Abstract
Background: This study investigated whether the age of patients undergoing pacemaker implantation is increasing.
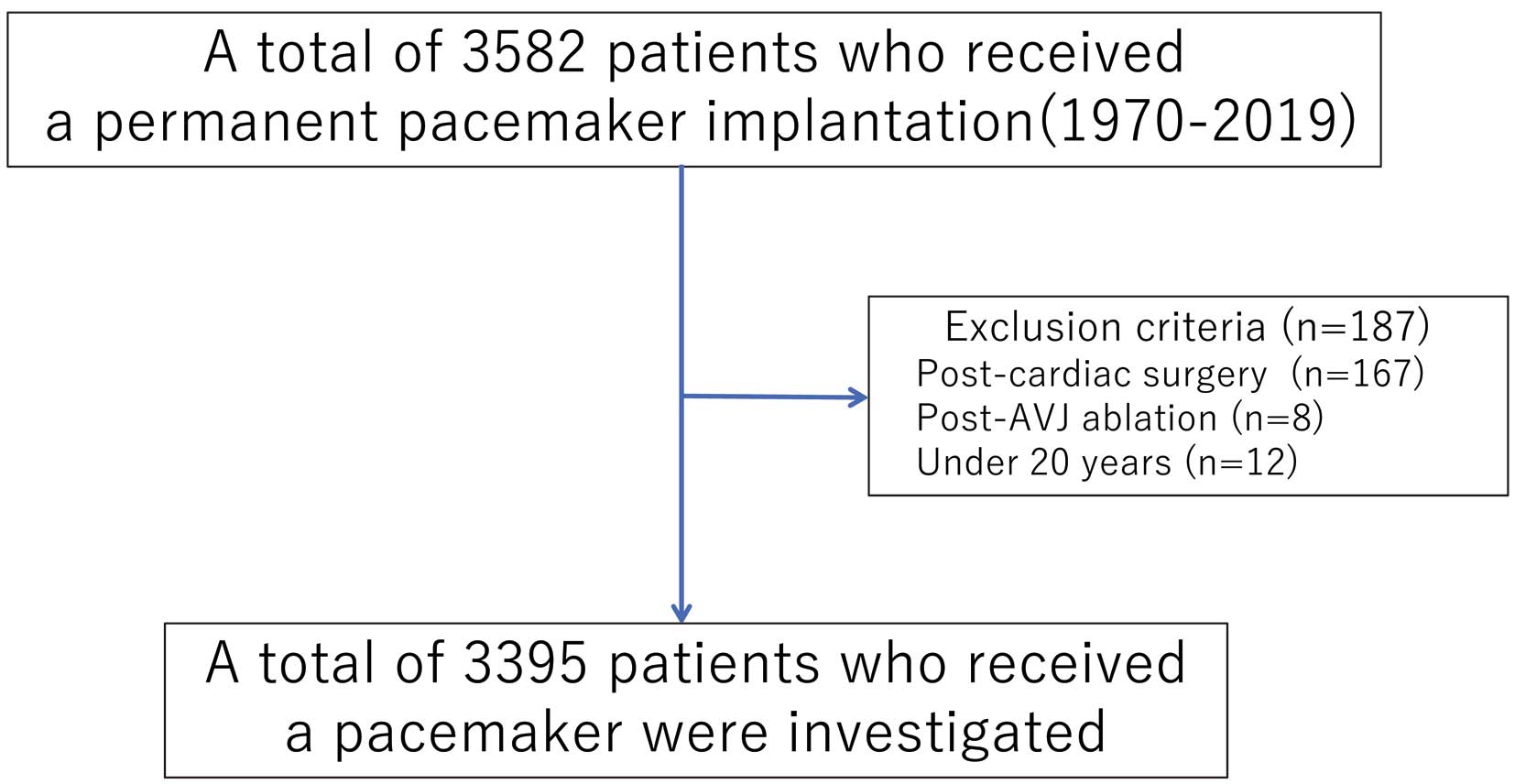
Methods and Results: This study retrospectively reviewed the consecutive cases of 3,582 patients who underwent an initial pacemaker implantation at our hospitals because of symptomatic bradyarrhythmias between 1970 and 2019. The exclusion criteria were: patients with AV block due to cardiac surgery or AV junction ablation, and patients aged <20 years. The patients were divided into 5×10-year groups: those treated in the 1970s (1970–1979), 1980s (1980–1989), 1990s (1990–1999), 2000s (2000–2009), and 2010s (2010–2019). A total of 3,395 patients satisfied the study criteria. The average age at which the patients underwent a first pacemaker implantation increased across the 10-year periods: 63.7±13.2 years in the 1970s, 66.2±12.6 years (1980s), 69.1±12.4 years (1990s), 72.0±11.1 years (2000s), and 75.8±10.0 years (2010s) and advanced significantly in the 1990s, 2000s, and 2010s compared to the 1970s (all P<0.001). The ratio of patients aged ≥80 and ≥90 years increased from 10.6% and 0% in the 1970 s to 38.2% (P<0.001) and 5.2% (P= 0.017) in the 2010s, respectively.
