to VA-ECMO initiation was 48 h. Fifty-five patients were diagnosed with myocarditis on endomyocardial biopsy and 2 were diagnosed on autopsy. The other 30 patients were diagnosed on clinical findings. There were no significant differences between survivors and non-survivors regarding reasons for cardiopulmonary resuscitation. There were also no significant differences in LV ejection fraction. Regarding cardiopulmonary resuscitation, the prevalence of arrhythmia tended to be higher in non-survivors. With regard to the laboratory data at 0 h, non-survivors had significantly higher total bilirubin and serum creatinine. Additionally, non-survivors also tended to have higher aspartate aminotransferase, lactate dehydrogenase, CK and C-reactive protein (Figure S1).
| All (n=87) |
Survivors (n=46) |
Non-survivors (n=41) |
P-value | |
|---|---|---|---|---|
| Age (years) | 53±16 | 52±16 | 55±15 | 0.44 |
| Female | 35 (40) | 21 (46) | 14 (34) | 0.38 |
| BMI (kg/m2)† | 22.4±3.7 | 22.2±3.7 | 22.5±3.7 | 0.70 |
| Hemopathological findings at 0 h | ||||
| Mean BP (mmHg)‡ | 63±18 | 64±17 | 61±20 | 0.56 |
| HR (beats/min)† | 108±34 | 113±34 | 102±34 | 0.17 |
| LVEF (%)§ | 21.7±11.8 | 21.9±9.3 | 21.6±14.1 | 0.92 |
| Time to VA-ECMO (h) | 48 (24–120) | 48 (24–96) | 48 (12–120) | 0.72 |
| Time from admission to VA-ECMO (h) | 24 (0–48) | 24 (0–24) | 24 (0–48) | 0.20 |
| VA-ECMO run time (h) | 143 (101–236) | 141 (101–173) | 174 (98–303) | 0.16 |
| CPR before VA-ECMO | 32 (37) | 15 (33) | 17 (41) | 0.50 |
| Reasons for CPR | 0.28 | |||
| Worsening heart failure | 37 (43) | 22 (48) | 15 (37) | |
| Hypotension | 29 (33) | 16 (35) | 13 (32) | |
| Arrhythmia | 21 (24) | 8 (17) | 13 (32) | |
| Pathological diagnosis (n=57) | 0.85 | |||
| Lymphocytic | 46 (81) | 25 (78) | 21 (84) | |
| Eosinophilic | 8 (14) | 5 (16) | 3 (12) | |
| Unknown | 3 (5) | 2 (6) | 1 (4) | |
| Concomitant therapy | ||||
| RTT | 55 (63) | 28 (61) | 27 (66) | 0.66 |
| Steroids | 23 (26) | 10 (22) | 13 (32) | 0.34 |
| IVIG | 36 (41) | 19 (41) | 17 (41) | 1.00 |
| Laboratory data at 0 h | ||||
| Hemoglobin (g/dL) | 13.1±2.1 | 13.1±2.0 | 13.1±2.2 | 0.89 |
| AST (U/L)‡ | 328 (134–1,062) | 197 (108–1,274) | 487 (165–1,025) | 0.21 |
| TB (mg/dL)† | 0.7 (0.5–1.0) | 0.6 (0.5–0.8) | 0.9 (0.5–1.3) | 0.03 |
| LDH (U/L)‡ | 933 (551–2,111) | 755 (496–2,153) | 1,177 (667–2,051) | 0.14 |
| CK (U/L)‡ | 904 (471–1,617) | 839 (464–1,447) | 1,112 (476–1,818) | 0.52 |
| SCr (mg/dL)‡ | 1.24 (0.98–2.04) | 1.10 (0.80–1.48) | 1.67 (1.20–2.10) | 0.004 |
| CRP (mg/dL)† | 4.96 (1.51–11.37) | 4.53 (1.33–9.37) | 6.00 (2.18–14.31) | 0.42 |
Data given as n (%), mean±SD or median (IQR). Missing values: †10–15%; ‡1–10%; §15–20%. 0 h, at VA-ECMO initiation; AST, aspartate aminotransferase; BMI, body mass index; BP, blood pressure; CK, creatine kinase; CPR, cardiopulmonary resuscitation; CRP, C-reactive protein; FM, fulminant myocarditis; Hb, hemoglobin; HR, heart rate; IVIG, intravenous immunoglobulins; LDH, lactate dehydrogenase; LVEF, left ventricular ejection fraction; RRT, renal replacement therapy; SCr, serum creatinine; TB, total bilirubin; VA-ECMO, venoarterial extracorporeal membrane oxygenation.
