Article ID: CJ-20-0499
Article ID: CJ-20-0499
Background: Sequential assessment using CT coronary angiography (coronary CT) and nuclear myocardial perfusion imaging (MPI) is considered an anatomical and functional evaluation of coronary artery disease (CAD). However, there can be unexpected radiation exposure. Hybrid MPI with stress-only nuclear MPI and rest CT-MPI using coronary CT may contribute to reducing the radiation dose in sequential assessment with nuclear MPI after coronary CT. We analyzed the diagnostic performance and total radiation dose of hybrid MPI for detection of significant CAD compared with sequential assessment using nuclear MPI after coronary CT.
Methods and Results: The results for 101 patients who underwent coronary CT, nuclear MPI and invasive coronary angiography within 3 months of all imaging were analyzed. We calculated the summed difference score (SDS) from standard nuclear MPI and hybrid SDS from hybrid MPI, which revealed myocardial ischemia. The diagnostic performance of SDS and hybrid SDS for detecting significant CAD was analyzed using receiver-operating characteristic (ROC) curve analysis. We also compared the total radiation dose of both methods. The area under the ROC curve was not different between SDS and hybrid SDS (0.901 and 0.815, P=0.079). Total radiation dose of hybrid MPI was significantly lower than standard nuclear MPI with CT angiography (4.62 mSv vs. 9.72 mSv, P<0.0001).
Conclusions: Hybrid MPI showed a precise diagnostic accuracy for significant CAD detection.
Standard nuclear myocardial perfusion imaging (MPI) is based on a combination of rest and stress perfusion imaging and clinically used for qualitative and semiquantitative assessment of ischemia by a visual scoring system.1 Rest nuclear MPI is used for the assessment of myocardial scarring or resting ischemia and is known to have diagnostic value for the estimation of prognosis,2 but has the negative effect of additional radiation exposure in the stress-first MPI protocol.
Previous studies have reported that the stress-only nuclear MPI protocol is one of the best practices for reducing the radiation dose because the subsequent rest perfusion imaging can be omitted if the stress image is completely normal.3,4 However, the requirement for all stress images to be securely assessed on the need for a subsequent resting image, can make a stress-only nuclear MPI protocol problematic. In order to resolve this difficulty of the stress-only MPI protocol, we need to obtain the information supplied by rest nuclear MPI by another non-nuclear imaging modality before stress-only nuclear MPI.
Sequential assessment with stress nuclear MPI after anatomical assessment of the coronary arteries using coronary CT with judgement of intermediate coronary stenosis or insufficient image quality is considered an appropriate clinical choice.5 Clinically, CT perfusion (CT-MPI) in coronary CT may not be assessed. However, the image dataset from coronary CT can be used not only for anatomical assessment of the coronary arteries but also for resting myocardial perfusion, including myocardial scar or infarction detection. A previous study suggested that CT-MPI showed good enough correlation with delayed enhancement on magnetic resonance imaging (MRI) for assessment of the size of the myocardial infarction (correlation coefficient r=0.93, P<0.001).6 Therefore, a protocol of stress-only nuclear MPI in sequential assessment with prior coronary CT protocol would have the benefit of reduced radiation dose and acquisition time.4 In the previous studies or in statements of hybrid imaging with a combination of nuclear MPI and cardiac CT, cardiac CT is assigned only to the detection of the anatomical region of CAD and nuclear MPI is used for physiological assessment of myocardial perfusion.7–12 The objective of our study was to analyze the diagnostic performance and total radiation dose of a hybrid MPI protocol using stress-only nuclear MPI with rest CT-MPI vs. standard sequential assessment with stress/rest nuclear MPI performed after coronary CT.
We analyzed 101 consecutive patients who underwent coronary CT, stress/rest nuclear MPI and then invasive coronary angiography (CAG) within 3 months of all imaging between 1 April 2015 and 30 September 2016. The nuclear MPI study was performed after coronary CT that resulted in equivocal coronary stenosis or insufficient image quality, in addition to direct referrals by physicians (Figure 1). Coronary anatomical findings were validated by invasive CAG following the standard stress/rest nuclear MPI or hybrid MPI protocol of stress-only nuclear MPI and rest CT-MPI (Figure 1).

