Article ID: CJ-22-0454
Article ID: CJ-22-0454
Background: Although a door-to-balloon (D2B) time ≤90 min is recognized as a key indicator of timely reperfusion for patients with ST-segment elevation myocardial infarction (STEMI), it is unclear whether regional disparities in the prognostic value of D2B remain in contemporary Japan.
Methods and Results: We retrospectively analyzed 17,167 STEMI patients (mean [±SD] age 68±13 years, 77.6% male) undergoing primary percutaneous coronary intervention. With reference to the Japanese median population density of 1,147 people/km2, patients were divided into 2 groups: rural (n=6,908) and urban (n=10,259). Compared with the urban group, median D2B time was longer (70 vs. 62 min; P<0.001) and the rate of achieving a D2B time ≤90 min was lower (70.7% vs. 75.4%; P<0.001) in the rural group. In-hospital mortality was lower for patients with a D2B time ≤90 min than >90 min, regardless of residential area, whereas multivariable analysis identified prolonged D2B time as a predictor of in-hospital death only in the rural group (adjusted odds ratio 1.57; 95% confidence interval 1.18–2.09; P=0.002). Importantly, the rural-urban disparity in in-hospital mortality emerged most distinctively among patients with Killip Class IV and a D2B time >90 min.
Conclusions: These data suggest that there is a substantial rural-urban gap in the prognostic significance of D2B time among STEMI patients, especially those with cardiogenic shock and a prolonged D2B time.
Early reperfusion by primary percutaneous coronary intervention (PPCI) is critical to reducing mortality for patients with ST-segment elevation myocardial infarction (STEMI).1 Door-to-balloon (D2B) time is a key indicator of early reperfusion and quality of care for STEMI. Since the 2013 American College of Cardiology Foundation/American Heart Association guidelines for STEMI recommended that D2B time should be reduced to 90 min or less at PPCI-capable hospitals,2 D2B time became the focus of quality improvement initiatives.3 Accordingly, nowadays, the achievement rate for D2B time ≤90 min in the US has increased to >80%.4 The guideline-based management has contributed to standardizing critical care for STEMI and narrowing the performance gap between rural and urban hospitals.
In Japan, a small island nation with a high-density population, acute myocardial infarction (AMI) is a major cause of mortality, just as in other developed nations.5 In Japan, there are 1,108 PPCI-capable hospitals (vs. 1,752 in the US).6 In terms of emergency care of AMI, patients in rural areas are less likely to be transported directly to PPCI-capable hospitals and miss undergoing timely PPCI as compared with patients in urban areas.7 Rural-urban differences in in-hospital mortality from AMI exist not only in Japan, but also in other countries.8–11 However, there few studies have explored the disparity of D2B time and clinical outcomes between rural and urban areas in a society with a declining birthrate and aging population. Thus, in the present study, we examined regional differences in D2B time and their prognostic impact in a super-aged society by analyzing data from a nationwide real-world registry study, namely the Japan Acute Myocardial Infarction Registry (JAMIR).
JAMIR is a nationwide and large-scale registry consisting of 10 representative regional AMI registry groups in Japan, with 214 PPCI-capable hospitals were involved (Supplementary Figure 1). A detailed protocol of JAMIR has been published previously.12 The present study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and was approved by the institutional review board of each participating hospital. Written informed consent was not required, because the present study was a non-invasive observational study and anonymized personal information appropriately.
Study SubjectsThe patient flow diagram is shown in Figure 1. Briefly, these study subjects were derived from the JAMIR database, in which 45,471 consecutive patients with AMI within 24 h of onset were enrolled between January 2011 and December 2016. Of these patients, 31,605 were diagnosed with STEMI. From there, patients without available D2B data (n=11,826) and those who underwent PPCI >6 h after hospital presentation (n=2,612) were excluded. Finally, 17,167 STEMI patients who were treated with PPCI within 24 h of symptom onset and 6 h of admission were analyzed in the present study. Compared with patients included in the analysis, those who were excluded were more likely to be older and female, and to have coronary risk factors, left main trunk lesions as culprit vessels, higher Killip classes, and higher in-hospital mortality (Supplementary Table).