ECG data at 0 h are listed in Table 2. Forty-nine patients (56%) had SR at 0 h. There were no significant differences in the prevalence of CAVB, AF, or VT/VF between survivors and non-survivors. Of the 5 patients classified as “others,” one of the non-survivors had AIVR while the other 4 had undetectable rhythm owing to the low voltage. No patients had AFL, PSVT, or SSS at 0 h. In terms of QRS duration, non-survivors had significantly prolonged QRS duration and higher prevalence of wide QRS than survivors.
| All (n=87) |
Survivors (n=46) |
Non-survivors (n=41) |
P-value | |
|---|---|---|---|---|
| Rhythm | ||||
| SR | 49 (56) | 31 (67) | 18 (44) | 0.03 |
| AF | 5 (6) | 4 (9) | 1 (2) | 0.36 |
| CAVB | 15 (16) | 5 (11) | 10 (24) | 0.08 |
| VT/VF | 13 (16) | 4 (9) | 9 (22) | 0.08 |
| Other | 5 (6) | 2 (4) | 3 (7) | 0.90 |
| QRS duration (ms) | 130 (106–152) | 120 (86–140) | 142 (128–156) | 0.001 |
| Wide QRS | 57 (66) | 24 (52) | 33 (80) | 0.006 |
Data given as n (%) or median (IQR). AF, atrial fibrillation; CAVB, complete atrioventricular block; SR, sinus rhythm; ECG, electrocardiogram; VT/VF, ventricular tachycardia or fibrillation. Other abbreviations as in Table 1.