Clinical setting of study. All patients underwent coronary CT, stress/rest nuclear MPI and invasive coronary angiography. (Center Upper) Standard stress/rest nuclear MPI, (Center Lower) hybrid MPI using stress-only nuclear MPI and rest CT-MPI. CT, computed tomography; MPI, myocardial perfusion imaging.
Coronary CT scanning was performed by 320-detector row CT (Aquilion One Vision edition, Canon Medical Systems, Japan). The single-phase real-time bolus tracking method with prospective gating half scan during venous injection of contrast medium (Iomeprol 350 mg/mL) in the right arm was performed for patients with heart rate <65 beats/min and no arrhythmia. The region of interest (ROI) was set in the ascending aorta in order to detect if contrast enhancement reached the threshold level (150 HU). Scan phase was set between 75% and 85% of the R-R interval on ECG for the single-phase scan. Intravenous landiolol hydrochloride (0.125 mg/kg) was used for the patients with heart rate >65 beats/min. Fast-acting nitrates were given sublingually to patients with systolic blood pressure ≥110 mmHg. All the patients were scanned with a peak tube voltage of 120 kV. CT CAG and rest CT-MPI were performed simultaneously as previously described.13 Rest CT-MPI was expressed as a multiplanar reconstruction (MPR) generated by dedicated software (Ziostation2, Ziosoft, Tokyo, Japan).
Interpretation of Rest CT-MPIThe rest CT-MPI was interpreted and scored automatically based on a measured attenuation value of the myocardium prior to the assessment of rest nuclear-MPI. The image of the left ventricular (LV) myocardium on the MPR was analyzed by the double oblique technique for assessment in the short-axial view, and the AHA 17-segment model was used for LV segmentation. Myocardial scar or hypoperfusion on the CT image was assessed with an optimized window setting based on the recommendation of the Society of Cardiovascular Computed Tomography (SCCT).14 Normal myocardium has ≥70 HU of attenuation whereas myocardial infarction is identified as a hypoattenuated segment in the range of 0–20 HU on first-pass CT-MPI.15,16 We defined that the attenuation value of myocardium from calculating as an average in the ROI of each segment in the present study, and the scoring scale of CT-MPI was assigned a quartile range of attenuation between 0 and 70 HU using a 5-point scoring system ranging from 0 to 4 (>70 HU: 0; 52.5–70 HU: 1; 35–52.4 HU: 2; 17.5–34.9 HU: 3; 0–17.4 HU: 4) (Figure 2). The summed score for rest CT-MPI was calculated and defined as the CT summed rest score (CT-SRS). In the present study, segments scoring 0 or 1 were determined as normal. CT-SRS was calculated for segments scoring ≥2.
