II. Evaluation and Treatment of Coronary Risk Factors
1. Comprehensive Risk Assessment and Risk Prediction Models
1.1 Comprehensive Risk Assessment
Comprehensive risk assessment is essential when considering any intervention on the risk factors of coronary artery disease (CAD), such as hypertension, diabetes, dyslipidemia, smoking, obesity, and chronic kidney disease (CKD). Here we define the comprehensive risk assessment as an: “Estimation of the probability (risk) of the incidence of or death from CAD using statistical models (risk prediction models), sharing decisions on treatment policies, establishing personalized treatment goals, providing complete treatment interventions, and continuing treatment intervention with regular follow-ups”.
The importance of comprehensive management of risk factors has been described in multiple international guidelines and consensus documents;18–20 the updated clinical practice guidelines for prevention in Europe and the USA recommend the upfront use of risk prediction models.21,22 Comprehensive risk assessment is also encouraged in this clinical practice guideline (Table 4).
Table 4.
Recommendation and Level of Evidence for Comprehensive Risk Assessment in the Primary Prevention of Cardiovascular Disease
| |
COR |
LOE |
Comprehensive risk assessment should be facilitated for the primary prevention of
cardiovascular disease |
I |
C |
COR, class of recommendation; LOE, level of evidence.
1.2 Risk Prediction Models
A statistical model that estimates the probability (risk) of a certain event to occur is known as a risk prediction model. As for the primary prevention of cardiovascular disease (CVD), we assess the adult subjects with no history of CVD. Several models have been developed both in other countries and Japan to predict the incident rate and mortality rate from CVD based on their risk factors, efforts are being made to implement the use of such models for comprehensive risk assessment.23
Absolute risk is often expressed as a probability within a certain period, typically 10 years. However, young individuals generally have a lower absolute risk than older individuals; hence, even if the estimated 10-year risk at a young age is low, the lifetime risk may be high. Absolute risk can also be presented as lifetime risk to avoid giving the misleading impression that the risk is low, especially in young people. In addition, an index known as the “risk age” may facilitate their understanding. The “risk age” is an estimate of how the subject’s risk profile corresponds to that of a person with an ideal risk profile (normal blood pressure [BP], no dyslipidemia, no diabetes, and no smoking habit).24
In randomized controlled trials (RCTs), presenting the “risk age” rather than the 10-year absolute risk was more likely to motivate lifestyle-related25 and risk factor26 improvement.
1.2.1 Western Risk Prediction Models
Western CVD prevention clinical practice guidelines recommend routine comprehensive risk assessments according to sex and age. The 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice21 use SCORE2/SCORE2-OP (Systematic Coronary Risk Estimation 2/-Older Persons) as the comprehensive risk assessment tool. The 2019 American College of Cardiology/American Heart Association (ACC/AHA) Guideline on the primary prevention of cardiovascular disease22 recommends using pooled cohort equations (PCE). These predictive models define atherosclerotic CVD (ASCVD) as a combination of stroke and CAD and estimate an individual’s absolute risk of the incidence of and death from ASCVD.
Clinical practice guidelines in other Western countries have adopted the clinical method of estimating the absolute risk from a risk prediction model and then setting goals of care and choosing an appropriate treatment plan through shared-decision making with the patient. In general, the risk factor management needs to be more aggressive the higher the estimated risk. In addition, for the aforementioned reasons, it is recommended to calculate the lifetime risk, risk age, and 30-year risk for young individuals. The 10-year risk, lifetime risk, and risk age can be calculated using the web or specific applications (ESC: Cardiovascular Risk Age Calculator Based on the European Society Of Cardiology Heart Score Model,27 ACC/AHA: ASCVD Risk Estimator Plus28).
1.2.2 Japanese Risk Prediction Models (Table 5)
Table 5.
Comparison of Cardiovascular Disease Absolute Risk Prediction Models That Use Data From Japanese Cohort Studies
| Cohort name |
Outcome |
Risk evaluation
period |
Variables |
Subjects |
Baseline |
Follow-up
period |
| Hisayama study29 |
Coronary artery
disease +
atherothrombotic
stroke |
10-year
prognosis |
Age, sex, systolic blood
pressure (mmHg),
diabetes, HDL cholesterol
(mg/dL), LDL cholesterol
(mg/dL), proteinuria,
current smoking habit,
and regular exercise |
2,454 individuals aged
40–84 years without a
history of cardiovascular
disease living in
Hisayama Town,
Fukuoka Prefecture |
1988 |
24
years |
| Suita study30 |
Coronary artery
disease + stroke |
10-year
prognosis |
Age, sex, systolic/
diastolic blood pressure
(mmHg), non-HDL/LDL
cholesterol (mg/dL), HDL
cholesterol (mg/dL),
smoking habit, diabetes,
proteinuria, and
electrocardiogram (left
ventricular hypertrophy) |
6,550 people aged
30–79 years without a
history of cardiovascular
disease living in Suita
City, Osaka Prefecture |
1989/1999 |
16.9
years |
| JALS31 |
Stroke, acute
myocardial infarction,
combined outcome
of stroke/acute
myocardial infarction,
and all cardiovascular
mortality |
5- and 10-year
prognosis |
Age, sex, blood pressure,
HDL cholesterol (mg/dL),
non-HDL cholesterol
(mg/dL), atrial fibrillation,
BMI (kg/m2), eGFR (mL/
min/1.73 m2), smoking,
and diabetes |
67,969 people aged
40–89 years who
participated in 22
community cohort
studies in Japan |
2002–2004
(varies by
cohort) |
6.9
years |
| EPOCH-JAPAN32 |
Coronary artery
disease, stroke,
coronary artery
disease + stroke
mortality |
10-year
prognosis |
Age, sex, smoking,
systolic blood pressure,
proteinuria, diabetes,
total cholesterol/HDL
cholesterol ratio, and
interaction terms (age/
systolic blood pressure,
age/smoking) |
44,869 people aged
40–79 years without a
history of cardiovascular
disease who
participated in eight
cohort studies in Japan |
1988–2002 |
12.7
years |
BMI, body mass index; eGFR, estimated glomerular filtration rate; LDL, low-density lipoprotein; HDL, high-density lipoprotein. (Modified from Honda et al 2022,29 Nakai et al 2020,30 Harada et al 2019,31 and Li et al 2021.32)
Several models for predicting the risk of CVD have been proposed in Japan.29–32 The Hisayama study29 and Suita study30 are well-known cohort studies that form the basis of such investigations. The Japan Atherosclerosis Longitudinal Study (JALS)31 and Evidence for Cardiovascular Prevention From Observational Cohorts in Japan (EPOCH-JAPAN)32 are large-scale meta-analyses that integrated data from multiple cohorts in Japan (Table 5). As shown in the Table 5, each risk prediction model has different predicted outcomes (mortality/incidence), risk assessment period, target population, and baseline year. Care must be taken when applying each model.
a. Statistical Models for Estimation of Lifetime Risk
In Japan, multiple cohort studies have reported lifetime risk models33–38 stratified by the presence/absence of risk factors. However, although lifetime risk can be presented according to each risk factor, these models have not been widely applied in clinical settings.
b. Risk Age Models
Many of the well-known predictive models in Japan are presented as score table formulas. Therefore, “risk age” calculation requires extra efforts. Even with a risk chart panel, the range of ages and risk factor levels displayed on the panel are generally too wide to obtain a well-estimated “risk age” for a given individual based solely on the panel. The development of applications and online tools that can easily calculate the risk age in the busy clinical setting is desirable.
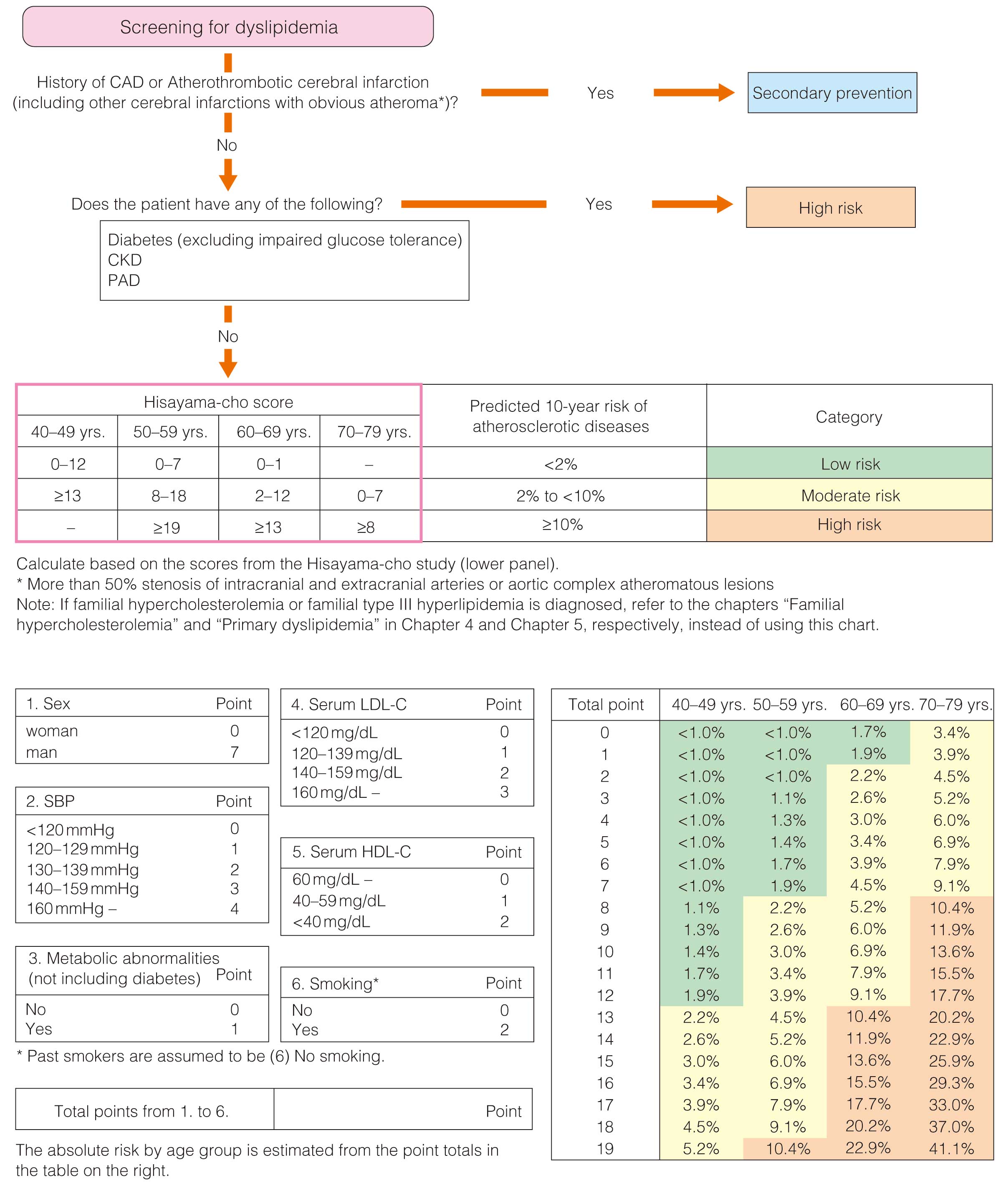
1.2.3 Application of Risk Prediction Models to Japanese Guidelines
According to the Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2022 endorsed by the Japan Atherosclerosis Society,39 individuals with diabetes, CKD, or peripheral arterial disease (PAD) are classified as “high risk”. In addition, the guidelines provide lipid management goals based on a classification of participants into 3 categories based on their 10-year absolute risk of ASCVD (CAD+atherothrombotic cerebral infarction): <2% corresponds to a low risk, 2–<10% corresponds to medium risk, and ≥10% corresponds to a high risk (calculated using a scoring system based on findings from the Hisayama study [for more details, see Chapter II.3 Dyslipidemia]). JAS provides a smartphone application and tool that enables prediction of the incidence of ASCVD on its website.40
The Japanese Society of Hypertension Guidelines for the management of hypertension (JSH 2019)41 recommend risk stratification (low, moderate, and high) with the combination of influential prognostic factors, and provides BP management guidelines based on this method of stratification, which has been confirmed to be consistent with the Hisayama model and JALS score, although the corresponding absolute risk has not been clarified.
1.2.4 Issues in Applying Risk Prediction Models in the Clinical Setting
Risk prediction models are created using real-life population data, but the prediction of absolute risk is known to be inaccurate when applied to groups or individuals with different characteristics (race, region, and baseline year). In fact, when the SCORE and Framingham scores used in Europe and the USA are applied to Japanese individuals, the absolute risk of CVD and CAD is overestimated.42,43
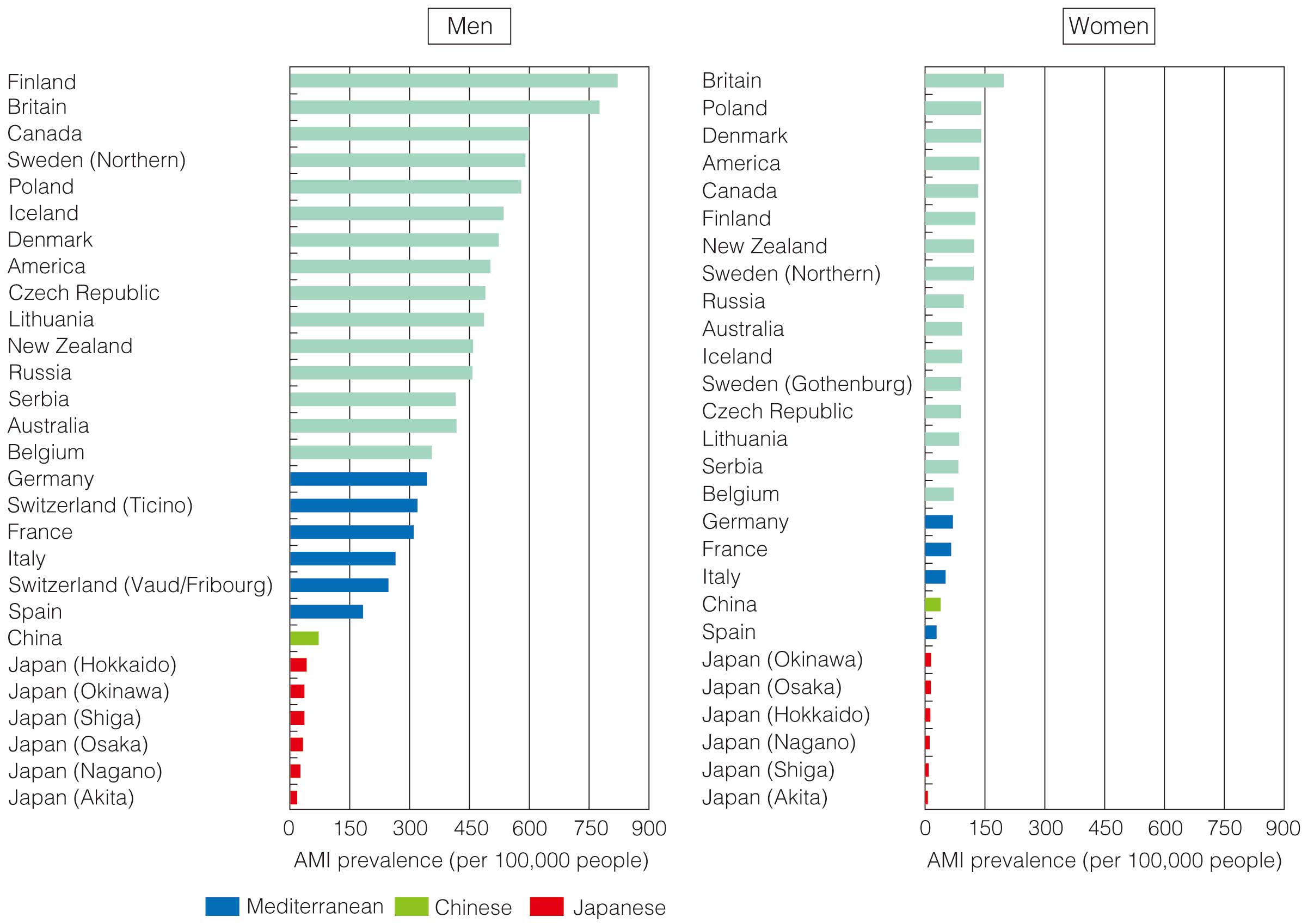
As mentioned in Chapter I.1, stroke events are more common in Japan than CAD-related events. Strokes are broadly classified as subarachnoid hemorrhage, intracerebral hemorrhage, and cerebral infarction. Cerebral infarctions are further clinically categorized as cardiogenic embolism, atherothrombotic cerebral infarction, lacunar infarction, and other cerebral infarctions. Of these, high low-density lipoprotein cholesterol (LDL-C) level (hyper-LDL-cholesterolemia) can be epidemiologically confirmed as a risk factor primarily for atherothrombotic cerebral infarction. In Japan, where other types of strokes are relatively predominant, hyper-LDL-cholesterolemia tends to be underestimated in models that predict outcomes including CAD and all types of stroke, which is a concern from the perspective of CAD prevention.
To address this concern, the JAS atherosclerosis prevention guidelines 201744 adopted the Suita score, with only CAD as an outcome, for risk evaluation of lipid disorders. In recent years, a new model has been developed based on the Hisayama study to predict composite outcomes of atherosclerotic cerebral infarction and CAD, and it has been adopted in the 2022 JAS guideline.39
1.3 Practical Application of Comprehensive Risk Assessment
1.3.1 Absolute Risk Estimation and Patient Communication
Estimating the future absolute risk using an appropriate risk prediction model is widely recognized as the initial step in patient assessment for preventing CAD. The risk prediction model is used to communicate with the patient, clarify the patient’s understanding of absolute risk, determine the expected risk reduction, and discuss the advantages and disadvantages of interventions.
1.3.2 Setting Treatment Goals
Based on specific treatment goals, other risk factors, complications, and the patient’s intentions, specific treatment goals and methods should be established with the patient’s agreement. (Each chapter should be referred to for treatment goals according to the absolute individual risk, age, and comorbidity.)
1.3.3 Practical Application of Comprehensive Risk Assessment
An individualized approach is needed to better understand the risks of each patient, to promote lifestyle changes, and to improve adherence to drug therapy. It is also necessary to recognize that there are various barriers to this process.45 Clinicians should be aware that risk comprehension literacy (cognitive factors), emotional factors, education level, mental state, and socioeconomic aspects, among others, affect the state of management. Additionally, factors that worsen drug therapy adherence, such as polypharmacy, the complexity of medications, the physician–patient relationships, lack of insight, misunderstanding of side effects, mental health issues, including depression, financial distress, and social conditions (e.g., living alone), among others, should be considered.46 Many studies have shown that motivational interviewing47 and multifaceted interventions by medical teams (such as shared decision-making support for treatment goals, multidisciplinary collaboration, patient motivation, and family collaboration) are useful.48,49
CQ: Is comprehensive risk assessment using risk prediction models for the primary prevention of CVD helpful in reducing mortality?
Multiple observational studies18–20 have reported that comprehensive management of modifiable risk factors reduces the risk of CVD in the general population. Findings from RCTs have shown that the tight control of modifiable cardiovascular risk factors also helps improve cardiovascular outcomes (CVOs) in patients with type 2 diabetes.50,51 Considering the above-mentioned research results and the rational importance of interventions to control multiple risk factors, comprehensive risk assessment is extremely important for primary prevention.