Conclusions: The average age at initial pacemaker implantation increased by 12.1 years over the last 50 years in Japan. In particular, the ratios of ≥80 and ≥90 years as the patients age increased significantly.
The aging of populations is poised to emerge as a worldwide demographic phenomenon. There were 703 million persons aged ≥65 years in the world in 2019. Globally, the share of the population aged ≥65 years increased from 6% in 1990 to 9% in 2019.1 The total population in Japan as of October 1, 2018 was 126.44 million people, and the number of individuals aged ≥65 years was 35.58 million (28.1% of the Japanese population).2 Japanese society has the highest percentage of older and elderly individuals in the world.3 From a historical perspective, population aging represents a human success story, based on successful public health measures, medical advances, and economic and social developments overcoming diseases, injuries, and early deaths. In many parts of the world, people are living much longer, and there will thus be an accompanying increase in patients with sick sinus syndrome (SSS) or atrioventricular block (AVB) who need the implantation of a cardiac pacemaker (PM). As mentioned previously, Japan is the world’s fastest aging country and the aging of the Japanese population is advancing rapidly, as reported by the Ministry of Health, Labor and Welfare.4 Many clinicians realize this situation during their daily medical practice in Japan; however, there are limited data concerning the aging of PM patients,5–8 especially those with no clinical data in Japan. Therefore, we conducted the present study to investigate whether the age of patients who undergo PM implantation has increased over the past decades.
Methods
We retrospectively analyzed the consecutive cases of 3,582 patients aged ≥20 years who underwent an initial implantation of a permanent PM for symptomatic bradyarrhythmias according to the JCS/JHRS guideline9 between January 1970 and December 2019 at the three affiliated hospitals of Juntendo University: Juntendo University Hospital, Urayasu Hospital, and Nerima Hospital. The number of patients treated at each hospital is shown in Table 1. All three hospitals are located in Tokyo or its suburbs.
Table 1. Number of Study Population Patients in Each Hospital Per 10-Year Period
| | 1970s | 1980s | 1990s | 2000s | 2010s |
|---|
| Juntendo University Hospital (JUH) | 108 | 221 | 303 | 691 | 670 |
| Urayasu Hospital | – | – | – | 300 | 677 |
| Nerima Hospital | – | – | – | 243 | 369 |
| Total | 108 | 221 | 303 | 1,234 | 1,716 |
The exclusion criteria were as follows: patients who had an implanted PM for AVB due to cardiac surgery, and those who had undergone catheter ablation for tachyarrhythmia.
Data CollectionPatient data for age, gender, diagnosis (including indication for PM implantation) were obtained from the patient’s medical records and our database for device implantation. We divided the indications for PM into 2 groups: SSS and AVB. We categorized bradycardia with atrial fibrillation or atrial flutter as AVB. The data for the average life expectancy in Japan was obtained from the website of the Ministry of Health, Labor and Welfare.4
Statistical AnalysisWe divided the study population into the following 5×10-year groups: 1970s: 1970–1979; 1980s: 1980–1989, 1990s: 1990–1999, 2000s: 2000–2009, and 2010s: 2010–2019. Patient age, gender, and diagnosis data are presented per 10-year period. We compared the data of these parameters in the 1970 s with those of the other 4 periods. Continuous variables are presented as the mean±standard deviation (SD). Categorical variables are presented as counts and percentages (%). The average age of each 10-year group was compared using Tukey’s honestly significant difference test. The statistical analyses were performed using JMP version 12.0 (SAS Institute, Cary, NC, USA). Significant differences were defined as those with a probability (P) value <0.05.