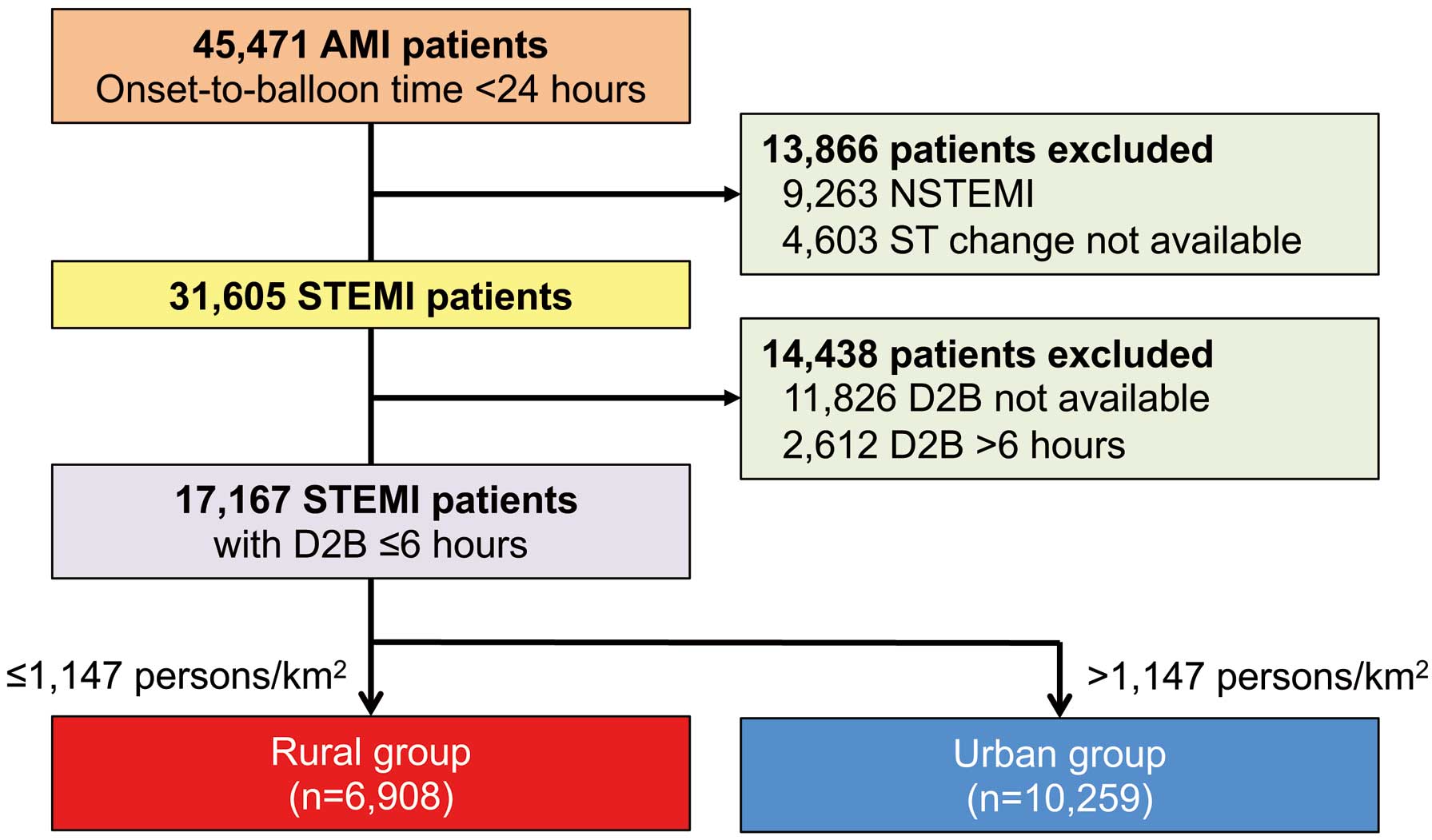
Flowchart for selection of the study population. Patients with ST-elevation myocardial infarction (STEMI) were divided into 2 groups (i.e., rural and urban) according to the Japanese median population density. AMI, acute myocardial infarction; D2B time, door-to-balloon time; NSTEMI, non-ST-segment elevation myocardial infarction.
The population density where patients resided was determined in reference to the 2010 Population Census conducted by the Statistics Bureau, Ministry of Internal Affairs and Communications of Japan.13 As in a previous study,10 patients enrolled in the present study were divided into 2 groups according to the median population density of 1,147 people/km2 into those residing in a rural area and those residing in an urban area. By region, the rural group consisted of 89 facilities, and the urban group consisted of 125 facilities.
Definitions and Clinical OutcomesSTEMI was diagnosed on the basis of ST-elevation ≥0.1 mV in at least 2 contiguous leads, a new left bundle branch block or new Q waves accompanied by chest pain, and/or a rise in cardiac biomarkers.14 Detailed definitions of risk factors for cardiovascular disease, including hypertension, dyslipidemia, diabetes, and smoking, have been published previously.15 PPCI was defined as procedures performed within 24 h after symptom onset, and the onset-to-door (O2D) time was defined as the interval from the onset of symptoms of ischemia to the arrival at PPCI-capable hospitals. D2B time was defined as the time from arrival at a PPCI-capable hospital to first balloon inflation or device use, and the onset-to-balloon (O2B) time (total ischemic time) was defined as the time from symptom onset to first balloon inflation or device use. Cut-off values of 90 min for delayed D2B time and 120 min for delayed O2D time were selected with reference to guidelines for STEMI and other previous reports.2,16–18 When assessing the severity of STEMI at presentation, Killip classification was used, and patients were divided into 3 groups as follows: (1) patients with no evidence of heart failure (Killip Class I); (2) patients with symptomatic heart failure (Killip Class II and III); and (3) patients with cardiogenic shock (CS; Killip class IV).
The primary outcome in the present study was in-hospital mortality.
Statistical AnalysisContinuous variables are presented as the mean±SD or median with interquartile range (IQR), whereas categorical variables are presented as percentages. Group comparisons were performed using the Mann-Whitney U test for continuous variables and the Chi-squared test for categorical variables. Multivariable analysis was used to clarify independent predictors of D2B time >90 min and in-hospital mortality. Clinically relevant factors and variables that differed significantly between rural and urban groups (P<0.1) were selected as covariates for the multivariable logistic regression model with the stepwise backward elimination procedure. Trends in in-hospital mortality for 4 D2B time intervals (0–45, 46–90, 91–180, and 181–360 min) were examined using the Cochran–Armitage trend test. Two-sided P<0.05 was considered statistically significant. All data analyses were performed using JMP version 16.0.0 (SAS Institute, Cary, NC, USA) and SPSS version 21 (IBM, Armonk, NY, USA).