A systematic review was conducted on this topic (“Is comprehensive risk assessment using a risk prediction model useful for reducing mortality as the primary prevention of CVD?”).
• From 1990 to September 2021, MEDLINE (Ovid) was used to locate systematic reviews and meta-analytic studies, and 2 reviewers independently extracted and evaluated the literature. Studies that used risk prediction models in adults with no history of CVD in primary care were included: 841 studies were extracted, of which 6 related systematic reviews52–57 were identified. Only 3 studies used cardiovascular death as an outcome. Of the 9 RCTs,58–66 only 1 showed a reduction in mortality rate.58
• None of the studies were meta-analyzed, because of their low quality and high heterogeneity. Therefore, the effectiveness of comprehensive risk assessment using a risk prediction model in reducing CVD mortality is uncertain.
• The use of absolute risk estimates from risk prediction models is only one method of “comprehensive risk assessment” for all modifiable risk factors. Problems such as a lack of intuitive understanding of the “absolute risk” among both patients and medical professionals and the validity of the cutoff values for absolute risk should be taken into account. Because some of the studies showed improvement in risk factor management rates, further studies of risk assessment methods and analysis of their effectiveness are expected in the future.
2. Hypertension (Table 6)
Table 6.
Recommendations and Levels of Evidence for the Treatment of Hypertension in the Primary Prevention Of CAD
| |
COR |
LOE |
| Diagnosis of hypertension |
Hypertension is defined as an office blood pressure ≥140/90 mmHg, a home blood pressure
≥135/85 mmHg, or a 24-h ambulatory blood pressure ≥130/80 mmHg |
I |
A |
When there is a discrepancy between office blood pressure-based and home blood pressure-
based diagnoses, the home blood pressure-based diagnosis should have priority |
I |
B |
| Target levels of blood pressure control* |
Target blood pressure is <130/80 mmHg in individuals <75 years. In individuals ≥75 years,
blood pressure target is <140/90 mmHg. If the blood pressure is lowered to <130/80 mmHg in
individuals >75 years, the treatment should be continued if tolerated |
I |
A |
| Antihypertensive therapy |
To maintain normal blood pressure (<120/80 mmHg), instruct the patient to maintain a lifestyle
that is less likely to promote hypertension and cerebrocardiovascular disease. Lifestyle
modifications should be attempted in all individuals with blood pressure ≥120/80 mmHg
(high-normal blood pressure level or higher categories) |
I |
C |
Antihypertensive drugs are selected from 5 main classes, based on compelling indications:
calcium-channel blockers, ARBs, ACE inhibitors, low-dose thiazide diuretics, and β-blockers.
Calcium-channel blockers, ARBs or ACE inhibitors, or thiazide diuretics should be the first-line
drugs if there is no compelling indication |
I |
A |
If the blood pressure target is not achieved, a combination of two different classes of drugs
should be used at an early stage. If the target is not met with two drugs, using three or, if
necessary, four drugs should be considered. |
I |
A |
*For details on target levels of blood pressure, refer to Table 7. CAD, coronary artery disease; COR, class of recommendation; LOE, level of evidence.
2.1 Hypertension as a Risk Factor for CAD
Hypertension is a major risk factor for development of CAD, with mortality increasing exponentially with increasing BP if the systolic BP (SBP) or diastolic BP (DBP) is ≥120 mmHg or ≥75 mmHg, respectively, according to the findings of the Prospective Studies Collaboration meta-analysis that included 1 million individuals across age categories from 40 to 80 years.67 In the EPOCH-JAPAN, a meta-analysis of 11 cohorts enrolling approximately 70,000 individuals in Japan, middle-aged (40–64 years) and elderly (65–74 years) people with BP ≥120/80 mmHg and late-aged people (75–89 years) with BP ≥140/90 mmHg showed a greater risk of increased BP than those with BP <120/80 mmHg, who were at the lowest risk of cardiovascular death.68
2.2 Evaluation of BP
Based on epidemiological studies conducted in Japan, such as the Hisayama study, Tanno/Sobetsu study, NIPPON DATA80, and meta-analysis of the International Database of HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO),69–73 the updated Japanese Society for Hypertension guidelines for the management of hypertension (JSH2019) set the diagnostic criteria for hypertension as office BP ≥140/90 mmHg and home BP ≥135/85 mmHg.74
The Ohasama study and others have shown that home BP has better predictive power for cardiovascular death than office BP.75 Therefore, when diagnosing hypertension, if there is a discrepancy between office-based and home-based BP, the home-based BP has priority.74
White-coat hypertension is defined as an office BP ≥140/90 mmHg but home BP <135/85 mmHg or a 24-h ambulatory BP monitoring (ABPM) <130/85 mmHg. For those individuals who are on antihypertensive medication, the condition is described as “hypertension accompanied by white coat phenomenon or white coat effect”. Because such patients have the same short-term risk of cardiovascular events as those with normal BP or well-controlled hypertension, in principle, the immediate initiation or enhancement of antihypertensive drug therapy is not necessary. However, in the long term, the condition progresses to hypertension and leads to an increased risk of cardiovascular events. Therefore, home BP measurement and lifestyle modifications should be recommended, and careful follow-up should be performed.74 Patients with office BP <140/90 mmHg but home BP ≥135/85 mmHg or 24-h ABPM ≥130/80 mmHg are considered to have masked hypertension, which includes nocturnal hypertension, morning hypertension, and workplace hypertension. The risk of cardiovascular events in masked hypertension is similar to that in hypertension, and hence the patient should be treated with antihypertensive drugs.74
Traditionally, office BP ranges of 120–139 and 80–89 mmHg were considered as normal and high-normal, respectively. However, in EPOCH-JAPAN and other large-scale real-world data analyses conducted in Japan, the risk of cerebral and cerebrocardiovascular events was more than double that in individuals with BP <120/80 mmHg.68,76 Therefore, in JSH2019, the category names were changed to “normal BP” for BP <120/80 mmHg, “high normal BP” for BP 120–129/<80 mmHg, and “high BP” for BP 130–139/80–89 mmHg.74 To maintain BP at less than the normal BP of 120/80 mmHg, individuals should be instructed to maintain lifestyle habits that prevent not only increased BP but also cerebrocardiovascular disease from a young age and throughout their lives. Lifestyle modifications should be introduced for all individuals with high-normal or higher categories of BP (≥120/80 mmHg).74
2.3 Target Levels of BP
In the Systolic Blood Pressure Intervention Trial (SPRINT), a RCT with 9,361 patients aged ≥50 years with high-risk hypertension and no history of diabetes or stroke, in the strict antihypertensive group (target: automatic office measurement of SBP <120 mmHg, equivalent to normal office SBP <130 mmHg), the composite cardiovascular endpoints (myocardial infarction [MI], other acute coronary syndromes [ACSs], stroke, heart failure, and cardiovascular death) were 25% lower than that in the conventional antihypertensive group.77 Notably, heart failure and cardiovascular death were reduced by 38% and 43%, respectively, and all-cause death was also reduced by 27%. Similar results were observed in the SPRINT Elderly subanalysis of 2,636 patients aged ≥75 years.78 In a meta-analysis of 123 RCTs with 613,815 patients undergoing antihypertensive therapy including SPRINT, a 10-mmHg reduction in SBP was associated with a 20% reduction in major cardiovascular events and a 17% reduction in coronary events. BP reduction aimed at SBP <130 mmHg is suggested to be useful in preventing major cardiovascular events, regardless of the baseline BP level or comorbidities.79
The SPRINT final report confirmed that strict BP reduction targeting an SBP <130 mmHg significantly reduced MI by 28%.80 In addition, in the Trial of Intensive Blood-Pressure Control in Older Patients with Hypertension (STEP), where 8,511 aged patients (60–80 years) with hypertension were randomized into either a strict control group (target SBP 110–129 mmHg) or a standard control group (target SBP 130–149 mmHg), in the strict control group, the primary composite endpoint (stroke, ACS, acute decompensated heart failure, coronary revascularization, atrial fibrillation, and cardiovascular death) decreased by 26%, and acute CAD by 33%, as compared to that in the standard control group.81 Furthermore, in the strict control group, a 30% reduction was observed in BP values, without increase in the occurrence of serious adverse events, such as syncope, bone fracture, dizziness, and worsening of renal outcomes (1) decreased estimated glomerular filtration rate (eGFR) ≥50% in patients with CKD, 30% in those without CKD, (2) increased serum creatinine (male >1.5 mg/dL, female >1.3 mg/dL), and (3) development of end-stage kidney disease (ESKD; eGFR <30 mL/min/1.73 m2).81
Consequently, a meta-analysis of 51 RCTs of antihypertensive drug treatment by the Blood Pressure Lowering Treatment Trialists’ Collaboration (BPLTTC) published in 2021, which included 357,707 patients, showed that lowering SBP by 5 mmHg reduced the incidence of major cardiovascular events (CAD + stroke + death + hospitalization for heart failure), CAD, stroke, and hospitalization for heart failure by approximately 10% (for each event).82 Furthermore, in all age categories, including elderly elder (<85 years), the relative risk (RR)-lowering effects were similar in all baseline BP categories (not only in the hypertension range but also in the <120/80 mmHg and 120–139/80–89 mmHg ranges), regardless of primary or secondary prevention of CVD.82,83
Based on these findings, the BP target for the primary prevention of CAD is <130/80 mmHg for individuals <75 years, and <140/90 mmHg for individuals aged ≥75 years. In addition, if BP can be lowered to <130/80 mmHg, treatment should be continued if tolerable, considering organ damage associated with BP lowering, drug interactions, medication adherence, and medical economic effects. Table 7 shows the BP reduction targets in JSH2019,74,84 aimed at the prevention of cerebrocardiovascular disease caused by high BP.74 Caution is necessary, especially in older patients, because rapid BP reduction by intensive antihypertensive treatment, vomiting, diarrhea, and profuse sweating may cause excessive hypotension, cerebral ischemic symptoms such as dizziness, lightheadedness, dizziness on standing up, fainting, renal dysfunction, and electrolyte abnormalities.
Table 7.
Target Levels of Blood Pressure Control
| |
Office BP
(mmHg) |
Home BP
(mmHg) |
Adults <75 years*1
Patients with cerebrovascular disease (without bilateral carotid artery stenosis
and cerebral main artery occlusion)
Patients with CAD
Patients with CKD (proteinuria positive)*2
Diabetic patients
Patients using antithrombotic drugs |
<130/80 |
<125/75 |
Older patients aged ≥75 years*3
Patients with cerebrovascular disease (bilateral carotid artery stenosis or
cerebral main artery occlusion present or unevaluated)
Patients with CKD (proteinuria positive)*2 |
<140/90 |
<135/85 |
*1Among treatment-naïve individuals with office BP 130–139/80–89 mmHg, lifestyle modification is started or reinforced for low-risk or moderate-risk cases, and measures including start of antihypertensive treatment are taken for high-risk cases (if BP is not reduced by lifestyle modification lasting for ≈1 month or longer) with a final target set at <130/80 mmHg. If antihypertensive treatment has already been started and BP is 130–139/80–89 mmHg, lifestyle modification is reinforced for low-risk or moderate-risk cases and measures including reinforced antihypertensive treatment are taken for high-risk cases, with a final BP target <130/80 mmHg.
*2Proteinuria is judged as positive if protein level in random urine sample is ≥0.15 g/gCr.
*3In case where the goal of antihypertensive treatment is usually set as BP <130/80 mmHg considering comorbidities or other factors, achieving the goal of <130/80 mmHg should be attempted even in older patients (aged ≥75 years) if tolerable. Care needs to be taken of the risk for excessive hypotensive effects both during and after the process of achieving the goal of antihypertensive treatment. The judgment of excessive hypotensive effects should take into account the features of individual cases because it can vary depending on not only the achieved level of BP but also the magnitude or rate of BP reduction and the conditions in individual cases.
BP, blood pressure; CAD, coronary artery disease; CKD, chronic kidney disease. (Adapted from JSH guideline 2019.74)
2.4 Cerebrocardiovascular Risk Assessment in Hypertension Management
JSH2019 recommends the stratification of the risk of cerebrocardiovascular disease (Figure 3A) by a combination of prognostic factors, and also recommends the management of hypertension along with the BP level at the first visit74 (Figure 3B). For all people with high-normal BP (≥120/80 mmHg), lifestyle modification (salt intake restriction, fruit/vegetable intake, cholesterol/saturated fatty acid [SFA] intake restriction, obesity control (body mass index [BMI] <25 kg/m2), exercise, alcohol consumption reduction, and smoking cessation) should be implemented. For the high-risk patients with “elevated blood pressure” and those with “hypertension” (≥140/90 mmHg), lifestyle modification should be actively introduced as non-pharmacological therapy, and antihypertensive drug treatment should be initiated as necessary. In high-risk hypertensive subjects, drug treatment should be initiated early in addition to lifestyle modifications. In low- and moderate-risk hypertensive subjects, focusing on lifestyle habit modification, assessing the characteristics of each patient, and examining the need for drug therapy with progression are recommended.

In the US American College of Cardiology/American Heart Association (ACC/AHA) hypertension guidelines 2017, cerebrocardiovascular risk assessment based on the absolute atherosclerotic disease risk is used for hypertension management.85 The overall absolute risk assessment for cerebrocardiovascular disease is based on the results of Western cohort studies, but hypertension control using this absolute risk assessment is recommended in Japan as well. However, compared with Europe and the USA, Japan has a different disease structure, with fewer CAD cases and more strokes (see Chapter I). Target setting for comprehensive BP management based on an original Japanese version of a cerebrocardiovascular risk prediction model derived from domestic cohort studies is warranted (see Chapter II.1).
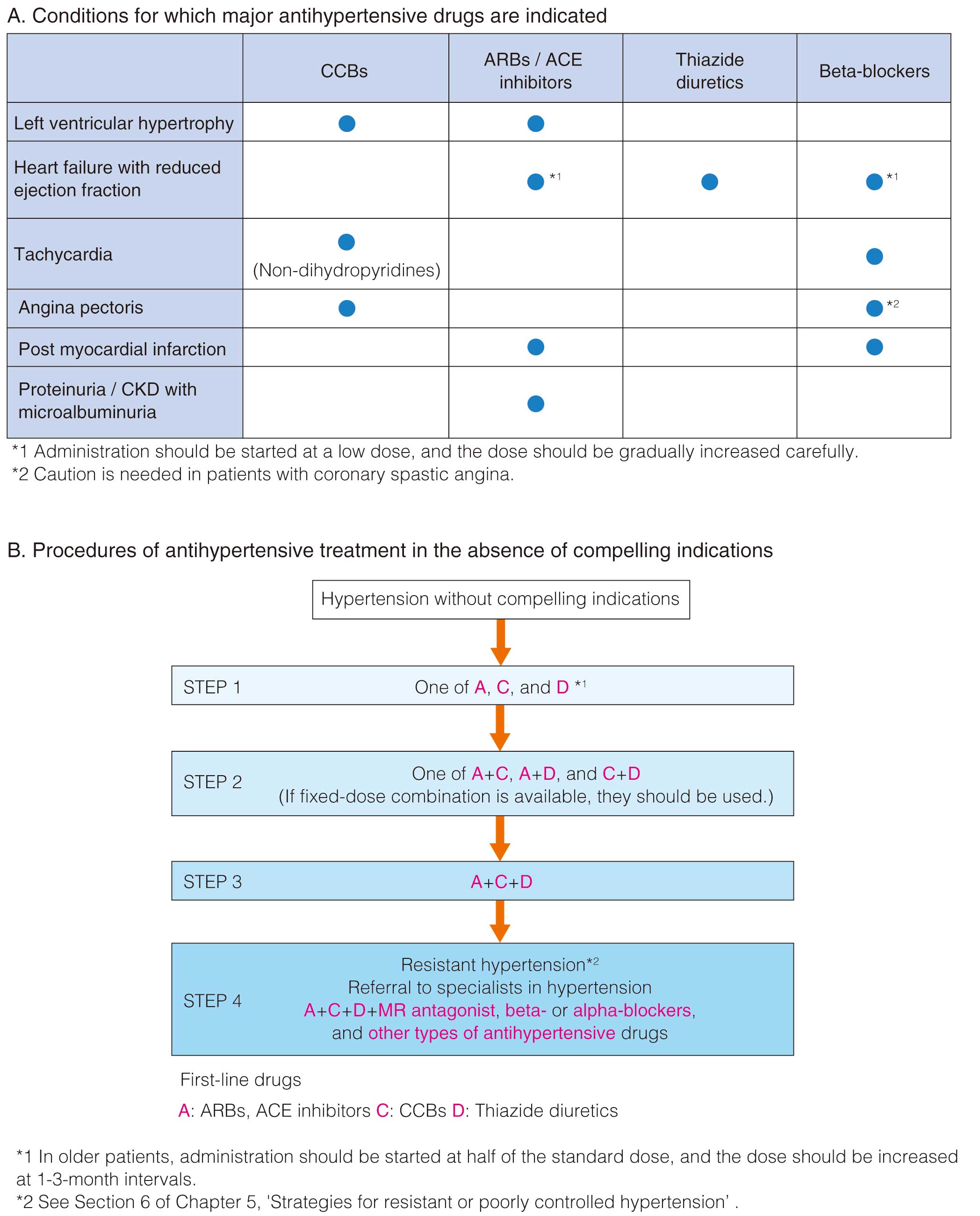
2.5 Drug Therapy for Hypertension
The major antihypertensive drugs belong to 5 classes that have been shown to prevent cerebrocardiovascular disease in large-scale RCTs: calcium-channel blockers (CCBs), angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), low-dose thiazide diuretics, and β-blockers.74 Compelling indications and recommendations for each major antihypertensive drug for treating conditions other than hypertension are shown in Figure 4A. CCBs, ARBs or ACE inhibitors, and thiazide diuretics are the first-line drugs for hypertension in the absence of compelling indications (Figure 4B). If the antihypertensive goal is not achieved, a combination of 2 different drug classes should be used from an early stage. If the lowering of BP is insufficient, 3 drugs should be used, and if necessary, ≥4 drugs.