Results
We analyzed the data from a total of 3,395 patients who satisfied the study criteria during the 50-year period from 1970 to 2019 (Figure 1). The mean age of the study population was 73.0 years; 53.5% were male, and 52.8% were diagnosed with AVB. The distribution of the age, gender, indication for PM, and device in the study population is shown in Table 2. Of these, 12 patients had additional indicating the use of a biventricular pacemaker (3 with cardiac resynchronization therapy pacemaker and 9 with cardiac resynchronization therapy defibrillator). The 11 patients who suffered from both SSS and AVB were from both the SSS and AVB groups, and thus in the comparisons of the SSS and the AVB groups, the study population was 3,406 patients.
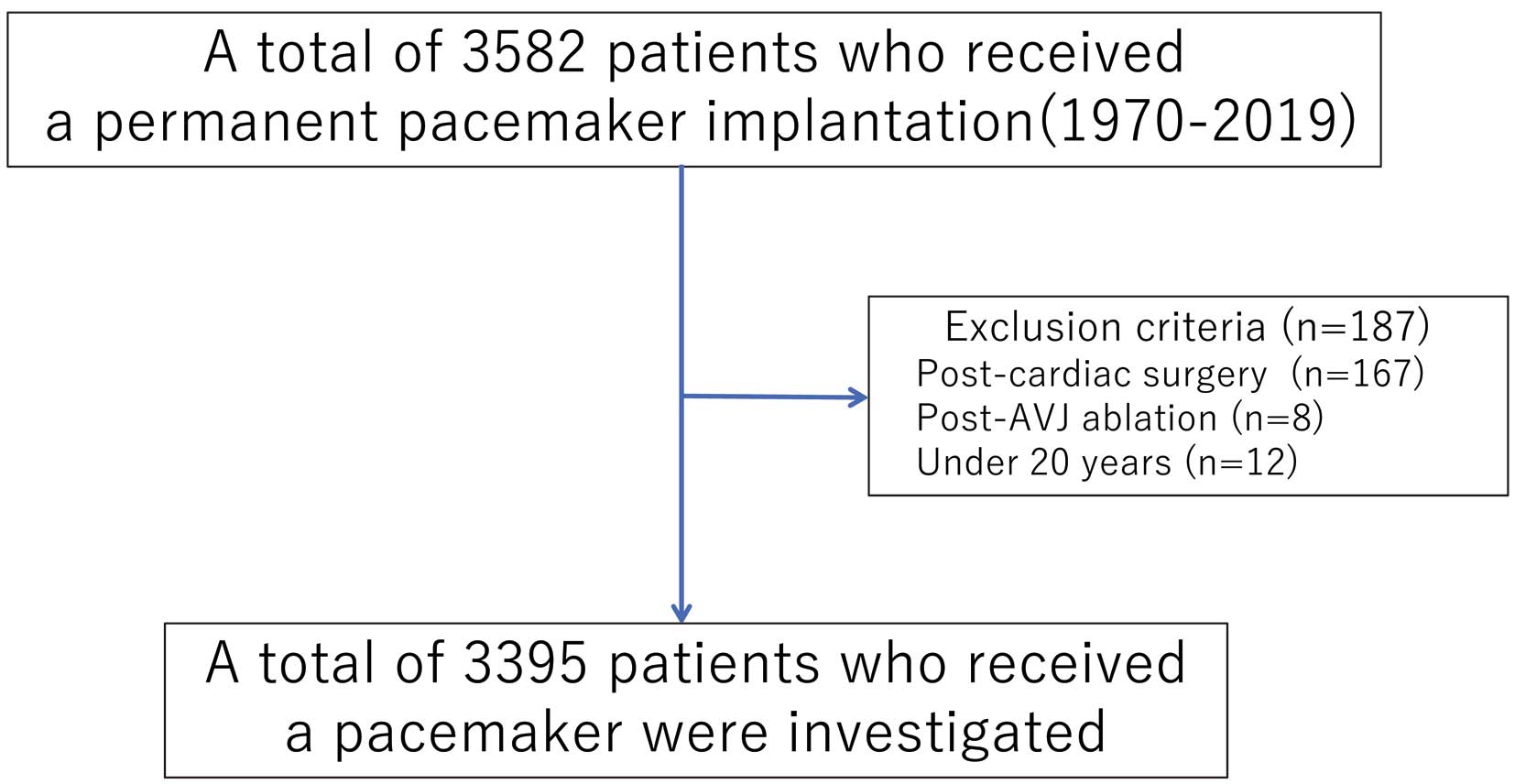
Table 2. Distribution of Age, Gender, Indication for PM, and PM Device in the Study Population
| Characteristics | Patients (n=3,395) |
|---|
| Average age (mean±SD, years) | 72.99±11.34 |
| Age (years) | n (%) |
| 20–29 | 15 (0.44) |
| 30–39 | 22 (0.64) |
| 40–49 | 96 (2.8) |
| 50–59 | 254 (7.5) |
| 60–69 | 682 (20.0) |
| 70–79 | 1,315 (38.7) |
| 80–89 | 880 (25.9) |
| >90 | 131 (3.9) |
| Gender |
| Male | 1,818 (53.5) |
| Female | 1,577 (46.5) |
| Indication* |
| SSS | 1,608 (47.2) |
| AVB | 1,798 (52.8) |
| Device |
| PM | 3,383 (99.65) |
| CRT-P/CRT-D | 12 (0.35) |
*Including 11 patients who had both SSS and AVB. AVB, atrioventricular block; CRT-D, cardiac resynchronization therapy defibrillator; CRT-P, cardiac resynchronization therapy pacemaker; PM, pacemaker; SSS, sick sinus syndrome.
