Article ID: CJ-21-0107
Article ID: CJ-21-0107
An 86-year-old woman was admitted to hospital for heart failure due to organic mitral insufficiency. Transthoracic echocardiography (TTE) on admission revealed normal left ventricular (LV) contraction and severe mitral regurgitation (MR) due to posterior mitral leaflet prolapse (Figure A). ECG on admission showed atrial fibrillation with no significant ST-T abnormalities (Figure B-1). Transcatheter mitral valve repair (TMVr) was successfully performed using the MitraClip NT device (Abbott Vascular, Santa Clara, CA, USA). Postoperative transesophageal echocardiography showed no wall motion abnormality, and successful placement of the clip in the flail region of the mitral valve. However, 4 h postoperatively, she developed sudden nausea and chest distress. ECG showed inverted T waves and QT prolongation in leads V2–5 (Figure B-2). The myocardial troponin-I and B-type natriuretic peptide levels were markedly elevated (1.25 ng/mL and 443 pg/mL, respectively). TTE showed severe apical LV hypokinesis despite hyperkinesis in the basal segments (Figure C,D; Supplementary Movie 1). Coronary angiography revealed no significant coronary artery disease; left ventriculography revealed apical akinesia and basal hyperkinesia (Figure E,F). Takotsubo syndrome (TTS) was confirmed based on the International Takotsubo Registry criteria. TTE showed normalization of apical LV motion, and ECG showed normalization of the ST-segment 46 days after onset (Figure G; Supplementary Movie 2). In this case, coronary air embolism via an iatrogenic atrial septal defect was also considered. Furthermore, transient LV systolic dysfunction due to afterload mismatch has been reported after TMVr. However, our patient showed the abnormal LV wall motion characteristic of TTS, and we suspect that psychological stress was the main trigger. To our knowledge, this is the first case of TTS after TMVr.
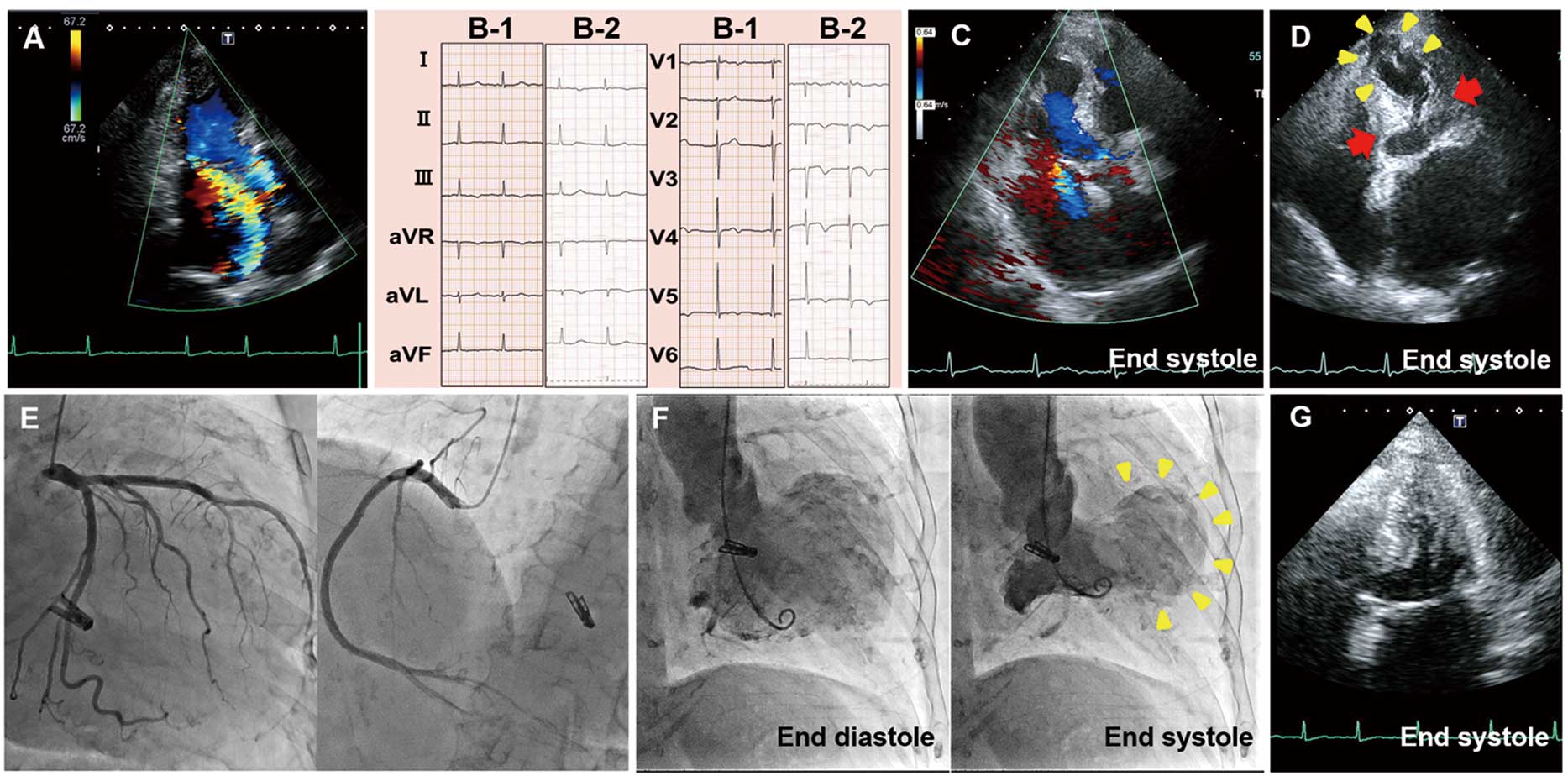
(A) Preprocedural TTE. (B-1) ECG on admission and (B-2) postprocedural day 1. (C) Postprocedural TTE showing mild residual MR. (D) TTE at onset of TTS symptoms showing apical akinesia (yellow arrowheads) and basal hyperkinesia (red arrows). (E) Coronary angiography. (F) Left ventriculography showing apical akinesia (yellow arrowheads) and basal hyperkinesia. (G) Follow-up TTE 46 days later. MR, mitral regurgitation; TTE, transthoracic echocardiography.
T.A. and T.N. are members of Circulation Journal’s Editorial Team.
Supplementary Movie 1. TTE showing severe apical LV hypokinesis despite hyperkinesis in the basal segments..
Supplementary Movie 2. TTE showing normalization of apical LV motion 46 days after onset of takotsubo syndrome.
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-21-0107