The clinical characteristics of the study subjects according to residential area are summarized in Table 1. Compared with patients in urban areas, those in rural areas were older, had a greater number of coronary risk factors (e.g., hypertension, dyslipidemia, and diabetes), and a higher prevalence of symptomatic heart failure (Killip Class ≥II) at presentation. In both groups, the rate of ambulance transport usage was approximately 90%.
| Overall | Rural group | Urban group | P value | |
|---|---|---|---|---|
| Age (years) | 67±13 | 68±13 | 67±13 | 0.002 |
| Male sex (%) | 77.6 | 78.2 | 77.2 | 0.15 |
| Hypertension (%) | 65.4 | 68.4 | 61.6 | <0.001 |
| Diabetes (%) | 31.7 | 32.7 | 30.3 | <0.001 |
| Dyslipidemia (%) | 50.0 | 52.7 | 46.6 | <0.001 |
| Smoking (%) | 43.2 | 36.8 | 47.6 | <0.001 |
| Ambulance transport (%) | 88.5 | 89.1 | 88.1 | 0.055 |
| O2D time (min) | 123 [60–280] | 150 [67–340] | 110 [59–342] | <0.001 |
| D2B time (min) | 65 [44–93] | 70 [49–98] | 62 [40–90] | <0.001 |
| O2B time (min) | 202 [130–360] | 232 [144–424] | 185 [125–320] | <0.001 |
| Killip classification (%) | 0.014 | |||
| I | 74.2 | 72.7 | 74.9 | |
| II–III | 16.1 | 17.2 | 15.5 | |
| IV | 9.7 | 10.1 | 9.6 | |
| Culprit vessel (%) | ||||
| LAD | 47.6 | 46.6 | 48.3 | 0.036 |
| LCX | 8.9 | 8.8 | 9.1 | 0.52 |
| RCA | 41.0 | 41.7 | 40.5 | 0.12 |
| LMT | 1.9 | 1.9 | 1.9 | 0.80 |
Data are given as the mean±SD, median [interquartile range], or %. D2B time, door-to-balloon time; LAD, left anterior descending artery; LCX, left circumflex artery; LMT, left main trunk; O2B time, symptom onset-to-balloon time; O2D time, symptom onset-to-door time; RCA, right coronary artery.
The overall median D2B time was longer (70 vs. 62 min; P<0.001) and the rate of achieving a D2B time ≤90 min was lower (70.7% vs. 75.4%; P<0.001) in the rural than urban group (Figure 2). In particular, notable regional differences were found between rural and urban areas in the percentage of patients with a D2B time ≤30 min (5.1% vs. 15.1%, respectively; P<0.001). Furthermore, O2D time was prolonged in the rural compared with urban group ( 150 vs. 110 min, respectively; P<0.001), contributing to the further expansion of a regional difference in total ischemic time in the rural group (232 vs. 185 min; P<0.001).
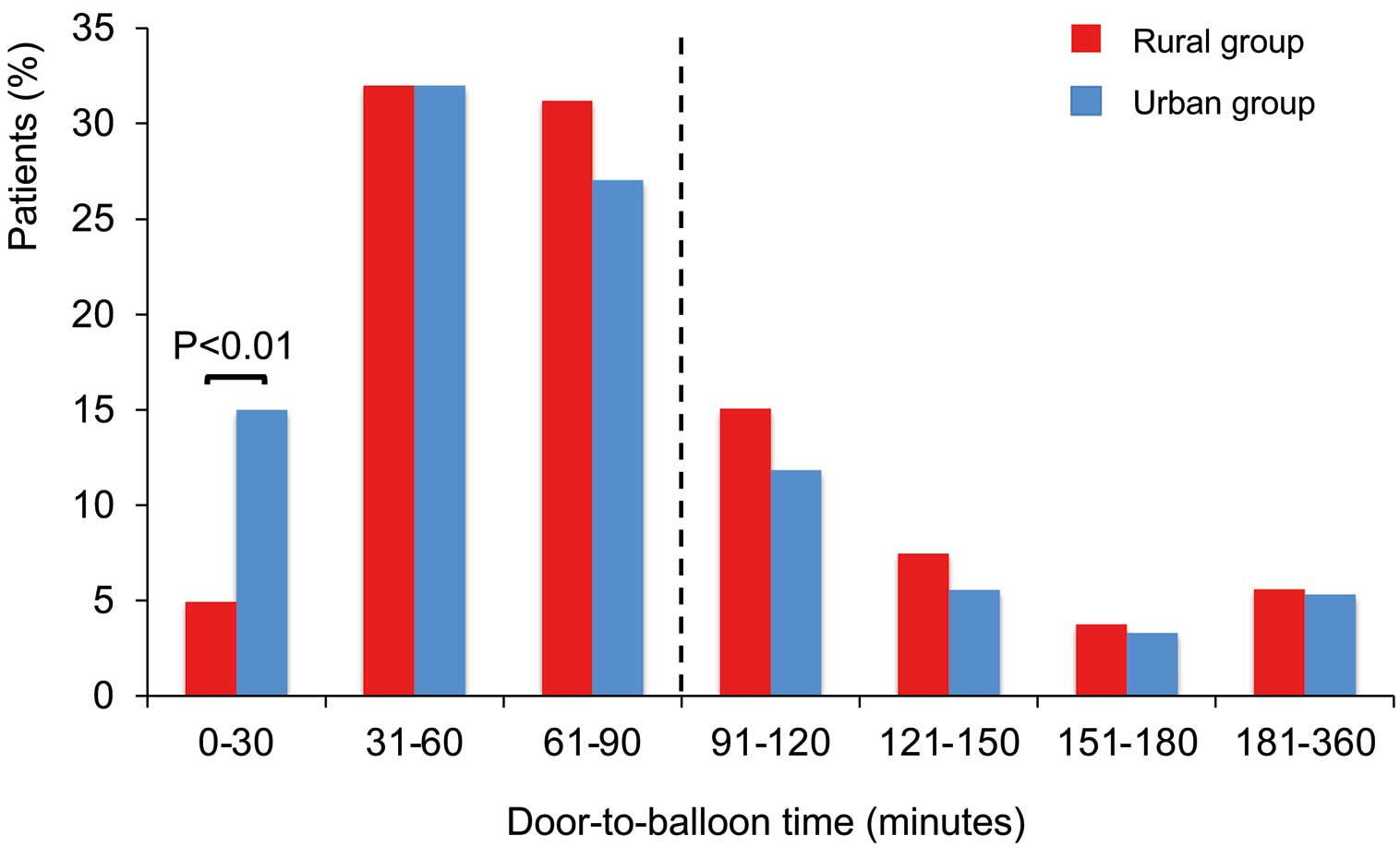
Distribution of door-to-balloon (D2B) time based on residential area. There was a significant difference between the rural and urban groups in the proportion of patients with a D2B time ≤30 min (P<0.01, Chi-squared test).
