Abstract
Background: It has been reported that patients with acute myocardial infarction (AMI) transferred to low-volume primary percutaneous coronary intervention (PCI) hospitals (<115/year) in low population density areas experience higher in-hospital mortality rates. This study compared in-hospital outcomes of patients admitted to high-volume primary PCI hospitals (≥115/year) with those for other regional general hospitals.
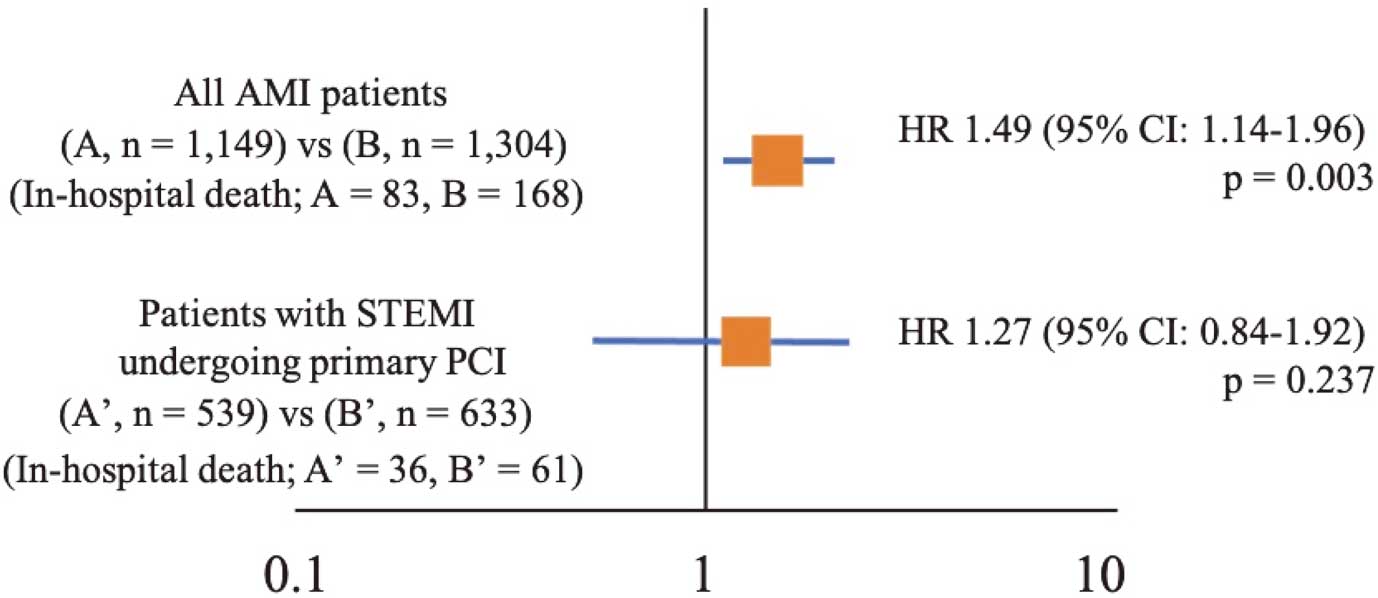
Methods and Results: Retrospective analysis was conducted on data obtained from 2,453 patients with AMI admitted to hospitals in Iwate Prefecture (2014–2018). Multivariate analysis revealed that the in-hospital mortality rate of AMI among patients in regional general hospitals was significantly higher than among patients in high-volume hospitals. However, no significant difference in mortality rate was observed among patients with ST-elevation myocardial infarction (STEMI) undergoing primary PCI. Although no significant difference was found in the in-hospital mortality rate of patients with Killip class I STEMI, significantly lower in-hospital mortality rates were observed in patients admitted in high-volume hospitals for Killip classes II, III, and IV.
Conclusions: Although in-hospital outcomes for patients with STEMI undergoing primary PCI were similar, patients with heart failure or cardiogenic shock exhibited better in-hospital outcomes in high-volume primary PCI hospitals than those in regional general hospitals.
