Article ID: CJ-18-0454
Article ID: CJ-18-0454
There is growing interest in nutritional status assessment as well as nutritional support as part of the comprehensive medical care for patients with not only cardiovascular diseases but also other chronic diseases.1 This is because, in hospitalized patients, protein-energy malnutrition is a common health problem and has been identified as a novel independent predictor of a poor prognosis.2–8 Given that malnutrition is often associated with cardiovascular events in heart failure (HF) patients,2,4,5 and that cachexia per se is a strong independent risk factor for death,1,9 a nutritional status assessment in patients with HF will likely prove meaningful.
Article p ????
Several parameters have been advocated to evaluate the nutritional status and used to predict prognosis in various disease conditions. The Controlling Nutritional Status (CONUT), Prognostic Nutritional Index (PIN), and Geriatric Nutritional Risk Index (GNRI) are 3 major objective indices, whereas the Subjective Global Assessment and the Mini-Nutritional Assessment short-form are subjective data assessed by medical staff. Although each parameter has advantages and disadvantages, simple and practicable methods using routinely measurable objective parameters are ideal in daily clinical practice.
The GNRI was originally proposed as a simple and accurate tool for predicting the risk of morbidity and mortality in elderly patients hospitalized with various diseases.10 There has been increasing evidence to indicate that this practical, easy-to-perform assessment tool is associated with cardiovascular events and predicts the prognosis in patients with cardiovascular diseases, including HF, as well as chronic kidney disease;2,4–8 it is therefore popular and well accepted. In this issue of the Journal, Minamisawa et al11 report that the GNRI independently predicted major adverse cardiovascular events (MACE), including cardiovascular death and hospitalization for worsening HF, in patients at risk for HF, namely, Stage A/B according to the American College of Cardiology and the American Heart Association (ACC/AHA) guidelines.12 Although previous studies have indicated that the GNRI is a useful parameter for predicting cardiovascular events in symptomatic HF subjects,2,4,5 the present study clearly showed the prognostic effect of the GNRI for risk stratification, even in patients before the development of symptomatic HF. Moreover, the mean follow-up period was over 4.7 years, and the authors ultimately observed cardiovascular events in 130 patients, which is valuable clinical information.
The ideal timing and conditions of body weight measurement must be considered, given that the study population comprised individuals with relatively mild symptoms in the current model. Because such patients (Stage A/B) do not always require hospitalization, and also because body weight varies in response to systemic treatment intervention (including diet and exercise), the timing and conditions of body weight measurement may be critical and substantially affect the GNRI. It would be interesting to investigate whether or not the GNRI measured at the time of discharge, rather than on admission, is more strongly associated with the incidence of MACE and more accurately predicts the prognosis of this population. In addition, it is important and meaningful to clarify whether or not nutritional interventions to improve the GNRI can slow the progression of HF and reduce the incidence of MACE in this patient population at an early stage.
Despite the GNRI being a promising parameter, careful interpretation is required for its specificity. First, whether or not the GNRI is the most suitable and useful valuation method among the available nutritional assessment indices (e.g., CONUT and PIN) remains unclear. Second, the GNRI was originally advocated as a prognostic indicator focused not specifically on patients with cardiovascular diseases but more generally on hospitalized patients with various diseases.10 Accordingly, the GNRI (as well as the other nutritional indices) can predict prognosis for not only HF patients but also patients with malignant diseases, and even for senescence per se (Figure). Therefore, we need to further establish for these nutritional indices whether they are independent parameters specific for cardiovascular diseases or if they more closely resemble comprehensive parameters for people with malnutrition. Further investigations and discussion will be required to address these issues, particularly considering that the present study by Minamisawa et al focused on patients with “pre-”symptomatic HF, who closely resemble the general population. At any rate, the present report has great clinical significance given that the Japanese Circulation Society has recently updated its guideline for acute and chronic HF, in which Stage A/B disease is particularly highlighted.
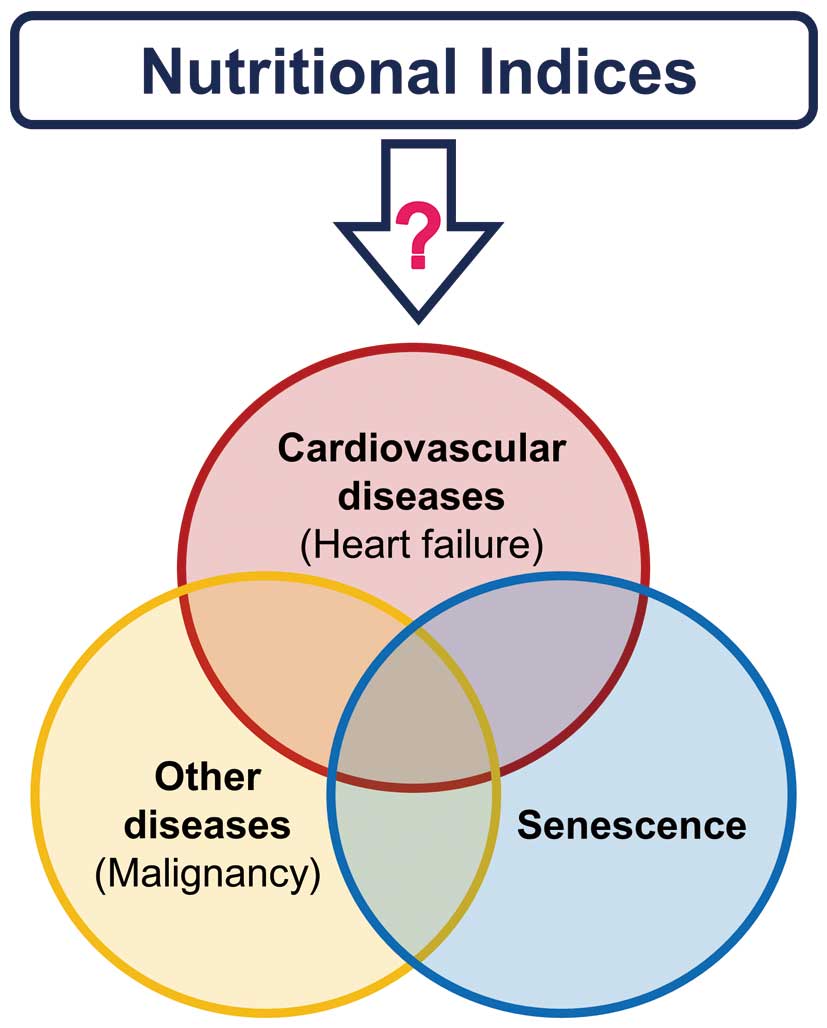
Nutritional indices reflect various disease conditions in which there may be malnutrition.