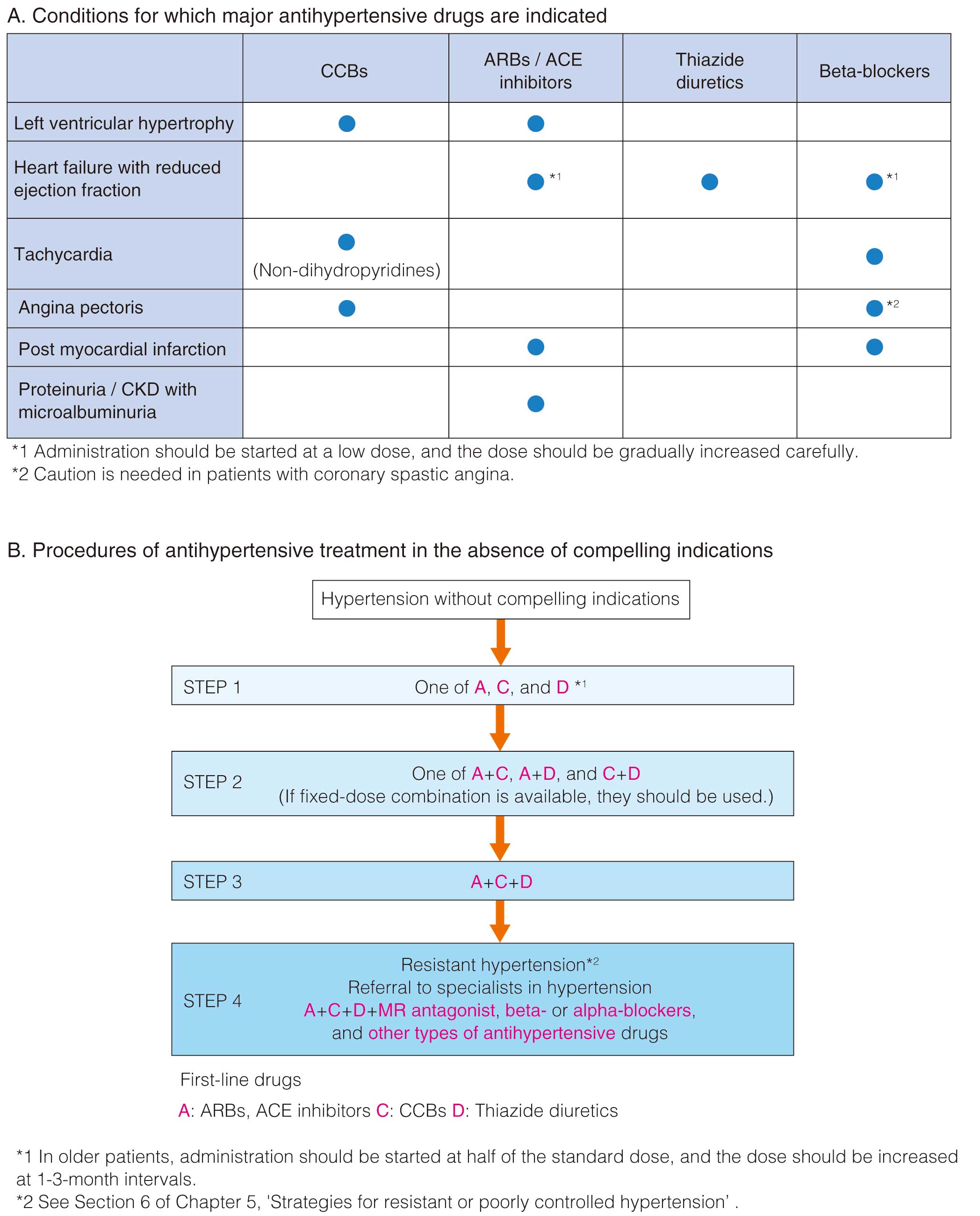
The effect of antihypertensive drugs on cerebrocardiovascular disease prevention largely depends on the degree of actual lowering of BP rather than the type of antihypertensive drug used.79,86 The Candesartan Antihypertensive Survival Evaluation in Japan (CASE-J), which targeted 4,703 high-risk hypertensive patients in Japan, found no difference in the incidence of angina pectoris and MI between the ARB candesartan and CCB amlodipine.87 In a meta-analysis of 26 RCTs conducted as a part of the 2007 BPLTTC study, which compared the effects of ACE inhibitors and ARBs on CAD inhibition with those of other treatments, although the BP-dependent reduction of CAD risk was equivalent, ACE inhibitors were suggested to exert a BP-independent reduction of CAD risk (i.e., a CAD preventive effect independent of BP-lowering).88 However, subsequent meta-analyses of more RCTs showed no significant difference between the actions of ACE inhibitors and ARBs and other antihypertensive agents in suppressing coronary events.79,86,89 Therefore, at present, clear evidence to confirm that 1 class of antihypertensive drug is superior to another in the primary prevention of CAD is unavailable.
When initiating antihypertensive treatment in people aged ≥75 years, clinicians should begin by administering half the standard dose. While paying attention to side effects, such as cerebral ischemic symptoms and decreased renal function, the dose should be titrated or combined with other medications to gradually lower the BP. Recommended first-line antihypertensive drugs and subsequent combination regimens are the same as those used for non-elderly patients.74
New antihypertensive drugs, such as an angiotensin-receptor neprilysin inhibitor (sacubitril valsartan) and a highly specific nonsteroidal mineralocorticoid receptor antagonist (MRA; esaxerenone), are suggested as effective for primary prevention of CAD. However, evidence to confirm their effects are lacking at the present time, and further investigation is awaited.
3. Dyslipidemia
3.1 Dyslipidemia as a Coronary Risk Factor and Screening
3.1.1 Changing Status of Screening for Dyslipidemia as a Coronary Risk Factor
This chapter is based on the concepts and recommendations from the Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2022,39 and Dyslipidemia treatment guide for the prevention of ASCVD,90 provided by the JAS for the evaluation and establishment of treatment goals for dyslipidemia. Table 8 shows the key recommendations for the treatment of dyslipidemia.
Table 8.
Recommendations and Levels of Evidence for Dyslipidemia Treatment in Primary Prevention of Cardiovascular Disease
| |
COR |
LOE |
Achievement of target goals decided by the comprehensive risk assessment for patients with
high LDL-C level should be prioritized via lifestyle modification and administration of cholesterol-
lowering therapy such as statins |
I |
A |
Non-HDL-C should be managed to reach the target goal after the LDL-C level has reached the
target goal |
IIa |
C |
In cases where the target level for LDL-C has been achieved, but hypertriglyceridemia persists
(with or without low HDL-C), drug treatment for dyslipidemia should be considered following the
implementation of appropriate lifestyle modifications |
IIa |
C |
COR, class of recommendation; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; LOE, level of evidence.
The clinical practice guideline endorsed by the JAS for primary prevention of atherosclerotic disease recommends a comprehensive evaluation including assessment of lipid level and other risk factors to estimate individual’s absolute cardiovascular risk.39 Therapeutic agents should not be administered based solely on the individual lipid levels, and it is important to understand the underlying pathology and comprehensive risk assessment of dyslipidemia before intervention. Dyslipidemia can be caused not only by genetic (and lifestyle) predispositions but also by secondary dyslipidemia as a result of other metabolic conditions that are present. Therefore, investigating underlying causes of dyslipidemia through blood sampling for biochemical and hormone level testing is important, and a thorough review of prescription drugs to treat the dyslipidemia90 (Table 9).
Table 9.
Classification and Etiology of Secondary Dyslipidemia
| Hypercholesterolemia |
| • Hypothyroidism |
| • Nephrotic syndrome |
| • Primary biliary cirrhosis |
| • Obstructive jaundice |
| • Diabetes |
| • Cushing’s syndrome |
| • Pheochromocytoma |
| • Drugs (diuretics, β-blockers, corticosteroids, oral contraceptives, cyclosporins, among others) |
| Hypertriglyceridemia |
| • Alcohol drinking |
| • Obesity |
| • Diabetes |
| • Nephrotic syndrome |
| • Chronic kidney disease |
| • Cushing’s syndrome |
| • Pheochromocytoma |
| • Uremia |
| • Systemic lupus erythematosus |
| • Serum protein abnormalities |
• Drugs (diuretics, non-selective β-blockers, corticosteroids, estrogens, retinoids, immunosuppressants, and anti-HIV
drugs, among others) |
(Adapted from Japan Atherosclerosis Society. 2018.90)
*Precautions for Lipid Measurements
Intravenous blood sampling for lipid levels should be performed after adequate fasting (≥10 h from the night before measurement, with exceptions for taking energy-free liquids such as water and tea).39 Lipid levels are measured for LDL-C, triglycerides (TG), high-density liporotein cholesterol (HDL-C), and total cholesterol (TC). Direct measurement of LDL-C level is recommended because the Friedewald’s equation (i.e., TC − HDL-C − 1 / 5 × TG) to estimate LDL-C is only valid when adequate fasting is performed with the patient’s TG level <400 mg/dL. With nonfasting random measurement, the levels of TC, HDL-C, and LDL-C (measured using the direct method) are minimally affected, although the level of TG alters at a wide range. Thus, direct measurement of LDL-C or non-HDL-C measurement (TC − HDL-C) should be used instead of the Friedewald’s equation.91 However, the accuracy of the 2 lipid level measurement methods can be altered when the TG level is extremely high (direct measurement of LDL-C: TG level ≥1,000 mg/dL, non-HDL-C: TG level ≥600 mg/dL). Additionally, lipid level measurement should be avoided in the following cases because the results may vary from the true value: decubitus position (as it increases circulating plasma volume), vasodilator treatment, high-volume infusions, acute phase of cardiogenic shock or ACS, and patients under heparin administration.92,93
3.1.2 Elevated LDL-C and Non-HDL-C Levels Associated With Development of CAD
Comparable to the results of epidemiological studies conducted in Europe and the USA, studies in Japan have also shown that the incidence and deaths due to CAD increase with higher levels of LDL-C.94–99 Furthermore, gradual increase in TC level with a threshold of around >220 mg/dL has also shown a statistically significant increase in the risk of incidence and death due to CAD in studies published before 1990,100–103 and after 1990.104–106 The incidence and deaths due to CAD and MI also increased when the non-HDL-C level increased at around >170 mg/dL.107–110
Evidence Related to Non-HDL-C Levels
Similar to high LDL-C levels, high non-HDL-C levels predict the onset of MI.104 In patients with dyslipidemia, high non-HDL-C levels differ from those of LDL-C by +30 mg/dL.109,111 When non-HDL-C is used for screening the general population, the difference between the non-HDL-C and LDL-C levels is <30 mg/dL, ranging with a difference of ≈20 mg/dL.112,113 Because non-HDL-C levels increase with increasing levels of lipoproteins related to atherosclerotic vascular disease, such as LDL and remnant lipoprotein, it is prognostically important in the risk assessment for potential CAD development in Japanese individuals.114 Of note, if there is a possibility of familial hypercholesterolemia (FH), familial combined hyperlipidemia, or familial type III dyslipidemia, all of which are high-risk primary dyslipidemias, special considerations for prevention and treatment are required.90
Based on this evidence, the 2022 JAS Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases recommend using a LDL-C cutoff value ≥140 mg/dL, which corresponds to a TC value of 220 mg/dL, or non-HDL-C value ≥170 mg/dL as the screening criteria for dyslipidemia.39 It is important to note that increases in lipid levels (except HDL-C) are linearly correlated with an increased risk for CAD development. Furthermore, when other risk factors are clustered with dyslipidemia, the incidence and mortality rate of CAD increase.115–117 Individuals with high non-HDL-C levels have an associated increased risk for MI when combined with a high TG level,118 and an increased risk for development of CAD with CKD.119 Based on these data, healthcare providers should comprehensively evaluate the individual’s risk for atherosclerotic vascular disease without relying solely on cholesterol measurement values (see Chapter III.2.1).
3.1.3 Low HDL-C and High TG Associated With Development of CAD
HDL-C levels show an inverse association with the risk of all-cause death,120 with an increase in the incidence of CAD at HDL-C levels <40 mg/dL.103,121,122 However, a number of cohort studies suggest that low levels of HDL-C alone are not associated with increased cardiovascular risk.123,124 Furthermore, some studies have reported an increase in the risk for CAD-related deaths with HDL-C level ≥80 mg/dL.125 Of note, women are known to have higher HDL-C levels than men, although studies on the association of sex difference and development of CAD remain scarce.121
High levels of fasting TG, especially >150 mg/dL, have been reported in association with the risk of development of CAD in the US Framingham study126 and other studies,127,128 as well as in Japan, regardless of adjustments for HDL-C levels.129–133 Furthermore, nonfasting TG levels have been reported in association with the development of CAD; thus, the European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS) has recognized a nonfasting TG level ≥175 mg/dL as indicating individuals at higher risk.134 Similarly, epidemiological studies in Japan have shown that a nonfasting TG level ≥165 mg/dL is associated with an increased risk for MI, stable angina, sudden death,129 and risk of ischemic CVD development.132 These findings prove that postprandial hypertriglyceridemia is an independent risk factor for CAD.
Based on these findings, the JAS Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2022 has set the screening criteria for dyslipidemia as follows: fasting TG ≥150 mg/dL or nonfasting TG ≥175 mg/dL; HDL <40 mg/dL.39 However, evidence indicating the efficacy of drug therapy targeted at directly lowering TG or increasing HDL-C is weak and inconclusive. Therefore, the addition or use of drug therapies to treat these conditions should be considered based on the individual’s risk on a case-by-case basis.
3.1.4 Correlation of Other Forms of Dyslipidemia and Development of CAD
Other forms of dyslipidemia such as remnant lipoprotein cholesterol, serum apolipoprotein B-48, high lipoprotein (a) [LP(a)], and small dense LDL39,90,135 have been reported in association with the development of atherosclerotic vascular disease and CAD, although evidence is lacking. Although these lipid measurements are not available in everyday practice, they may hold independent prognostic importance for the development of CAD.
3.2 Treatment of Dyslipidemia as a Coronary Risk Factor
3.2.1 Comprehensive Risk Assessment for Determining Treatment Goals and Setting Management Goals
The guidelines developed for the primary prevention of CAD in Europe, the USA, and Japan are all based on identifying and applying appropriate interventions in the high-risk population. First, the absolute risk of developing CAD should be calculated using a predictive model that includes various coronary risk factors, and subsequent interventions are based on the estimated risk. The 2018 ACC/AHA guideline136 recommends initiating high-intensity statins to individuals with LDL-C level >190 mg/dL, and initiating moderate-intensity statins to individuals aged 40–75 years with diabetes mellitus (DM). For the others, the guideline recommends initiating a moderate-intensity statin or achieving the LDL-C reduction goal according to an estimated 10-year ASCVD risk obtained with “ASCVD Risk Estimator Plus”. No specific target for LDL-C values is given in the 2018 ACC/AHA guideline. The 2021 ESC guideline21 recommends treating individuals without known CVD but with CKD, DM, or FH as high risk. For individuals without any of these conditions, the 2021 ESC guideline recommend the use of the SCORE2 system to predict 10-year risk of fatal and nonfatal cerebrocardiovascular events (acute MI [AMI] and cerebral infarction) corresponding to the individual’s age category: <50 years, 50–69 years, and >70 years. Additionally, depending on the individual’s age category, the 2021 ESC guideline suggests an initial step of lowering SBP to <140 mmHg (preferably <130 mmHg) and LDL-C level <100 mg/dL for individuals with a 7.5–10% estimated risk. Furthermore, the recommended 2nd step is lowering SBP to <130 mmHg and LDL-C level to <70 mg/dL. However, it is important to note that the risk models developed in Europe and the USA have consistently overestimated the risk for the incidence of CAD in cohort studies in Japan.42
The 2017 JAS Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases adopted the Suita score as an absolute risk prediction model because it estimates the absolute risk of CAD appropriately accounting for LDL-C levels in the Japanese population. However, the Suita score only includes CAD as the outcome of interest and does not include stroke, in contrast to the United States Pooled Cohort Equation or the SCORE2. In light of the increasing incidence of atherothrombotic cerebral infarction in Japan in recent years, the 2022 JAS Guidelines39 adopted the risk prediction model based on the findings of the Hisayama study published in 2021. The Hisayama model predicts the onset of ASCVD, including both CAD and atherothrombotic cerebral infarction as a composite outcome, and it was considered to be more practical to set the LDL-C level for managing goals based on that study.39
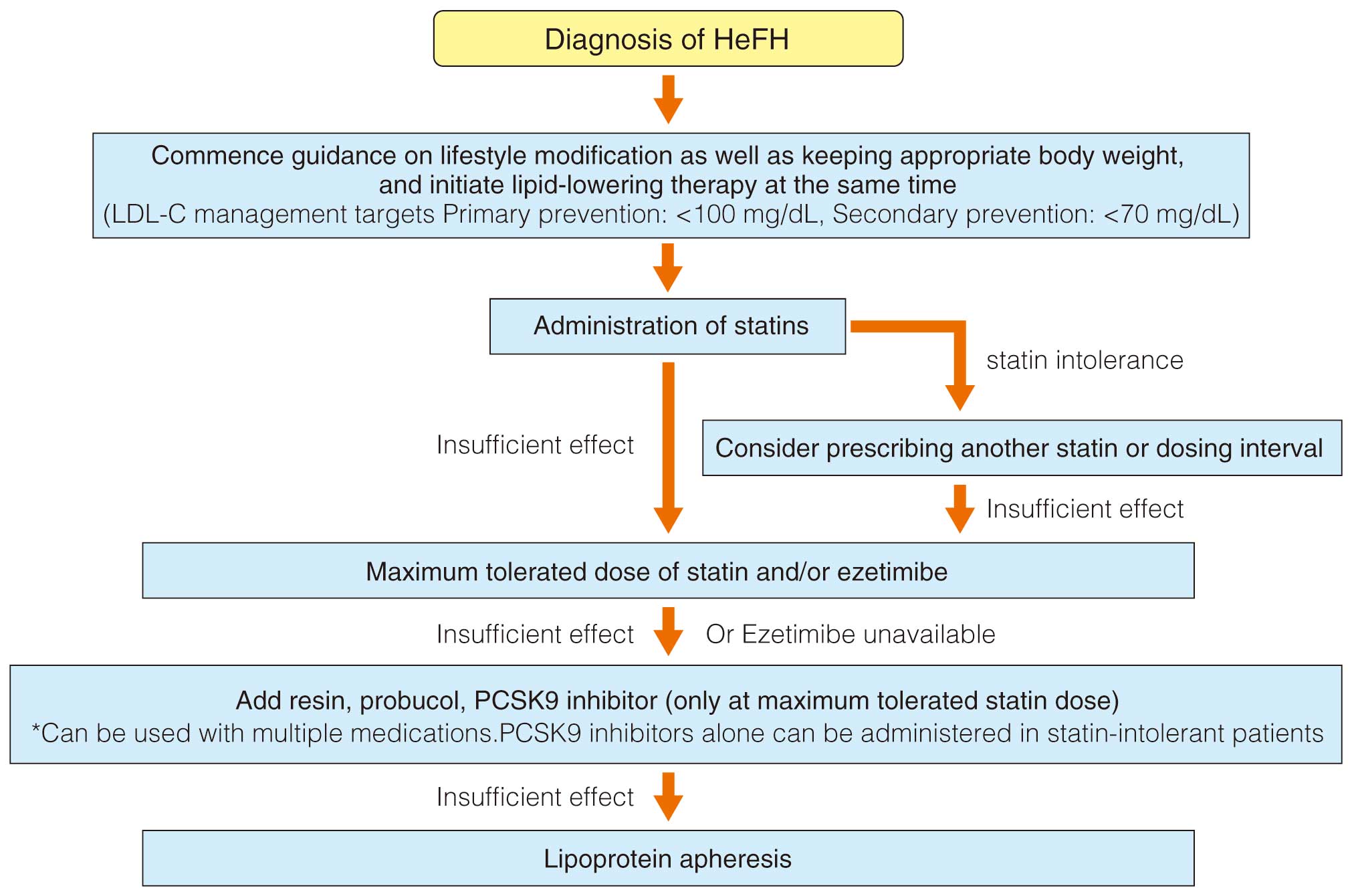
3.2.2 Approach to Atherosclerotic Disease Primary Prevention (Figure 1)
In the 2022 JAS Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases, individuals with a previously known history of CAD, atherothrombotic cerebral infarction, or other atherosclerotic cerebral infarctions (involving blood vessel stenosis ≥50% of the intracranial and extracranial arteries or complex aortic atheromatic lesions) are considered to be targets for secondary prevention. Individuals are considered as high risk if they have DM, CKD, or PAD. Other individuals should undergo comprehensive risk assessment by calculating the absolute 10-year risk of ASCVD using the Hisayama risk prediction model. Individuals will be categorized as “low risk (<2%)”, “moderate risk (2–<10%)” or “high risk (≥10%)” (Figure 5).39 Furthermore, target lipid management levels have been established for each of these risk categories (Table 10).39 Patients with DM associated with PAD, diabetic microangiopathy (retinopathy, nephropathy or neuropathy), or current smoking habit, are recommended to lower their LDL-C level to <100 mg/dL (non-HDL-C level <130 mg/dL). Of note, the high-risk group defined in the ESC guideline with an estimated risk of 7.5–10% has the same LDL-C target set for lowering risk.