Despite the establishment of guidelines for primary percutaneous coronary intervention (PCI) in acute myocardial infarction (AMI), clinical outcomes in rural hospitals appear to lag behind those in urban centers. A recent study indicated that the in-hospital mortality rate among patients with AMI was higher in less populated areas of Japan, a trend most noticeable in hospitals conducting fewer annual primary PCI procedures.1 According to Matsuzawa and colleagues, patients with AMI should be triaged at onset and directly transported to hospitals conducting more annual primary PCI procedures (PCI high-volume centers). Additionally, it is important to note that the disparity in clinical outcomes for patients with heart failure (HF) and AMI significantly varies between rural and urban hospitals. Comprehensive efforts in primary PCI, clinical, and public health fields must address these disparities.2
Iwate Prefecture, one of Japan’s least populated areas with a density of 84.1 persons/km2
(average nationwide density: 338 persons/km2), spans 15,280 km2. Figure 1 illustrates the 9 medical areas (Morioka, Iwate-Chubu, Isawa, Ryoban, Kesen, Kamaishi, Miyako, Kuji, and Ninohe) in Iwate Prefecture from 2014 to 2018, each served by a regional core hospital providing acute cardiac care. Of them, only 2 hospitals in the Morioka area qualify as “high-volume primary PCI hospitals,” as defined by Matsuzawa et al’s study (Iwate Medical University moved from Morioka to Yahaba-cho, Shiwa-gun in 2019).1

High-volume centers with trained staff conducting PCI can reduce the door-to-balloon time, improving prognosis.3 However, directing all patients with AMI to these 2 hospitals within an expansive area such as Iwate Prefecture is impractical. Similar to other rural areas, patients with AMI in Iwate Prefecture are initially transported to a regional core hospital for treatment. However, due to resource constraints in rural hospitals, some patients have to be transferred to high-volume hospitals located up to 100 km from the regional hospital. The long transportation time potentially delays revascularization, affecting primary PCI outcomes in patients with ST-elevation myocardial infarction (STEMI).4 Despite this, no study has compared the outcomes of rural patients with AMI receiving care at regional general hospitals that are not high-volume with those of patients transported to distant high-volume hospitals. Therefore, this study aimed to compare the short-term outcomes of patients with AMI treated at high-volume primary PCI hospitals with those treated at regional general hospitals.
Methods
Research Participants
A multicenter study, known as the “Iwate Heart Disease Registry Project”,5 was conducted across 11 primary general hospitals within Iwate Prefecture (forming the Iwate acute coronary syndrome [ACS] registry). The Iwate ACS registry collects and records data on patients with AMI admitted to 11 core hospitals spanning the 9 medical regions within Iwate Prefecture. These data enable analysis of the background, clinical course, treatment, and in-hospital prognosis of patients with ACS within the prefecture. As almost all emergency patients in Iwate Prefecture receive treatment at these 11 hospitals, the data should provide a comprehensive view of trends of patients with AMI across the entire prefecture. Our analysis included data from 2,453 patients enrolled from October 1, 2014, to December 31, 2018.
This study was performed in compliance with the Declaration of Helsinki (Brazilian revision, 2013) and received approval from the ethics committee of each participating medical center (MH2021-116). Because it was a retrospective observational study, patient informed consent was waived. However, an opt-out opportunity was made available on the Iwate Medical University website as an alternative measure (https://iwate-heart.jp/public_information/). This study was also registered with the University Hospital Medical Information Clinical Trials Registry, which meets the criteria of the International Committee of Medical Journal Editors (UMIN000046643).
Definition of High-Volume Primary PCI Hospitals and Classification of Target Patients
We used a registration list of anonymized patients to gather clinical data on patients with type 1 AMI aligning with the Third Universal Definition,6 which encompassed data such as age, sex, drugs, device usage, length of hospital stay, and discharge status. This definition includes some cases of MI without coronary occlusion. We excluded cases of patients not resuscitated outside a hospital cardiopulmonary arrest or being diagnosed with Takotsubo cardiomyopathy after admission. High-volume primary PCI hospitals were defined as those conducting >115 primary PCI procedures per year, as per the definition used in a previous study.1
We divided patients with AMI into 2 groups: Group A comprised patients admitted to high-volume hospitals and Group B comprised patients admitted to regional general hospitals. We further divided patients admitted to high-volume hospitals into 2 subgroups: Group A1 comprised those who were directly admitted to PCI high-volume centers within their medical area, and Group A2 comprised those admitted to high-volume hospitals after long-distance transportation from outside their medical area. A separate analysis included only patients with STEMI, excluding those with non-STEMI (NSTEMI) and those who did not undergo primary PCI. According to the hospital, as described above, patients with STEMI undergoing primary PCI were classified into 3 groups: Group A1’, Group A2’, and Group B’.
