Article ID: CJ-20-1067
Article ID: CJ-20-1067
Background: Infective endocarditis (IE) in patients with adult congenital heart disease (ACHD) remains a diagnostic challenge due to difficulties in detecting endocardial lesions by echocardiography. 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) has shown good diagnostic performance in prosthetic valve IE. This study aimed to assess its additional diagnostic value in ACHD-associated IE and to characterize its advantages.
Methods and Results: Overall, 22 patients with ACHD and clinical suspicion of IE were retrospectively studied. 18F-FDG PET/CT was performed in addition to conventional assessment based on the modified Duke criteria. The final IE diagnosis was determined by an expert team during a 3-month clinical course, resulting in 18 patients diagnosed with IE. Seven patients (39%) were diagnosed with definite IE only by initial echocardiography. An 18F-FDG PET/CT assessment revealed endocardial involvement in the other 9 patients, resulting in the diagnosis of definite IE in 16 in total (88%). Right-sided endocardial lesions were more common (n=12, 67%) but rarely identified by echocardiography, whereas 18F-FDG PET/CT revealed right-sided lesions in 9 patients. A negative 18F-FDG PET/CT (n=7, 39%) assessment was associated with a native valve IE (71% vs. 0%). In 4 patients who were identified with not-IE, neither echocardiography nor 18F-FDG PET/CT detected any suspicious cardiac involvement.
Conclusions: In the diagnosis of ACHD-associated IE, characterized by right-sided IE, 18F-FDG PET/CT assessment should be useful.
The number of patients with adult congenital heart disease (ACHD) is increasing due to the development of congenital heart surgery.1,2 Infective endocarditis (IE) is one of the lethal complications in these patients, with a 27-to 44-fold higher prevalence than that in the non-ACHD population with valvular heart disease.3–5 The diagnosis of IE in patients with ACHD is challenging due to their congenitally and postoperatively complex anatomy and difficulties in detecting endocardial lesions by echocardiography. An inaccurate diagnosis may lead to delayed clinical management, such as administering antibiotics and performing cardiac surgery, and thus a poor prognosis. The 2015 European Society of Cardiology (ESC) guidelines for the management of IE integrated 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) into the diagnostic criteria for prosthetic valve IE, showing additional value in detecting endocardial involvement around the prosthetic valve.6 Similarly, the 2017 Japanese Circulation Society guideline on prevention and treatment of IE recommended 18F-FDG PET/CT be incorporated in the diagnostic algorithm.7 This was based on numerous studies regarding left-sided IE in a non-ACHD population.8–12 In contrast, prosthetic materials in patients with ACHD are frequently placed on the right side of the heart, potentially cause right-sided IE. However, there was only one report on ACHD-associated IE in which 18F-FDG PET/CT increased diagnostic sensitivity to prosthetic material IE.13 No study has clarified the relationship between clinical characteristics and the efficacy of an 18F-FDG PET/CT assessment in various ACHD-associated IE. Therefore, we aimed to assess the diagnostic accuracy of 18F-FDG PET/CT in various ACHD-associated IE and to characterize its advantages.
Editorial p ????
We retrospectively studied 22 consecutive patients with ACHD and clinically suspicious IE evaluated by 18F-FDG PET/CT at Kyushu University Hospital between 2012 and 2019. The final IE diagnosis was determined by an expert team and was based on data collected during a 3-month clinical course after admission.8,13
The following data were collected from the clinical records: age, sex, underlying congenital heart disease (CHD), history of prior cardiac surgery, history of prior IE, evaluation by the modified Duke criteria (DC) at admission, causative pathogens, site of IE, C-reactive protein (CRP) level, duration from the initiation of an antibiotic agent to the 18F-FDG PET/CT evaluation, heart failure episode, embolic events, indications for cardiac surgery, and in-hospital outcomes. Prosthetic materials were defined as any intravascular or intracardiac implanted foreign materials, either biological or non-biological, in permanent contact with the bloodstream.