To explore factors associated with D2B time >90 min, univariable and multivariable logistic regression analyses were performed by residential area; results are presented in Table 2. In both rural and urban areas, ambulance transport was related to achieving a D2B time ≤90 min, whereas higher Killip classes were associated with a D2B time >90 min.
| Rural group | Urban group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariable analysis | Multivariable analysis | Univariable analysis | Multivariable analysis | |||||||||
| OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | |
| Age, per 10-year increase | 1.09 | 1.05–1.13 | <0.001 | 1.08 | 1.03–1.14 | 0.003 | 1.09 | 1.06–1.13 | <0.001 | |||
| Male sex | 0.82 | 0.73–0.93 | 0.002 | 0.84 | 0.76–0.93 | 0.001 | ||||||
| Smoking | 0.94 | 0.84–1.04 | 0.24 | 0.84 | 0.77–0.92 | <0.001 | 0.82 | 0.69–0.96 | 0.017 | |||
| Hypertension | 0.98 | 0.88–1.10 | 0.75 | 1.27 | 1.11–1.45 | <0.001 | ||||||
| Dyslipidemia | 0.89 | 0.80–0.99 | 0.025 | 0.98 | 0.87–1.12 | 0.79 | ||||||
| Diabetes | 1.05 | 0.94–1.17 | 0.39 | 1.23 | 1.08–1.41 | 0.002 | 1.21 | 1.20–1.43 | 0.033 | |||
| Anterior infarction | 0.92 | 0.83–1.02 | 0.11 | 1.19 | 1.08–1.31 | 0.001 | ||||||
| Killip classification | ||||||||||||
| I | – | – | Ref. | – | – | Ref. | – | – | Ref. | – | – | Ref. |
| II–III | 1.23 | 1.05–1.44 | 0.012 | 1.21 | 1.01–1.45 | 0.035 | 1.45 | 1.28–1.64 | <0.001 | 1.50 | 1.21–1.87 | <0.001 |
| IV | 1.61 | 1.32–1.95 | <0.001 | 1.63 | 1.31–2.03 | <0.001 | 1.99 | 1.72–2.29 | <0.001 | 2.05 | 1.55–2.72 | <0.001 |
| Ambulance transport | 0.68 | 0.58–0.81 | <0.001 | 0.70 | 0.58–0.85 | <0.001 | 0.47 | 0.41–0.53 | <0.001 | 0.44 | 0.36–0.54 | <0.001 |
| O2D time >120 min | 0.87 | 0.78–0.98 | 0.017 | 0.86 | 0.75–0.98 | 0.024 | 0.94 | 0.86–1.04 | 0.24 | 0.77 | 0.65–0.91 | 0.002 |
CI, confidence interval; O2D time, symptom onset-to-door time; OR, odds ratio.
In-hospital mortality tended to be higher in the rural than urban group (6.2% vs. 5.5%; P=0.05; Figure 3A). Patients with a D2B time ≤90 min had lower in-hospital mortality than those with a D2B time >90 min in both the rural and urban groups (Figure 3B). Table 3 presents the results of univariable and multivariable logistic regression analyses for factors associated with in-hospital mortality by residential area. In the multivariable analysis, age, anterior infarction, and higher Killip classes at presentation were common predictors for in-hospital death in both the urban and rural groups, whereas D2B time >90 min was independently correlated with in-hospital mortality only in the rural group (adjusted odds ratio 1.57; 95% confidence interval 1.18–2.09; P=0.002), and not in the urban group.
