Article ID: CJ-18-0375
Article ID: CJ-18-0375
Background: Brain natriuretic peptide (BNP) and N-terminal proBNP (NT-proBNP) are prognostic biomarkers. Although these 2 peptides differ with regard to biological characteristics, there are few reports on the differences between BNP and NT-proBNP with regard to cardiovascular events or according to sex.
Methods and Results: Between 2005 and 2012, this study analyzed 3,610 of 4,310 Japanese outpatients (mean age, 65 years; men, n=1,664; women, n=1,947) with a history of at least one cardiovascular event who were recruited to the Japan Morning Surge-Home Blood Pressure Study. During an average 4-year follow-up, there were 129 cardiovascular events. Both median BNP (21.1 pg/mL; IQR, 10.9–40.6 pg/mL vs. 16.2 pg/mL, IQR, 7.2–36.2 pg/mL, P<0.001) and median NT-proBNP (54.7 pg/mL; IQR, 30.2–102.6 pg/mL vs. 44.9 pg/mL, IQR, 20.7–92.6 pg/mL, P<0.001) were significantly higher in women than in men. A 1-SD increment in log-transformed BNP (hazard ratio [HR], 2.18; 95% CI: 1.53–3.10) and NT-proBNP (HR, 2.39; 95% CI: 1.73–3.31) was associated with a significant increase in cardiovascular events in women; in men, only NT-proBNP showed this association. There was an interaction between log-transformed BNP (P=0.007) or NT-proBNP (P=0.001) and cardiovascular events according to sex.
Conclusions: Both BNP and NT-proBNP predicted cardiovascular outcomes in a large Japanese clinical population. BNP and NT-proBNP were significantly stronger predictors in women than in men.
Serum levels of natriuretic peptide hormones, in particular brain natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP), are useful biomarkers for ruling out heart failure,1–3 as well as strong prognostic markers for cardiovascular events in not only heart failure and hypertensive populations but also the general population.4–6
BNP, in contrast to NT-proBNP, is biologically active when released into the circulation.7,8 In some studies comparing the utility of BNP and NT-proBNP for heart failure screening and prognostic value for cardiovascular events, no practical difference was observed.3,9 The value of those studies, however, was limited by their evaluation of selected patients. One study involved a small sample of patients with suspected heart failure,3 and another study was performed in a stable and symptomatic heart failure population.9
In addition, both BNP and NT-proBNP are higher in women than in men.10–12 Although the effects of BNP or NT-proBNP on prognosis have been reported according to sex in heart failure populations, the results are conflicting.13,14 This may explain why data were unable to discriminate between BNP and NT-proBNP in heterogeneous heart failure populations, yielding inconsistent results.
The aim of this study was therefore to investigate differences between BNP and NT-proBNP with regard to cardiovascular events and extend the search for this difference to sex, in a large clinical population with cardiovascular risk factors.
We used baseline data from the Japan Morning Surge-Home Blood Pressure (J-HOP) Study. The protocol of the J-HOP study has been published (Supplementary File 1).15 Briefly, the J-HOP study is a prospective observational study (University Hospital Medical Information Network Clinical Trials Registry, UMIN000000894) evaluating the use of home blood pressure (BP) measurements to predict cardiovascular events between January 2005 and May 2012 in 4,310 Japanese ambulatory patients who had a history of and/or risk factors for cardiovascular disease (CVD) as follows: hypertension, dyslipidemia, diabetes, glucose intolerance, metabolic syndrome, chronic kidney disease (CKD), history of CVD, atrial fibrillation, current smoking, chronic obstructive pulmonary disease, or sleep apnea syndrome. All participants provided written informed consent for their data to be used, and the Institutional Review Board of Jichi Medical School approved the study.
Of the 4,310 patients enrolled in the J-HOP study, we excluded 691 lacking data for both BNP and NT-proBNP. A final total of 3,619 patients was included in the present analysis. Diabetes was defined as fasting glucose ≥126 mg/dL and/or a casual glucose ≥200 mg/dL or treatment for diabetes. Dyslipidemia was defined as total cholesterol ≥240 mg/dL or treatment for dyslipidemia. CKD was defined as the presence of proteinuria or estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2. Past history of CVD was defined as diagnosed angina pectoris, myocardial infarction (MI), or stroke. The average of 3 office BP measurements carried out in a sitting position at 2 clinic visits were taken by a physician or nurse using an upper arm cuff and an oscillometric BP device (HEM-5001; Omron Healthcare, Kyoto, Japan), and used in the present study.