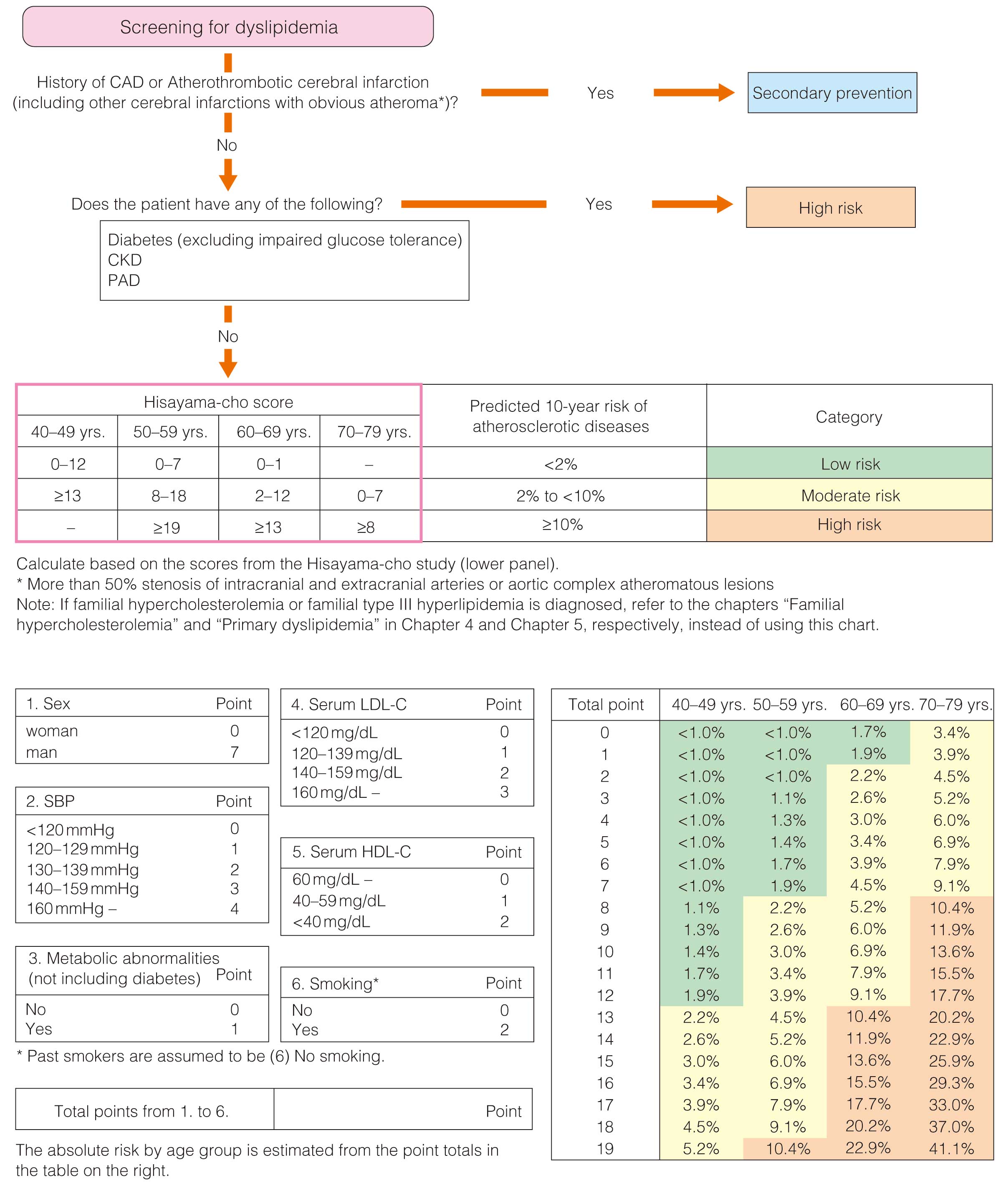
Table 10.
Management Target Values by Risk Category in the Primary Prevention of Coronary Artery Disease
| After lifestyle improvement, the indications for drug therapy should be considered |
| Lipid management targets (mg/dL) |
LDL-C |
Non-HDL-C |
| Low-risk (<2%)* |
<160 |
<190 |
| Medium-risk (2–9%) |
<140 |
<170 |
| High-risk (>9%) |
<120 |
<150 |
| Diabetes** complications |
<100 |
<130 |
*The percentages shown are the expected 10-year risks of atherosclerosis development.
**Diabetes and PAD, microangiopathy (retinopathy, nephropathy, or neuropathy), or a smoking habit in the patient should be
considered. |
| |
TG |
HDL-C |
| Lipid management targets (mg/dL) |
<150#
<175
(non-fasted) |
≥40 |
#Management of the TG and HDL-C values should be considered when the management target values for LDL-C and non-HDL-C are achieved. Fasting refers to a state of fasting ≥10 h. The intake of calorie-free liquids, such as water and tea, among others, is allowed.
HDL, high-density lipoprotein; LDL, low-density lipoprotein; PAD, peripheral artery disease; TG, triglycerides. (Adapted from Japan Atherosclerosis Society. 202239 with modifications)
Treatment decisions for individuals younger than 40 years of age should be made through discussion between the individual and the physician, because risk prediction is not possible from the Hisayama study, which included a cohort aged ≥40 years. In addition, the evidence for blood cholesterol-lowering interventions has been derived from populations aged <80 years.
Management target values are simply achievement targets. The physician should make the final judgment for deciding treatment goals and methods after considering variations in the characteristics, living environment, and adherence level of individual patients.
3.2.3 Management Goals for Patients With Diabetic Dyslipidemia
Extensive studies of Japanese populations have reported on the management of patients with diabetic dyslipidemia. The elevation of LDL-C levels increased the risk of CAD in patients with diabetes,137 and LDL-C-lowering therapy with statins significantly decreased coronary events.138,139 In the EMPATHY study, the number of cardiovascular events in patients targeting LDL-C of 100–120 mg/dL did not differ from those targeting <70 mg/dL among Japanese patients with diabetic retinopathy.140 However, the EMPATHY study showed a low achievement rate for the targeted LDL-C values, and an additional analysis of the population that achieved the target value revealed a lowered risk for cardiovascular events.141 The 2021 ESC guideline also recommends LDL-C ≤100 or ≤70 mg/dL for moderate-/high-risk patients with diabetes, respectively.136 Thus, the desired LDL-C control target was set as ≤100 mg/dL for patients with diabetes and diabetes-associated complications (Table 10). Of note, the 2021 ESC guideline indicates that the risk status for CKD is equal to or greater than that of DM,137 although the evidence indicating such risk remains insufficient in Japan.
3.2.4 Lifestyle Improvement and Drug Treatment for Dyslipidemia
Primary prevention should begin with lifestyle modifications, including the aspects shown in Chapter II.5, II.6 and II.7. Only after assessing the effectiveness of these efforts for 3–6 months, should drug treatment(s) be considered.
Table 11 shows the expected effects of blood cholesterol-lowering agents that are available for use in Japan and their common side effects.90 Statins, ezetimibe, anion exchange resins, probucol, and proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors are generally used to lower LDL-C levels. Fibrates, selective peroxisome proliferator-activated receptor-α modulators (SPPARMα; Pemafibrate), eicosapentaenoic acid (EPA) or n-3 polyunsaturated fatty acids (PUFAs), and nicotinic acid derivatives are used to lower TG levels. Although the efficacy and safety of the majority of these therapeutic agents have been established, the safety of long-term administration of PCSK9 inhibitors has not yet been confirmed.90 According to the Statin Intolerance Clinical Guide 2018 by the JAS Statin Intolerance Clinical Guide Working Group, statins have been discontinued in 15–20% of patients due to side effects such as myalgia and elevated creatine kinase levels.142 However, detailed review of those cases showed that the incidence of “true” statin intolerance that require complete discontinuation of statins was estimated to be 0.5%, and most cases of “statin intolerance” can be resolved by reducing the dose or discontinuing for a short duration and restarting statin therapy after relief in symptoms. In addition, the decrease in HDL-C levels observed during use of probucol is thought to be the result of activation of reverse cholesterol transport and is considered useful to reduce atherosclerotic plaque progression.143
Table 11.
Characteristics and Side Effects of Current Therapeutic Agents for Hyperlipidemia
| Category |
LDL-C |
Non-HDL-C |
TG |
HDL-C |
Side effects |
Generic names |
| Statins |
↓↓ ∼ ↓↓↓ |
↓↓ ∼ ↓↓↓ |
↓ |
− ∼ ↑ |
Rhabdomyolysis, myopathy-like
symptoms such as myalgia and
weakness, liver disorders, cognitive
dysfunction, elevated fasting blood
glucose and HbA1c levels, and interstitial
pneumonia, among other symptoms |
Pravastatin, simvastatin,
fluvastatin, atorvastatin,
pitavastatin, rosuvastatin |
Small intestinal
cholesterol
transporter
inhibitors |
↓↓ |
↓↓ |
↓ |
↑ |
Gastrointestinal symptoms, liver
damage, increased CK
*Caution is required as drug efficacy
may be enhanced when the drugs are used in
combination with warfarin |
Ezetimibe |
Anion exchange
resins |
↓↓ |
↓↓ |
↑ |
↑ |
Gastrointestinal symptoms
*Caution is required as the drug efficacy
may be reduced when used in
combination with digitalis or warfarin |
Cholestymid,
cholestyramine |
| Probucol |
↓ |
↓ |
− |
↓↓ |
Reversible QT prolongation and
gastrointestinal symptoms, among
other symptoms |
Probucol |
| PCSK9 inhibitors |
↓↓↓↓ |
↓↓↓↓ |
↓ ∼ ↓↓ |
− ∼ ↑ |
Injection site reaction, nasopharyngitis,
gastroenteritis, liver damage, and
increased CK, among other symptoms |
Evolocumab, alirocumab |
| MTP inhibitor* |
↓↓↓ |
↓↓↓ |
↓↓↓ |
↓ |
Hepatitis, liver dysfunction, and
gastrointestinal disorders |
Lomitapide |
| Fibrates |
↑ ∼ ↓ |
↓ |
↓↓↓ |
↑↑ |
Rhabdomyolysis, cholelithiasis, and
liver damage, among other symptoms |
Bezafibrate, fenofibrate,
clinofibrate, clofibrate |
Selective PPARα
modulator |
↑ ∼ ↓ |
↓ |
↓↓↓ |
↑↑ |
Rhabdomyolysis and cholelithiasis,
among other symptoms |
Pemafibrate |
Nicotinic acid
derivatives |
↓ |
↓ |
↓↓ |
↑ |
Flushing, headache, and liver damage,
among other symptoms |
Niceritrol, nicomol,
tocopherol nicotinate |
n-3 polyunsaturated
fatty acids |
− |
− |
↓ |
− |
Digestive symptoms, bleeding tendency,
and rash, among other symptoms |
Icosapent ethyl, omega-3
fatty acid ethyl |
*Indicated for patients with homozygous familiar hypercholesterolemia.
↓↓↓↓: <−50% ↓↓↓: −50∼30% ↓↓: −20∼30% ↓: −10∼−20% ↑: 10∼20% ↑↑: 20∼30% −: −10∼10%
HDL, high-density lipoprotein; LDL, low-density lipoprotein; TG, triglycerides. (Adapted from Japan Atherosclerosis Society. 2018.90)
3.2.5 Intervention for High LDL and High Non-HDL-C Dyslipidemia
Achieving the management target value for LDL-C should be prioritized over control of non-HDL-C (Table 10). After the target LDL-C value is achieved, management of non-HDL-C should be considered. The target non-HDL-C level should be set as the LDL-C level (mg/dL) plus 30 mg/dL.144,145 Therapeutic benefits can be also obtained with a proportional decrease in LDL-C level, as set in guidelines published in other countries. If the patient is categorized as low- or moderate-risk, the aforementioned target can be reasonably replaced with a target of 20–30% LDL-C reduction.39
Statins are recommended as the first-line drug for the treatment of high LDL-C based on the abundance of evidence showing demonstrating efficacy (Table 11).90 In Japan, a study has shown that administration of high-intensity statins is effective for reducing CAD events in the secondary prevention setting.146 Primary prevention using medications targeting lower blood cholesterol levels has been proven effective at reducing cardiovascular events in various meta-analyses.147–150 Similar results on primary prevention for CAD have been reported from Japanese studies such as the MEGA Study,151 and the 10-year J-LIT study.152 Thus, aiming for the management target values set in these studies is recommended. Statins have been shown to prevent coronary events among the elderly aged <75 years,153,154 and their use in elderly patients is recommended in the 2022 JAS Guidelines.39
A meta-analysis of RCTs showed that non-statin LDL-lowering interventions using diet modification, anion exchange resin, or ezetimibe also demonstrated a reduction in cardiovascular events when compared with a control group.155 If the management target value cannot be achieved through administration of standard-dose statin, statins should be titrated to the maximum tolerated dose, or the addition of ezetimibe can be considered. In Japan, ezetimibe has been shown to decrease cardiovascular events by 34% compared with patients who only had diet modification among elderly individuals aged from 75 to 84 years.156 Nonetheless, ezetimibe has not been shown to reduce cardiovascular risk when administered as the sole blood cholesterol-lowering agent or as an adjunct to statins in the primary prevention setting, although it suppresses cholesterol absorption induced by statin use and lower LDL-C.157
PCSK9 inhibitors, which block PCSK9 associated with the reuse of LDL receptors, are extremely potent agents for lowering the LDL-C level. Results from clinical trials indicate that PCSK9 inhibitors, in combination with statins or statins and ezetimibe, are effective in secondary prevention.39 However, there is limited evidence to confirm whether the use of PCSK9 inhibitors is effective for primary prevention of cardiovascular events.158
If the non-HDL-C level remains high despite LDL-C achieving the target level, high quantities of residual lipoprotein and Very low-density lipoprotein particles, which are often known as the source of “residual risk for atherosclerotic disease”, are likely to be present. In many of these cases, high TG levels are also observed in the presence of lipoproteins containing a large quantity of TG (TG-rich lipoproteins including remnant lipoproteins). The importance of non-HDL-C management after LDL-C level management in cases of high TG levels has been recognized in Japan,39,150 and its validity has been confirmed in overseas studies in recent years.159,160 In the 2021 ESC guideline, the non-HDL-C level is used to calculate risk with the SCORE2 system, although the LDL-C level is set as the treatment target.137 In such situations, the dose of statins is often increased, and ezetimibe, fibrates, SPPARMα, EPA or n-3 PUFAs are used in combination with statins, although evidence supporting the efficacy of such an approach remains scarce.
3.2.6 Intervention for High TG and Low HDL Levels
High TG and low HDL-C levels are associated with obesity (especially metabolic syndromes associated with an increase in visceral fat), excessive intake of carbohydrates and fats, and physical inactivity. Furthermore, insulin resistance and diabetes impair lipoprotein metabolism and cause high TG and low HDL-C levels by increasing the levels of remnant lipoproteins and destabilizing HDL particles. Therefore, when high TG and low HDL-C is confirmed, lifestyle modification should be the initial strategy to achieve management goals.39 Concurrently, appropriate therapeutic interventions should be considered for controlling LDL-C and non-HDL-C levels. According to the 2021 ESC guideline,21 if a high-risk patient with a TG level ≥150 mg/dL cannot maintain the TG level at <200 mg/dL with lifestyle modification alone, the administration of drugs (statins, fibrates, PCSK9 inhibitors or n-3 PUFAs) should be considered. The 2022 JAS Guidelines also recommend the use of medical therapy when individuals cannot achieve the management goal of fasting TG <150 mg/dL, nonfasting TG <175 mg/dL, or HDL-C level ≥40 mg/dL after 3–6 months of lifestyle modification.39
It is shown that fibrates, EPA, n-3 PUFAs, and SPPARMα effectively lower TG levels and increase HDL-C levels (Table 11), but few studies have shown a reduction in cardiovascular events. A large meta-analysis of RCTs showed that a decrease in non-HDL-C levels were associated with significantly lower RR, although a decrease in TG levels led to no significant difference in the RR for cardiovascular events.161 Based on these findings, the 2022 JAS Guidelines recommend using TG-lowering drugs for patients who have achieved their LDL treatment goal but have high non-HDL-C and high TG levels, with the objective of lowering cardiovascular risk.39
The therapeutic effect of TG-lowering agents depends on the lipid status of the individual prior to treatment. Fenofibrate exhibits limited efficacy when used in patients with only high TG levels,162–164 but is effective in those with both high TG and low HDL-C levels when co-administered with statins.163,165,166 However, the JELIS study conducted in Japan failed to show a significant primary preventive effect of EPA in the overall study population,167 although a subgroup analysis showed potential benefit in those with high TG and low HDL-C levels.168 Preventive effects have also been observed in individuals with controlled LDL-C levels but high non-HDL-C levels,169 and in patients with diabetes/hyperglycemia;170 the study population contained a secondary prevention population of approximately 20%.
Overseas data have shown the primary preventive effect of icosapent ethyl (4 g/day), which is a similar to EPA, among patients with diabetic complications, on statins (LDL-C <100 mg/dL), and with high TG levels (150–499 mg/dL).171 In contrast, n-3 PUFAs, which include both EPA and DHA, have not been effective in reducing events.172 Thus, when deciding the treatment for high TG for the purpose of primary prevention, coexistence of high non-HDL-C or low HDL-C must be taken into consideration. Of note, nicotinic acid, a therapeutic agent that increases the HDL-C level, has not been effective in preventing coronary-related events.173 Probucol has been shown to reduce risk of cerebrocardiovascular diseases among patients with FH or CAD, warranting its use for secondary prevention. However, the effectiveness of probucol for primary prevention remains to be demonstrated.174,175
4. Diabetes / Obesity
4.1 DM and Impaired Glucose Tolerance (IGT) as Coronary Risk Factors
Individuals with DM have a 2–4-fold higher prevalence of CAD compared with individuals without DM.176–178 The presence of DM is known to be equivalent to possessing 2 of the 3 established CAD risk factors, namely BP, cholesterol, and smoking.179 In addition, studies conducted in other Western countries have shown that the incidence of first MI in patients with DM is as high as that of recurrent MI in those without DM.180 In Japan, evidence from the J-ACCESS study supports this finding.181 However, the risk of CAD events varies considerably, depending on various factors such as the disease duration, glycemic control status, treatment methods, and complication status. Therefore, the results may differ according to the characteristics of the population in question.