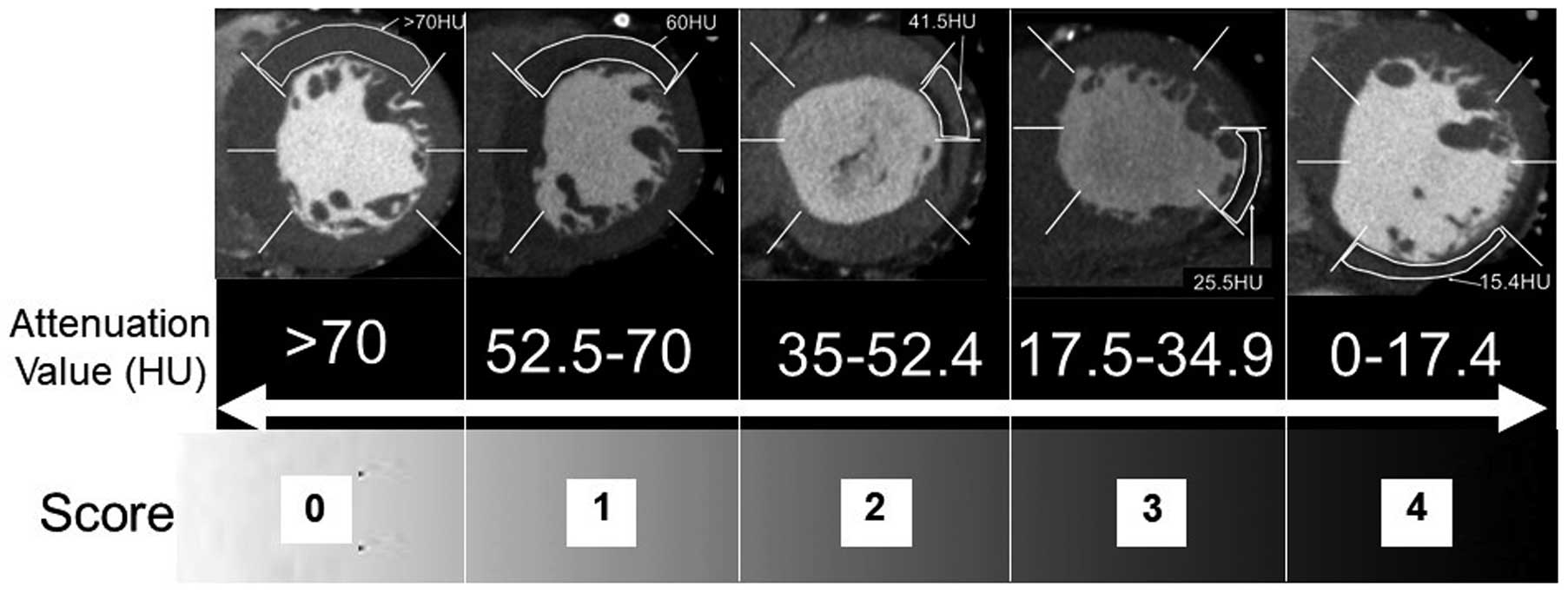
Scoring scale of CT-SRS derived from rest CT-MPI. Segmental score of CT-MPI: attenuation value >70 HU: 0, 52.5–70 HU: 1, 35–52.4 HU: 2, 17.5–34.9 HU: 3, 0–17.4 HU: 4. CT, computed tomography; HU, Hounsfield units; MPI, myocardial perfusion imaging; SRS, summed rest score.
Nuclear MPI was performed by semiconductor scanner D-SPECT (Spectrum Dynamics Medical, Israel). The stress/rest nuclear MPI protocol was a stress-first 1-day protocol with injection of 296 MBq 99 mTc-tetrofosmin for stress and 740 MBq 99 mTc-tetrofosmin for rest imaging. The stress protocol was performed by pharmacological stress (adenosine or dobutamine) or exercise stress testing. Single-photon emission computed tomography (SPECT) images (short-axis, vertical and horizontal long-axis) were generated by Autoquant (Cedars-Sinai Medical Center, LA, USA). The LV ejection fraction (EF) and end-diastolic volume (EDV) in both stress and rest ECG-gated MPI were automatically calculated by the same software.
Interpretation of Nuclear MPIThe nuclear MPI was scored semiquantitatively by 2 experienced readers based on the 17-segment model of the LV using a 5-point scoring system (0, normal uptake; 1, mildly reduced uptake; 2, moderately reduced uptake; 3, severely reduced uptake; 4, almost no uptake).17,18 Consensus reading between readers resolved discordance of image interpretation. The SRS, summed stress score (SSS) and summed difference score (SDS) were calculated as previously described.19
Hybrid Assessment of CAD With Stress-Only Nuclear MPI and Rest CT-MPIIn order to compare the diagnostic performance of detecting significant CAD between standard nuclear stress/rest MPI and the hybrid MPI, we defined a new index of hybrid SDS by subtracting the CT-SRS from SSS. Examples of the hybrid SDS for ischemic and infarcted patients are shown in Figure 3. In this study the CT-SRS and nuclear SRS were scored independently; we scored the hybrid SDS as 0 when the CT-SRS was larger than the SSS.