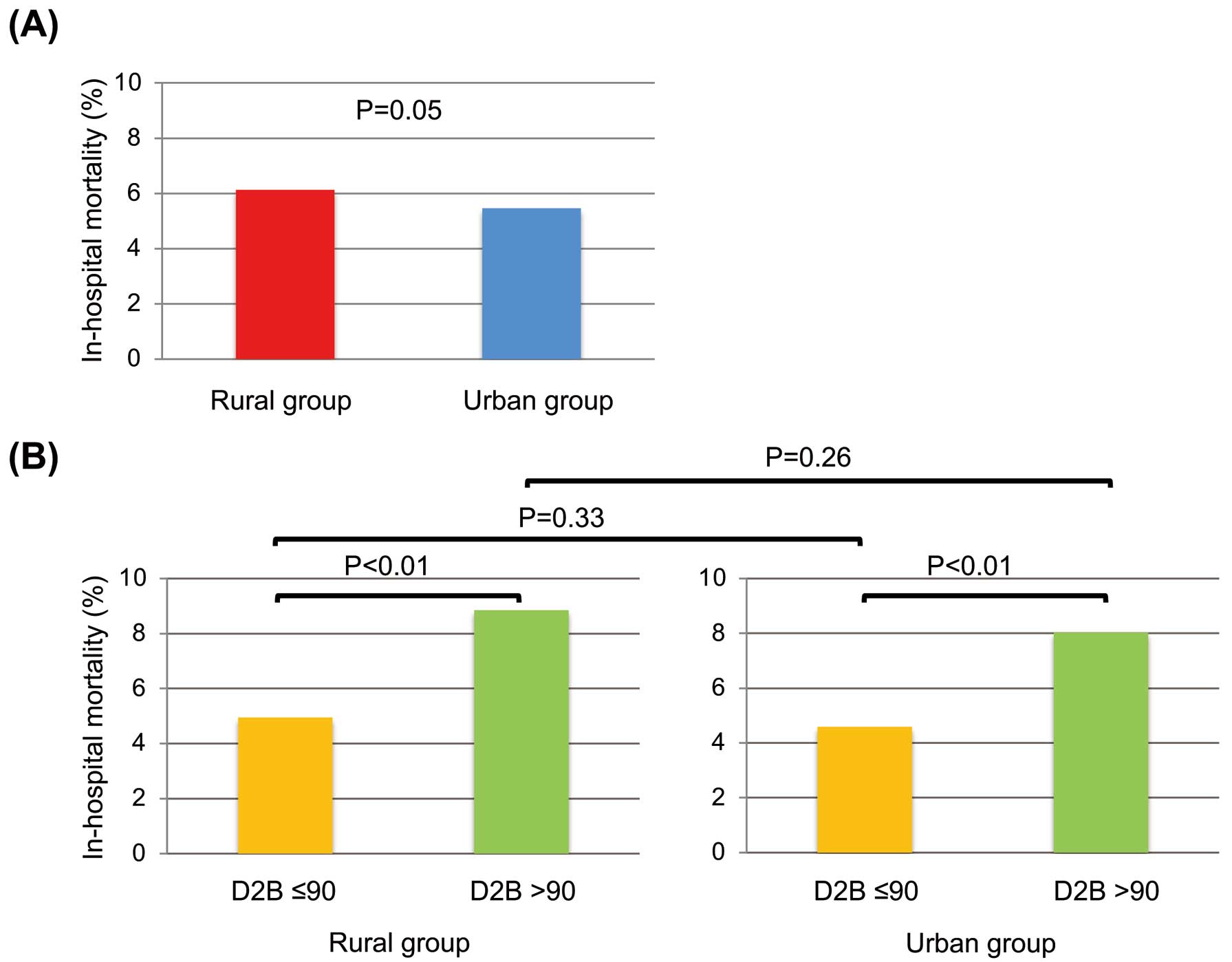
Comparison of in-hospital mortality (A) between the rural and the urban groups and (B) between patients with a door-to-balloon (D2B) time ≤90 and >90 min in the rural and urban groups.