According to the 2015 ESC modified diagnostic criteria,6 18F-FDG PET/CT was performed in addition to the conventional assessment based on the modified DC as follows:14 (1) positive blood cultures consistent with IE; (2) cardiac lesions proved by echocardiography IE; and (3) minor criteria such as predisposition, fever, vascular phenomena, immunological phenomena, and microbiological evidence. Both transthoracic echocardiography and transesophageal echocardiography were performed in all patients at admission and results were interpreted by experienced cardiologists, focusing on valve function, vegetation, and peri-annular complications, in accordance with international guidelines.15
An 18F-FDG PET/CT was performed following the standard protocol. To reduce the physiological uptake of FDG in the myocardium, the patients fasted for at least 24 h prior to the 18F-FDG PET/CT assessment. The intravenous administration of 4 MBq/kg 18F-FDG was performed after the blood glucose level (<180 mg/dL) was checked. After the patient had rested for 60 min, images were acquired using a PET/CT scanner (Discovery STE, General Electric, Boston, U.S. or Biograph Vision, Siemens, Munich, Germany). PET images were fused and analyzed with CT images. The data were analyzed and interpreted visually by a consensus of 2 experienced cardiologists. Abnormal 18F-FDG uptake was confirmed in uncorrected images and attenuation-corrected maximal intensity (MIP) images. An 18F-FDG PET/CT was classified as positive based on an intensity at the target area obviously superior to that in the liver, and negative based on the lower intensity and homogenous uptake in the liver.16 A semiquantitative analysis was also performed by using the maximal standardized uptake value (SUVmax), which was obtained by normalizing the tissue concentration of FDG activity and the patient’s weight (Vincent, FUJIFILM, Tokyo, Japan).
This study protocol was approved by the Ethics Committee of Kyushu University Hospital (Approval #2020-174) and the study complied with the Declaration of Helsinki.
Statistical AnalysisContinuous variables are shown as the median (interquartile range [IQR]) and were compared using the Mann-Whitney U-test. Categorical data are expressed as the number (percentage) and were compared using Fischer’s exact test. A 2-tailed P value <0.05 was considered statistically significant. Statistical analysis was performed with the JMP V.14 statistical software package (SAS Institute, Cary, NC, USA).
Patient characteristics are summarized in Table 1. The median (IQR) patient age was 35 (24, 43) years, and 72% of patients were male. Underlying CHD included tetralogy of Fallot in 9 patients, partial atrioventricular septal defect in 3, transposition of the great arteries in 3, and Ebstein’s anomaly in 3. Prior cardiac surgery was performed on 21 patients (95%) (all except for 1 patient with patent ductus arteriosus). Twenty patients (90%) had prosthetic materials; bioprosthetic pulmonary valve in 10, and conduit for the right ventricular outflow tract in 6. Right-sided prosthetic materials were more common than left-sided materials. The blood culture was positive in 20 patients (90%). The median duration from prior cardiac surgery to IE was 82 (28, 237) months (however, 1 patient was diagnosed 3 months after prosthetic valve replacement). There was only 1 patient with diabetes and all patients kept target blood glucose level (85 [77, 110] mg/dL) at 18F-FDG PET/CT assessment.
| n=22 | |
|---|---|
| Age at IE, years | 35 (24, 43) |
| Male | 16 (72) |
| Type of underlying congenital heart disease | |
| Tetralogy of Fallot | 9 (41) |
| Partial atrioventricular septal defect | 3 (14) |
| TGA | 3 (14) |
| Ebstein’s anomaly | 3 (14) |
| Congenitally corrected TGA | 2 (9) |
| Patent ductus arteriosus | 1 (4) |
| Bicuspid aortic valve | 1 (4) |
| Prior cardiac surgery | 21 (95) |
| Number of cardiac surgeries | 3 (2, 4) |
| Prosthetic material implantation | 20 (90) |
| Mechanical valve | |
| Aortic valve | 4 |
| Mitral valve | 2 |
| Tricuspid valve | 2 |
| Bioprosthetic valve | |
| Pulmonary valve | 10 |
| Tricuspid valve | 2 |
| Valved aortic graft | 2 |
| Conduit for the RVOT | 6 |
| Patches for the RVOT | 6 |
| Patches for a VSD | 6 |
| Epicardial permanent pacemaker | 2 |
| Duration from prior surgery, months | 82 (28, 237) |
| Prior IE | 4 (18) |
| Blood culture positive | 20 (90) |
| Causative pathogen | |
| Staphylococcus species | 10 (50) |
| Streptococcus species | 4 (20) |
| Others | 6 (30) |
| Blood glucose level at PET/CT, mg/dL | 85 (77, 110) |
Continuous variables are expressed as the median (interquartile range), and categorical data are expressed as n (%). IE, infective endocarditis; PET/CT, 18F-fluorodeoxyglucose positron emission tomography/computed tomography; RVOT, right ventricular outflow tract; TGA, transposition of the great arteries; VSD, ventricular septal defect. Some patients had one or more prosthetic devices implanted.