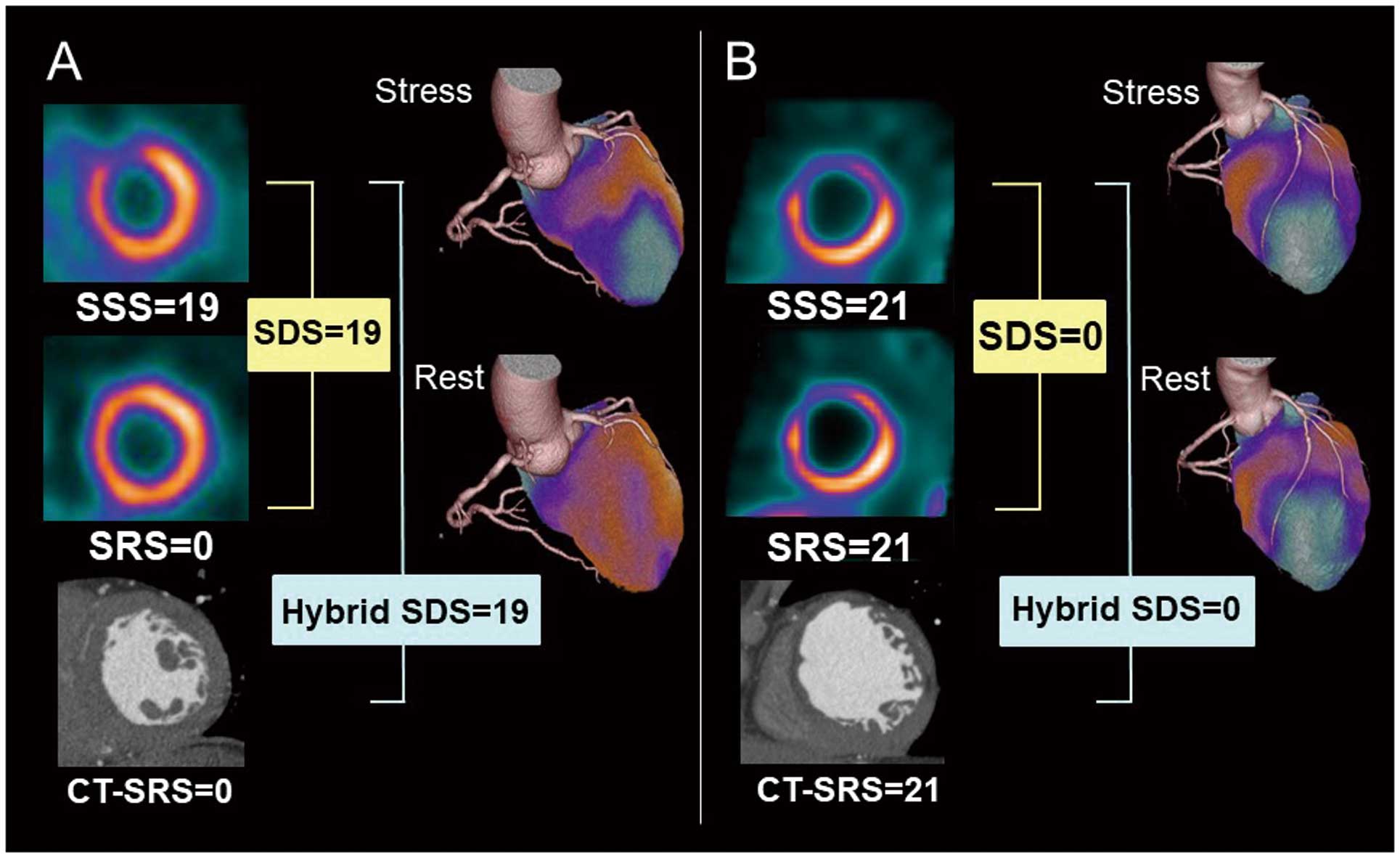
Examples of (A) stress-induced ischemia and (B) myocardial infarction.
We compared the total estimated effective radiation dose between hybrid MPI and stress/rest nuclear MPI with prior coronary CT, based on the recommendation of the International Commission on Radiological Protection (ICRP).20 For cardiac CT it was calculated using the dose-length product and a conversion factor of 0.014 mSv/(mGy · cm). The radiation dose of stress and rest nuclear MPI with 99 mTc-tetrofosmin was calculated by a conversion factor of 0.0069 mSv/MBq.
Invasive CAGAll patients underwent invasive CAG within 3 months of nuclear MPI. Significant CAD was defined as stenosis ≥75% in >1 coronary artery or ≥75% stenosis in the left main coronary artery.