Statistical Analysis
The primary endpoint was in-hospital death or survival to discharge. We represented descriptive statistics as mean±standard deviation or median (25–75%) for continuous variables and percentages for categorical variables, as applicable. Chi-square and Mann-Whitney U-tests were used to compare 2 groups, and the Kruskal-Wallis test was used to compare 3 groups. The Kaplan-Meier method was used to calculate the cumulative event rate, and a Cox proportional hazards model calculated the risk ratio of event occurrence. For the multivariate analysis, we selected age, sex, and chronic kidney disease as independent variables, considering their significant variance between the 2 groups. We conducted statistical analyses using SPSS ver. 25.0 for Mac (IBM, Chicago, USA). A P value <0.05 was considered significant for all analyses.
Results
Patients With AMI
Table 1A and Table 2A present the characteristics, treatment details, and outcomes of all patients with AMI, and significant differences between the groups are outlined in Supplementary Tables 1,2. Patients at regional general hospitals were significantly older than those at high primary PCI volume hospitals (70.6±13.7 years vs. 68.4±13.0 years, P<0.001). There were more males in high-volume hospitals than in regional general hospitals (77.4% vs. 73.6%, P=0.029). A larger proportion of patients at regional general hospitals had chronic kidney disease than those at high-volume hospitals (42.1% vs. 35.4%, P<0.001).
Table 1. Clinical Characteristics of Patients With AMI or STEMI According to Hospital Type
| (A) Patients with AMI |
Total patients (n=2,453) |
P value |
| |
(A) High-volume primary PCI hospitals
(2 hospitals, n=1,149) |
(B) Regional
general hospitals
(9 hospitals,
n=1,304) |
(A) vs. (B) |
| |
(A1) Inside the
medical area
(n=840) |
(A2) Outside the
medical area
(n=309) |
| Age, years |
69.5±13.4 |
68.4±13.0 |
68.1±13.2 |
69.0±12.3 |
70.6±13.7 |
<0.001 |
| Sex, male |
75.3% |
77.4% |
76.9% |
78.6% |
73.6% |
0.017 |
| BMI (kg/m2) |
24.1±3.9 |
24.2±3.9 |
24.3±4.0 |
24.1±3.6 |
24.0±3.8 |
0.126 |
| Obesity (BMI ≥25.0) |
37.1% |
37.2% |
37.1% |
37.6% |
37.1% |
0.955 |
| Diabetes mellitus |
34.5% |
35.7% |
35.0% |
37.5% |
33.4% |
0.236 |
| Hypertension |
69.6% |
70.5% |
69.7% |
72.5% |
68.9% |
0.409 |
| Dyslipidemia |
53.0% |
50.9% |
48.5% |
57.5% |
54.9% |
0.055 |
| Current smoking |
33.7% |
31.0% |
30.8% |
31.4% |
36.1% |
<0.001 |
| Myocardial infarction |
9.6% |
10.1% |
9.8% |
10.8% |
9.2% |
0.483 |
| Cerebral infarction |
9.8% |
9.2% |
9.7% |
7.7% |
10.3% |
0.356 |
| Chronic heart failure |
3.7% |
3.4% |
3.8% |
2.3% |
4.0% |
0.383 |
| eGFR (mL/min/1.73 m2) |
63.5±22.0 |
65.0±22.7 |
65.1±21.8 |
65.0±21.2 |
62.1±21.2 |
<0.001 |
| Chronic kidney disease* |
38.9% |
35.4% |
35.0% |
36.2% |
42.1% |
<0.001 |
| HbA1c (%) |
6.2±1.5 |
6.3±1.4 |
6.4±1.4 |
6.2±1.3 |
6.1±1.6 |
0.635 |
