Article ID: CJ-19-0662
Article ID: CJ-19-0662
When a patient goes to a hospital, he or she usually hopes for a doctor who is experienced and knowledgeable. Something else to wish for? A female cardiologist. A new study suggests that whether your doctor is male or female could affect your life.
Article p ????
In a study reported in this issue of the Journal, Nakayama et al,1 a team of researchers at the University of Tokyo – a representative teaching-hospital in Japan – found that patients hospitalized with cardiovascular diseases and treated by female cardiologists had a lower emergency readmission risk within 30 days after discharge than did those treated by male cardiologists. The rate of total outcomes composed of emergency readmissions and 30-day mortality after discharge also proved to be lower in patients treated by female cardiologists than in those treated by male cardiologists. These findings also suggested that the beneficial effects of being treated by a female doctor on the readmission rate ware not influenced by the severity of the cardiac disease.
This beneficial effect of female doctors has been reported in US studies included elderly patients with all cardiovascular diseases. A study of more than 1.5 million hospitalized Medicare patients found that patients treated by female internists had lower 30-day mortality and 30-day hospital readmission rates than those treated by male internists.2 The difference in mortality was slight, about half a percentage point, but if male physicians had the same outcomes as female physicians, it would be estimated that 32,000 fewer patients would die each year. Another study of more than 580,000 heart patients admitted over 2 decades to emergency rooms in Florida found that female patients had a significantly higher survival rate when a woman treated them.3
There are statistically significant differences in how men and women provide medical care. For example, research evidence reveals that compared with their male peers, female physicians more often provide the following to patients: preventive care;4,5 adherence to clinical guidelines and practicing evidence-based medicine;6,7 patient-centered communication (including patients as partners in care and sharing some decision-making);8–11 more time with patients (female primary care physicians waited an average of 3 minutes before interrupting a patient. Male doctors waited an average of 47 s);10,12 psychosocial counseling (asking more psychosocial questions, offering encouragement and reassurance);10 had less trouble in treating female patients; and skillful in surgery.13
Taken together with previous evidence suggesting that male and female physicians may practice differently, the study’s findings indicate that potential differences in practice patterns between male and female physicians may have important clinical implications for patient outcomes.
Although the number of female doctors has been continuously growing worldwide in the past decades, the rate of female doctors is the lowest in Japan among the OECD countries, at 21% (median, 44%) (Figure A).14 Female cardiologists constitute 9.5% of all cardiologists.15 Moreover, the proportion of Japanese female doctors younger than age 35 years showed just a slight increase over the past decade (31% in 2006 and 33% in 2016).14 One of the reasons could be sexual discrimination before starting medical careers. In 2018 a Japanese government investigation revealed that the administrators of medical schools manipulated the entrance examination scores of female applicants to suppress the number of women by about 30% (Figure B).16 Therefore, the ratio of males and females who have passed the National Examination for Physicians has remained at roughly 7:3. Still, there is a gap in the gender ratio between medical students (35%) and doctors (21%) in 2017 (Figure A,B). Female graduates would quit working full-time because of marriage, pregnancy, and childcare and the affiliated hospitals of the universities rely heavily on a majority male workforce.