Statistical AnalysisContinuous variables are expressed as median and quartile. The correlation between SRS and CT-SRS was analyzed by Spearman’s rank regression test, in addition to the same analysis between hybrid SDS and SDS. We calculated the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy in detecting significant CAD on a per-patient basis with usual equations. Paired t-test was performed for the evaluation of EF and EDV between stress and rest. Receiver-operating characteristic (ROC) curve analysis for detection of significant CAD was performed and area under the ROC curve (AUC) was calculated. We compared the ROC curves of SDS and hybrid SDS. We determined the cutoff value of hybrid SDS and SDS for detection of significant ischemia as ≥3.
The Wilcoxson test was used for comparison of total effective radiation dose between standard stress/rest nuclear MPI with prior coronary CT and hybrid MPI. Statistical analysis was performed by dedicated software (MedCalc ver. 19.1.5).
Research EthicsThis study was performed in accordance with the Declaration of Helsinki and the ethical standards of the hospital’s institutional review board (reference no. 20170904). Written informed consent was given by all the study patients.
Coronary risk factors were as follows: hypertension, 74.3%; dyslipidemia, 56.4%; diabetes, 37.6%; current smoking, 11.9%. The median body mass index (BMI) was 25.0 (kg/m2).
| Median [quartile] or n (%) | |
|---|---|
| n | 101 |
| Age | 67.0 [59.0, 74.0] |
| Female | 26 (25.7) |
| Height (cm) | 165.0 [159.0, 170.0] |
| Weight (kg) | 68.0 [56.0, 77.0] |
| BMI (kg/m2) | 25.0 [22.0, 28.0] |
| Prior MI | 16 (16.0) |
| Prior PCI | 33 (32.7) |
| Hypertension | 75 (74.3) |
| Dyslipidemia | 57 (56.4) |
| Diabetes | 38 (37.6) |
| Current smoking | 12 (11.9) |
| Family history of CAD | 2 (2.0) |
| CKD | 17 (16.8) |
BMI, body mass index; CAD, coronary artery disease; CKD, chronic kidney disease; MI, myocardial infarction; PCI, percutaneous coronary intervention.
We determined the cutoff value of hybrid SDS and SDS for detection of significant CAD as ≥3. Adenosine stress test was performed in 96 patients (95.0%), 2 patients (1.9%) underwent dobutamine stress test and 3 patients (2.9%) had an exercise stress test. Defect scores and functional parameters in nuclear MPI are listed in Table 2. The median nuclear SRS was 0 but 9 patients had nuclear SRS ≥3 and 16 patients had CT-SRS ≥3 (Tables 2,3).
| Median [quartile] | |
|---|---|
| n | 101 |
| SSS | 2.0 [1, 5.0] |
| SRS | 0 [0, 1.0] |
| SDS | 2.0 [0, 3.0] |
| EF at stress (%) | 63.0 [53.0, 69.0]* |
| EF at rest (%) | 67.0 [55.0, 73.0] |
| EDV at stress (mL) | 83.0 [64.0, 102.0]** |
| EDV at rest (mL) | 75.0 [61.0, 96.0] |
*P<0.0001, paired t-test between stress and rest EF; **P<0.0001, paired t-test between stress and rest EDV. EDV, end-diastolic volume; EF, ejection fraction; SDS, summed difference score; SRS, summed rest score; SSS, summed stress score.
| SRS (%) | CT-SRS (%) | SDS (%) | Hybrid SDS (%) | |||||
|---|---|---|---|---|---|---|---|---|
| <3 | ≥3 | <3 | ≥3 | <3 | ≥3 | <3 | ≥3 | |
| CAD (−) n=74 | 65 (87.8) | 9 (12.2) | 58 (78.4) | 16 (21.6) | 57 (77.0) | 17 (23.0) | 58 (78.4) | 16 (21.6) |
| CAD (+) n=27 | 20 (74.1) | 7 (25.9) | 20 (74.1) | 7 (25.9) | 3 (11.1) | 24 (88.9) | 7 (25.9) | 20 (74.1) |
CAD, coronary artery disease; SDS, summed difference score; SRS, summed rest score.
Median heart rate during CT scanning was 58 beats/min, the median contrast dose was 50 mL, and 15 patients (14.8%) were able to undergo coronary CT without the β-blocker.