Changes in heart rhythm during VA-ECMO are shown in Figure 2. Of the 49 patients with SR at 0 h, 36 maintained SR during VA-ECMO. Similarly, 7 of the 15 patients with CAVB maintained CAVB. Of 7 patients whose heart rhythm converted from SR to CAVB, 6 had wide QRS at 0 h.
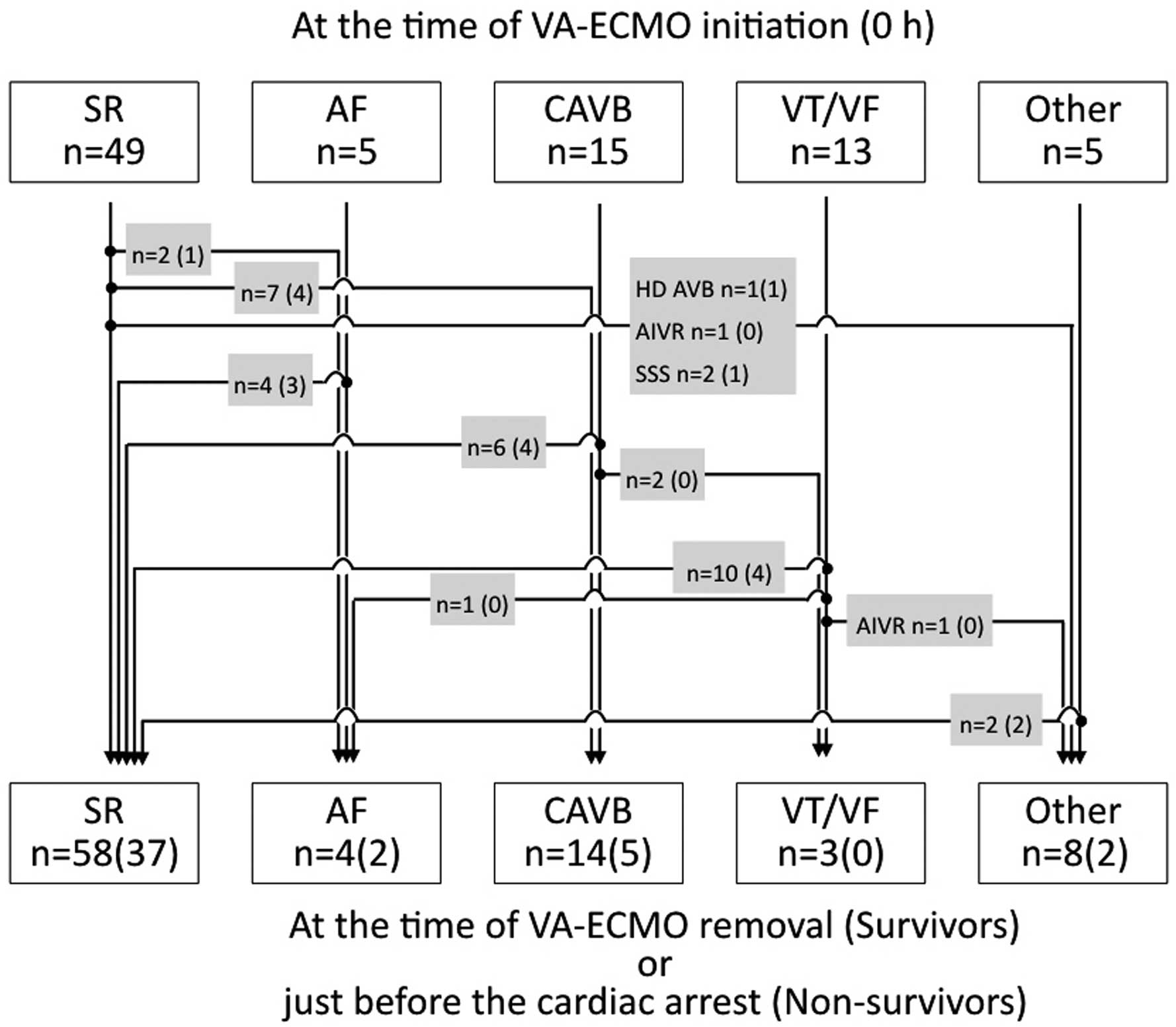
Changes in heart rhythm in fulminant myocarditis patients. AF, atrial fibrillation; AIVR, accelerated idioventricular rhythm; CAVB, complete atrioventricular block; HD AVB, high-degree atrioventricular block; SR, sinus rhythm; SSS, sick sinus syndrome; VA-ECMO, venoarterial extracorporeal membrane oxygenation; VT/VF, ventricular tachycardia or fibrillation. (n), no. surviving patients.
Logistic regression analysis was carried out to evaluate the prognostic value of the ECG data. Comparison with SR with narrow QRS, SR with wide QRS, CAVB and VT/VF predicted a 3.1-, 7.2- and 8.1-fold higher risk of in-hospital death, respectively, although AF had no prognostic value (Figure 3).