The following points should be noted as characteristics of DM/IGT when considering the CAD risk: (1) poor glycemic control (high HbA1c) increases the risk of CAD;7 (2) patients in the prediagnostic stage of DM (i.e., with IGT, in which the HbA1c levels have not yet increased) are at a higher risk of CAD than patients with normal glucose tolerance;183–185 (3) the risk of CAD increases with progression of microalbuminuria to overt nephropathy, and the complication/progression of diabetic nephropathy further increases the risk of CAD;186 (4) the progression of diabetic retinopathy is closely related to the progression of CAD.187,188
4.2 Therapeutic Intervention for DM and IGT
4.2.1 Strict Blood Glucose Control
Evidence from meta-analyses of previous intervention trials has shown that enhanced glycemic control reduces the incidence of MI.189,190 However, for the beneficial effect of strict glycemic control to manifest, relatively longer-term follow-up is needed. In the UKPDS study for type 2 DM, no significant difference was observed in the incidence of MI during the study period (median 10.4 years) in the group that underwent strict glycemic control after the diagnosis of DM compared with the group that underwent more gradual glycemic control under normal treatment.191 In addition, the ACCORD, ADVANCE, and VADT studies did not show a significant inhibitory effect on cardiovascular events through strict glycemic control during the relatively short treatment period.192–194 However, even in those trials, follow-up studies conducted after the completion of the intervention trials did show a significant suppressive effect of intensive treatment on cardiovascular events.195–197 Hence, sufficient glycemic control from an early stage (early diagnosis) is important to prevent cardiovascular events (Table 12). Conversely, enhanced glycemic control using insulin or sulfonylurea (SU) drugs is likely to promote obesity and increase the frequency of hypoglycemia.192,193 Because these factors can increase the risk of CAD, care must be taken to avoid promoting obesity and hypoglycemia during therapeutic interventions.
Table 12.
Recommendations and Levels of Evidence for Patients With Diabetes and Obesity
| |
COR |
LOE |
In patients with obesity, metabolic syndrome, impaired glucose tolerance/diabetes associated with
obesity, weight loss should be first attempted via lifestyle improvement. Concurrent long-term
management of modifiable risk factors is necessary using drug therapy and other resources |
I |
B |
| Appropriate glycemic control should be performed from the early stage of diabetes diagnosis |
I |
A |
Nonhyperglycemic coronary risk factors, such as obesity, hypertension, dyslipidemia, and chronic
kidney disease, should also be managed comprehensively in patients with diabetes |
I |
B |
COR, class of recommendation; LOE, level of evidence.
4.2.2 Glucose-Lowering Agents
Table 13 shows the hypoglycemic drugs that are currently available in Japan.198 From the viewpoint of CAD prevention, it is desirable to select drugs that do not promote obesity or cause hypoglycemia.
Table 13.
Characteristics of Hypoglycemic Drugs
| Mechanism |
Type |
Primary effects |
Risk of
hypoglycemia
when
administered
alone |
Effect on
body
weight |
Major side effects |
Contraindications |
Precautions for use |
Main evidence |
Non-insulin
secretagogues |
α-glucosidase inhibitor (α-GI) |
Suppression of
postprandial blood
glucose elevation by
delaying the absorption
and decomposition of
carbohydrates in the
intestinal tract |
Low |
None |
Gastrointestinal
disturbances,
flatus, liver
damage |
Common contraindications
for oral antidiabetic drugs* |
(1) Treat hypoglycemia with
monosaccharides such as
glucose
(2) Can be used in combination
with insulin in patients with
type 1 diabetes |
|
| SGLT2 inhibitor |
Promotion of urinary
glucose excretion by
inhibiting glucose
reabsorption in the
kidney |
Low |
Weight
loss |
Genital/urinary
tract infections,
dehydration, rash,
ketosis |
Common contraindications
for oral antidiabetic drugs* |
(1) In patients with type 1
diabetes, some preparations
can be used in combination
with insulin
(2) Hypoglycemia cannot be
expected in patients with
severe renal dysfunction with
eGFR <30 |
(1) Exerts a
protective effect
on the heart and
kidneys
(2) Exerts a
suppressive
effect on heart
failure |
| Thiazolidinediones |
Improvement of insulin
resistance in skeletal
muscles and the liver |
Low |
Weight
gain |
Edema, heart
failure |
Heart failure, history of
heart failure, bladder cancer
treatment, type 1 diabetes,
common contraindications
for oral antidiabetic drugs* |
(1) Causes fluid retention and
promotes the differentiation
of adipocytes, resulting in
weight gain and edema
(2) Increases the risk of fractures
in postmenopausal women |
Increases HDL-C
and lowers TG |
| Biguanide drug |
Suppression of glucose
production in the liver |
Low |
None |
Gastrointestinal
disturbances, lactic
acidosis, low
vitamin B12 levels |
Dialysis cases, eGFR
<30 mL/min/1.73 m2, history
of lactic acidosis, heavy
drinking, type 1 diabetes,
contraindications for oral
antidiabetic drugs* |
(1) Maximum dose of metformin
for each eGFR (30≤eGFR
<45; 750 mg, 45≤eGFR<60;
1,500 mg)
(2) In patients with eGFR 30–60,
metformin should be
discontinued before or during
iodine-contrast imaging. Do
not restart metformin for 48 h
after the administration of an
iodinated contrast medium,
and in case of concerns about
worsening renal function,
reintroduce after the eGFR is
measured to assess renal
function |
Suppresses
macroangiopathy in
patients with type 2
diabetes with obesity |
Insulin
secretagogues |
Glucose-
dependent |
Imeglimin |
Glucose-dependent
insulin secretagogue
mediates the improvement
of insulin resistance |
Low |
None |
Gastrointestinal
disorders |
Common contraindications
for oral antidiabetic drugs* |
(1) Not recommended for patients
with eGFR <45 mL/min/1.73 m2
(2) Increased frequency of
gastrointestinal symptoms in
combination with metformin |
|
| DPP-4 inhibitor |
Stimulation of blood
sugar-dependent insulin
secretion by inhibiting the
degradation of GLP-1 and
GIP and suppression of
glucagon secretion |
Low |
None |
Increased
hypoglycemia,
gastrointestinal
disorders, skin
disorders, and
pemphigoid in
combination with
SU drugs |
Type 1 diabetes, common
contraindications for oral
antidiabetic drugs* |
(1) Concomitant use of SU drugs
and insulin may increase the
incidence of hypoglycemia;
thus, reduction of the dose of
SU drugs and insulin should
be considered |
|
GLP-1 receptor
agonist |
Enhancement of GLP-1
action without
degradation by DPP-4
promotes glucose-
dependent insulin
secretion and suppresses
glucagon secretion |
Low |
Weight
loss |
Gastrointestinal
disorders, injection
site reactions
(redness and rash,
among other
symptoms) |
Type 1 diabetes, common
contraindications for oral
antidiabetic drugs* |
(1) The concomitant use of SU
drugs and insulin may
increase the incidence of
hypoglycemia; thus, reduction
of the dose of SU drugs and
insulin should be considered |
Exerts a protective
effect on the heart
and kidneys |
Glucose-
independent |
Sulfonylurea
(SU) drugs |
Stimulation of insulin
secretion |
High |
Weight
gain |
Liver damage |
Type 1 diabetes, common
contraindications for oral
antidiabetic drugs* |
(1) Risk of hypoglycemia is high
in the elderly, so administration
should be initiated at a low
dose
(2) Risk of hypoglycemia
increases in patients with
advanced renal or hepatic
dysfunction |
|
Fast-acting
insulin
secretagogues
(glinides) |
Promotion of more rapid
insulin secretion and
improvement of
postprandial
hyperglycemia |
Moderate |
Weight
gain |
Liver damage |
Type 1 diabetes, common
contraindications for oral
antidiabetic drugs* |
(1) Do not use with SU drugs |
|
Insulin
preparations |
(1) Basal insulin preparations
(long-acting dissolved insulin
preparations, intermediate-
acting insulin preparations)
(2) Additional insulin preparations
(rapid-acting insulin
preparations, rapid-acting
insulin preparations
(3) Mixed-type insulin
preparations that are a
mixture of ultra fast-acting
and intermediate-acting
insulins
(4) Combined solubilized insulin
preparations of ultra-fast-
acting and long-acting
dissolution |
Rapid-acting and fast-
acting insulins improve
postprandial
hyperglycemia, and long-
acting dissolving and
intermediate-acting
insulins improve fasting
hyperglycemia |
High |
Weight
gain |
Injection site
reactions
(redness, rash,
edema, and
subcutaneous
nodules, among
others) |
History of hypersensitivity
to the drug |
(1) Super fast-acting insulin
should be administered
immediately before meals
(2) Fast-acting insulin
preparations should be
administered 30 min before
meals |
|
If lifestyle changes, such as diet and exercise, are not effective in combination with 1 type of drug, the combined use of ≥2 types of drugs should be considered. Combinations of drugs with different mechanisms of action are considered effective, but the efficacy and safety of some drug combinations have not been established. For details, refer to the package insert of each drug.
*Common contraindications for oral antidiabetic drugs: severe ketosis, disturbed consciousness, severe infection, pre- and post-surgical states, severe trauma, severe liver dysfunction, pregnancy or potential pregnancy, history of hypersensitivity to the drug (taken from the Treatment Guide for Diabetes 2022–2023198).
eGFR, estimated glomerular filtration rate.
Metformin has been shown to suppress the development of CAD in individuals with obesity and type 2 DM.199 In addition, some sodium glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide 1 (GLP-1) receptor agonists have been reported as effective in suppressing cardiovascular events for primary and secondary prevention purposes.200–204 Evidence from some reports also suggests that α-glucosidase inhibitors205 and pioglitazone206,207 suppress cardiovascular events, but the evidence is insufficient at present. Conversely, DPP4 inhibitors (the most frequently used hypoglycemic drugs in Japan at the time of publication of this Guideline) have not been shown to suppress or promote cardiovascular events compared with placebo.208–211 With respect to insulin therapy in patients with IGT or early-onset DM, participants in the ORIGIN study did not show an increase or decrease in cardiovascular events in response to a long-acting dissolving insulin formulation compared with placebo.212
Considering improvement in total CVOs, including CAD, metformin, used in almost all of the recent large RCTs, is the first choice, followed by SGLT2 inhibitors200,201,213 and GLP-1 receptor agonists.202–204,214 Cost, frailty, and susceptibility to infection, among other factors, must be considered when selecting SGLT2 inhibitors. Although the cost and side effect profile of GLP-1 receptor agonists should also be considered in the similar manner, their use is preferred in patients with severe obesity.
4.2.3 Comprehensive Management of Risk Factors
In addition to glycemic control, BP and lipid interventions have been shown to be effective in preventing CAD.138,215–218 For example, in the Steno-2 study,50 patients with type 2 DM presenting with microalbuminuria received comprehensive and stronger management of glycemic control, lipids, and BP for an average of 7.8 years. The CVD risk showed a significant reduction of 53% (hazard ratio [HR] for CAD alone not reported). In the J-DOIT3 study conducted in Japan,51 a group with stricter control goals than in the Steno-2 study (intensive comprehensive treatment group) was compared with a group with conventional control goals. No reduction in CAD risk was observed, but a significant reduction was observed in the stroke incidence in the intensive comprehensive treatment group. From the perspective of CVD prevention, it is important to comprehensively achieve the management goals for existing risk factors.
4.2.4 Aspirin
The previous guideline (2011 edition) stated that “for the primary prevention of ischemic heart disease, the use of aspirin should be considered in patients with diabetes who also have coronary risk factors unless contraindicated”.219 However, in scientific evidence that has since been published, the efficacy of antiplatelet therapy with low-dose aspirin has been reported for secondary prevention,220 but its efficacy in primary prevention is unclear. JPAD, a primary prevention trial in Japanese patients with type 2 DM, reported a 20% reduction in the risk of cardiovascular events in the aspirin group, but the difference was not significant.221 In addition, 3 RCTs222–224 and a meta-analysis that included these RCTs225 examined the primary preventive effect of aspirin in patients with DM and did not report efficacy. In a recent report (ASCEND), in which the primary preventive effect of aspirin in patients with DM was examined, a significant reduction in cardiovascular events was observed in the aspirin group, but a significant increase was also observed in the bleeding risk.226
4.2.5 Summary of the Interventions for DM
Based on the above findings:
• Patients with microvascular complications (nephropathy, retinopathy, and potential peripheral neuropathy) are at high risk of CAD.
• Good glycemic control suppresses the occurrence of macrovascular events, such as MI, but treatment effects require ≥10 years to manifest. Glycemic control is recommended from the early stages of diagnosis and treatment.
• As a guide for selecting glucose-lowering agents, the Japan Diabetes Society’s Treatment Algorithm Consensus Statement for Type 2 Diabetes can be recommended (available Japanese version only, English version to be published).227 This algorithm facilitates the selection of an appropriate drug by considering each of the following steps in order: Step 1: disease state (obesity/non-obesity), Step 2: drug safety/side effect profile, Step 3: additional benefits of each agent, Step 4: patient background.
• The use of SGLT2 inhibitors and GLP-1 receptor agonists can be recommended for CAD high-risk patients, in particular patients with obesity.
• In addition to glycemic control, the comprehensive control of coronary artery risk factors, such as hypertension, dyslipidemia, and CKD, is important for improving prognosis.
• The routine use of antiplatelet agents for the primary prevention of CAD is not recommended.
4.3 Obesity and Metabolic Syndrome as Coronary Risk Factors
A 26-year observational study in the Framingham Heart Study demonstrated that obesity is a risk factor independent of other CAD risk factors, such as aging, smoking, dyslipidemia, hypertension, and DM.228 Observational studies of Japanese individuals also yielded similar results; compared to those with BMI of 23–24.9 kg/m2, the risk of CAD increases in a dose–response manner from BMI approximately ≥27 in both men and women.229
Obesity, especially the excessive accumulation of visceral fat, is associated with multiple CAD risk factors, such as increased BP, increased TGs, decreased HDL-C,230 and IGT,231 associated with insulin resistance. The overlap of CAD risk factors associated with the excess accumulation of visceral fat is defined as metabolic syndrome.231 The Hisayama study showed that metabolic syndrome increased the risk of CAD by 1.94-fold in men and 2.86-fold in women.232 Similarly, the Suita study also revealed a 1.5-fold increase in the risk of CAD in men and a 2.7-fold increase in women with metabolic syndrome.233
4.4 Therapeutic Interventions for Obesity and Metabolic Syndrome
Whether reducing obesity directly reduces the incidence of CAD has not been confirmed to date. However, that does not imply that obesity correction is ineffective in preventing CAD, but rather implies that it is difficult to maintain an appropriate body weight for a long period of time through lifestyle intervention alone.
For example, in the Look AHEAD trial,234 a long-term randomized controlled intervention study in the USA of individuals with type 2 DM, the researchers investigated whether the incidence of cardiovascular events and death could be reduced with a positive lifestyle intervention aimed at weight loss through energy intake restriction and exercise, compared with ordinary diabetes education and support. In that study, no statistically significant inhibitory effect on cardiovascular events was observed. However, with respect to the weight changes between the intervention and control groups, the weight loss from the beginning of the study till after 1 year was 8.6% in the intervention group and 0.7% in the control group, which was the largest difference between the groups. Following this trial, the intervention group showed a tendency to rebound (weight gain), whereas the control group continued to exhibit gradual weight loss. Consequently, the weight in the intervention group had decreased by 6.0%, and the control group had decreased by 3.5% at the end of the study (9.6 years later). However, long-term interventions aimed at weight loss were effective in improving the profile of CAD risk factors and reducing drug dosages and movement disorders. The usefulness of weight loss in patients with DM and obesity was also suggested. A 3-year observational study that compared Japanese specific health checkup active support participants with nonparticipants also reported improvements in body weight and metabolic factors in the participants with active support.235
Thus, the components of metabolic syndrome (dyslipidemia, hypertension, and hyperglycemia) are expected to improve with weight loss through lifestyle improvement in the longer term. In the Diabetes Preventive Program, a RCT for individuals with IGT in the USA, a lifestyle intervention targeting 7% weight loss achieved 5% weight loss, and as a result, significant inhibitory effects on DM and metabolic syndrome were observed.236,237 According to the Obesity Clinical Practice Guidelines 2016 of the Japan Society for the Study of Obesity, when weight loss of 1–3% occurs through active support for participants requiring specific health checkup guidance, improvement can be seen in the levels of TGs, LDL-C, HDL-C, HbA1c, and liver function. Further, significant improvements in SBP and DBP, fasting blood glucose levels, and uric acid levels were observed with 3–5% weight loss.238 Therefore, the goal of weight loss treatment for metabolic syndrome has been proposed as “reduce 3% or more from the current weight in 3 to 6 months”. A recent meta-analysis of weight loss in patients with type 2 DM and obesity showed that a 5% weight loss significantly improved the diabetes-related clinical indicators. The consensus report of the American Diabetes Association states that the current weight management goal for patients with diabetes is “5% reduction of current weight”.239 Although we do not have any evidence showing that intervention for obesity and metabolic syndrome directly reduces the incidence of CAD, it may contribute to the reduction of body weight and the improvement of obesity-related parameters.
5. Diet and Nutrition (Table 14)
Table 14.
Recommendations and Levels of Evidence for Diet and Nutrition for Primary Prevention of CAD
| |
COR |
LOE |
| To prevent CAD, maintain an adequate total energy intake and appropriate body weight |
I |
C |
| To prevent CAD, reduce salt intake |
I |
A |
| To prevent CAD, reduce saturated fatty acids and cholesterol intake |
I |
A |
| To prevent CAD, increase dietary fiber intake |
I |
A |
| To prevent CAD, consider consuming fish oil |
IIa |
B |
To prevent CAD, consider replacing saturated fatty acids with n-6 polyunsaturated fatty acids,
particularly linoleic acid |
IIa |
B |
| To prevent CAD, consider replacing saturated fatty acids with monounsaturated fatty acids |
IIb |
C |
| To prevent CAD, consider reducing the intake of processed foods containing fructose |
IIb |
C |
| To prevent CAD, consider increasing the intake of soybean and soy products |
IIb |
C |
| To prevent CAD, consider increasing the intake of nuts |
IIb |
C |
| To reduce the risk of health problems, reduce the intake of alcohol |
III (No
benefit) |
B |
| To prevent CAD, avoid the intake of trans fatty acids |
III
(Harm) |
B |
| To reduce the risk of health problems, avoid excessive intake of vitamins D, E, and C |
III
(Harm) |
B |
CAD, coronary artery disease; COR, class of recommendation; LOE, level of evidence.
Tips for a Healthier Diet
1) In general, the maintenance of a proper total energy intake and proper body weight, with a fat/total energy ratio of 20–25% and a carbohydrate/total energy ratio of 50–60%, is recommended.
2) The target salt intake should be less than 6 g/day.
3) Consume lean meat and avoid processed meat. Milk and dairy products contain SFAs and cholesterol, which raise the serum cholesterol level. However, these foods are beneficial for the intake of potassium, calcium, magnesium, and dairy protein. Therefore, low-fat and non-fat products are recommended for patients with hypertension and dyslipidemia. Butter, lard, and coconut oil are high in saturated fats; hence, one should be careful not to consume these in excess and avoid foods that contain these. We should aim that less than 7% of the total energy is derived from saturated fats.