Invasive CAG FindingsOf the 101 patients who underwent invasive CAG, 18 (17.8%) had 1-vessel disease, 5 (4.9%) had 2-vessel disease, and 4 (3.9%) had 3-vessel disease; 14 patients (13.8%) had significant stenosis in the left anterior descending coronary artery, 17 (16.8%) had it in the left circumflex coronary artery, and 9 (8.9%) had it in the right coronary artery.
Comparison of Nuclear SRS and CT-SRSThe CT-SRS score for assessment of myocardial scar or infarction significantly correlated with the SRS results from nuclear MPI (correlation coefficient r=0.511, 95% confidence interval (CI): 0.351–0.643, P<0.0001). Scatter plots and Bland-Altman plots are shown in Figure 4A,B. There were 24 patients who scored SRS=0 and CT-SRS ≥1 and none of patients had visible myocardial scar by CT-MPI. Of these cases, 11 (45.8%) were scored CT-SRS=2 and 13 cases (54.2%) had CT-SRS ≥2 in the apex and adjacent segment. There were 19 cases of CT-SRS=0 and SRS ≥1, and of these, 12 patients (63.2%) were scored SRS=1, 2 patients (10.5%) were scored SRS=2, including a patient with dilated cardiomyopathy, and 4 patients (21.1%) with chronic total occlusion (CTO) of the coronary artery had SRS ≥3. The comparison of CT-SRS and nuclear SRS in CAD (+) and CAD (−) groups are shown in Table 3. The number of patients scored CT-SRS ≥3 was larger than the number of the patients scored nuclear SRS ≥3 in the CAD (−) group, but the same number of patients scored ≥3 by CT-SRS and nuclear SRS in the CAD (+) group.

Correlation between (A,B) SRS and CT-SRS and (C,D) SDS and hybrid SDS. CT, computed tomography; SDS, summed difference score; SRS, summed rest score.
Scatter plots and Bland-Altman plots for comparison of nuclear SDS and hybrid SDS are shown in Figure 4C,D. The value of SDS and hybrid SDS were significantly correlated (r=0.837, P<0.0001, 95% CI: 0.766–0.887). The number of the patients with hybrid SDS ≥3 in CAD (+) group was similar to that for patients with SDS ≥3 in the CAD (−) group (16 (21.6%) vs. 17 (23.0%), respectively), whereas the number of the patients with hybrid SDS ≥3 was slightly lower than the number with SDS ≥3 in the CAD (+) group (20 (74.1%) vs. 24 (88.9%), respectively) (Table 3).
Diagnostic Performance of Hybrid SDSThe diagnostic performance of the hybrid SDS for detection of significant CAD on a per-patient basis was not significantly different from the result of standard stress/rest nuclear MPI (AUC: 0.815 vs. 0.901, 95% CI: −0.012 to 0.181, P=0.079; Figure 5A). Per-patient analysis, sensitivity, specificity, PPV, NPV and accuracy with a cutoff value of SDS and hybrid SDS ≥3 for detection of significant CAD were as follows: 88.9%, 77.0%, 58.5%, 95.0%, 80.2%, for SDS; 74.1%, 78.4%, 55.6%, 89.2%, 77.2%, for hybrid SDS, respectively. Comparisons of the hybrid SDS and SDS in the CAD (+) and CAD (−) groups are shown in Table 3. The hybrid SDS tended to have lower sensitivity and higher specificity than the SDS.