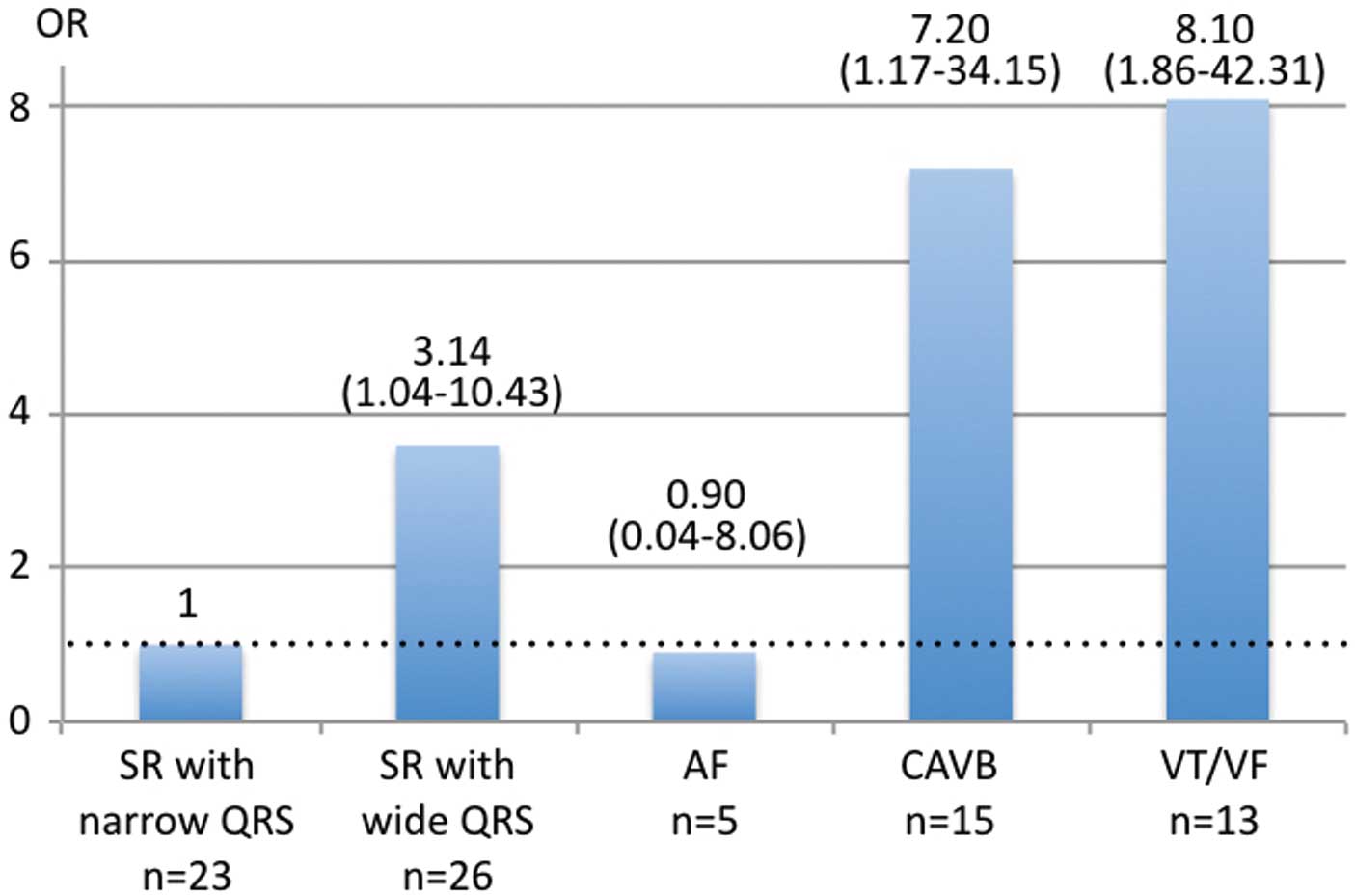
OR (95% CI) for in-hospital death in patients with fulminant myocarditis (OR reference, SR with narrow QRS [QRS duration <120 ms]). Wide QRS, QRS duration ≥120 ms. Abbreviations as in Figure 2.
To clarify the relationship between abnormal ECG and myocardial damage in patients with FM, we investigated the changes in serum CK according to subgroup (Figure 4). Serum CK was significantly higher in the SR with wide QRS, CAVB, and VT/VF groups than in the SR with narrow QRS group at 0 h. In addition, serum CK at 24 h after initiation of VA-ECMO was elevated in the SR with wide QRS and VT/VF groups.

Change in serum creatine kinase (CK) in fulminant myocarditis patients with SR with narrow QRS compared with (A) SR with wide QRS; (B) CAVB; and (C) VT/VF. Abbreviations as in Figure 2. *P<0.05, comparison of 2 groups by the Wilcoxon rank-sum test; †P<0.05, compared with 0 h in the same group by the Wilcoxon signed-rank test.