| TG (mg/dL) |
126.6±90.3 |
123.1±85.2 |
128.2±90.0 |
110.1±70.0 |
129.8±94.7 |
0.212 |
| TC (mg/dL) |
185.0±46.0 |
184.4±45.6 |
184.8±47.1 |
183.3±41.4 |
185.7±46.5 |
0.535 |
| LDL-C (mg/dL) |
114.1±38.1 |
112.5±36.5 |
112.8±37.5 |
111.8±33.8 |
115.6±39.6 |
0.147 |
| HDL-C (mg/dL) |
49.3±16.1 |
47.5±15.1 |
47.9±15.1 |
47.1±15.2 |
50.7±16.7 |
<0.001 |
| STEMI |
65.9% |
61.1% |
60.4% |
63.1% |
70.2% |
<0.001 |
| Killip class I/II/III/IV (%) |
72.6/13.8/6.0/7.6 |
74.3/11.6/6.1/7.9 |
75.2/11.6/5.9/7.3 |
71.9/11.6/6.8/9.6 |
71.2/15.6/5.8/7.4 |
0.179 |
| LVEF (%) |
50.2±13.9 |
51.7±12.2 |
51.6±12.1 |
52.0±12.6 |
48.7±15.3 |
<0.001 |
(B) Patients with
STEMI undergoing
primary PCI |
Total patients (n=1,269) |
P value |
| |
(A’) High-volume primary PCI hospitals
(2 hospitals, n=575) |
(B’) Regional
general hospitals
(9 hospitals,
n=694) |
(A’) vs. (B’) |
| |
(A1’) Inside the
medical area
(n=417) |
(A2’) Outside the
medical area
(n=158) |
| Age, years |
67.6±13.1 |
67.2±13.1 |
66.9±13.3 |
67.8±12.8 |
68.0±13.0 |
0.043 |
| Sex, male |
79.7% |
78.8% |
77.0% |
83.5% |
80.5% |
0.239 |
| BMI (kg/m2) |
24.2±3.7 |
24.4±3.8 |
24.4±4.1 |
24.4±3.2 |
24.0±3.6 |
0.200 |
| Obesity (BMI ≥25.0) |
37.9% |
38.4% |
38.4% |
38.2% |
37.5% |
0.743 |
| Diabetes mellitus |
32.6% |
32.1% |
33.0% |
29.7% |
33.0% |
0.722 |
| Hypertension |
66.6% |
66.7% |
66.3% |
67.9% |
66.5% |
0.939 |
| Dyslipidemia |
53.7% |
49.6% |
47.2% |
56.1% |
57.1% |
<0.001 |
| Current smoking |
30.3% |
29.9% |
29.7% |
30.4% |
37.9% |
0.376 |
| Myocardial infarction |
7.4% |
7.0% |
7.5% |
5.7% |
7.7% |
0.645 |
| Cerebral infarction |
7.7% |
7.8% |
8.1% |
7.1% |
7.6% |
0.872 |
| Chronic heart failure |
1.5% |
0.9% |
1.2% |
0.6% |
2.0% |
0.093 |
| eGFR (mL/min/1.73 m2) |
67.2±20.0 |
68.1±20.9 |
67.8±20.3 |
69.1±22.5 |
63.6±20.4 |
0.013 |
| Chronic kidney disease* |
32.0% |
29.6% |
29.3% |
30.4% |
34.0% |
0.056 |
| HbA1c (%) |
6.3±1.4 |
6.4±1.5 |
6.4±1.5 |
6.3±1.3 |
6.2±1.4 |
0.216 |
| TG (mg/dL) |
129.6±90.9 |
124.7±84.4 |
128.6±91.1 |
115.0±61.1 |
133.8±96.0 |
0.252 |
| TC (mg/dL) |
188.4±46.1 |
188.1±47.1 |
187.3±49.3 |
190.6±40.7 |
188.8±45.0 |
0.573 |
| LDL-C (mg/dL) |
117.2±37.1 |
116.1±36.7 |
114.4±88.0 |
120.5±32.3 |
118.3±37.5 |
0.363 |
| HDL-C (mg/dL) |
48.9±14.1 |
47.4±15.3 |
47.6±15.2 |
46.9±15.6 |
50.2±12.9 |
<0.001 |
| STEMI |
100.0% |
100.0% |
100.0% |
100.0% |
100.0% |
– |
| Killip class I/II/III/IV (%) |
73.9/14.3/4.3/7.4 |
73.9/13.1/4.5/8.5 |
74.4/13.3/3.8/8.5 |
72.4/12.5/6.6/8.6 |
74.0/15.3/4.1/6.6 |
0.750 |
| LVEF (%) |
49.1±13.1 |
50.7±11.1 |
50.8±11.2 |
50.3±10.9 |
47.4±14.7 |
0.003 |
*eGFR <60 mL/min/1.73 m2. AMI, acute myocardial infarction; BMI, body mass index; eGFR, estimated glomerular filtration rate; HbA1c, hemoglobin A1c; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; STEMI, ST-segment elevation myocardial infarction; TC, total cholesterol; TG, triglyceride.