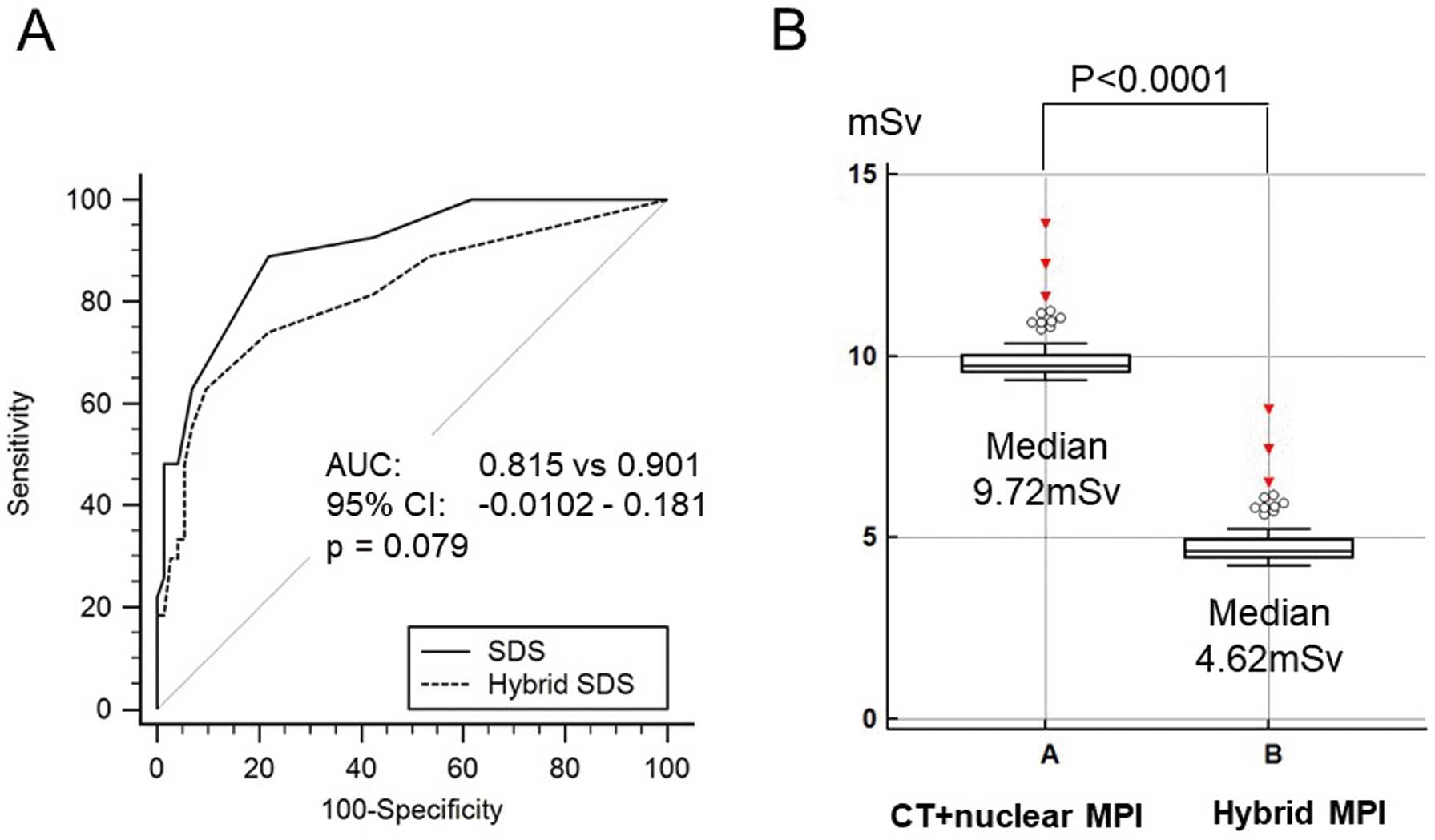
(A) Comparison of diagnostic performance of hybrid SDS and SDS by ROC analysis. (B) Total effective radiation dose of standard stress/rest MPI with prior coronary CT and hybrid MPI. CT, computed tomography; SDS, summed difference score; MPI, myocardial perfusion imaging; ROC, receiver-operating characteristic; Sv, sievert.
Total effective radiation dose for hybrid MPI using stress-only nuclear MPI with prior coronary CT angiography was significantly lower than with standard sequential assessment using stress/rest nuclear MPI with prior rest CT angiography (median: 4.62 mSv vs. 9.72 mSv, P<0.0001) (Figure 5B).