During a 3-month clinical course after admission, 18 of 22 patients were diagnosed with IE by an expert team (Figure 1). The other 4 patients with tetralogy of Fallot, transposition of the great arteries (TGA), Ebstein’s anomaly, and congenitally corrected TGA were identified with alternative cause of fever, including pneumonia, aortic infection, and skin abscess in 2.

Diagnosis of infective endocarditis (IE) by an expert team. During a 3-month clinical course after admission, 18 of 22 patients were diagnosed with IE by an expert team. The other 4 patients were identified with alternative diagnosis.
In 18 patients who were diagnosed with definite IE during a 3-month clinical course, the initial blood culture was positive; one of the major criterions of modified DC. Transthoracic echocardiography (TTE) was positive in 6 patients, and transesophageal echocardiography (TEE) was positive in 1 patient, at admission. Thus, only 7 of 18 patients (39%) were diagnosed with definite IE based on the modified DC, and the other 11 patients with negative echocardiography were considered to have possible IE based on 1 major criterion and 1 or 2 minor criteria by the initial assessments (Figure 2). Prosthetic material was involved as the site of IE in 3 of these definite IE patients (aortic mechanical valves in 2 patients and a pulmonary bioprosthetic valve in 1 patient). Of those with possible IE, 9 had pulmonary bioprosthetic valves, and 2 had tricuspid bioprosthetic valves. Two patients received a permanent epicardial pacemaker, but no patient in this study developed a cardiac device infection (CDI). Patients with possible IE based on the echocardiographic assessment (n=11) had more right-sided IE (100% vs. 14%, P=0.03), more prosthetic material IE (100% vs. 43%, P=0.01) and shorter intervals after the latest cardiac surgery (67 [34, 86] vs. 169 [7, 297] months, P=0.04) than patients diagnosed with definite IE only by the echocardiographic assessment (Table 2).
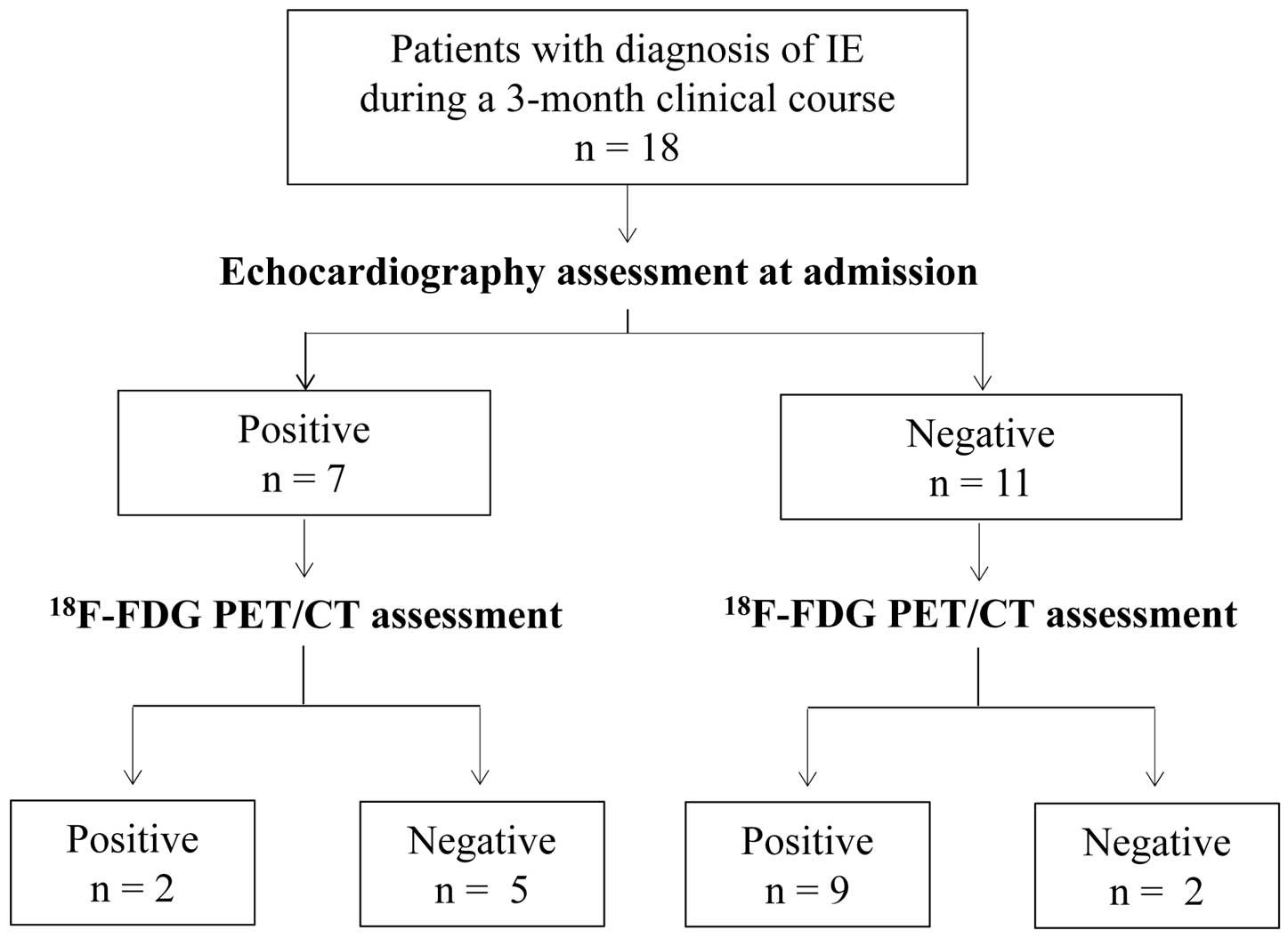
Initial assessment of infective endocarditis (IE) by echocardiography and 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) (18F-FDG PET/CT). In 18 patients who were diagnosed with definite IE during a 3-month clinical course, echocardiographic assessment at admission identified 7 patients as positive. The addition of 18F-FDG PET/CT for patients with negative echocardiography revealed endocardial lesions in 9 additional patients, resulting in the initial diagnosis of definite IE in a total of 16 of 18 patients. In contrast, the 18F-FDG PET/CT assessment for patients with positive echocardiography revealed endocardial lesions only in 2 patients.