Table 2. Treatment Details and Outcomes of Patients With AMI or STEMI According to Hospital Type
| (A) Patients with AMI |
Total patients (n=2,453) |
P value |
| |
(A) High-volume primary PCI hospitals
(2 hospitals, n=1,149) |
(B) Regional
general hospitals
(9 hospitals,
n=1,304) |
(A) vs. (B) |
| |
(A1) Inside the
medical area
(n=840) |
(A2) Outside the
medical area
(n=309) |
| Emergency CAG |
80.1% |
85.0% |
85.1% |
84.7% |
75.7% |
<0.001 |
| Emergency PCI |
73.3% |
75.4% |
75.8% |
74.1% |
71.6% |
0.032 |
| CABG |
3.7% |
7.3% |
5.2% |
12.9% |
0% |
– |
| Respirator |
6.8% |
6.2% |
5.8% |
7.1% |
7.3% |
0.282 |
| IABP |
8.5% |
10.0% |
9.3% |
12.0% |
7.1% |
0.010 |
| VA-ECMO |
1.3% |
1.8% |
1.9% |
1.6% |
0.9% |
0.051 |
| Door-to-balloon time (min)* |
90.0 |
85.0 |
97.5 |
65.0 |
94.0 |
<0.001 |
Onset-to-balloon time
(min)* |
175.8 |
195.0 |
160.0 |
270.0 |
162.0 |
<0.001 |
Final TIMI grade
(3/2/1/0) (%) |
93.5/3.5/1.5/1.5 |
94.0/4.0/1.3/0.7 |
94.1/5.9/1.8/0.2 |
93.7/3.7/0.5/2.1 |
93.0/3.3/1.6/2.1 |
0.732 |
| In-hospital mortality rate |
10.2% |
7.2% |
7.7% |
5.8% |
12.9% |
<0.001 |
(B) Patients with
STEMI undergoing
primary PCI |
Total patients (n=1,269) |
P value |
| |
(A’) High-volume primary PCI hospitals
(2 hospitals, n=575) |
(B’) Regional
general hospitals
(9 hospitals,
n=694) |
(A’) vs. (B’) |
| |
(A1’) Inside the
medical area
(n=417) |
(A2’) Outside the
medical area
(n=158) |
| Emergency CAG |
100.0% |
100.0% |
100.0% |
100.0% |
100.0% |
– |
| Emergency PCI |
100.0% |
100.0% |
100.0% |
100.0% |
100.0% |
– |
| CABG |
1.1% |
1.6% |
1.4% |
1.9% |
0% |
– |
| Respirator |
7.0% |
5.6% |
5.3% |
6.3% |
8.2% |
0.066 |
| IABP |
9.9% |
10.3% |
10.3% |
10.1% |
9.7% |
0.719 |
| VA-ECMO |
1.6% |
2.1% |
2.2% |
1.9% |
1.2% |
0.184 |
| Door-to-balloon time (min)* |
85.0 |
77.0 |
86.0 |
63.0 |
87.0 |
<0.001 |
Onset-to-balloon time
(min)* |
154.8 |
168.0 |
145.8 |
255.0 |
145.8 |
<0.001 |
Final TIMI grade
(3/2/1/0) (%) |
94.0/3.6/1.4/1.0 |
94.2/3.8/1.5/0.4 |
94.0/3.9/1.8/0.3 |
94.9/3.6/0.7/0.7 |
93.9/3.4/1.3/1.5 |
0.606 |
| In-hospital mortality rate |
7.6% |
6.3% |
6.5% |
5.7% |
8.8% |
0.056 |
*Median. CABG, coronary artery bypass grafting; CAG, coronary angiography; IABP, intra-aortic balloon pumping; PCI, percutaneous coronary intervention; VA-ECMO, venoarterial extracorporeal membrane oxygenation. Other abbreviations as in Table 1.
High-volume primary PCI hospitals tended to have a significantly lower proportion of patients with STEMI compared with regional general hospitals (61.1% vs. 70.2%; P<0.001), and these were the only 2 high-volume hospitals in Iwate Prefecture providing cardiovascular surgical services. Some patients with NSTEMI were transferred to these hospitals for coronary artery bypass surgery. Higher proportions of emergency coronary angiography (CAG) and PCI procedures were performed in high-volume hospitals (85.0% and 75.4%, respectively) compared with regional general hospitals (75.7% and 71.5%, respectively; P<0.001 and P=0.032, respectively). No significant differences were found between the 2 groups in terms of the distribution of Killip classes I–IV (P=0.179) and final TIMI grade (P=0.732).
Patients were classified into Group A (n=1,149) and Group B (n=1,304), with Group A further divided into Group A1 (n=840) and Group A2 (n=309). Figure 2A and Figure 3A depict this classification and the cumulative in-hospital survival rates, respectively, of the groups comprising patients with AMI. No significant differences were observed in the 30-day in-hospital survival rates between Group A1 and Group A2 (P=0.141). However, Group B exhibited significantly lower survival rates than Groups A1 and A2 (P<0.001 for both groups).