| Rural group | Urban group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariable analysis | Multivariable analysis | Univariable analysis | Multivariable analysis | |||||||||
| OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | |
| Age, per 10-year increase | 1.58 | 1.45–1.72 | <0.001 | 1.49 | 1.32–1.69 | <0.001 | 1.60 | 1.49–1.72 | <0.001 | 1.35 | 1.17–1.54 | <0.001 |
| Male sex | 0.57 | 0.46–0.70 | <0.001 | 0.72 | 0.60–0.87 | 0.001 | ||||||
| Smoking | 0.54 | 0.43–0.68 | <0.001 | 0.55 | 0.46–0.67 | <0.001 | ||||||
| Hypertension | 0.74 | 0.61–0.91 | 0.004 | 0.72 | 0.54–0.98 | 0.037 | 0.99 | 0.78–1.27 | 0.96 | |||
| Dyslipidemia | 0.43 | 0.35–0.52 | <0.001 | 0.56 | 0.42–0.76 | <0.001 | 0.46 | 0.35–0.60 | <0.001 | 0.58 | 0.41–0.82 | 0.002 |
| Diabetes | 1.26 | 1.03–1.55 | 0.024 | 1.07 | 0.83–1.38 | 0.62 | ||||||
| Anterior infarction | 1.92 | 1.56–2.35 | <0.001 | 2.03 | 1.51–2.72 | <0.001 | 2.45 | 1.97–3.03 | <0.001 | 2.56 | 1.76–3.71 | <0.001 |
| Killip classification | ||||||||||||
| I | – | – | Ref. | – | – | Ref. | – | – | Ref. | – | – | Ref. |
| II–III | 4.61 | 3.31–6.41 | <0.001 | 3.31 | 2.27–4.81 | <0.001 | 4.87 | 3.78–6.27 | <0.001 | 4.12 | 2.69–6.32 | <0.001 |
| IV | 29.0 | 21.6–38.8 | <0.001 | 24.2 | 17.4–33.7 | <0.001 | 23.7 | 19.0–29.6 | <0.001 | 28.9 | 19.6–42.5 | <0.001 |
| Ambulance transport | 1.91 | 1.26–2.88 | 0.002 | 1.74 | 1.26–2.40 | 0.001 | ||||||
| O2D time >120 min | 0.86 | 0.70–1.06 | 0.16 | 0.83 | 0.69–0.99 | 0.042 | ||||||
| D2B time >90 min | 1.94 | 1.59–2.36 | <0.001 | 1.57 | 1.18–2.09 | 0.002 | 1.87 | 1.57–2.23 | <0.001 | |||
Abbreviations as in Tables 1,2.
To investigate the potential cause of regional disparities in the prognostic impact of D2B time, we performed a subgroup analysis based on the severity of STEMI, represented by Killip classification on admission; higher Killip classes were found to be associated with both a prolongation of D2B time and increased in-hospital mortality (Table 2; Table 3). As shown in Figure 4A, in-hospital mortality was higher in rural than urban group only among patients with Killip Class IV (38.0% vs. 29.5%, respectively; P<0.001). Furthermore, among patients with Killip Class IV, a regional difference in in-hospital mortality was found only for patients with a D2B time >90 min (47.2% vs. 33.3% for rural vs. urban, respectively; P=0.002), and not for those with a D2B time ≤90 min (31.9% vs. 27.3% for rural vs. urban, respectively; P=0.16; Figure 4B). Indeed, as shown in Figure 5, among patients in the rural group with Killip Class IV, in-hospital mortality kept increasing significantly with a prolongation of D2B time, whereas patients with Killip Classes I–III, regardless of residential area, and those with Killip Class IV in the urban group had a modest upward trend in in-hospital mortality with increasing D2B time. Consequently, a marked rural-urban difference in in-hospital mortality emerged in patients with Killip Class IV with prolonged D2B time >90 min (Figure 5).
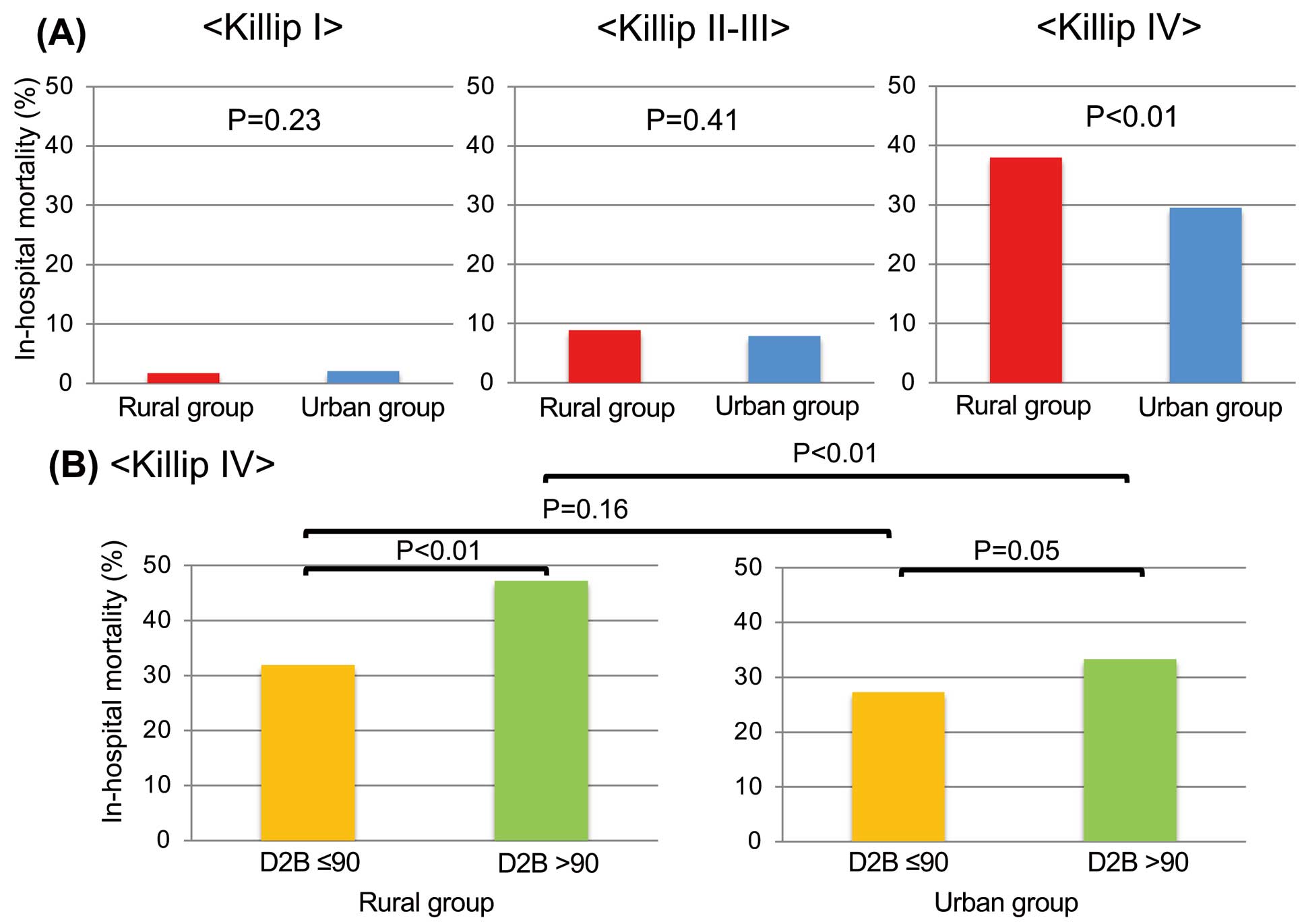
(A) Comparison of in-hospital mortality between the rural and urban areas for each Killip class. (B) Comparison of in-hospital mortality between Killip IV patients with door-to-balloon (D2B) time ≤90 min and >90 min in the rural and urban groups.