| Positive for echocardiography (n=7) |
Negative for echocardiography (n=11) |
P value | |
|---|---|---|---|
| Age, years | 39 (27, 45) | 25 (21, 37) | 0.40 |
| Male | 5 (71) | 6 (55) | 0.40 |
| Site of IE | |||
| Right-sided IE | 1 (14) | 11 (100) | |
| Left-sided IE | 6 (86) | 0 (0) | 0.01* |
| Prosthetic material IE or Native valve IE | |||
| Prosthetic material IE | 3 (43) | 11 (100) | |
| Native valve IE | 4 (57) | 0 (0) | 0.01* |
| Prior cardiac surgery | 6 (86) | 11 (100) | 0.10 |
| Number of cardiac surgeries | 2 (2, 3) | 3 (2, 4) | 0.09 |
| Prosthetic device implantation | 4 (57) | 11 (100) | 0.04* |
| Duration from prior surgery, months | 169 (7, 297) | 67 (34, 86) | 0.04* |
| Prior IE | 1 (14) | 3 (27) | 0.50 |
| Causative pathogen | |||
| Staphylococcus species | 3 (43) | 6 (55) | |
| Streptococcus species | 2 (29) | 2 (18) | |
| Others | 2 (29) | 3 (27) | 0.80 |
Continuous variables are expressed as the median (interquartile range), and categorical data are expressed as n (%). *P values <0.05, indicating statistical significance. IE, infective endocarditis.
The 18F-FDG PET/CT assessment combined with the modified DC for patients with possible IE revealed endocardial inflammatory lesions in 9 additional patients, resulting in the diagnosis of definite IE in a total of 16 patients (Figure 2). The diagnostic sensitivity was significantly increased from 39% to 88% after the addition of 18F-FDG PET/CT information to the echocardiography. The sites of IE identified only by the 18F-FDG PET/CT assessment were a bioprosthetic pulmonary valve in 5 patients, graft for a pulmonary artery in 2, right outflow tract conduit with a pulmonary bioprosthetic valve in 1, and right-sided patch for a ventricular septal defect in 1. As expected, 18F-FDG PET/CT showed additional value in detecting prosthetic material IE. It is worth noting that right-sided IE was rarely detected by echocardiography but clearly identified by 18F-FDG PET/CT (Figure 3). All 9 patients diagnosed with definite IE after the addition of 18F-FDG PET/CT had right-sided IE, whereas only 1 patient diagnosed by echocardiography had right-sided IE (100% vs. 14%, P=0.01; Table 3).