Patients With STEMI
Analysis of only patients with STEMI who underwent primary PCI (excluding nonprimary PCI and NSTEMI patients) were added in Group A1’ (n=417), Group A2’ (n=158), and Group B’ (n=694), as depicted in Figure 2B. Table 1B and Table 2B show the characteristics and outcomes of patients, respectively, and significant group differences are provided in Supplementary Tables 1,2. Figure 3B shows the lack of a significant difference in 30-day in-hospital survival rates among the 3 groups (P=0.208).
Hazard ratios associated with in-hospital deaths after being adjusted for age, sex, and chronic kidney disease are illustrated in Figure 4. For all patients with AMI, the hazard ratio of in-hospital death in Group A was significantly higher than in Group B (1.49; 95% confidence interval: 1.14–1.96, P=0.003). However, among patients with STEMI undergoing primary PCI, no significant differences in the in-hospital mortality rate were found between Group A’ and Group B’, with a hazard ratio of 1.27 (95% confidence interval: 0.84–1.92, P=0.237).
Age Distribution and Number of Emergency CAGs and Primary PCIs
Figure 5 illustrates the rates of CAG performed in high-volume primary PCI and regional general hospitals; the data were categorized by patients’ age. Regional general hospitals had a higher proportion of geriatric patients than high-volume hospitals. Rates of emergency CAG and PCI were 80.7% and 71.3%, respectively, in high-volume hospitals for elderly patients aged ≥75 years, and the respective rates for these patients in regional general hospitals were 64.3% and 61.6%. There were significantly fewer emergency CAG and PCI procedures performed in regional general hospitals than in high-volume hospitals (P<0.001 and P=0.001, respectively).

Figure 6 is an analysis of patients with STEMI who underwent primary PCI, grouped according to their Killip classification. No significant differences were observed in short-term prognoses between high-volume primary PCI hospitals and regional general hospitals for Killip class I patients, comprising the majority of patients with STEMI (P=0.489). However, compared with high-volume hospitals, regional general hospitals demonstrated significantly higher in-hospital mortality rates among patients with STEMI having HF (P=0.027) and cardiogenic shock (P=0.029). Among patients treated within the same medical area (excluding Group A1’), the median door-to-balloon time was 86.0 min and 87.0 min in Groups A2’ and B’, respectively (P=0.376).
Discussion
Our results indicated that short-term prognoses for patients with AMI admitted to regional general hospitals were less favorable than for those admitted to high-volume primary PCI hospitals. This finding is consistent with those of a previous study.1 However, no significant difference in short-term prognosis was observed between patients with STEMI undergoing primary PCI in high-volume hospitals and those undergoing primary PCI in regional general hospitals. However, the in-hospital mortality rate of patients with STEMI Killip classes II, III, and IV was higher in regional general hospitals than in high-volume hospitals.
In this study, the elderly population was predominantly in the rural areas, and rates of emergency CAG and PCI procedures in elderly patients with AMI were notably low. It has been established that early PCI for patients with AMI can improve prognosis,7 so the lack of primary PCI may negatively affect the short-term prognosis of elderly patients with AMI in regional hospitals. Elderly patients with dementia or limited ability with daily living activities are frequently omitted from indications for emergency PCI,8,9 which might explain the lower rates of emergency PCI observed among elderly patients with AMI in rural areas in this study.
Admission to a hospital during the acute phase of STEMI typically warrants primary PCI.10 There were no significant differences in the door-to-balloon time, onset-to-balloon time, final TIMI 3 grade, or in-hospital mortality rate between patients in Groups A1’ and B’ who underwent primary PCI in the same area where the STEMI occurred. These findings could justify the implementation of primary PCI at the presenting hospital, irrespective of whether it is a high-volume or regional general hospital, provided that the hospital is capable of performing primary PCI after the onset of STEMI. Conversely, the low in-hospital mortality rate in Group A2’ suggests that if primary PCI cannot be performed in the regional general hospitals where patients with STEMI are first admitted, it would be beneficial to transfer these patients to high-volume hospitals as soon as possible, regardless of the distance between hospitals, to improve survival rates. This indicates that the transfer of patients, when feasible, can be a lifesaving strategy. However, we acknowledge that selection bias may have influenced these results, considering that physicians may have preferred to transfer patients deemed “stable enough for transfer”. Patients with severe AMI who cannot be treated at regional hospitals in Iwate Prefecture are often transferred by an ambulance or helicopter to high-volume hospitals with intensive care units. However, patients who are deemed incapable of surviving long-distance transport by their physicians succumb to AMI in the presenting hospital. This factor may contribute to the high in-hospital mortality rates observed among AMI patients at the regional general hospitals.