4) A fish-based diet is recommended for the intake of n-3 PUFAs.
5) Limit the intake of processed foods, confectionery items using margarine, shortening, and fat spreads, and fried food, which contain high levels of trans fatty acids.
6) Chicken egg yolk contains high levels of cholesterol (approximately 220–240 mg/piece). Therefore, for patients with hyper-LDL-cholesterolemia or diabetes, it is desirable to consider limiting its intake (less than 200 mg/day), and even healthy individuals should refrain from excessive intake. Fish roe, fish with roe, small fish, and internal organs (liver and offal) also contain high levels of cholesterol and should not be consumed in excess.
7) Aim for a dietary fiber intake of 25 g/day or more. Among cereals, barley rice, brown rice, rice with 7/10 grains (polished germ), and millet grains are recommended over white rice, and whole grain bread is recommended over white bread, because the former contains more dietary fiber. Actively consume vegetables and fruits to prevent the onset of arteriosclerotic diseases.
8) Per recommendations, the intake of processed foods containing fructose should be reduced.
9) Consume seaweed, soybean, and soybean products, which are typical food items in the Japanese diet, and nuts, which are typical food items in the Mediterranean diet.
10) The intake of all vitamins from normal foods in appropriate quantities is desirable for reducing the risk of CVD and maintaining appropriate serum lipid levels.
11) To reduce the risk of health problems, such as CAD, cerebral hemorrhage, and cancer, it is desirable to reduce the alcohol intake to less than 25 g/day or as much as possible.
5.1 Total Energy Intake and Fat/Total Energy Ratio
Individuals who are overweight or are obese are at high risk for arteriosclerotic diseases, regardless of whether or not they have metabolic disorders.240–243 The risk for all-cause death reduces significantly with weight loss interventions.244 and physical activity and dietary intervention reduce BP, TC, LDL-C, and TG and increase HDL-C in individuals without glucose metabolism disorders.245 Therefore, maintaining an adequate total energy intake and an appropriate body weight are important for CAD prevention.
A carbohydrate/total energy ratio ranging from 50% to 55% is associated with the lowest risk of all-cause death. A low-carbohydrate or high-carbohydrate diet increases the risk of all-cause death.246 Even for individuals on a low-carbohydrate diet, a high intake of animal fat is associated with a higher risk of all-cause death, whereas a high intake of vegetable fat is associated with a lower risk.246 With respect to serum lipid levels, a low-fat diet reduces the TC and LDL-C levels, increases the TG levels, and decreases the HDL-C levels, in contrast to a high-fat diet.247 Therefore, setting a fat/total energy ratio of 20–25% and carbohydrate/total energy ratio of 50–60% under an appropriate total energy intake is recommended.
Setting an Energy Intake Goal
The target weight of an individual is calculated using the following formula, considering that the BMI with the lowest all-cause mortality varies by age248 and the definition of obesity.249
18–49 years old: [height (m)]2 × 18.5 − 24.9 kg/m2, 50–64 years old: [height (m)]2 × 20.0 − 24.9 kg/m2, 65–74 years old: [height (m)]2 × 21.5 − 24.9 kg/m2, 75 years and older: [height (m)]2 × 21.5 − 24.9 kg/m2. Optimize your total energy intake based on your target weight and daily activity level. The total energy intake (kcal/day) = target weight (kg) × level of physical activity (25–30 for light physical activity, 30–35 for moderate physical activity, 35 or greater for vigorous physical activity).248,250 However, in the elderly, appropriate judgment should be made based on the current body weight and evaluation of frailty, eating status, and metabolic status.248,250
5.2 Salt Intake
Increased salt intake increases BP,251,252 and low-salt dietary interventions significantly reduce SBP and DBP in hypertensive individuals and SBP in normotensive individuals.253 Findings from numerous clinical studies have shown that lowering BP reduces the risk of CAD and stroke.79,82 Although the relationship between salt intake and the risk of CVD and all-cause death may or may not be significant, depending on the study country, sex, and target population, no consistent conclusions have been reported.252,254,255 Studies of 24-h urinary sodium excretion have reported that higher sodium intake or excretion is associated in a dose-dependent manner with a higher risk of CVD incidence and all-cause death.256,257 In addition, when individual CVDs are considered, many reports indicate that the risk of stroke incidence and death increases with increasing salt intake.254,255,257 However, in CAD, the risk cannot be determined with the same certainty as in stroke.254,255,257–261
According to these findings, excessive intake of salt increases BP. Thus, not only high-risk patients but also healthy individuals should reduce their daily salt intake. If the individual also has comorbidities, such as hypertension and obesity, this is expected to prevent the development of CAD and stroke.
Based on the current situation in Japan, the target intake is <6 g/day.41 Of note, cohort studies and meta-analyses involving patients at a high risk of CVD have indicated a J-type or U-type relationship between salt intake and the risks of CVD and all-cause death, despite the difference in methods used to measure salt intake or excretion;256,257 thus, it is necessary to consider the individual pathophysiological condition when reducing salt intake.258,262 Conversely, especially in the elderly, excessive reduction of salt intake may lead to dehydration and lack of energy owing to decreased appetite, which may lead to undesirable weight loss and sarcopenia.39,41 Even when consuming low-salt foods, excessive intake of such food products will lead to salt overdose.
Tips for a Healthier Diet
Approximately 70% of the salt intake in Japanese people is from seasonings; thus, the addition of seasonings should be kept to a minimum. Salt-rich foods include pickled plums (umeboshi), pickles, miso soup, preserved foods such as dried seafood, fish paste products such as kamaboko, and processed meats (ham, bacon, sausage, and fried chicken). Therefore, avoid the consumption of these foods in combination. A useful method is to avoid drinking the soup in noodle dishes/oden.
5.3 Fatty Acids
Intake of SFAs increases serum TC and LDL-C levels, and reduction of SFA intake leads to decreases in serum TC and LDL-C levels. SFA restriction also reduces the risk of CVD.263 Additionally, replacing SFAs with PUFAs has reduced the risk for the incidence of CVD by 21%, but the effect of replacing SFAs with monounsaturated fatty acids (MUFAs) is unclear.263 SFA intake should be maintained at <7% of the total energy intake (7%E) to prevent CAD.
A meta-analysis of RCTs investigating the effects of n-3 PUFAs (including dietary or capsule formulations of fish oil or α-linolenic acids) on the risk of cardiovascular death or the incidence of CVD and CAD remains inconsistent.264–268 Furthermore, even in reports that showed a significant decrease in CAD incidence, the risk was only mildly suppressed (5–9%).266,268 Similarly, cohort studies in Europe and the USA have shown inconsistent results for the association of fish intake and risk for the incidence of CVD.269–277 However, in a cohort study of Japanese participants, the risk for the incidence of nonfatal CAD278 or death from CVD was reduced in groups with a high intake of fish and n-3 PUFAs.279,280 Meta-analyses of cohort studies showed a reduced risk for both CAD events281 and stroke.282 Therefore, even though the results of meta-analyses of RCTs and cohort studies are not necessarily concordant, fish oil intake may suppress CAD incidence. As for the serum lipid levels, increasing fish oil intake is effective for reducing the TG level.283 With respect to n-6 PUFAs, replacing SFAs with n-6 PUFAs, especially linoleic acid, may reduce the risk of CAD incidence or death.284 However, the effect of increasing the intake of n-6 PUFAs remains unclear. Replacing SFA of 9.6%E with the same energy ratio of n-6 PUFA resulted in significantly lower levels of TC and LDL-C in an RCT of subjects at moderate atherosclerotic disease risk.272 In another RCT, n-6 PUFA 19%E with corn oil lowered the levels of TC, LDL-C, and TG compared with the same energy-ratio of butter in dyslipidemic individuals.273 A meta-analysis of RCTs also showed a reduction in TC in the group of high n-6 PUFA intake.268
MUFAs are found in many foods, such as meat, fats, grains, and soybeans. Meta-analyses of RCTs and cohort studies have shown that replacing SFAs with MUFAs was not associated with a reduction in the risk for all-cause death, the incidence of CVD, MI and stroke, or death from CAD.263,285 However, in an analysis conducted in a US cohort study showed that the risk of all-cause death and CVD death decreased when SFAs were replaced with plant-derived MUFAs.284 Therefore, the intake of plant-based foods is desirable. With respect to serum lipid levels, a high-MUFA diet reduced the TC, LDL-C, and HDL-C levels to a greater extent than a high-SFA diet in patients with dyslipidemia.286–288 Another study showed that a MUFA intake >12%E exerted no significant effect on serum lipids compared with intake ≤12%E.289 Thus, increasing the MUFA intake may improve the serum lipid levels, but excessive intake will not exert the same effect. Compared to high SFA diet, a decrease in HDL-C level in high MUFA diet and high PUFA diet were reported.286–288 Nevertheless, the magnitudes of such decrease were small and no adverse effect from the decline was observed.
With respect to trans-fatty acids, a lack of consensus exists on whether naturally occurring trans fatty acids (beef, mutton, milk, and dairy products) should be treated in the same manner as industrially produced trans-fatty acids (during the hydrogenation and refining of fats and oils).290–294 However, in US cohort studies, trans-fatty acid intake was associated with an increased risk of all-cause and CVD deaths.284,295 A cross-sectional study in Japan showed that the serum concentrations of elaidic acid, an industrially derived trans-fatty acid, were high in patients with metabolic syndrome and young patients with CAD.296 Also, in Japanese patients with CAD, the serum concentration of elaidic acid was an independent risk factor for unstable plaques.297
Trans-fatty acids increase the LDL-C levels,290,298–301 and the level of Lp(a), a lipoprotein that promotes atherosclerosis,299,302,303 and decrease the HDL-C levels.290,291,302 Therefore, we should refrain from consuming trans-fatty acids to prevent CAD.
Tips for a Healthier Diet
1) Red meat/processed meat
The largest source of SFA among Japanese people are through meat. Meta-analysis of cohort studies has shown that increase in the amount of meat (beef, pork etc.) and processed meat (bacon, sausage etc.) intake has been associated with increased risk in all-cause mortality, coronary heart disease, stroke and heart failure risk.304,305 With respect to serum lipid levels, not only red meat and processed meat but also poultry with skin can include high quantity of SFA that can cause high level of LDL-C. Thus, consumption of non-fatty meat, and avoidance of meat with skin and processed meat is recommended.
2) Dairy products
Dairy products contain high quantity of SFAs306,307 and raises LDL-C.308–314 In contrast, low-fat milk, skimmed milk, or powdered milk can help normalize blood cholesterol.315–317 In addition, potassium, calcium, and magnesium in milk can help lower BP.307,318 Milk proteins also are beneficial for healthy nutrition. Thus, low-fat milk is recommended to reduce total energy and SFAs and by increasing amount of potassium, calcium and magnesium.
3) Fish consumption is recommended. Fish roe, baby fish and small fish are high in cholesterol and should not be consumed in excess.
4) Butter, lard, and coconut oil contains high level of SFAs, thus, avoiding excessive intake of these and foods using these materials is recommended.
5) Trans fatty acids
Trans fatty acids raise LDL-C and are found in processed foods such as margarine, shortening, fast spread-based confectionery and fried foods, and thus avoiding these processed foods is recommended.
5.4 Cholesterol
In cohort studies conducted in the late 1990s, the relationship between cholesterol intake and the risk for CAD incidence or all-cause death was inconsistent.319–322 However, a recent meta-analysis of US cohort studies showed that increased cholesterol or egg intake was dose-dependently associated with an increased risk of CVD and all-cause death.323 A meta-analysis of data from other major studies also showed a significant dose-dependent relationship between egg intake and the incidence of CVD.324
Many studies have been conducted on the effects of dietary cholesterol on serum lipids. A meta-analysis of 55 RCTs with restricted cholesterol intake showed that an increased cholesterol intake increased the LDL-C levels of participants.325 An RCT comparing a high-cholesterol diet (600 mg/day) with a low-cholesterol diet (200 mg/day) showed that the high-cholesterol diet significantly increased the LDL-C levels compared with the low-cholesterol diet.326 Similarly, in a meta-analysis that showed increases in the TC, LDL-C, and HDL-C levels with increased cholesterol intake, when the control group had a cholesterol intake ≤200 mg/day, a significant increase was observed in the LDL-C levels in the group with higher cholesterol intake.327
Based on these findings, in patients with high LDL-C, cholesterol intake should be maintained at <200 mg/day to lower the LDL-C. Notably, increased cholesterol intake leads to increased LDL-C even in individuals without high LDL-C. Although evidence for aiming at a specific target cholesterol intake is not sufficient, it is desirable to maintain a low level of cholesterol intake.
Tips for a Healthier Diet
1) Chicken eggs
The dietary sources of cholesterol for Japanese people are eggs (50.1%), meat (20.5%), and seafood (18.1%).328 Cholesterol-containing foods often also contain SFAs (meat also often contains SFAs; chicken eggs and shrimp have more cholesterol than SFAs), and the cholesterol absorption rates vary considerably between individuals. Cholesterol is synthesized throughout the body, and although its synthesis in the liver accounts for approximately 10% of the total synthesized quantity, liver regulates approximately 70% of serum lipoproteins. For these reasons, the effects of cholesterol intake on serum lipids are complex and vary between individuals (hyper-responder, hypo-responder).329,330 In a meta-analysis of chicken egg intake, the TC, LDL-C, and HDL-C levels increased with egg yolk intake.331 In a meta-analysis of hyper- and hypo-responders, egg intake significantly increased the LDL-C levels in hyper-responders, but not in hypo-responders.332 Meanwhile, cohort studies and meta-analyses have shown that for patients with diabetes, the incidence of CVD, especially CAD, or death increases in the group with a high consumption of chicken eggs.333–337 Therefore, patients with high LDL-C or diabetes should limit egg intake. Even healthy individuals should refrain from overconsumption since LDL-C levels can increase due to increase in cholesterol intake.
2) Fish roe, fish with eggs, small fish, and internal organs (liver and offal) contain high levels of cholesterol; thus, the excess intake of these products should be avoided.
3) Chicken thighs (meat) have higher cholesterol content than chicken breasts (meat). Eating chicken meat with its skin should be avoided.
5.5 Dietary Fiber
Dietary fiber is contained in grains, vegetables, fruits, seaweed, and other food products, and is classified as soluble or insoluble. Because dietary fiber can prolong the retention time of food in the stomach, it can prevent a rapid elevation in blood glucose and TG levels, and help maintain satiety, which can help prevent overeating. It may also promote defecation and bile acid synthesis, and suppress cholesterol absorption.338,339 In a Japanese cohort study, the intake of soluble, insoluble, and total dietary fiber was inversely associated with the risk of CVD deaths in men and in women.340 In addition, a meta-analysis of cohort studies, including those conducted overseas, showed a reduced risk of all-cause death,341–344 CVD death,342–345 and incidence of CVD,344,346 CAD,344,346 and stroke344,347–349 with dietary fiber intake. With respect to the effect on serum lipid levels, meta-analyses of many RCTs in which total and soluble dietary fiber were used showed that the TC,344,350–352 LDL-C344,350–354 and non-HDL-C levels353,354 decreased, but the HDL-C and TG levels were unaffected.350–352 Therefore, dietary fiber intake is effective in improving serum lipid levels. In general, a fiber intake ≥25 g/day is recommended to prevent the aggravation of lifestyle-related diseases.248,344
Tips for a Healthier Diet
1) Grains
Grains are the staple food in many regions of the world, the most being rice, wheat, corn, and potatoes, among others, and all are mainly composed of carbohydrates. The type of grains that benefit human health the most is unclear. Unrefined whole grains suppress all-cause mortality,355–358 CVD deaths,355–358 and the incidence of CAD,355,359 and CVD.355,360 No large-scale study has been conducted on the effects of brown rice on the development of arteriosclerotic disease, and the effects on serum lipids have been inconsistent.361,362 Conversely, the intake of barley and oats, which are rich in water-soluble dietary fiber, improves serum lipid levels.363–365 In a meta-analysis of cohort studies, buckwheat intake was associated with lower levels of blood glucose, TC, and TG.366
The glycemic index and glycemic load affect the postprandial blood glucose levels. However, their association with all-cause death, CVD incidence, and associated risk factors is inconsistent, and clear results have not been reported.367
2) Fruits and vegetables
Meta-analyses of cohort studies in Europe, the USA, and Japan have shown that the intake of vegetables or fruits, or their combination, reduces the risk of all-cause death, CAD, stroke, or type 2 DM in a dose-dependent manner.368–377 Vegetables and fruits should be consumed in adequate quantities to prevent atherosclerotic disease. However, considering the possibility of an increase in the levels of TG and uric acid (fructose utilizes ATP during phosphorylation and leads to excessive purine synthesis),378 excessive intake of fruits should be avoided. In addition, it is necessary to pay attention to the increase in salt intake with consumption of pickles.379,380 With respect to fruits, the consumption of canned foods has been reported to increase both all-cause and CVD deaths;355,363 hence, it is more desirable to consume fresh fruits.
3) Seaweed
Seaweed contains dietary fiber, vitamins, and minerals and is habitually consumed as part of the Japanese diet, which reduces the risk of all-cause and CVD deaths.381–384 Individuals who eat seaweed almost every day have a lower risk of developing ischemic heart disease (24% less for men and 44% less for women) than individuals who eat lesser quantities of seaweed; however, no relationship has been observed between seaweed intake and stroke risk (cohort study of Japanese participants).385 Conversely, no significant reduction was observed in the risk of CAD deaths386 or incidence.387 These studies were observational, and the conclusion is that seaweed consumption may reduce the incidence and deaths of CAD and cerebrovascular diseases; however, the results are inconsistent. In addition, seaweed contains iodine at high concentrations, and some types of seaweed contain high levels of arsenic, so excessive seaweed consumption is best avoided.
5.6 Processed Foods Containing Fructose
High intake of processed foods containing fructose (including sugar) may increase the risk of CAD owing to excessive energy intake, obesity, elevated TG levels, exacerbation of insulin resistance, and development of type 2 diabetes. Evidence from cohort studies and meta-analyses of studies in Europe and the USA has shown that the higher the intake of sugary drinks, the higher is the risk of all-cause death, CVD, CAD, stroke, weight gain, hypertension, and type 2 diabetes. However, the research results are not always consistent.388–395 An intervention study in which fructose was added to the control diet (increased total energy intake) increased the TG levels.396 An increase in postprandial TG levels has also been observed with additional fructose intake.397 Subgroup analyses of RCTs and non-RCTs exploring dose–response showed that fructose intake ≥50 g/day, and ≥100 g/day resulted in significantly higher levels of postprandial, and fasting TG, respectively.398 Therefore, lowering the intake of fructose-containing processed foods should decrease the TG level. Therefore, TG reduction can be enabled by reducing the intake of processed foods containing fructose. Considering the potential effects on CAD, the reduction of fructose intake is recommended.
5.7 Soybean and Soybean Products
Soybean and soybean products are commonly consumed by the Japanese people, but meta-analyses of cohort studies conducted in Japan and overseas have not yielded consistent results on the relationship between the intake of soy products and atherosclerotic diseases.399–401 Conversely, evidence from Japanese cohort studies shows that a high intake of soybean and soybean products is associated with reduced risk of stroke.402,403 Meta-analyses and systematic reviews of RCTs have been conducted on atherosclerotic disease risk factors for dietary soybean, soybean products, soy protein, and isoflavones. Among these, TC or LDL-C reduction was observed in some cases,404–406 but not in others.407,408 Soy and soy product intake may thus be associated with a reduction in CAD and stroke incidence.