Representative cases of infective endocarditis (IE) with a positive 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) (18F-FDG PET/CT) assessment in patients with normal initial echocardiography. A 25-year-old man with repaired tetralogy of Fallot and pulmonary valve replacement (Bioprosthetic valve 23 mm with a graft patch). He had intermittent fever and a positive blood culture for Staphylococcus capitis. The first transthoracic echocardiography (TTE) did not show any abnormalities around the pulmonary prosthetic valve (A). The 18F-FDG PET/CT performed 4 days after the first TTE showed abnormal uptake around the pulmonary prosthetic valve, resulting in the diagnosis of definite IE. The 18F-FDG PET/CT images are presented as merged (PET+CT) attenuation-corrected maximal intensity (MIP) projection images (B). A 21-year-old man with repaired tetralogy of Fallot and pulmonary valve replacement (Bioprosthetic valve 21 mm with a conduit). He had continuous fever after a motorcycle accident and a positive blood culture for Staphylococcus epidermidis. The first TTE did not show any abnormalities around the pulmonary prosthetic valve and a conduit (C). The 18F-FDG PET/CT performed 5 days after the first TTE showed abnormal uptake around the pulmonary prosthetic valve (D), resulting in the diagnosis of definite IE. A 37-year-old man with repaired tetralogy of Fallot and pulmonary valve replacement (Bioprosthetic valve 19 mm with a conduit) and Down syndrome. He was transported to our hospital with septic shock and a positive blood culture for Staphylococcus aureus. The first TTE did not show any abnormalities around the pulmonary prosthetic valve and a conduit (E). The 18F-FDG PET/CT performed 18 days after the first TTE showed abnormal uptake around the pulmonary prosthetic valve and a conduit (F), resulting in the diagnosis of definite IE. Ao valve, aortic valve; PA, pulmonary artery; RVOT, right ventricular outflow tract.
| DC (n=7) |
DC with PET/CT (n=9) |
P value | |
|---|---|---|---|
| Age, years | 39 (27, 45) | 25 (21, 31) | 0.05 |
| Male | 5 (71) | 3 (33) | 0.31 |
| Duration of antibiotics, days | 23 (12, 34) | 18 (7, 27) | 0.70 |
| CRP level at PET/CT, mg/dL | 1.8 (0.7, 2.5) | 1.0 (0.2, 4.2) | 0.40 |
| Blood culture positive at PET/CT | 1 (14) | 1 (11) | 1.00 |
| Site of IE | |||
| Right-sided IE | 1 (14) | 9 (100) | |
| Left-sided IE | 6 (86) | 0 (0) | 0.01* |
| Prosthetic material IE or Native valve IE | |||
| Prosthetic material IE | 3 (43) | 9 (100) | |
| Native valve IE | 4 (57) | 0 (0) | 0.02* |
| Prior cardiac surgery | 6 (86) | 9 (100) | 0.44 |
| Number of cardiac surgeries | 2 (2, 3) | 4 (2, 4) | 0.14 |
| Prosthetic device implantation | 4 (57) | 9 (100) | 0.06 |
| Duration from prior surgery, months | 169 (7, 297) | 73 (41, 92) | 0.32 |
| Prior IE | 1 (14) | 2 (22) | 0.69 |
| Causative pathogen | |||
| Staphylococcus species | 3 (43) | 6 (67) | |
| Streptococcus species | 2 (29) | 1 (11) | |
| Others | 2 (29) | 2 (22) | 0.57 |
Continuous variables are expressed as the median (interquartile range), and categorical data are expressed as n (%). *P values <0.05, indicating statistical significance. CRP, C-reactive protein; DC, Duke criteria; IE, infective endocarditis; PET/CT, 18F-fluorodeoxyglucose positron emission tomography/computed tomography.