The average age at which the patients underwent a first implantation of a PM increased across the 10-year periods: 63.7±13.2 years in the 1970s, 66.2±12.6 years in the 1980s, 69.1±12.4 years in the 1990s, 72.0±11.1 years in the 2000s, and 75.8±10.0 years in the 2010s (shown as a bar graph in Figure 2). There was a significant increase in the average age from the 1970s to the 1990s, 2000s, and 2010s (all P<0.001). The average age at the initial PM implantation increased by 12.1 years from the 1970s to the 2010s. The average life expectancy in Japan (also shown as a line graph in Figure 2), rose gradually from 73.1 years in the 1970s to 83.0 years in 2010s.4 The patients’ average age at PM implantation and the life expectancy in Japan exhibited a similar trend in this period.

Regarding the percentage of males receiving PM implantation during each 10-year period, 50.0% were men in the 1970s, 54.2% in the 1980s, 52.9% in the 1990s, 55.8% in the 2000s and 52.2% in the 2010s. The ratio of males and females in each period was not significantly different among the 5 periods. The average age stratified by gender in each period is shown in Figure 3 (shown as a bar graph for each gender); it increased across the 10-year periods and showed a similar trend with the life expectancy in Japan (shown as a line graph in each figure) for both genders.4
Although the age at the initial PM implantation for both genders increased significantly over the decades, the average age of the female patients advanced further (14.7 years: from 61.3 years in the 1970s to 76.0 in the 2010s, P<0.001) compared to that of the males (9.6 years: from 66.1 years in the 1970s to 75.7 in the 2010s, P<0.001).
Figure 4 shows the trend in the ratio of age distribution at the initial PM implantation. The ratio of elderly patients (≥70 years) remarkably increased after 2000s, especially for those aged ≥80 years in 2010s. The ratio of patients aged ≥80 years per period increased significantly from 10.6% in the 1970 s to 21.6% in the 1990s, 24.8% in the 2000s and 38.2% in the 2010s (P=0.013, =0.001 and <0.001, respectively). The ratio of patients aged ≥90 years per period also increased from 0% in the 1970s to 5.2% in the 2010s (P=0.017).
Figure 5 shows the ratio of SSS and AVB in each age group. The ratio of AVB was predominant in young (<60 years) and older (≥80 years) groups.
The trend in the ratio of single- and dual-chamber PMs was analyzed in 3,069 patients, excluding 326 patients with permanent atrial fibrillation (AF) or atrial flutter (AFL). This trend was shown in Figure 6. Dual chamber (DDD) and single atrial (AAI) pacing expanded in the 1980s, and dual-chamber PM (DDD) drastically increased after the 1990s.
Discussion
The major findings of this study were as follows: (1) the average age of the patients at their initial PM implantation rose by 12.1 years (from 63.7 years to 75.8 years) over the last 50 years in parallel with the increase in life expectancy in Japan. This aging was more prominent in females (a 14.7-year increase) compared to males (a 9.6-year increase); (2) the ratio of the elderly (≥70 years) patients remarkably increased after the 2000s. The ratio of patients aged ≥80 years increased from 10.6% (1970s) to 38.2% (2010s) (P<0.001), and that of patients aged ≥90 years increased from 0% (1970s) to 5.2% (2010s) (P=0.017); and (3) dual-chamber PM drastically increased after the 1990s.