The main findings of the present study are as follows: (1) CAVB and VT/VF at 0 h had predictive value for in-hospital death in FM patients on VA-ECMO; (2) wide QRS also was a risk factor for in-hospital death even if in SR at 0 h; and (3) these abnormal ECG findings were associated with elevated serum CK.
It is important to distinguish between abnormal ECG for the correct diagnosis of acute myocarditis.11 It is hardly surprising that hemodynamically compromising arrhythmia, such as CAVB and VT/VF, had a negative impact on prognosis: arrhythmia requiring any treatment has been found to increase the risk of in-hospital mortality in FM patients on VA-ECMO.9 Little is known, however, about which types of arrhythmia influence prognosis in FM patients on VA-ECMO. Thus, we investigated the relationship between ECG data and prognosis and found that CAVB and VT/VF, but not AF, were associated with a higher risk of in-hospital mortality compared with SR with narrow QRS. We also identified the importance of wide QRS for the prediction of in-hospital death. Wide QRS has been found to predict poor outcome in patients with acute myocarditis with non-fulminant presentation.16,17 In addition, Ammirati et al reported that patients with FM have a worse outcome than those without FM.18 In the present study, wide QRS, even in patients with SR at the initiation of VA-ECMO, also predicted poor outcome in FM patients.
Arrhythmia and Myocardial DamageSerum CK was significantly lower in patients with SR with narrow QRS than in those with CAVB or VT/VF at 0 h (Figure 4B,C). This suggests that CAVB and VT/VF might reflect the severity of myocardial damage. Interestingly, however, the patients with CAVB had no significant elevation in serum CK after 24 h (Figure 4B), although those with VT/VF did have a significant serum CK increase (Figure 4C). This may be explained by the differences in the pathophysiological mechanisms. In other words, myocardial damage caused by myocarditis might have already become widespread and almost complete in patients with CAVB, thus inducing no further subsequent damage. In contrast, VT/VF itself inhibits myocardial perfusion, which leads to additional myocardial damage and elevation of serum CK.
Significance of QRS DurationPatients with wide QRS also had significantly elevated serum CK during the 24 h after VA-ECMO initiation (Figure 4A). In addition, 13 patients with SR at 0 h had conversion to other arrhythmias (Figure 2). Of these, 10 (77%) had wide QRS. Therefore, we deduce that wide QRS implies mild or early-stage progressive myocardial damage arising from myocarditis. If wide QRS reflects mild myocardial damage, SR might be maintained; if, however, it reflects the early stage of ongoing damage, wide QRS may anticipate the progression of myocardial damage, which evokes volatile arrhythmias. Therefore, clinicians should take care not to fall behind the curve at the occurrence of hemodynamically compromising arrhythmia in patients with wide QRS, even while in SR.
Earlier Risk Stratification on ECGWe should interpret the clinical significance of abnormal ECG with caution, because the sensitivities for CAVB and VT/VF to predict in-hospital mortality were low, although specificities were relatively high (Table 3). The potential for risk stratification at 0 h, however, deserves mention.
| Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|
| SR with wide QRS | 0.283 | 0.683 | 0.500 | 0.459 |
| CAVB | 0.244 | 0.891 | 0.667 | 0.569 |
| VT/VF | 0.220 | 0.913 | 0.692 | 0.568 |
NPV, negative predictive value; PPV, positive predictive value. Other abbreviations as in Tables 1,2.
We previously reported the difficulty of outcome prediction at 0 h in FM.10 In that study we focused on the recovery of cardiac function and changes in biochemistry markers during the 48 h after VA-ECMO initiation. As we have clarified in the present study, however, ECG may have the potential to provide some prognostic information during the early clinical course of FM. Miyake et al reported that arrhythmia was associated with low voltage on ECG and worse outcome in pediatric patients with acute myocarditis,19 although we could not investigate the voltages in the present study. Therefore, we consider that the ECG provides clinicians with useful, although not definitive, information for initial judgment regarding risk stratification. Additionally, to determine a more reliable treatment strategy we recommend that clinicians focus on the changes that occur in cardiac function and in biochemistry markers.