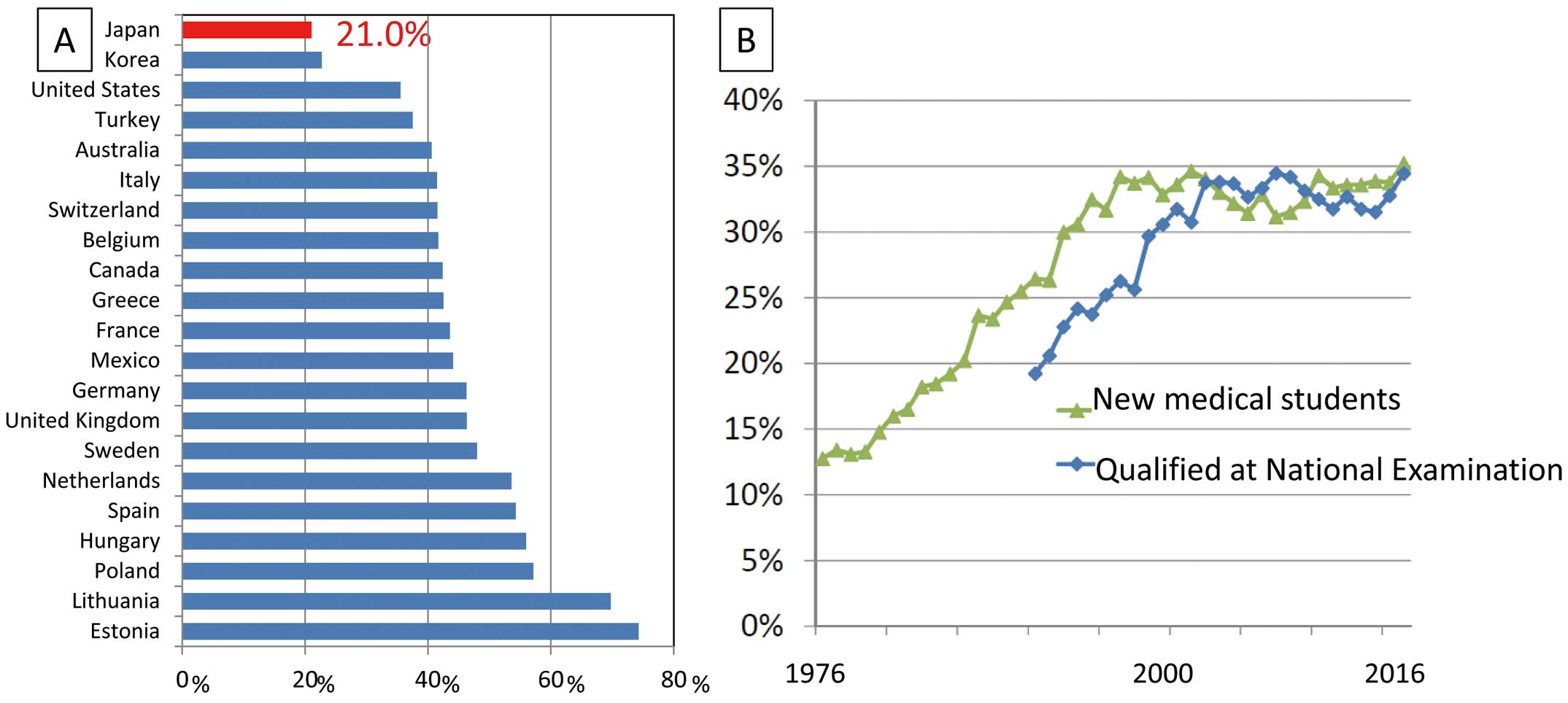
(A) Proportion of female doctors: Japan ranked last among OECD nations in 2016, with just 21% of all doctors. (B) Proportion of female new medical students and qualifying students at the National Medical Practitioners Qualifying Examination in Japan. The proportion of female new medical students has remained around 35% and not increasing after year 2000, resulting in a similar ratio of female students among those passing the National Medical Practitioners Qualifying Examination.16 The proportion of actual female doctors is even lower (21%).
To keep the numbers below those of death from overwork, so-called “karoshi”, the Health, Labor and Welfare Ministry has drafted a plan to introduce regulatory limits of 100 hours of overtime per month and 960 hours per year for general hospital doctors. As exceptions, however, doctors will be allowed to put in up to 1,860 hours of overtime per year if necessary to maintain community healthcare or in cases where intensive work is required for interns and doctors in training. In Japan, the majority of hospitals do not support flexible ways of working, which poses difficulties in balancing work and family life. It is time to introduce flexible ways of working and work sharing to utilize the capabilities of all physicians, regardless of gender, rather than restricting female students on admission to medical schools.
Despite our ignorance of how or why these beneficial patient outcomes are associated with female physicians, the more relevant point is the need to continue these investigations so that we can learn what factor or combination of factors contributes to improving outcomes. If female physicians or cardiologists are doing something different than males that not only reduces patient readmissions but improves their survival, then the salient pursuit is identifying what that is so that all physicians can use those practices to improve outcomes for all patients.
None.