Natriuretic PeptidesFasting morning blood and spot urine samples were collected at study enrollment. Plasma BNP was measured with a chemiluminescent enzyme assay (MI02 Shionogi BNP; Shionogi, Osaka, Japan). NT-proBNP was measured with an automated Cobas analyzer using an electrochemiluminescent immunoassay (Roche Diagnostics, Japan).
Outcome MeasurementThe primary outcome was the first occurrence of a cardiovascular event during the study period, including fatal and non-fatal stroke and fatal and non-fatal coronary artery disease, defined as acute MI, angina pectoris requiring percutaneous coronary intervention, and sudden death ≤24 h after abrupt onset of symptoms. If events occurred on ≥2 occasions, the first occurrence was included in the analysis (Supplementary File 1).
Statistical AnalysisData are expressed as mean±SD, median (IQR), or percentage. The distribution of BNP and NT-proBNP was highly skewed and was log-transformed before the statistical analysis. Continuous variables were compared using Student’s t-test, and categorical variables were compared using the chi-squared test. Univariate associations were assessed using Pearson’s correlation. Cumulative incidences of cardiovascular events in quartiles of BNP and NT-proBNP in the entire group and according to gender were plotted as Kaplan-Meier curves, and the differences were assessed with the log-rank test. The hazard ratio (HR) and 95% CI of cardiovascular events in quartiles of BNP and NT-proBNP in the entire group and according to gender were calculated using unadjusted and adjusted Cox regression analyses after adjustments for traditional cardiovascular risk factors, that is, age, gender, body mass index (BMI), smoking, pre-existing CVD, total cholesterol, high-density lipoprotein cholesterol (HDL-C), diabetes, use of an antihypertensive drug or statin, eGFR, and clinic-measured systolic blood pressure (SBP). The proportionality assumption for the Cox analysis was confirmed graphically and via the inclusion of a time×BP interaction. In the group stratified by sex, Cox regression analysis was performed with adjustment for similar covariates except for gender. To evaluate the association of elevated BNP and NT-proBNP with cardiovascular events, we used log-transformed BNP and NT-proBNP per 1 SD as a continuous variable in a Cox regression analysis that included similar covariates in the entire group and according to gender. Moreover, we used Cox proportional hazard regression to calculate adjusted HR, using dichotomized BNP (35 pg/mL as threshold) and NT-proBNP (125 pg/mL as threshold), which are recommended by the European Society of Cardiology for subjects with suspected heart failure.16 All statistical analysis was performed with Stata version 15.0 (StataCorp, College Station, TX, USA). P<0.05 was considered statistically significant for all tests.
There were no significant differences in baseline characteristics between participants included in the current study and those who were not included (Table S1). The participant demographic and clinical characteristics according to gender are given in Table 1. The proportion of women was 53.9%. Women were older than men. The prevalence of cardiovascular risk factors was higher in men than in women. Average BNP and NT-proBNP ere significantly higher in women than in men. There was a significant association between log-transformed BNP and log-transformed NT-proBNP in both groups (men, r=0.790, P<0.001; women, r=0.838, P<0.001).
| Women (n=1,951) |
Men (n=1,668) |
P-value | |
|---|---|---|---|
| Age (years) | 65.7±10.2 | 64.3±11.0 | <0.001 |
| BMI (kg/m2) | 24.3±3.8 | 24.2±3.1 | 0.818 |
| Current smoker | 3.6 | 22.0 | <0.001 |
| Daily drinker | 7.6 | 51.3 | <0.001 |
| Antihypertensive medication | 77.2 | 81.5 | 0.001 |
| Diabetes | 22.2 | 27.2 | <0.001 |
| Statin use | 28.2 | 18.8 | <0.001 |
| Pre-existing CVD | 8.3 | 18.2 | <0.001 |
| TC (mg/dL) | 208.6±31.6 | 195.7±32.3 | <0.001 |
| HDL-C (mg/dL) | 60.6±14.8 | 54.5±14.9 | <0.001 |
| Office SBP (mmHg) | 141.6±16.7 | 141.4±15.6 | 0.771 |
| Office DBP (mmHg) | 80.9±10.1 | 82.6±10.2 | <0.001 |
| BNP (pg/mL) | 21.1 (10.9–40.6) | 16.2 (7.2–36.2) | <0.001 |
| NT-proBNP (pg/mL) | 54.7 (30.2–102.6) | 44.9 (20.7–92.6) | <0.001 |
Data given as mean±SD, median (95% CI) or %. BMI, body mass index; BNP, brain natriuretic peptide; CI, confidence interval; CVD, cardiovascular disease; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; NT-proBNP, N-terminal-pro-brain natriuretic peptide; SBP, systolic blood pressure; TC, total cholesterol.