In our study, automated analysis of myocardial scarring using CT-SRS derived from the attenuation value of rest CT-MPI was significantly associated with the SRS derived from nuclear MPI with a semiconductor scanner as well as showing a correlation between the hybrid SDS and SDS. Lower sensitivity and higher specificity of the hybrid SDS may be attributable to the tendency for CT-SRS to be scored higher than the SRS, which results in a smaller score for the hybrid SDS. Although CT-SRS is not dependent on visual analysis, we may need to be careful about the tendency for a higher score of CT-SRS. In our results CT-SRS tended to show a higher defect score in the apex even in patients with SRS=0. The lower attenuation value of CT-MPI in the apical segment can be explained by the distal area of the coronary territory. Thus, it should be noted that CT-SRS tends to have higher sensitivity than nuclear SRS due to lower attenuation value in the apical segment of CT-MPI. In addition, there were several discrepant cases with CT-SRS=0 and SRS ≥2 in patients with CTO of the coronary artery, which can be attributed to underestimation of viable myocardium by the 99 mTc-labeled tracer.21
In our study, rest CT-MPI was obtained only from the first-pass narrow-band single-shot image without delayed scanning, which may not be enough for detecting myocardial scar or infarction. However, CT-MPI derived from rest coronary CT is useful for detecting myocardial scar, and the necessity of myocardial scar imaging with delayed CT scan is still controversial. In fact, Bettencourt et al reported that the diagnostic performance of rest and stress CT-MPI for detection of CAD was not significantly improved by additional delayed CT-MPI.22 Our results clearly showed a significant association between the rest nuclear SRS and CT-SRS, which may be consistent with the previous report by Yoshinaga et al that described similarity of the myocardial extraction fraction between 99 mTc tracer and iodine contrast medium.23
In the present study, we performed stress imaging with 296 MBq of 99 mTc-labeled tracer and a semiconductor scanner. It may be possible to perform stress-only nuclear MPI with a lower dose of 99 mTc. The imaging guideline of the American Society of Nuclear Cardiology (ASNC) in 2016 recommended 148–222 MBq of 99 mTc tracer for stress-only nuclear MPI if newer technology, including semiconductor scanners, is available.24 Furthermore, a previous study reported the potential of semiconductor scanners to achieve an extremely lower dose protocol using <148 MBq of 99 mTc without sacrificing image quality or diagnostic performance.25,26 Stress-only nuclear MPI with 296 MBq of 99 mTc tracer can be performed even with a conventional gamma camera in a patient with BMI ≤25 (kg/m2).24 Adjustment of 99 mTc activity based on the patient’s BMI must be considered if a conventional gamma camera is used for stress nuclear MPI if diagnostic performance is not to be reduced.24,27 Zafrir et al previously reported using a half-dose (185 MBq) 99 mTc protocol for stress nuclear MPI using a conventional gamma camera and dedicated image processing.24,28
To our knowledge, this is the first study to assess myocardial ischemia using a combination of 2 different modalities: stress nuclear MPI for depiction of MPI in the hyperemic state and rest CT-MPI for detection of myocardial scar or infarction. 99 mTc-tetrofosmin and 201Tl are the most commonly used radiopharmaceuticals for nuclear MPI in Japan. 99 mTc has a shorter half-life (6 h) than 201Tl (73 h), which may lead to minimized radiation dose for sequential assessment by stress-only nuclear MPI and rest CT-MPI. Mouden et al reported that stress nuclear MPI with a semiconductor scanner detected patients more frequently as normal, which was identical to 1-year clinical follow-up, in comparison with conventional gamma camera and concluded that semiconductor scanners lower the need for an additional rest scan, resulting in lower radiation dose.29 Stress-only nuclear MPI protocol has not been considered practical because of the difficulty of secure assessment of the need for additional rest imaging, although it is already known as an effective method of reducing the radiation dose.3,4 Our findings underscore the fact that a hybrid MPI protocol may be a method for decreasing the radiation dose by half. Thus, hybrid assessment using stress-only nuclear MPI with a semiconductor scanner after coronary CT for the assessment of rest MPI may be confidently selected.
Study LimitationsThis was a single-center retrospective study. Rest CT-MPI findings were not confirmed by cardiac MRI with delayed enhancement as the gold standard of myocardial scar assessment. Only 16% of patients had a prior myocardial infarction in the present study. Further research in a larger number of patients with prior myocardial infarction is needed.
Hybrid assessment of myocardial ischemia using a combination of stress-only nuclear MPI and rest CT-MPI had equivalent diagnostic performance and significantly reduced the total radiation dose in comparison to the standard sequential assessment with stress- and rest nuclear MPI with prior coronary CT.
None.
The authors do not have any conflict of interest to declare.
The de-identified participant data will not be shared.
The authors declare no conflicts of interest.
Name of the institutional review board (IRB): the Review Board of Clinical Research, Nihon University Hospital. Reference no. IRB: 20170904.