18F-FDG PET/CT was negative in 5 patients with definite IE diagnosed by the modified DC with echocardiography. The other 2 patients were considered to have possible, but not definite, IE even after the 18F-FDG PET/CT assessment (Figure 2). In total, 7 patients (39%) were negative for 18F-FDG PET/CT. Characteristics of a negative cardiac 18F-FDG PET/CT assessment are summarized in Table 4. Patients with a negative 18F-FDG PET/CT assessment had more native valve IE (71% vs. 0%, P=0.02), left-sided IE (71% vs. 9%, P=0.02) and were older (45 [39, 74] vs. 25 [21, 27] years, P=0.01) than those with a positive 18F-FDG PET/CT assessment. The duration of antibiotic therapy to the time of the 18F-FDG PET/CT assessment tended to be longer in the negative group (23 [8, 34] days vs. 16 [5, 25] days, P=0.49), but the difference was not significant. At the time of the 18F-FDG PET/CT assessment, the rate of a positive blood culture (0% vs. 18%, P=0.49) and CRP level (1.8 [0.7, 2.1] mg/dL vs. 1.0 [0.2, 3.0] mg/dL, P=0.43) was not different between the negative and positive groups. Blood glucose level (114 [94, 121] vs. 83 [79, 99] mg/dl, P=0.02) was higher in the negative group, but both are within the target level. The causative pathogen tended to be different between the 2 groups (Staphylococcus, Streptococcus, others: 43%, 14%, and 43% vs. 9%, 73%, and 18% respectively, P=0.05); however, the differences did not reach statistical significance. We confirmed a lower SUVmax in 18F-FDG PET/CT-negative patients than in 18F-FDG-positive patients (0 [0, 4.6] vs. 9.4 [5.7, 12.3], P=0.01). We showed a representative case of a negative 18F-FDG PET/CT in a patient with positive echocardiography in Figure 4.
| Negative for PET/CT (n=7) |
Positive for PET/CT (n=11) |
P value | |
|---|---|---|---|
| Age, years | 45 (39, 74) | 25 (21, 27) | 0.01* |
| Male | 6 (86) | 5 (45) | 0.15 |
| Duration of antibiotics, days | 23 (8, 34) | 16 (5, 25) | 0.49 |
| CRP level at PET/CT, mg/dL | 1.8 (0.7, 2.1) | 1.0 (0.2, 3.0) | 0.43 |
| Blood culture positive at PET/CT | 0 (0) | 2 (18) | 0.49 |
| Blood glucose level at PET/CT, mg/dL | 114 (94, 121) | 83 (79, 99) | 0.02* |
| Site of IE | |||
| Right-sided IE | 2 (29) | 10 (91) | |
| Left-sided IE | 5 (71) | 1 (9) | 0.02* |
| Prosthetic material IE or Native valve IE | |||
| Prosthetic material IE | 2 (29) | 11 (100) | |
| Native valve IE | 5 (71) | 0 (0) | 0.02* |
| Prior cardiac surgery | 2 (29) | 11 (100) | 0.39 |
| Number of cardiac surgeries | 3 (2, 3) | 4 (2, 4) | 0.14 |
| Prosthetic device implantation | 4 (57) | 11 (100) | 0.04* |
| Duration from prior surgery, months | 169 (29, 296) | 67 (22, 86) | 0.09 |
| Prior IE | 2 (29) | 2 (18) | 1.00 |
| Causative pathogen | |||
| Staphylococcus species | 3 (43) | 1 (9) | |
| Streptococcus species | 1 (14) | 8 (73) | |
| Others | 3 (43) | 2 (18) | 0.05 |
| SUVmax | 0 (0, 4.6) | 9.4 (5.7, 12.3) | 0.01* |
Continuous variables are expressed as the median (interquartile range), and categorical data are expressed as n (%). *P values <0.05, indicating statistical significance. SUVmax, maximal standardized uptake value. Other abbreviations as in Table 3.

Representative case of infective endocarditis (IE) with a negative 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) (18F-FDG PET/CT) assessment in a patient with positive echocardiography. A 39-year-old man with partial atrioventricular septal defect and Down syndrome. He underwent left atrioventricular valvuloplasty twice and had no prosthetic materials. He had fever and a positive blood culture for Streptococcus sanguinis. The first transthoracic echocardiography (TTE) (A) and transesophageal echocardiography (TEE) (B) revealed vegetations on the left atrioventricular valve and severe regurgitation, resulting in the diagnosis of definite IE. The 18F-FDG PET/CT performed 24 days after the first TTE showed no cardiac uptake, including around the left atrioventricular valve (white arrow). The 18F-FDG PET/CT images are presented as merged (PET+CT) attenuation-corrected maximal intensity (MIP) projection images (C). The surgeries were performed after antibiotic therapy due to uncontrollable heart failure. The postoperative histological examination verified the pathological lesions as healed IE. Thereafter, there has been no recurrence of heart failure and IE.