During a mean follow-up of 4.0±2.1 years (14,490 person-years), 129 cardiovascular events were observed. In the entire group, the incidence of cardiovascular events increased with increasing BNP and NT-proBNP quartiles, on Kaplan-Meier curve analysis (Figure 1). On unadjusted Cox regression analysis, the top quartile of BNP was a risk factor for cardiovascular events compared with the lowest quartile in men (HR, 2.88; 95% CI: 1.49–5.56; P=0.002) and in women (HR, 3.82; 95% CI: 1.66–8.80; P=0.002) and the top quartile of NT-proBNP was a risk factor for cardiovascular events compared with the lowest quartile in men (HR, 3.56; 95% CI: 1.83–6.96; P<0.001) and in women (HR, 6.28; 95% CI: 2.19–18.04; P=0.001). On multivariable Cox regression analysis after adjustment for age, sex, BMI, smoking, diabetes, total cholesterol and HDL-C, use of an antihypertensive drug or statin, past history of CVD, eGFR, and clinic-measured SBP, the top quartile of BNP was associated with a higher risk of cardiovascular events (Table 2). This association was similar for the quartiles of NT-proBNP. A 1-SD increment in log-transformed BNP was associated with a significant increase in cardiovascular events (HR, 1.34; 95% CI: 1.10–1.63, P=0.004). The association between a 1-SD increment in NT-proBNP and cardiovascular events was also similar (HR, 1.49; 95% CI: 1.24–1.79, P<0.001).
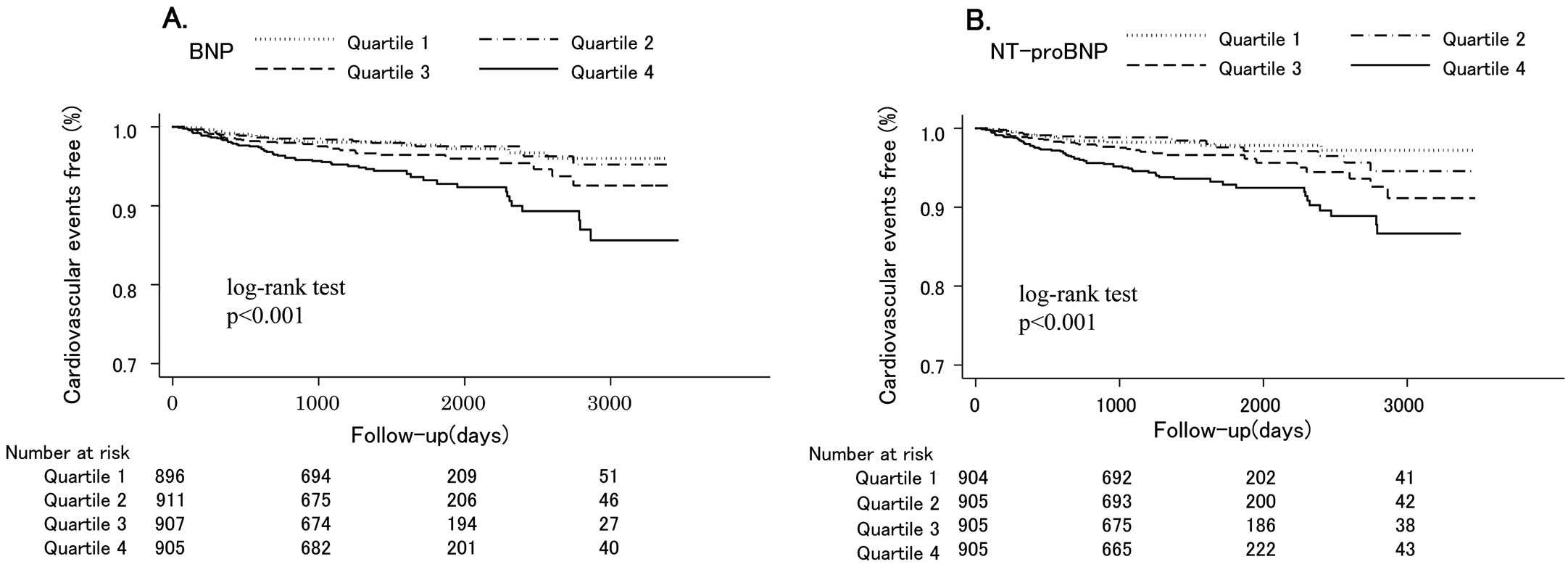
Kaplan-Meier cardiovascular event-free rate according to (A) brain natriuretic peptide (BNP) and (B) N-terminal pro-brain natriuretic peptide (NT-proBNP) quartiles.