Trend of in-hospital mortality according to door-to-balloon (D2B) times for each Killip class in the rural and urban groups. *P values determined using the Cochran-Armitage test. ¶P<0.05 compared with the urban group (Chi-squared test).
In addition, a longer O2D time was consistently observed in the rural vs. urban group regardless of Killip class at presentation (Killip I, 145 vs. 117 min, respectively [P<0.01]; Killip II–III, 151 vs. 121 min, respectively [P<0.01]; Killip IV, 90 vs. 68 min, respectively [P<0.01]). Also of note is the fact that the rate of achieving an O2D time ≤120 min was especially pronounced among Killip Class IV patients in the urban group compared with their rural counterparts (69.6% vs. 58.2%, respectively; P<0.001; Supplementary Figure 2).
The major findings of the present study are that: (1) D2B time was more prolonged and in-hospital mortality tended to be higher in rural than urban AMI patients in Japan; (2) patients with a D2B time >90 min had higher crude in-hospital mortality than those with a D2B time ≤90 min, regardless of residential area, whereas D2B time >90 min was associated with in-hospital mortality only in the rural, and not urban, group after adjusting for demographic and clinical comorbidities; and (3) the rural-urban difference in in-hospital mortality was the most pronounced for the subset of patients with CS and a prolonged D2B time >90 min.
Regional Differences in D2B Time and In-Hospital Mortality in JapanIt is well known that rural residents are disadvantaged when it comes to cardiovascular healthcare, including having poor access to critical care for acute cardiovascular problems.19 Even today, in the US (land area 9,833,517 km2), cardiovascular mortality rates are higher in rural than urban areas.20 Patients with AMI are less likely to undergo cardiac catheterization and PPCI at rural compared with urban hospitals.20,21 Despite Japan being a relatively small island country (land area 377,971 km2), a number of hospitals provide PPCIs for AMI patients under a universal health insurance system. According to a report from the National Cardiovascular Data Registry’s CathPCI Registry in the US, in 2011 the median D2B time was 63 min and in-hospital mortality from STEMI was 5.3%.22 In Korea, between 2011 and 2015, the median D2B time was 59 min and 30-day mortality from STEMI was 6.4%.23 In the present study analyzing the nation-wide JAMIR, the D2B time for urban patients was 62 min and in-hospital mortality was 5.5%. These findings, from geographically separate locations and different healthcare systems, indicate that D2B time seems to be a reliable indicator for evaluating systems of care for STEMI patients.
The focus of the present study was on rural-urban disparity in D2B time, which has rarely been investigated. Patients in the rural group had a longer D2B time (median 70 min) and a tendency for higher in-hospital mortality (6.2%) than patients in the urban group. We confirmed that crude in-hospital mortality was lower for patients with a D2B time ≤90 min than for those with a D2B time >90 min, regardless of residential area. After adjusting for covariates, delayed D2B time was an independent predictor of in-hospital mortality only in the rural, and not in the urban, group. These findings suggest that improvements in D2B time may bring further benefits to patients in rural areas of Japan, and, by lowering D2B time, they could decrease the total ischemic time. To obtain early recanalization for patients in rural areas, shortening the D2B time may become more important to compensate for the increased transportation time. Indeed, Matsuzawa et al recently demonstrated that rural AMI patients transported directly to high-PPCI-volume hospitals where D2B time is often shortened had a better prognosis regardless of distance.10 Considering the continuous association between shorter D2B time and reduced risk of mortality,23 regional differences in the proportion of patients with a D2B time ≤30 min may be largely associated with the prognostic difference between rural and urban areas.