All patients were alive at the time of discharge. They were initially treated with antibiotic therapy according to recommended guidelines. Seven patients underwent cardiac surgery due to the following reasons: uncontrollable infection in 4, uncontrollable heart failure in 2, and multiple systemic emboli in 1. For the 4 patients with uncontrollable infection, only 18F-FDG PET/CT could detect the endocardial lesions in advance of cardiac surgery, and the postoperative histological examination verified the pathological lesions as active IE. These patients had undergone right-sided cardiac surgery and right-sided IE; there was a bioprosthetic pulmonary valve in 3 patients and a conduit for the right ventricular outflow tract with a biological prosthetic valve in 1. These data suggest that an 18F-FDG PET/CT assessment could result in selecting an appropriate treatment strategy for ACHD-associated IE, especially right-sided prosthetic material IE.
Diagnostic Specificity of the Modified DC in Combination With an 18F-FDG PET/CTIn the present study, 4 of 22 patients were diagnosed with not-IE by an expert team, because firm alternate diagnosis explaining the fever emerged. In 4 patients who were identified with not-IE, the initial blood culture was positive in 2 (50%) and neither echocardiography nor 18F-FDG PET/CT assessment showed suspicious of the cardiac involvement. Thus, all of these 4 patients were not diagnosed with IE by the modified DC in combination with 18F-FDG PET/CT, whereas half of them were considered to have possible IE based on 1 major criterion (positive blood cultures consistent with IE) and 2 minor criteria (predisposition and fever), and other 2 patients was rejected with IE. Therefore, the diagnostic specificity of the modified DC in combination with 18F-FDG PET/CT was 100% in the study.
The present study demonstrated that an 18F-FDG PET/CT assessment, in addition to the modified DC with echocardiography could improve the diagnostic value in ACHD-associated IE, with an increase in sensitivity from 39% to 88%. These findings are consistent with a previous report on IE associated with ACHD and prosthetic material.13
This study was the first to show an advantage of 18F-FDG PET/CT, especially in right-sided IE, in patients with ACHD. Emerging evidence showing the increased diagnostic accuracy of 18F-FDG PET/CT in prosthetic IE has focused mainly on left-sided IE.8–12 No previous study has examined the efficacy of 18F-FDG PET/CT in right-sided IE, except for CDIs.12 In contrast, the present study assessed right-sided cardiac involvement, including a bioprosthetic pulmonary valve without CDIs, by using 18F-FDG PET/CT. We thus demonstrated the advantage of an 18F-FDG PET/CT assessment on right-sided cardiac structures even without cardiac devices.
Right-sided IE accounts for 40% of all ACHD-associated IE,3 whereas general IE accounts for only 5–10%.17 In this study, the rate of right-sided IE in the present study (67%) is higher than that found in previous data. In general, echocardiography plays a key role in the assessment of IE, with high sensitivity to detect endocardial involvement (75% by TTE and 85–90% by TTE).18 However, in right-sided IE with involvement of the prosthetic pulmonary valve or a reconstructed conduit in the right ventricular outflow tract, the sensitivity distinctly decreases to 62% by TTE and 57% by TEE.19 In accordance with this report, right-sided cardiac involvement was rarely detected by TTE and TEE in the present study. Anatomic interference or acoustic shadowing caused by prosthetic materials may limit the sensitivity of TTE, though TTE is more advantageous than TEE for right-sided structures that are located anteriorly and close to a TTE transducer. In addition, the sensitivity of echocardiography can be further limited in patients with moderate or severe CHD,1,2 due to their complicated anatomy and postoperative status with prosthetic materials.
Contrast-enhanced multislice CT is expected to improve the sensitivity in detecting life-threatening periannular complications according to the 2015 ESD guidelines for the management of IE. However, multislice CT is insufficient for detecting right-sided endocardial lesions due to difficulties in adjusting the timing of the contrast injection during both right-sided and left-sided phases.20,21 Therefore, the significant benefits of 18F-FDG PET/CT need to be emphasized for right-sided IE or prosthetic material IE in ACHD-associated IE.