| BNP | NT-proBNP | |||||
|---|---|---|---|---|---|---|
| Range (pg/mL) |
No. events/ Total no. subjects |
HR (95% CI) |
Range (pg/mL) |
No. events/ No. subjects |
HR (95% CI) |
|
| Quartile 1 | ≤9.2 | 20/896 | Re. | <25.52 | 17/904 | Ref. |
| Quartile 2 | 9.3–18.7 | 20/911 | 1.01 (0.54–1.91) | 25.54–50.35 | 18/905 | 0.96 (0.49–1.89) |
| Quartile 3 | 18.8–38.5 | 32/907 | 1.39 (0.77–2.52) | 50.47–97.34 | 33/905 | 1.71 (0.93–3.16) |
| Quartile 4 | ≥38.6 | 57/905 | 1.90 (1.07–3.36)* | >97.37 | 61/905 | 2.48 (1.36–4.49)** |
*P<0.05, **P<0.01 vs. Reference. HR are adjusted for age, sex, BMI, smoking, pre-existing CVD, TC, HDL-C, diabetes, use of an antihypertensive drug or statin, estimated glomerular filtration rate, and clinic-measured SBP. BNP, brain natriuretic peptide; HR, hazard ratio; NT-proBNP, N-terminal-pro-brain natriuretic peptide. Other abbreviations as in Table 1.
In women, increased BNP and NT-proBNP quartiles were associated with cardiovascular events on Kaplan-Meier curve analysis (Figure 2). These associations were observed in men. On multivariable Cox regression analysis after adjustment for age, BMI, smoking, diabetes, total cholesterol and HDL-C, use of an antihypertensive drug or statin, past history of CVD, eGFR, and clinic-measured SBP, the top quartiles for both BNP and NT-proBNP were associated with a higher risk of cardiovascular events in women, whereas only NT-proBNP had this association in men (Table 3). A 1-SD increment in log-transformed BNP and NT-proBNP was associated with a significant increase in cardiovascular events in women, whereas only NT-proBNP had this association in men. There was an interaction between log-transformed BNP or NT-proBNP and cardiovascular events according to sex (Table 4). On further analysis, both BNP and NT-proBNP were associated with cardiovascular events, irrespective of sex (Table S2). Although the HR of BNP and NT-proBNP was high in women compared with men, the interaction between NT-proBNP and cardiovascular events according to sex was marginal.

Kaplan-Meier cardiovascular event-free rate according to (A,C) brain natriuretic peptide (BNP) and (B,D) N-terminal pro-brain natriuretic peptide (NT-proBNP) quartiles in (A,B) men and (C,D) women.
| BNP | NT-proBNP | |||||
|---|---|---|---|---|---|---|
| Range (pg/mL) |
No. events/ Total no. subjects |
HR (95% CI) |
Range (pg/mL) |
No. events/ Total no. subjects |
HR (95% CI) |
|
| Men | ||||||
| Quartile 1 | ≤7.2 | 12/417 | Ref. | <20.67 | 11/417 | Ref. |
| Quartile 2 | 7.3–16.1 | 15/413 | 0.97 (0.44–2.10) | 20.72–44.86 | 13/417 | 1.03 (0.45–2.34) |
| Quartile 3 | 16.2–36.1 | 21/421 | 1.22 (0.58–2.59) | 44.90–92.36 | 19/417 | 1.25 (0.57–2.72) |
| Quartile 4 | ≥36.2 | 34/417 | 1.49 (0.72–3.10) | >92.64 | 39/417 | 2.25 (1.06–4.75)* |
| Women | ||||||
| Quartile 1 | ≤10.8 | 7/483 | Ref. | <30.15 | 4/487 | Ref. |
| Quartile 2 | 10.9–21.0 | 3/491 | 0.45 (011–1.78) | 30.19–54.68 | 7/488 | 1.33 (0.38–4.69) |
| Quartile 3 | 21.1–40.5 | 11/488 | 1.22 (0.44–3.37) | 54.70–102.5 | 11/488 | 2.29 (0.69–7.61) |
| Quartile 4 | ≥40.6 | 26/489 | 2.85 (1.11–7.32)* | >102.6 | 25/488 | 4.22 (1.33–13.37)* |
*P<0.05 vs. Reference. HR are adjusted for age, BMI, smoking, pre-existing CVD, TC, HDL-C, diabetes, use of an antihypertensive drug or statin, estimated glomerular filtration rate, and clinic-measured SBP. Abbreviations as in Tables 1,2.