Comparison With Similar Previous StudiesSeveral studies have reported that PM patients are becoming older.5–8 An investigation conducted in Western Australia reported that the mean age at PM implantation increased from 73.8 years in 1995–1999 to 75.3 years in 2005–2009 (P<0.001).5 In a study from the United States, the average age of dual-chamber PM patients was 73.3 years in 1993 and it increased to 75.4 years in 2009 (P<0.001); the average age of the single-ventricular PM patients was 77.5 years in 1993 and it increased to 80.1 years in 2009 (P<0.001).6 The Spanish pacemaker registry also showed that the mean age at PM implantation increased from 74.9 years in 1994–2003 to 78.7 years in 2019.7,8 Although our present study findings mirror those of the cited studies, these former investigations covered periods of ≤25 years. The present study was of the longest period: a 50-year period from 1970 to 2019, including the average age during each 10-year period and the trend in aging for the PM implantation in each gender. The previous studies indicated that the average age advanced 1.3–1.9 per 10 years,5–8 whereas we observed that the average age increased by more; that is, 2.9 years during the 1990s–2000s and by 6.7 years during the 1990s–2010s, which is in close parallel to the life expectancy in Japan. Since the Japanese population is the most aged in the world,3 we speculated that the marked increase in the number of elderly individuals in Japan may be accompanied by a higher age of patients needing a PM implantation, as shown in Figure 4.
Reasons for Increasing Age at the Initial Pacemaker ImplantationThere are several reasons for the increasing age at the initial PM implantation. First, aging is associated with increases in arrhythmias and conduction disorders. Factors related to arrythmias in the elderly include the following: (1) physiologic aging (coronary artery stenosis, fibrosis of conduction system, decrease in sinoatrial cells, atrial dilatation, interstitial fibrosis, calcification of valves and annulus); (2) pathologic changes (ischemic heart disease, myocardial hypertrophy due to hypertension, etc.); and (3) functional factors (influences of lung disease, renal insufficiency, etc. and drugs).10–12 The number of pacemaker cells in the sinoatrial node decreases significantly after the age of 60 years, and by the age of 75 years, it decreases to <10% of the number in young adults.13
The factors influencing SSS are an extreme decrease in the number of sinoatrial cells beyond the physiological range, fibrosis, and fatty infiltration, in addition to the decrease of sinoatrial cells within the physiological range.12,14 The interstitial fibrosis in cells also influences the atrioventricular conduction system;11,12,14 however, a disorder of the atrioventricular conduction system is not likely to induce AVB immediately, and the addition to calcification of valves and annulus causes AVB.12,14,15 Calcification of the cardiac skeleton, particularly in the region including the central fibrous body and the left-sided valves (aortic and mitral valve rings) is the result of aging, although the degree of calcification varies.13,14 The AV node, AV bifurcation, and the proximal left and right bundle branches are located near the central fibrous body, and thus the delay conduction occurs with increasing age-related changes.13 Our result of the ratio of SSS and AVB in each age group (Figure 5) showed that the ratio of AVB was predominant in the young (<60 years) population, and SSS became dominant in those who were aged in their 60s; however, AVB prevalence increased in older (≥80 years) population. Therefore, we could not conclude which is more influenced by aging in PM patients, SSS or AVB. Larger population studies may be needed to clarify this issue.
As shown in Figure 4, a remarkable increase in the number of elderly (≥70 years) patients after the 2000s seems to contribute to the aging of patients receiving an initial PM implantation in our study.
The prolongation of life expectancy due to successful public health measures and medical advances can be expected to have an effect on patients’ age at the initial PM implantation. The progress in PM technology may also have expanded the indications or PM implantation. The development of PM leads, devices, and other instruments could allow us to more easily implant cardiac PMs. Our results demonstrated the widespread use of dual-chamber PM after the 1990s, as shown in Figure 6. Advancement of atrial leads may have contributed to choosing either AAI or DDD PMs in the 1980–1990s, and more sophisticated leads might have had an influence on the increase in DDD with a backup ventricular lead instead of AAI after the 2000s.
Study LimitationsThere are several limitations in this study. It was a retrospective analysis, and the consecutive data could be obtained only from a single center (Juntendo University Hospital) between the 1970s and 1990s. In our affiliated hospitals, one hospital (Nerima Hospital) was opened in 2007, so the data were only obtained since the 2000s. In the other hospital (Urayasu Hospital), which was opened in 1984, however, the consecutive data were not captured in the 1980s and 1990s. In addition, cardiac pacing therapy was not widely used before the 1980s.16 Pacemakers were made non-invasively programmable in the mid-1970s, and dual-chamber PMs were developed by the end of the 1970s.16 This historical background would reflect that the sample size from 1970 to 1990 is very limited compared to that after the 2000s.17 Nonetheless, we demonstrated that the age at initial PM implantation advanced significantly in Japan, which has not been reported officially so far. We believe that our study results are important in understanding the medical situation in Japan.