It has been reported that the diagnostic sensitivity of 18F-FDG PET/CT for native valve IE is relatively poor9,22 compared to that for prosthetic valve IE. Regarding ACHD-associated IE, native valve IE rarely contains a literal ‘native’ valve but rather one after valvuloplasty, but a previous study on an 18F-FDG PET/CT assessment for ACHD-associated IE did not include these patients.13 In the present study, we investigated patients with a native valve after valvuloplasty and found that an 18F-FDG PET/CT showed limited diagnostic value for IE with valvuloplasty. This finding may be due to the continuous movement of cardiac valves during acquisition and the small size of vegetations, which might make it difficult to distinguish them from background activity.
Recent studies have reported a negative 18F-FDG PET/CT assessment in patients with native valve IE, a low CRP level or a long duration of antibiotic therapy.8,19 In the present study, we observed a similar tendency for native valve IE, and an echocardiography could reveal the lesion. Therefore, to detect endocardial lesions, the selection of proper modalities according to their advantages is important (i.e., 18F-FDG PET/CT for right-sided IE and prosthetic material IE and echocardiography for native valve IE).
It was reported that a high blood glucose level was associated with an 18F-FDG PET/CT false positive due to physiological uptake of FDG in the myocardium.23 Our finding of a higher, but within target, blood glucose level in the 18F-FDG PET/CT negative group might have no clinical significance.
In the present study, the patients fasted for at least 24 h prior to the 18F-FDG PET/CT assessment and the blood glucose level was 85 (77, 110) mg/dL at the 18F-FDG PET/CT assessment with all patients keeping the target level (<180 mg/dL). 18F-FDG PET/CT images were analyzed and interpreted visually by a consensus of experienced cardiologists according to a previous study.16 As a result, the SUVmax was higher in 18F-FDG PET/CT-positive patients than in 18F-FDG-negative patients (9.4 [5.7, 12.3] vs. 0 [0, 4.6], P=0.01). These findings were consistent with those from a previous report, although there was no consensus for a threshold value of SUVmax.10,24 This result suggests that the definition of a positive 18F-FDG PET/CT assessment in the present study was reasonable.
Study LimitationsThere are several limitations to the present study that should be acknowledged. First, we studied a low number of patients enrolled from a single center, though various underlying CHDs were included in the present study. Therefore, caution is needed when generalizing the present findings. Interesting, the diagnostic specificity in the study demonstrated 100%, which is incredibly high. This was calculated only by using 4 cases. It has been reported that FDG uptake may occur in the perivalvular area even in the absence of infection due to the migration and proliferation of inflammatory cells, myofibroblasts, and capillary endothelial cells as a healing process.25 Therefore, its diagnostic specificity might be limited, and an interpretation of 18F-FDG PET/CT should be performed carefully. Second, the timing of the 18F-FDG PET/CT assessment was later after the initiation of antibiotic therapy (17 [7, 25] days) than that in other studies (5–6 days),8,13 which might be due to the retrospective nature of the present study. As a consequence, the number of 18F-FDG PET/CT-negative patients might be higher, although other modalities could have revealed endocardial lesions in these subjects in the present study.
18F-FDG PET/CT can improve the diagnostic value of ACHD-associated IE, especially right-sided IE. Native valve IE and older age were associated with a negative 18F-FDG PET/CT assessment. This imaging modality could be an useful tool in the comprehensive assessment of ACHD-associated IE, characterized by right-sided and postoperative IE and complicated anatomy.
This study was supported by a grant from the Japan Society for the Promotion of Science, Tokyo, Japan (Grants-in-Aid for Young Scientists 20K17085 to A.I.).
The authors declare no conflicts of interest. H. Tsutsui is a member of Circulation Journal’s Editorial Team.
The study was approved by the Ethics Committee of the Faculty of Medicine at Kyushu University (Reference no.: 2020-174).
1. Will the individual deidentified participant data (including data dictionaries) be shared? Yes.
2. What data in particular will be shared? All de-identified participant data collected during the study.
3. Will any additional, related documents be available? No.
4. When will the data become available and for how long? After this article is accepted, and for 1 year.
5. By what access criteria will the data be shared (including with whom)? E-mail to the corresponding author. The data will be shared with anyone on a request basis.
6. For what types of analysis, and by what mechanism will the data be available? For any purpose, the data will be shared as Excel files via E-mail.