Study LimitationsThere are some limitations regarding this study. First, we clarified the significance of wide QRS but did not take into consideration the other abnormal ECG data, such as abnormal Q wave, voltage, ST-T abnormality, and poor R progression, because we were unable to collect these data in this retrospective chart review. In addition, we could not deny the existence of measurement bias, because investigation of the ECG was performed by a cardiologist in each institute. Second, we did not investigate serum CK-MB or troponin because of the large number of missing data. We consider, however, that higher serum CK indicated myocardial damage, although it would also be influenced by the low perfusion of skeletal muscle or poor systemic condition. Third, the present cohort consisted of a small number of patients. Although we reported that AF had no prognostic value with respect to in-hospital mortality, this could not be regarded as conclusive because the prevalence of AF was appreciably low. Fourth, we did not investigate the support flow rate or cannula size in VA-ECMO, although these parameters would be important for management. The present results therefore require verification in a larger population.
CAVB and VT/VF are risk factors for in-hospital death in patients with FM on VA-ECMO. Wide QRS also predicts a poor outcome in patients with SR at the initiation of VA-ECMO. These abnormal ECG findings might reflect the severity of myocardial damage and should be useful for initial risk stratification.
We thank the collaborators and members of the CHANGE PUMP study group.
Steering Committee of the CHANGE PUMP Study
Nagoya University Graduate School of Medicine: T. Murohara, A. Sawamura, T. Okumura; Mie University Graduate School of Medicine: M. Ito; Fujita Health University: Y. Ozaki; Nagoya City University Graduate School of Medical Science: N. Ohte; Aichi Medical University: T. Amano.
Investigators at Participating Medical Institutions in the CHANGE PUMP Study
Aichi Medical University: T. Mizuno, K. Mukai, T. Amano; Anjo Kosei Hospital: M. Koyasu, Y. Ozaki; Chubu Rosai Hospital: K. Harada, H. Funakubo; Chutoen General Medical Center: S. Morikawa, R. Ota; Fujita Health University: Y. Kato, Y. Ozaki; Gifu Prefectural Tajimi Hospital: T. Shigeta; Hamamatsu Medical Center: M. Muto; Handa City Hospital: M. Sakakibara; Ise Red Cross Hospital: T. Seko, K. Unno; Japan Community Healthcare Organization Chukyo Hospital: K. Kada, M. Yoshida, H. Kato; Japanese Red Cross Nagoya Daiichi Hospital: S. Shimizu; Japanese Red Cross Nagoya Daini Hospital: Y. Aoyama; Kainan Hospital Aichi Prefectural Welfare Federation of Agricultural Cooperatives: M. Miura; Kariya Toyota General Hospital: M. Goto; Komaki Municipal Hospital: H. Imai; Mie University Graduate School of Medicine: K. Dohi, K. Moriwaki, E. Sugiura, N. Fujimoto, S. Fukuoka, N. Kumagai, T. Omori, M. Ito; Nagoya City University Graduate School of Medical Science: S. Kitada, N. Ohte; Nagoya Ekisaikai Hospital: D. Tanimura; Nagoya University Graduate School of Medicine: H. Kawase, S. Aoki, A. Sawamura, T. Okumura, T. Murohara; Ogaki Municipal Hospital: Y. Morita; Okazaki City Hospital: M. Niwa; Tose General Hospital: M. Ajioka, T. Kanbara; Toyohashi Municipal Hospital: S. Shimazu; Toyota Kosei Hospital: M. Shinoda, S. Kaneko, T. Kamihara, K. Yamaguchi; Toyota Memorial Hospital: K. Suga; Yokkaichi Municipal Hospital: W. Suzuki.
The authors declare no conflicts of interest.
Supplementary File 1
Figure S1. AST, LDH, and CK according to survival status in fulminant myocarditis patients.
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-18-0136