According to a report comparing outcomes of patients with AMI in 4 rural prefectures and Tokyo,11 patients with STEMI in rural areas were less likely to be transported directly to hospitals performing primary PCI compared with patients in Tokyo, potentially leading to delays in primary PCI that may affect prognosis. Another study found no significant difference in the in-hospital mortality rate of patients with STEMI admitted to hospitals with varying annual volumes of primary PCI procedures.12 Importantly, over the years, the disparity in short-term prognoses of patients with STEMI between rural and urban areas has been diminishing and improving, respectively.13
In this cohort, the door-to-balloon time for Group A2 and Group A2’ was extremely short. Patients from outside the medical region who are transferred to a high-volume hospital typically arrive with an established diagnosis of AMI made by the referring physician. Because Iwate Prefecture is vast, it often takes approximately 2 h to transport these patients from outside the medical area, but this extended transit time allows physicians, and staff in the emergency room, angiography room, and intensive care unit to prepare for primary PCI. Thus, the door-to-balloon time is considerably shorter for transferred patients than for those who are directly admitted to high-volume hospitals or hospitals in their medical area.
In a previous study, patients with STEMI who underwent primary PCI after interfacility transfer (e.g., Group A2’ patients) had significantly higher cumulative incidences of death and HF hospitalization in the first 5 years after onset than those who underwent primary PCI after direct hospitalization.14 This suggests that conducting primary PCI in patients with STEMI in nearby hospitals, even if these are located in rural areas with low primary PCI volumes, might yield more favorable short- and long-term outcomes. However, outcomes between regional general and high-volume hospitals do not uniformly favor the former among patients with STEMI. In our study, the in-hospital mortality rate was significantly higher in patients presenting with cardiogenic shock and HF at regional general hospitals than in those in high-volume hospitals. Data from the JROAD-DPC database indicates that patients with AMI admitted to hospitals staffed by ≥9 cardiologists had a significantly lower 30-day mortality rate than those admitted to hospitals staffed by ≤8 cardiologists.15 Moreover, patients with AMI with cardiogenic shock admitted to urban or large hospitals had lower in-hospital mortality rates than those admitted to rural or smaller hospitals. This difference in mortality rates may be attributed to the fact that patients with AMI admitted to urban or large hospitals are more likely to undergo early CAG, PCI, and receive the necessary mechanical circulatory support.16 The treatment of patients with severe STEMI with cardiogenic shock and HF often necessitates ventilators and mechanical circulatory support, which can pose a challenge in understaffed regional general hospitals. Only 2 (i.e., high-volume) hospitals in Iwate Prefecture are equipped with intensive care units and cardiovascular surgery units, which may have conferred an advantage in handling complications developing in cases of moderate or high severity AMI.
Study Limitations
This is the first study to assess the suitability of primary PCI for patients with STEMI in regional general hospitals in rural areas. However, this study has some limitations. First, we were constrained by the data collected during hospitalization, and long-term prognostic data after discharge was unavailable. Therefore, future studies should consider using a prospective design that permits longitudinal follow-up of patients. Second, this study may not have encompassed all relevant cases, such as walk-in patients with HF presenting at facilities lacking cardiologists or cases of sudden death. Nevertheless, such cases are rare, and this study likely reflects the general trend. Third, we did not have information about the experience and skill level of the PCI operators. Although previous studies17–19 have shown a positive correlation between the number of procedures performed by PCI operators and patient outcomes, this relationship was not explored. Lastly, some rural hospitals in Iwate Prefecture faced fluctuating staffing with cardiologists during the study period, limiting the consistent provision of primary PCI. However, this factor is unlikely to adversely affect the comparisons made between patients who received primary PCI at regional general hospitals and those requiring long-distance transfer to high-volume primary PCI hospitals.
Conclusions
Although in-hospital outcomes for patients with STEMI undergoing primary PCI were found to be comparable between high-volume primary PCI hospitals and regional general hospitals, superior in-hospital outcomes were observed for patients with HF or cardiogenic shock at high-volume hospitals.
Acknowledgments
We express our sincere gratitude to Iwate Medical Association, the staff of the 11 hospitals in Iwate Prefecture, and Ms. Kayoko Fujiwara, and Ms. Yumiko Okuyama for their cooperation in data collection throughout this study.
Disclosures
M.I. received lecture fees from Abbott Medical Japan and Terumo Corporation. Other authors declare no conflicts of interest. Y. Morino is a member of Circulation Journal’s Editorial Team.
IRB Information
Medicine Ethics Committee of Iwate Medical University Faculty (MH2021-116)
Supplementary Files
Please find supplementary file(s);
https://doi.org/10.1253/circj.CJ-23-0188
References
- 1.