Conclusions
The results of our analysis demonstrated that the average age at initial PM implantation rose by 12.1 years over the last 50 years, which is in parallel with the life expectancy in Japan. Notably, the ratios of patients aged ≥80 and ≥90 years increased significantly during this period.
Disclosures
T. Minamino is a member ofCirculation Journal’s Editorial Team.
IRB Information
Juntendo Clinical Research and Trial Center (20-122) approved this study.
References
- 1. United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019 Highlights. United Nations New York; 2019. https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf (accessed October 1, 2021).
- 2. Cabinet Office Japan June 2019. Annual Report on the Ageing Society [Summary]. FY 2019. https://www8.cao.go.jp/kourei/english/annualreport/2019/pdf/2019.pdf (accessed October 1, 2021).
- 3. Scherbov S. Aging Demographic Data Sheet 2018. 15 January 2018. https://iiasa.ac.at/web/home/research/researchPrograms/WorldPopulation/PublicationsMediaCoverage/ModelsData/AgingDemDataSheet2018_web.pdf (accessed October 1, 2021).
- 4. Ministry of Health, Labor and Welfare. Trend of life expectancies at birth. https://www.mhlw.go.jp/english/database/db-hw/lifetb10/1.html (accessed October 1, 2021).
- 5. Bradshaw PJ, Stobie P, Knuiman MW, Briffa TG, Hobbs MS. Trends in the incidence and prevalence of cardiac pacemaker insertions in an ageing population. Open Heart 2014; 1: e000177.
- 6. Greenspon AJ, Patel JD, Lau E, Ochoa JA, Frisch DR, Ho RT, et al. Trend in permanent pacemaker implantation in the United States from 1993 to 2009: Increasing complexity of patients and procedures. J Am Coll Cardiol 2012; 60: 1540–1545.
- 7. Samartín RC. Spanish Registry of Pacemakers. Second Official Report of the Working Group on Cardiac Stimulation of the Spanish Society of Cardiology (1994–2003). Rev Esp Cardiol 2004; 57: 1205–1212.
- 8. Jiméneza MP, Pérezb ÓC, Garcíac JC, Bertomeu-Gonzálezd V. Spanish Pacemaker Registry. 17th Official Report of the Section on Cardiac Pacing of the Spanish Society of Cardiology (2019). Rev Esp Cardiol 2020; 73: 1038–1048.
- 9. Kurita T, Nogami A, Abe H, Ando K, Ishikawa T, Imai K, et al. 2018 JCS/JHRS Guideline on Non-Pharmacotherapy of Cardiac Arrhythmias. https://www.j-circ.or.jp/cms/wp-content/uploads/2018/07/JCS2018_kurita_nogami.pdf (accessed January 1, 2022).
- 10. Mori T. Cardiac Arryhthmias in the Elderly [in Japanese]. Nichinoishi 2016; 65: 136–143.
- 11. Mizra M, Strunets A, Shen W, Jahangir A. Mechanisms of arrhythmias and conduction disorders in older adults. Clin Geriatr Med 2012; 28: 555–573.
- 12. Tsuneda T, Inoue H. Arrhythmias in elderly population and their management [in Japanese]. Nichiroishi 2005; 42: 261–270.
- 13. Chow G, Marine J, Fleg J. Epidemiology of arrhythmias and conduction disorders in older adults. Clin Geriatr Med 2012; 28: 539–553.
- 14. Ohkawa S. Gender and aging as vulnerable factors developing arrhythmias: Aging changes of the conduction system. Jpn J Electrocardiology 2008; 28: 109–118.
- 15. Fukuda K, Nakata Y, Sakurai H, Takagi T, Okada R, Kitamura K. Right bundle branch block and left axis deviation due to the calcification at the central fibrous body [in Japanese]. Shinzo 1977; 9: 525–529.
- 16. Aquilina O. A brief history of cardiac pacing. Images Paediatr Cardiol 2006; 8: 17–81.
- 17. Uslan DZ, Tleyjeh IM, Baddour LM, Friedman PA, Jenkins SM, St Sauver JL, et al. Temporal trends in permanent pacemaker implantation: A population-based study. Am Heart J 2008; 155: 896–903.