| HR | 95% CI | P for interaction | |
|---|---|---|---|
| Log BNP (per 1 SD increase) | |||
| Men | 1.15 | 0.91–1.46 | 0.007 |
| Women | 2.18 | 1.53–3.10** | |
| Log NT-proBNP (per 1 SD increase) | |||
| Men | 1.29 | 1.04–1.60* | 0.001 |
| Women | 2.39 | 1.73–3.31** | |
*P<0.05, **P<0.01. HR are adjusted for age, BMI, smoking, pre-existing CVD, TC, HDL-C, diabetes, use of an antihypertensive drug or statin, estimated glomerular filtration rate, and clinic-measured SBP. Abbreviations as in Tables 1,2.
In the present study, both BNP and NT-proBNP were significantly higher in women than in men in a large Japanese population of individuals with a history of and/or risk factors for CVD. This is consistent with previous studies.10–12 Both BNP and NT-proBNP were independently associated with cardiovascular events, irrespective of sex. Interestingly, the association between BNP or NT-proBNP and cardiovascular events in women was significantly stronger than in men.
Both BNP and NT-proBNP have been used for heart failure screening and as prognostic biomarkers in general and clinical populations.4–6 These natriuretic peptides are produced by the cleavage of precursor proBNP, and exhibit differences in biological characteristics, such as bioactivity, half-life, and involvement in metabolic processes.7,8 Although several reports have compared the clinical utility of BNP and NT-proBNP, there was no significant difference in diagnostic accuracy for screening of symptomatic heart failure in a small population,3 in prognostic power for all-cause mortality and morbidity, or in hospitalization for heart failure in a stable and symptomatic heart failure population.9 The present results have confirmed previous reports that both BNP and NT-proBNP provide prognostic power for cardiovascular events in a large clinical population with cardiovascular risk factors.
In the present study a significant interaction was noted between male and female sex according to the prognostic power of BNP and NT-proBNP for cardiovascular events. In addition, the HR of the top quartile compared with that for the lowest quartile for BNP and NT-proBNP (Table 3), and the HR for a 1-SD increment in log-transformed BNP and NT-proBNP (Table 4) was approximately 2-fold higher in women than in men. Although sex differences in the effect of BNP or NT-proBNP for cardiovascular events have been unclear, the present findings support the previous studies. Kara et al compared the prognostic value of BNP and NT-proBNP for cardiovascular events in 3,589 individuals in the general population.17 Although they found that both higher BNP and higher NT-proBNP were associated with cardiovascular events in men, only BNP had this association in women.17 Ballo et al reported that in a population with hypertension and/or type 2 diabetes, NT-proBNP above the sex-specific 80th percentile was associated with a 3.6-fold higher risk of cardiac events in women and a 2.9-fold higher risk in men, compared with that below the 80th percentile; moreover, there was an interaction for risk between men and women.18 In contrast, sex differences in the association of BNP or NT-proBNP with cardiovascular events in patients with heart failure or suspected heart failure are controversial. Christ et al reported that in patients with acute dyspnea, abnormal BNP (>500 pg/mL) was associated with a 5.1-fold and a 1.8-fold increased risk of cardiac events in men and women, respectively, compared with the risk of BNP ≤500 pg/mL; there was also a significant interaction for this association between men and women,13 whereas in a large registry of admitted heart failure patients the ability of BNP to predict in-hospital mortality was similar between men and women.14 Thus, the prognostic value of BNP and NT-proBNP may be greater for women than men in the population without clinical heart failure. In contrast, when cardiovascular risk is high, the differential prognostic value of BNP and NT-proBNP according to sex might be weakened.