Rural-Urban Disparity of Mortality in Patients With CSThe rural-urban disparity in the relationship between D2B time and in-hospital mortality in accordance with disease severity has never been systematically evaluated. The Killip classification for the severity of heart failure and/or CS has proven useful for the early risk stratification of AMI patients.24 In the present study, higher Killip classes were significantly correlated not only with the prolongation of D2B time, but also with increased in-hospital mortality. Importantly, we revealed that the rural-urban difference in in-hospital mortality was found only in Killip Class IV, taken as synonymous with CS, which is the most severe clinical condition in AMI. CS occurs in 5–13% of patients with STEMI and is associated with significant morbidity and mortality.25,26 Timely reperfusion via PPCI is essential to improve survival in patients with STEMI-associated CS.27–30 We demonstrated that shorter D2B time had survival benefits for CS patients in both the rural and urban groups. Further, rural CS patients with delayed D2B time had higher in-hospital mortality than their urban counterparts, whereas among those with shorter D2B time, there was no significant difference in in-hospital mortality between the rural and urban groups. Thus, it is conceivable that CS patients with a prolonged D2B time contribute to the rural-urban disparity in short-term clinical outcomes. Among patients with CS complicating AMI, the rural-urban difference in in-hospital mortality increased with increasing D2B time, and became significant at a D2B time >90 min. In short, achieving a D2B time ≤90 min for rural CS patients may be of crucial importance for reducing the regional gap in outcomes. Five strategies have been proposed to achieve this:31 (1) the emergency medicine physician activating the cath lab; (2) one call activating the cath lab; (3) the cath lab team being ready within 30 min; (4) prompt data feedback to team members; and (5) an optional prehospital electrocardiogram (ECG) activating the cath lab. Achieving such a very short D2B time may require the prehospital diagnosis of AMI with mobile ECG or telemedicine systems provided by paramedics.32–35 The significance of prehospital diagnosis is corroborated by the multivariable analysis findings in the present study that ambulance transport is an independent predictor for shorter D2B time. Importantly, it has been reported that patients treated with a mobile telemedicine system that continuously transmits real-time 12-lead ECG from ambulances in a prehospital setting had decreased reperfusion delays, including symptom onset, first medical contact, and D2B intervals in Japan.35
Study LimitationsThis study has several limitations. First, this was a non-randomized retrospective observational study, and thus residual confounding or selection bias could not be completely excluded as an alternative explanation of the findings. In addition, this study could only identify associations, rather than causality. Second, there was insufficient data about medical therapies, such as antithrombogenic agents, including P2Y12 inhibitors, detailed PPCI procedures, and the rates and types of mechanical circulatory support devices used, for analysis. In addition, we had no detailed information regarding baseline clinical characteristics, such as body mass index, baseline hemoglobin, baseline serum creatinine, and atrial fibrillation. Third, this study included only patients with an O2B time within 24 h, which may result in some selection biases. Fourth, we did not have any data on the long-term prognosis of subjects after discharge. Fifth, because we did not have any data regarding patients’ addresses and the hospital where patients were transported, it was difficult to discuss traffic networks, the distance from the onset site to PPCI-capable hospitals, and the PPCI volume and size of the hospitals. Moreover, actual data regarding the number of PPCI operators in each institution, which may be inversely associated with both in-hospital mortality and D2B time of AMI patients,11 was lacking. Hence, further studies with more detailed data and post-discharge prognosis are needed to gain a deeper understanding of the relationship between regional differences in D2B time and the short-term prognosis of STEMI patients.
The present nationwide real-world registry study of JAMIR demonstrates that D2B time was associated with in-hospital mortality only in the rural, and not urban, area. The prognostic rural-urban difference, which is pronounced in STEMI patients with CS and prolonged D2B time, is a major problem to be resolved.
The authors would like to thank all the investigators, clinical research coordinators, and data managers involved in the JAMIR study for their contributions. The JAMIR consisted of the following existing regional registries and members: Sapporo ACS Network: Takashi Takenaka (Hokkaido Medical Center), Daisuke Hotta (Hokkaido Cardiovascular Hospital); Iwate ACS Registry: Tomonori Itoh (Iwate Medical University School of Medicine); Yamagata AMI Registry: Tetsu Watanabe (Yamagata University School of Medicine); Miyagi AMI Registry Study: Hiroaki Shimokawa (Tohoku University); Jichi Medical University: Kazuomi Kario; Tokyo CCU Network: Takeshi Yamamoto (Nippon Medical School Hospital); Atsuo Namiki (Kanto Rosai Hospital); Hiroshi Suzuki (Showa University Fujigaoka Hospital); Yokohama Cardiovascular Workshop: Masami Kosuge (Yokohama City University Medical Center); Mie ACS Registry: Takashi Tanigawa (Matsusaka Chuo Hospital); NCVC AMI Registry: Yasuhide Asaumi (National Cerebral and Cardiovascualr Center); Kumamoto Acute Coronary Events Study: Kenichi Tsujita (Kumamoto University); JAMIR data center: Yoshihiro Miyamaoto (National Cerebral and Cardiovascualr Center).
This study was supported, in part, by a Grant-in-Aid Scientific Research (17K09452) from the Ministry of Education, Science, and Culture, Japan. There are no other financial relationships.
S.Y., Y.S., K.K. are members of Circulation Journal’s Editorial Team. The remaining authors have no conflicts of interest to disclose.
The present study was approved by the Ethics Committee Tohoku University Graduate School of Medicine (Reference no. 2019-1-809).
Please find supplementary file(s);
https://doi.org/10.1253/circj.CJ-22-0454