Matsuzawa Y, Konishi M, Nakai M, Saigusa Y, Taguri M, Gohbara M, et al. In-hospital mortality in acute myocardial infarction according to population density and primary angioplasty procedures volume. Circ J 2020; 84: 1140–1146.
- 2.
Minhas AMK, Sheikh AB, Ijaz SH, Mostafa A, Nazir Salik, Khera R, et al. Rural-urban disparities in heart failure and acute myocardial infarction hospitalizations. Am J Cardiol 2022; 175: 164–169.
- 3.
Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: A quantitative review of 23 randomised trials. Lancet 2003; 361: 13–20.
- 4.
Loccoh EC, Maddox KEJ, Wang Y, Kazi DS, Yeh RW, Wadhera RK. Rural-urban disparities in outcomes of myocardial infarction, heart failure, and stroke in the United States. J Am Coll Cardiol 2022; 79: 267–279.
- 5.
Itoh T, Nakamura A, Nohara M, Onoda T, Satoh K, Nozaki T, et al. Acute coronary syndrome registry in Iwate prefecture: From the Iwate acute coronary syndrome pilot registry to the Iwate prefecture regional heart disease registry. J Coron Artery Dis 2023; 29: 20–25.
- 6.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol 2012; 60: 1581–1598.
- 7.
Thiemann DR, Coresh J, Oetgen WJ, Powe NR. The association between hospital volume and survival after acute myocardial infarction in elderly patients. N Engl J Med 1999; 340: 1640–1648.
- 8.
Tehrani DM, Darki L, Erande A, Malik S. In-hospital mortality and coronary procedure use for individuals with dementia with acute myocardial infarction in the United States. J Am Geriatr Soc 2013; 61: 1932–1936.
- 9.
Toshima T, Watanabe T, Goto J, Kobayashi Y, Otaki Y, Wanezaki M, et al. Impact of activities of daily living on percutaneous coronary intervention and acute and long-term mortality in patients with acute myocardial infarction: Yamagata AMI registry. J Cardiol 2022; 80: 313–318.
- 10.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018; 39: 119–177.
- 11.
Matsuda J, Kishi M, Kumagai N, Yamazaki T, Sakata K, Higuma T, et al. Rural-urban disparity in emergency care for acute myocardial infarction in Japan. Circ J 2018; 82: 1666–1674.
- 12.
Kumbhani DJ, Cannon CP, Fonarow GC, Liang L, Askari AT, Peacock WF, et al. Association of hospital primary angioplasty volume in ST-segment elevation myocardial infarction with quality and outcomes. JAMA 2009; 302: 2207–2213.
- 13.
Bashar H, Matetić A, Curzen N, Mamas MA. Invasive management and in-hospital outcomes of myocardial infarction patients in rural versus urban hospitals in the United States. Cardiovasc Revasc Med 2022; S1553–S8389: 00727–00728.
- 14.
Nakatsuma K, Siomi H, Morimoto M, Furukawa Y, Nakagawa Y, Ando K, et al. Inter-facility transfer vs. direct admission of patients with ST-segment elevation acute myocardial infarction undergoing primary percutaneous coronary intervention. Circ J 2016; 80: 1764–1772.
- 15.
Matoba T, Sakamoto K, Nakai M, Ichimura K, Mohri M, Tsujita Y, et al. Institutional characteristics and prognosis of acute myocardial infarction with cardiogenic shock in Japan: Analysis from the JROAD/JROAD-DPC Database. Circ J 2021; 85: 1797–1805.
- 16.
Vallabhajosyula S, Dunlay SM, Barsness GW, Rihal CS, Holmes DR Jr, Prasad A. Hospital-level disparities in the outcomes of acute myocardial infarction with cardiogenic shock. Am J Cardiol 2019; 124: 491–498.
- 17.
Srinivas VS, Hailpern SM, Koss E, Monrad ES, Alderman MH. Effect of physician volume on the relationship between hospital volume and mortality during primary angioplasty. J Am Coll Cardiol 2009; 53: 574–579.
- 18.
Vakili BA, Kaplan R, Brown DL. Volume-outcome relation for physicians and hospitals performing angioplasty for acute myocardial infarction in New York state. Circulation 2001; 104: 2171–2176.
- 19.
Kansagra SM, Curtis LH, Anstrom KJ, Schulman KA. Trends in operator and hospital procedure volume and outcomes for percutaneous transluminal coronary angioplasty, 1996 to 2001. Am J Cardiol 2007; 99: 339–343.