5.8 Nuts
Nuts are one of the important components of the Mediterranean, DASH, and vegetarian diets, and include almonds, hazelnuts, walnuts, pistachios, cashews, macadamia nuts, and peanuts. Numerous observational studies have reported the association between higher nutrient consumption of nuts and reduced CVD risk.409–417 A meta-analysis of data from cohort studies in which the association among nut intake, CVD, and CAD was studied showed that individuals who consumed nuts had lower risk of the incidence of CVD, death from CVD, CAD incidence, and CAD death: 15%, 23%, 18%, and 24%, respectively.418 Also, reportedly, the intake of nuts reduces the levels of TC, LDL-C, and non-HDL-C.419–424 Thus, the consumption of nuts may be useful in preventing the onset of arteriosclerotic disease; however, evidence from studies conducted in Japan is insufficient.
5.9 Vitamins
Vitamin D,425–439 vitamin E,440–443 and vitamin C443–446 should be adequately absorbed from regular food products. For vitamin D, maintaining an appropriate blood 25(OH)D concentration is desirable for reducing the risk of CVD death or incidence and for maintaining appropriate BP. However, research results on the effects of vitamin supplements are inconsistent.446–464 Rather, the following have been reported: an increased risk of stroke when vitamin D is combined with calcium,465 heart failure with vitamin E monotherapy,466 and significantly increased cardiovascular mortality in postmenopausal patients with diabetes who underwent vitamin C monotherapy.467 In addition, combined intervention with vitamins E and C increased the risk of all-cause death in postmenopausal patients with CAD,468 and vitamin E intervention significantly increased the risk of hemorrhagic stroke.469,470 Therefore, the aggressive use of vitamin supplements is not recommended, considering their efficacy and safety. In addition to the above, the excessive intake of vitamin A and β-carotene can cause health problems and is generally not recommended.471 Care should be taken to ensure that other supplements are consumed appropriately.
5.10 Alcohol
Heavy alcohol consumption (≈46–60 g/day or more) is a risk factor for CAD and stroke. On the other hand, light-to-moderate alcohol consumption was thought to reduce the risk of CVD (i.e., forms a J curve).472–483 However, it has been also reported that this suppressive effect diminished when participants had multiple complications.483 In addition, meta-analyses of cohort studies and case–control studies have shown that binge drinking also increases the risk of CAD.484
However, in a recent meta-analysis limited to high-quality cohort studies, the protective effect of low-dose alcohol consumption on all-cause mortality risk diminished,485 and the reduction in CAD death was not observed in young individuals aged ≤55 years.486
A Mendelian randomization meta-analysis of studies with a European population of 261,991 people showed that the lower the amount of alcohol consumption, the lower the risk of CAD, indicating the negative results for the J-curve phenomenon.487 Another Mendelian randomization analysis in China and South Asia showed no significant dose–response relationship between alcohol consumption and the risk of CAD, although a monotonic association was reported between alcohol consumption and the risk of stroke, and each of cerebral infarction and cerebral hemorrhage.488 A study integrating data from 195 countries and regions found that the level of alcohol consumption that minimized all alcohol-related health disorders, including CAD (including all-cause death and carcinogenesis489), was zero drink, and health disorders rose with an increase in the amount of alcohol consumption, although the risk of CAD increased from more than approximately 10 g/day of pure alcohol intake.490
Thus, considering that heavy drinking is a risk factor for CAD, the CAD-suppressing effect of low-dose drinking is unclear and alcohol consumption is associated with health risks such as increased cerebral hemorrhage and carcinogenesis, alcohol consumption should be maintained at ≤25 g/day39 or should be reduced as much as possible.
Tips for a Healthier Diet
Pure alcohol is calculated by amount of alcohol drunk (mL) × [alcohol content (%) / 100 ] × 0.8
For example
1 large bottle of beer (633 mL)
Approximately 180 mL of sake (1-go)
0.7 go of shochu (when drinking with hot water or water with shochu 6: water 4 ratio)
Approximately 250 mL of wine
6. Exercise and Physical Activity (Table 15)
Table 15.
Recommendations and Levels of Evidence for Exercise and Physical Activity
| |
COR |
LOE |
To prevent coronary artery disease, aerobic exercise (of moderate* or high intensity)
should be performed daily for ≥30 min (at least 3 days/week) |
I |
B |
To lower the risk of coronary artery disease, it is recommended to reduce sedentary behavior,
even for those who exercise regularly |
IIa |
C |
*Guidelines for moderate exercise are as follows.
• Exercise intensity equivalent to that of normal walking
• In terms of METs (a unit of physical activity that indicates how many times the resting metabolism should be increased for performing an exercise), moderate-intensity exercise (walking) generally requires 3 METs, although the requirement varies depending on the physical strength of each individual
• In terms of the subjective exercise intensity during exercise, the intensity is equivalent to a Borg index of 11–13 (easy to slightly hard)
COR, class of recommendation; LOE, level of evidence.
6.1 Efficacy of Exercise and Physical Activity as Preventive Measures
Many observational studies have shown that “active or regular physical activity in daily life or occupation prevents the incidence of coronary artery disease and reduces mortality”.491–493 Regular exercise and physical activity reduce risk factors such as hypertension, diabetes, obesity, and dyslipidemia and reduce the incidence of or death from CAD. The effectiveness of exercise therapy for the primary and secondary prevention of CAD has been established.44,219 Because physical activity is an intervening factor, all patients or subjects should be evaluated for exercise/physical activity and advised to exercise regularly/increase their physical activity. “Physical activity” is defined as any physical movement accompanied by the contraction of skeletal muscle that causes energy consumption and includes not only exercise but also lifestyle-related activities such as physical work and movement. The Ministry of Health, Labour and Welfare also states that physical activity = lifestyle activities + exercise.494
6.2 Epidemiology of Physical Inactivity
According to the National Health and Nutrition Survey, Japan (2017), 35.9% of men and 28.6% of women have a habit of exercising for ≥30 min/day at least twice per week in continuity for ≥1 year. No significant increase or decrease in this value has been observed in the past 10 years.495 The average number of steps is 6,846/day for men and 5,868/day for women and this has decreased by 500–1,000 steps/day over the past 10 years.495,496 Japan has the highest percentage of people without an exercise habit in East Asia.497 The Ministry of Health, Labour and Welfare recommends 23 MET-hours/week (equivalent to 8,000–10,000 steps/day) as a physical activity standard for health promotion. However, >50% of adults do not follow this recommendation.494
6.3 Risks of Physical Inactivity
In addition to inadequate exercise habits, physical inactivity in daily life is a risk factor for CAD. After smoking and hypertension, physical inactivity is the largest risk factor for death from noncommunicable diseases in Japanese individuals.498 In Japan, physical inactivity is estimated to have a population contribution risk ratio of 10% for CAD. In other words, a 10% reduction in CAD can be expected in the absence of inactivity in adults.499
In addition to decreased physical activity, increased sitting time (defined as all awake behavior with energy expenditure ≤1.5 METs in a seated or supine position) is a risk factor for CAD.500 Reportedly, long durations of sitting at work leads to CVD and contributes to an increase in total deaths.501,502 Additionally, the longer a person watches television, the higher is their mortality rate from CVD and CAD.503 Even with exercise, an individual will be unable to perform sufficient activity if they spend a substantial duration of the day sitting (when not exercising). Thus, it is important to not only increase total exercise time but also reduce the total inactivity time such as sitting.
6.4 Effects of Physical Activity on Atherosclerotic Disease and CAD
There is no high-quality RCT that has provided substantial evidence on the primary prevention of CAD through exercise. However, based on findings from large-scale observational studies, an increase in exercise and a decrease in the duration of inactivity are associated with a lower incidence of CVD, including CAD, and lower total deaths. Therefore, exercise is expected to suppress CAD.491–493 According to the findings from a systematic review of cohort studies that evaluated the association between physical activity, including aerobic exercise and lifestyle activities, and atherosclerosis, CAD and CVD deaths, and total deaths were shown to be significantly lower in the high physical activity group than in the inactive group.493,504 The effect was also observed with low-intensity (1.6–2.9 METs) physical activity, such as housework and walking at work.505,506 Therefore, any increase in physical activity, including aerobic exercise, may effectively suppress the incidence of atherosclerotic disease, including CAD, and improve life expectancy.
6.5 Potential Effects of Exercise
Exercise therapy has been shown to improve classic coronary risk factors through the following effects.
• Antihypertensive Effect: Aerobic exercise exerts an antihypertensive effect. In a meta-analysis, moderate- to high-intensity aerobic exercise performed for an average of 40 min/day, 3–4 times/week for at least 12 weeks lowered the SBP and DBP of individuals by 2–5 mmHg and 1–4 mmHg, respectively, regardless of the presence or absence of hypertension.41,507
• Glucose Metabolism: Exercise therapy improves glycemic control and obesity, visceral fat accumulation, and insulin resistance in patients with type 2 diabetes. A meta-analysis reported that HbA1c was reduced by 0.66% in patients with type 2 diabetes when they performed aerobic and resistance exercises at an average of 3.4 times/week for ≥8 weeks (18 weeks on an average).508
• Lipids: Exercise therapy improves the lipid profile of individuals. In a meta-analysis comparing the effects of moderate (3–5.9 METs/day) aerobic exercise and non-exercise for 10–96 weeks in healthy adults without CAD, exercise therapy increased the HDL-C level by 10 mg/dL.509 In a meta-analysis of healthy East Asian adults, aerobic exercise decreased the TC and TG levels and increased the HDL-C level (TC −5.8 mg/dL, TG −13.7 mg/dL, and HDL-C +2.2 mg/dL).510 In addition, if we only included studies in which participants exercised for ≥150 min/week, the LDL-C level was also found to decrease (−8.9 mg/dL).510
Based on these results, the following processes are believed to occur. Increased physical activity and habitual aerobic exercise increase energy expenditure, and the body uses visceral fat and subcutaneous fat as energy sources. As a result, the abdominal circumference and weight of the individual are reduced. Additionally, by improving insulin resistance in skeletal muscles, metabolic syndrome-related factors are improved.494,511,512
In addition to typical risk factors, the secretion from blood mononuclear cells of tumor necrosis factor-α and interferon-γ, which induce atherosclerosis, and the levels of blood C-reactive protein (CRP) were found to reduce in response to continued moderate exercise for >6 months.513 Reportedly, the incidence of cardiovascular events can be reduced by suppressing inflammation.514 Therefore, although it may not improve the classical cardiovascular risk factors, habitual exercise may prevent CAD by suppressing atherosclerosis.
6.6 Types of Exercise
Exercise can be classified as aerobic or resistance. Aerobic exercise refers to the rhythmic movement of large muscles over a period and includes walking, running, swimming, and cycling. Resistance exercise refers to any exercise in which movements are repeated under load, such as strength training. Aerobic exercise can improve cardiopulmonary function and the endurance of the entire body, and resistance exercise can increase muscle strength, muscular endurance, and muscle mass. Ideally, both types of exercises should be performed. For the prevention of lifestyle-related diseases and treatment of hypertension, dyslipidemia, glucose metabolism disorders, and obesity, aerobic exercise is recommended based on its efficacy and safety.41
6.7 Aerobic Exercise
Moderate-intensity aerobic exercise (requiring 40–60% of maximal oxygen uptake) is recommended from a risk and effectiveness perspective (Table 15). In primary prevention, only a few opportunities are available to measure the maximal oxygen uptake; hence, as a general index, exercise with a Borg index of ≈11–13 (easy to slightly hard) based on subjective symptoms is recommended (Table 16).44,515 As specific exercises, walking, slow jogging, cycling, and underwater exercise, among others, are recommended (Figure 6).
Table 16.
Borg Index and Subjective Exercise Intensity
| Index |
Subjective exercise
intensity |
Exercise intensity |
| 20 |
Absolute limit |
100 |
| 19 |
Extremely hard |
95 |
| 18 |
|
|
| 17 |
Very hard |
85 |
| 16 |
|
|
| 15 |
Hard |
70 |
| 14 |
|
|
| 13 |
Slightly hard |
55 (corresponds to AT) |
| 12 |
|
|
| 11 |
Easy |
40 |
| 10 |
|
|
| 9 |
Very easy |
20 |
| 8 |
|
|
| 7 |
Extremely easy |
5 |
| 6 |
|
|
AT, anaerobic threshold. Oxygen intake immediately before anaerobic metabolism is considered as aerobic metabolism. Exercise at levels less than the AT is considered as aerobic exercise. Acidosis progresses and catecholamine secretion increases in physical activity in which the AT is exceeded.
(Adapted from Araki E, et al. Directors of the JCS and JDS. 2020.515)
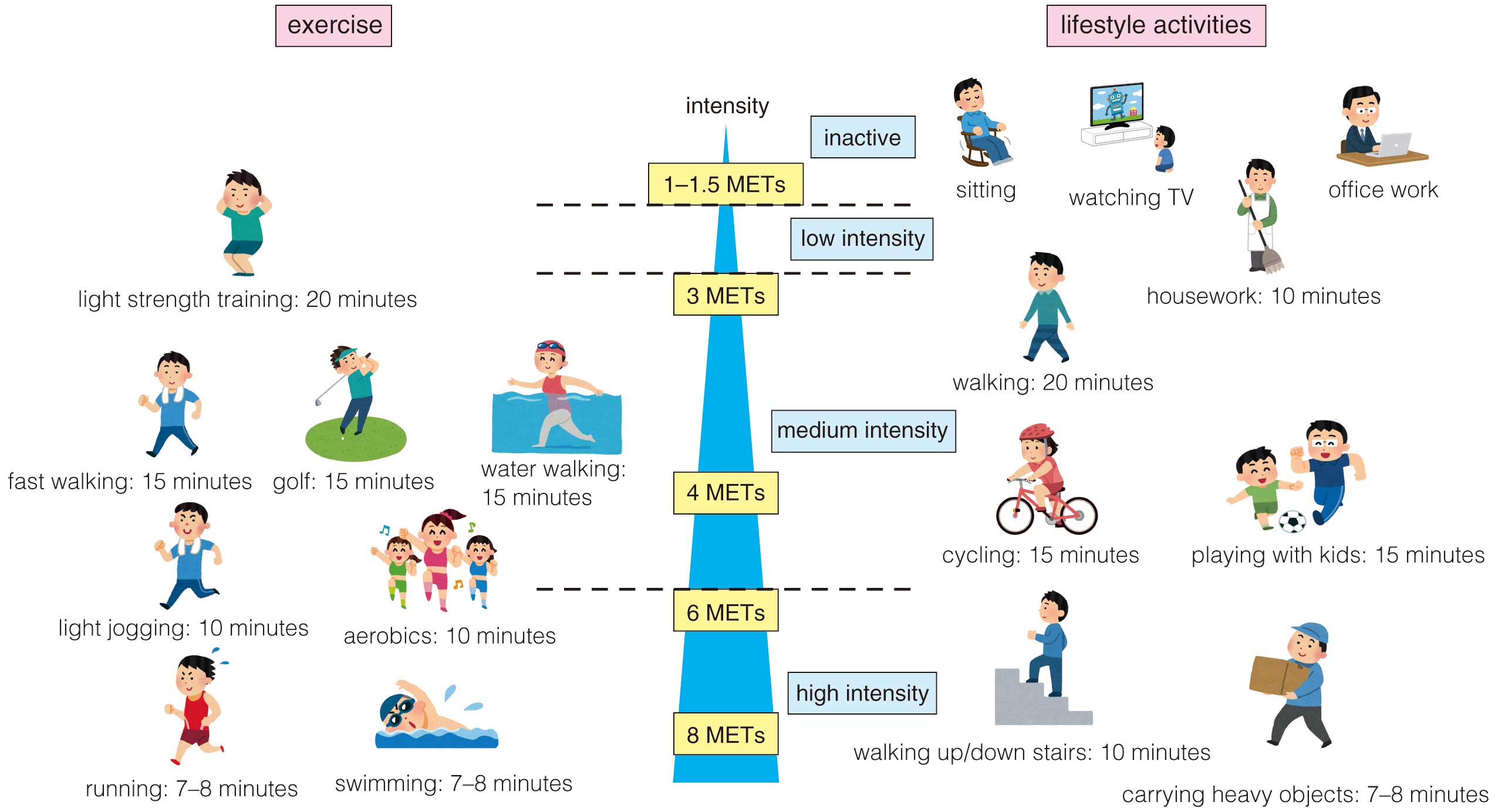
The goal is to perform moderate- or high-intensity aerobic exercise (requiring ≥3 METs) for ≥30 min/day, three times or more per week (daily if possible), or ≥150 min/week.44 Additionally, young people and patients with high cardiopulmonary function may achieve the same effect at a higher exercise intensity (75 min/week).22 Furthermore, even when individuals cannot perform moderate- or high-intensity exercise, low-intensity physical activity at home and at work is considered effective in preventing CAD, as compared with no physical activity. Therefore, low-intensity physical activity is also recommended.22,505,506
6.8 Resistance Exercise
Different studies have reported varying views on resistance exercise. Limited evidence is available from such studies in Japan, and no specific implementation method has been established. However, in the case of older people with reduced muscle strength and mass, resistance exercise is useful for improving stamina/muscle strength and the risk factors of atherosclerosis. In most cases, for a given exercise, a suitable form of resistance exercise involves performing the maximum number of repetitions possible (≈12 on average) at a weight that is 50–85% (≈70% on average) of the weight at which the individual can only perform 1 repetition (the 1-repetition max., i.e., the weight at which the exercise can be performed only once). A rest period of 1–2 min is provided between the sets. Initially, 1 set of 1 exercise is performed, and subsequently, the number of sets is gradually increased to 5 (≈3 sets per exercise). Ultimately, 6–7 exercises targeting both the upper- and lower-body muscles are to be performed for 2–3 times/week on nonconsecutive days.22,44
6.9 Reducing Sedentary Time
In addition to exercise therapy, to reduce the time spent sitting/lying down, individuals are recommended to frequently get up for walks and to intersperse long stretches of uninterrupted seated/supine time with physical activity (Table 15).44
6.10 Individualized Exercise Therapy
Exercise therapy should not be recommended uniformly across age groups; rather, it should be prescribed and instructed according to the physical fitness (endurance and muscular strength), health complications, lifestyle, and other characteristics of each individual. Walking is the most common form of aerobic exercise. In the beginning, exercise should be “easy” to “moderately easy”. The goal is to increase the intensity to “moderately difficult” once the individual gets accustomed to exercising.
In 2013, the Ministry of Health, Labour and Welfare formulated physical activity standards and guidelines (Activity Guidelines) for health promotion as measures against lifestyle-related diseases. To prevent lifestyle-related diseases, individuals should begin with “PLUS-TEN”, an effort to add 10 min of exercise time to their current daily habits. The goal is to include an active time of 60 min/day for adults and ≥40 min/day for older individuals. For those without exercise habits, PLUS-TEN is an effective way to increase activity.494 To prevent injury, it is important to warm up for the first 5 min of exercise and to cool down for the last 5 min to gradually increase or to decrease the load placed on the body.515
6.11 Risks of Exercise and Medical Evaluations Necessary Before Initiation
Before exercise (therapy) is initiated, the patient’s health complications should be evaluated, physical condition, including orthopedic diseases, should be monitored, and the need for exercise restriction should be considered. Screening for CVD is generally not necessary if the patient is asymptomatic and exercises moderately. Before high-intensity exercise is recommended, patients with high cardiovascular risk and older people should undergo screening with their attending physician and, if necessary, an exercise stress test.