Although this study was not conducted to determine the pathological mechanism accounting for the differential effect of natriuretic peptide for cardiovascular outcomes according to sex, a previous study may have partially explained this phenomenon. Chen et al investigated age-related cardiac remodeling and functional changes according to sex differences in a large, healthy population.19 In that study, women had a steeper slope for echocardiographic increase in left ventricular mass with aging compared with men, and the results were strongly associated with NT-proBNP.19 Increased left ventricular mass is a powerful predictor of cardiovascular events,20 thus explaining the present results showing superior prognostic power for BNP and NT-proBNP in women than in men, given that the present patients were relatively older. Moreover, endogenous sex hormones in postmenopausal women might have affected the association between natriuretic peptide and cardiovascular outcomes in women. In the present study, the average age of the female subjects was 65 years. Creatsa et al reported that, in postmenopausal women, a higher free androgen index, as one of the markers of circulating androgen, was associated with subclinical organ damage,21 in the same way that carotid artery intima-media thickness and pulse wave velocity are markers of cardiovascular risk.22,23 Glisic et al reported that a higher free androgen index was associated with lower NT-proBNP in postmenopausal women.24 From these two previous studies, we can thus speculate that higher androgen may decrease natriuretic peptide, whereas it may increase cardiovascular risk in postmenopausal women. As a result, even if the absolute circulating natriuretic peptide level is similar between a man and a woman, the woman might be at higher risk of cardiovascular events than the man.
In this study, both BNP and NT-proBNP were higher in women than in men. This is consistent with previous reports. Several studies have reported that both BNP and NT-proBNP are significantly higher in women than in men in the general population, regardless of age or health status.10–12,25 The physiologic basis for these sex differences in natriuretic peptide is unclear, although a stimulatory effect of female sex hormones on natriuretic peptide gene expression has been proposed.26,27 A prior population-based cohort study reported that BNP was 21% higher in women on hormone replacement therapy (HRT) than in those not on HRT.10 This suggests that BNP production may be sensitive to estrogen regulation and production.
In the present study, on unadjusted Cox regression analysis the top quartile of BNP was a risk factor for cardiovascular events compared with the lowest quartile in men, but this association disappeared after adjustment for covariates. A higher prevalence of smoking, past history of CVD and use of antihypertensive medication was also noted in men compared with women. Therefore, the weak association between BNP and cardiovascular events in men might be attributed to the different characteristics between men and women in this study. This should be confirmed in another population.
This study had several limitations. Some patients had high BNP or NT-proBNP. Although participants with symptoms of heart failure were not enrolled in the J-HOP study, we cannot completely exclude the possibility that the present cohort included patients with compensated heart failure. Given that this was an observational study, we had no information on drug treatment effects on natriuretic peptide levels during follow-up. In addition, there was a lack of data on sex hormones or menopause status, despite the possible relationship between estrogen level and the prognostic value of NT-proBNP.
Based on a large Japanese population with cardiovascular risk factors, both increased BNP and NT-proBNP were associated with cardiovascular events, and BNP and NT-proBNP were significantly stronger predictors in women than in men.
We gratefully acknowledge the numerous study investigators, fellows, nurses, and research coordinators at each of the study sites, who have participated in the J-HOP study. The physicians who participated in this study and the participating centers are listed in Appendix S1. We also gratefully acknowledge Ms Kimiyo Saito for coordination and data management, and Ms Ayako Okura for editorial assistance.
K. Kario has received research grants from Teijin Pharma Limited, Novartis Pharma K.K., Takeda Pharmaceutical Co., Ltd., Omron Healthcare Co., Ltd., Fukuda Denshi, and honoraria from Mochida Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., Daiichi Sankyo Co., Ltd., and Sumitomo Dainippon Pharma Co., Ltd. K. The other authors declare no conflicts of interest.
This study was financially supported, in part, by a grant from the 21st Century Center of Excellence Project run by Japan’s Ministry of Education, Culture, Sports, Science and Technology; a grant from the Foundation for Development of the Community (Tochigi); a grant from Omron Healthcare Co., Ltd, a Grant-in-Aid for Scientific Research (B) (21390247) from The Ministry of Education, Culture, Sports, Science and Technology (MEXT) of Japan, 2009 to 2013; and funds from the MEXT-Supported Program for the Strategic Research Foundation at Private Universities, 2011 to 2015 Cooperative Basic and Clinical Research on Circadian Medicine (S1101022) to K. Kario Funding sponsors had no role in forming the study design or conducting the study; collection, management, analysis, or interpretation of the data; preparation of the article; or decision to submit the article for publication.
Supplementary File 1
Supplementary Methods
Appendix S1. Participants and Participating Centers
Table S1. Subject baseline characteristics vs. J-HOP inclusion status
Table S2. Prognostic power for cardiovascular events vs. sex
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-18-0375