• With respect to hypertension, patients with grade III hypertension per the definition in “Hypertension Treatment Guidelines 2019” should exercise after undergoing antihypertensive therapy. Exercise (therapy) is indicated in patients with hypertension ≤grade II and no cerebrocardiovascular disease. In patients with hypertension, BP increases considerably during high-intensity exercise. Even after exercise, the risk of endogenous vasopressor system activation remains. Therefore, for safety, moderate exercise is recommended.41
• With respect to diabetes, in patients with proliferative retinopathy or more serious conditions, activities that cause physical impact, such as jumping, those that involve lowering of the head, and those in which the individuals need to hold their breath should be avoided. Patients with autonomic neuropathy are said to experience multiple exercise-induced adverse events owing to various factors, such as a decreased circulatory response to exercise load, orthostatic hypotension, thermoregulatory disorders, and visual impairment.515 Because cardiovascular autonomic neuropathy is an independent risk factor for cardiovascular death and asymptomatic MI, its degree determines the feasibility of exercise (therapy) in patients.515
• If the patient has bone or joint disease, exercises that are appropriate for such physical conditions, such as flexibility or resistance exercises, of the diseased joint should be performed with the supervision of orthopedic specialists to avoid overload. Unfamiliar exercises can put such individuals at risk of musculoskeletal impairment and lead to the development of orthopedic diseases.
Patients at a high risk of atherosclerosis may have heart disease, such as asymptomatic myocardial ischemia, which may lead to sudden death or MI.44 However, the risk does not compromise the benefits of exercise; hence, individualized exercise is recommended for all patients.
7. CAD Risk in Behavioral and Environmental Factors, Public Awareness and Patient Education
This section introduces the relationship among behavioral factors (e.g., smoking and oral hygiene), environmental factors (e.g., seasonal/temperature changes and air pollution) and CAD. In addition, we will discuss findings related to public awareness and patient education for managing the symptom development of CAD and the recent evidence on hyperuricemia management for CAD prevention.
In addition to the CAD risk factors mentioned above, several other factors have been identified as contributing to CVD, including sleep disorders such as sleep apnea, psychiatric disorders, and socioeconomic factors. Effective management of these disorders in accordance with clinical guidelines, as well as collaboration with specialists, can improve the prognosis of CAD.21 It is important to recognize that these risk factors, as well as socioeconomic factors, are interconnected with traditional CAD risk factors.22 Hence, it is crucial to address them concurrently with the management of other traditional risk factors for optimal outcomes.
7.1 Behavioral Factors and CAD
7.1.1 Smoking and CAD (Table 17)516
Table 17.
Recommendations and Levels of Evidence for Smoking Cessation on Primary Prevention of CAD
| |
COR |
LOE |
Conduct screenings at the outpatient department and hospital reception and provide
guidance for smoking cessation for smokers and smoking prevention for non-smokers |
I |
A |
Novel tobacco products should be screened in the same way as conventional cigarettes,
and information and guidance should be provided for smoking cessation and prevention |
I |
C |
See Standard procedure for smoking cessation treatment version 8.1.516 CAD, coronary artery disease; COR, class of recommendation; LOE, level of evidence.
a. Firsthand Smoking
Smoking is a major risk factor for CAD, and reportedly, in Japan, smoking increases the risk of CAD development.517 Observational studies conducted in Japan have also shown a dose-dependent relationship in which the risk of CAD increases with the number of cigarettes smoked per day.518 Furthermore, findings from a meta-analysis showed that smoking even 1 cigarette/day was associated with a 1.65-fold increase in CAD risk relative to that in nonsmokers.519
b. Smoking Cessation and Weight Gain
Studies have shown that maintaining complete smoking cessation can result in a reduction of 40–50% in the risk of CAD within the first 5 years or so compared with those who continue smoking.518,520 Conversely, there has been rising concern regarding the fact that weight gain after smoking cessation is a commonly observed phenomenon that may offset the beneficial effects of smoking cessation. A prospective cohort study on 69,910 Japanese men and women aged 45–74 years was conducted to address this topic. Assuming the CAD risk of continuous smokers to be 1, the risk of CAD incidence among individuals who quit during the 5-year follow-up period was found to have decreased to 0.58 in the 0.1–5.0 kg weight gain group and 0.51 in the no weight gain group.521 A Korean study reported a significant reduction in the HR for the incidence of MI even in the group with weight gain ≥4 kg after quitting smoking.522 Thus, weight gain after smoking cessation is unlikely to negate the cardiovascular protective effects of smoking cessation.
Furthermore, in recent years, health insurance coverage for smoking cessation treatment has been expanded to include the following measures: (1) removal of restrictions on health insurance treatment based on the age and lifetime smoking volume (Brinkman index), (2) lifting the ban for online therapy, and (3) application of these measures to users of heated tobacco products. Therefore, the use of behavioral and drug therapies to support smoking cessation is recommended.
c. Secondhand Smoking
Evidence from multiple reports suggests that secondhand smoking increases the risk of CAD.523,524 In a study conducted in the USA, 32,046 nonsmoking women aged 36–61 years were studied for 10 years, and the risk of nonfatal and fatal CAD development relative to that in women unexposed to tobacco smoke was 1.58 in the intermittent secondhand smoking group and 1.91 in the constant secondhand smoking group.525 A meta-analysis of data collected from East Asians, including Chinese individuals, also reported that exposure to secondhand smoke significantly increased the risk of CAD (RR: 1.23).526
d. Effectiveness of Legislative Measures to Prevent Secondhand Smoking
A meta-analysis of studies reported that hospitalizations due to CAD events significantly reduced after the enacting of secondhand smoking control laws (RR: 0.85). Furthermore, hospitalizations due to CAD events declined to a greater extent with higher degree of comprehensiveness of the smoking ban law (i.e., the number of places imposing smoking bans).527
In addition, hospitalizations for ACS in 9 Scottish hospitals decreased by 17% after enacting a smoking cessation law. The reduction was greater among nonsmokers: 14% for smokers, 19% for former smokers, and 21% for nonsmokers. Reportedly, the duration of exposure (per week) of nonsmokers to secondhand smoke and serum biomarkers of nicotine exposure significantly decreased after the law was enacted.528
These findings suggest that improving the social environment by various laws on secondhand smoking contributes to a reduction of CAD risk in the entire population.
e. Novel Tobacco Products
Novel tobacco products are categorized as shown in Table 18.39 Heated tobacco products involve the heating of tobacco leaves to produce aerosolized compounds that the user inhales. Because the quantity of nicotine present in the aerosols generated by these products and the blood-nicotine dynamics after inhalation are similar to those of cigarettes,529 a rising concern is that the use of these products may lead to nicotine dependence.530 These products also contribute to secondhand smoke.531 Heated tobacco products may not pose as high a CVD risk as conventional tobacco products, according to the findings of a systematic review; however, nonsmokers who begin using heated tobacco products may be at an increased risk of developing CVD.532,533 In animal experiments, heated tobacco products were shown to impair vascular endothelial function to the same extent as traditional cigarettes,534 which gives rise to concerns about the role of heated tobacco products in atherosclerotic diseases.
Table 18.
Categories of Novel Tobacco Products
| Heated tobacco products (HTPs) |
Products in which the user inhales substances generated by the direct heating of tobacco leaves (processed products thereof) or
products in which substances generated by heating glycerin or other substances are passed through tobacco leaf capsules and
then inhaled by the user |
| Electronic cigarettes (e-cigarettes) |
A product that is used by attaching a cartridge containing a flavored or fragrant solution containing nicotine, propylene glycol,
and glycerin, among other components, to the inhaler (body) and inhaling the aerosol generated by heating with a battery or the like |
| • Nicotine-containing products |
| Their sale is prohibited in Japan. However, personal import is possible through the internet or other sources |
| • Non-nicotine-containing products |
| Because there is no regulation, such products can also be sold to minors on the internet and in stores |
(Excerpted from Japan Atherosclerosis Society, Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2022 [in Japanese], Japan Atherosclerosis Society, 2022.39)
7.1.2 Oral Hygiene and CAD
Periodontal disease has been reported to be a risk factor or marker for CAD,535,536 with strong evidence provided in the Consensus Report of the 2013 European Society of Periodontology and the American Society of Periodontology Joint Workshop.537 In Japan, the prevalence of CAD is reportedly high among individuals with periodontal disease.538 With respect to the mechanism by which periodontal disease contributes to the development of CAD, multiple periodontal disease-related bacteria have been detected in vascular lesions, such as those formed in atherosclerosis.539,540 In addition, periodontal-disease-associated bacteria have been reported to induce platelet aggregation,541 and chronic inflammation associated with periodontal disease induces CAD.542 Conversely, the absence of a relationship between periodontal disease and CAD has also been reported,543 and in a systematic review by the AHA the fact that periodontal disease affects the onset or progression of CAD could not be supported by sufficient evidence.544
7.1.3 Season / Climate and CAD (Table 19)
Table 19.
Recommendation and Level of Evidence for the Role of Season/Climate Changes in the Primary Prevention of CAD
| |
COR |
LOE |
Cold (low temperature in winter), heat (high temperature in summer), and sudden
temperature fluctuations increase the risk of CAD induction; thus, individuals at a high
risk of CAD should be instructed to keep these in mind |
IIa |
C |
CAD, coronary artery disease; COR, class of recommendation; LOE, level of evidence.
Changes in the environmental temperature cause physiological changes in circulatory dynamics, such as BP and heart rate; therefore, lifestyle-related guidance should be provided to avoid sudden temperature fluctuations for patients at a high risk of CAD. A review of seasonal variations in CVD incidence and death showed that hospitalizations and mortality rates were higher in winter. The number of days (lag) from the change in temperature to the increase in the event occurrence rate is longer in winter and shorter in summer. Moreover, such seasonal differences are particularly significant in temperate climate zones.545
In Japan, most reports on season/temperature and CAD/CVD indicate the increased risk of CVD in the winter season or at low temperatures.546–548 With respect to deaths, a 1℃ lower maximum temperature in the 2 days before death increases the risk of CVD death by 1.8%, and the association is stronger among individuals aged <80 years.546 Findings from a Japanese regional CVD registry study showed that the highest temperature in summer and the lowest temperature in winter were associated with higher incidence of AMI.549 A subanalysis of 3,283 AMI cases in the J-MINUET study showed that the prognosis of winter-onset patients was poor, in addition to the high incidence of AMI in winter.547 In addition, based on a diagnosis procedure combination (DPC) analysis of 1,067,171 onset cases in the JROAD study, the greater the temperature fluctuation on the day before admission, the higher the number of CVD hospitalizations, and the association has been shown to be stronger in individuals aged ≥75 years compared with individuals aged <65 years.550 An analysis of 56,863 consecutive cases of ST-elevation MI (STEMI) from the J-PCI registry similarly showed that temperature fluctuations were associated with the occurrence of STEMI throughout the year, but with low minimum temperatures only in winter.551
7.1.4 Air Pollutants and CAD (Table 20)
Table 20.
Recommendation and Level of Evidence for the Role of Air Pollutants in the Primary Prevention of CAD
| |
COR |
LOE |
| People at a high risk of CAD should avoid exposure to air pollution |
IIa |
C |
CAD, coronary artery disease; COR, class of recommendation; LOE, level of evidence.
Because air pollutants can affect wide areas, they can have a significant effect on the entire population.552 According to estimates by the WHO, 58% of the 4.2 million excess deaths that occurred owing to air pollutants in 2016 could be attributed to CAD and stroke, which is considerably higher than the 18% attributable to chronic obstructive pulmonary disease (COPD) and the 6% attributable to lung cancer.553
The smaller the particle, the longer they float in the atmosphere and the easier it is for them to be inhaled and deposited. Among suspended particulate matter (SPM) present in the atmosphere, those with a particle size of 10–2.5 μm are defined as PM10–2.5, those with a particle size <2.5 μm are defined as PM2.5, and those with a particle size <0.1 μm are defined as ultrafine. A number of studies have shown the association of PM2.5
particle exposure and incidence of CAD.
a. Short-Term Exposure
Epidemiological studies in Japan have reported an increase in the risk of CAD death554 and out-of-hospital cardiac arrest555 due to elevated PM2.5
concentrations. However, the relationship between PM10–2.5
particles and CAD has not been definitively stated at this stage,556 and further research is warranted.
b. Long-Term Exposure
An 18-year follow-up of the American Cancer Society study showed that a 10μg/m3
increase in the PM2.5
concentration increased the ischemic heart disease death risk by 7.5%.557 In addition, findings from the ESCAPE Project showed that even exposure at levels less than the average annual limit of 25μg/m3, which is the European environmental standard for PM2.5, significantly increases the risk of ACS.558
However, the evidence reported in Japan is insufficient. A 24-year follow-up of NIPPON DATA80 showed no association between long-term SPM exposure and CVD deaths.559 Japan Public Health Center data showed an increased risk of MI incidence, but no association with the risk of death from CVD.560 Thus, the long-term results of follow-up studies conducted in Japan are inconsistent. In Japan, the definition of particulate matter was not detailed in the assessment before the PM2.5
concentration environmental standards were set in 2009. Therefore, for the time being, the effects of long-term exposure to PM2.5
at specific concentrations can only be assessed using reports from other countries. Conclusions from studies conducted in Europe and the USA clearly show that PM2.5
particles increase the risk of CAD,561 and people at a high risk of CVD are recommended to avoid exposure to air pollution as much as possible.562
7.2 Patient Education and Public Awareness Regarding Management of CAD Onset (Table 21)
Table 21.
Recommendations and Levels of Evidence for Patient Education and Public Awareness About Responses to the Onset of CAD
| |
COR |
LOE |
High-risk CAD patients should be educated about the symptoms and emergency medical
service requests at the time of CAD onset |
I |
C |
To prevent sudden death due to acute coronary syndromes and all types of CAD,
heightening public awareness of all potential bystanders about the symptoms of CAD, the
importance of requesting emergency medical service, and cardiopulmonary resuscitation
techniques is recommended |
I |
C |
CAD, coronary artery disease; COR, class of recommendation; LOE, level of evidence.
Delayed treatment initiation after AMI onset leads to poor prognosis,563 so both early treatment in the acute phase via appropriate judgment and treatment during onset are important. Therefore, all medical professionals should educate CAD high-risk individuals with risk factors such as hypertension, diabetes, and dyslipidemia on lifestyle modification and drug treatment (i.e., take measures to prevent the development of CAD). In addition, patients should be educated about the importance of understanding the symptoms at onset and requesting the emergency medical service. In particular, the elderly and patients with diabetes often do not exhibit typical symptoms, such as chest pain and chest tightness; hence, such cases require more careful guidance. A systematic review of information on symptoms observed at onset showed that typical symptoms such as chest pain are perceived by ≈80% of the general population, and only 10–28% of people understood atypical symptoms (e.g., stomach/abdominal discomfort, nausea, and vomiting). Additionally, more than half of the individuals who developed ACS did not understand that their symptoms were due to heart disease.564 In addition, although this was not a case for CAD, a survey of 5,172 residents in Japan showed that the percentage of people who understand the 5 symptoms of a stroke was ≈20–30%, even among individuals with chronic diseases.565 The level of awareness regarding symptoms and countermeasures at the onset of CVD remains insufficient.
In addition, information on the appropriate first-aid at the time of CAD onset should be made widely available, not only to CAD high-risk individuals but also to citizens who can be bystanders at home and at work. A continuous case observation study of out-of-hospital cardiac arrest in Japan has shown that appropriate cardiopulmonary resuscitation by a bystander improves prognosis.566 For public awareness, it is important to disseminate knowledge about the symptoms of CAD and the importance of requesting the emergency medical service, and applying appropriate cardiopulmonary resuscitation techniques.
7.3 Hyperuricemia and CAD (Table 22)
Table 22.
Recommendations and Levels of Evidence for the Management of Hyperuricemia in the Primary Prevention of CAD
| |
COR |
LOE |
Assess and control/intervene atherosclerotic risk factors, such as obesity, hypertension,
diabetes, metabolic syndrome, and chronic kidney disease, in patients with hyperuricemia
as those conditions often coexist with hyperuricemia |
I |
A |
Administration of uric acid-lowering agents for the prevention of CAD is not recommended
for patients with hyperuricemia* |
III (No
benefit) |
C |
*Does not apply to the administration of uric acid-lowering agents for the prevention of gouty arthritis, gouty nodules, or urinary tract stones. CAD, coronary artery disease; COR, class of recommendation; LOE, level of evidence.
In this guideline, hyperuricemia is defined as ≥7.0 mg/dL. Several epidemiological studies have reported that, in the general population, hyperuricemia is associated with various atherosclerotic risk factors, such as obesity,567 hypertension,568 diabetes,569 metabolic syndrome,570 and CKD.571 The association between hyperuricemia and CAD incidence in the general population has been assessed in many epidemiological studies and Mendelian randomization analysis, with inconsistent results.572–582
7.3.1 Uric Acid-Lwering Agents and Primary Prevention of CAD
The findings from a case–control study comparing patients with first-onset MI with controls suggested that allopurinol administration may reduce the risk of MI developing.583 In a retrospective observational study comparing allopurinol-treated and allopurinol-untreated groups in the general middle-aged population and aged hypertensive patients using propensity score matching, all-cause death and cardiac event rates were found to be significantly lower in the allopurinol-treated group.584,585 These results suggest that uric acid-lowering agents might be effective in preventing the development of CAD. However, at present, large-scale RCTs directly examining the preventive effects of uric acid-lowering agents in the general population are absent, and limited evidence is available to actively recommend the use of uric acid-lowering agents to prevent the development of CAD.
Although limited evidence is available for the primary prevention of CAD using uric acid-lowering agents, hyperuricemia is associated with various atherosclerosis risk factors, as described above. Patients with hyperuricemia should be screened for the presence of these risk factors and treated. In addition, lifestyle habits, such as overeating, excessive fructose intake, alcohol consumption, high-fat/high-protein diets, and lack of exercise not only cause hyperuricemia, but are also associated with other risk factors such as obesity, hypertension, diabetes, and metabolic syndrome. In the primary prevention of CAD in patients with hyperuricemia, other coexisting risk factors are significant contributors to CAD risk, thus, lifestyle modification is also important.586
III. Cases/Pathological Conditions That Require Specific Attention
1. Older Adults (Table 23)
Table 23.
Recommendations and Levels of Evidence for Primary Prevention of CAD in Older Adults
| |
COR |
LOE |
Although non-pharmacological therapy should be promoted aggressively, treatment should be
individualized with respect to the individual's QOL |
I |
C |
Older adults who can visit outpatient clinics on their own should, in principle, be proactively
treated with drugs; treatment should be individualized with respect to the individual's QOL |
I |
A |
Frailty, cognitive function, ADL, nutritional status, and medication adherence should be assessed
prior to treating older adults |
I |
C |
| Consider discontinuing drug therapy in older adults when approaching end of life |
IIa |
C |
ADL, activities of daily living; CAD, coronary artery disease; COR, class of recommendation; LOE, level of evidence; QOL, quality of life.
1.1 Approach to Treating the Elderly for Primary Prevention of CAD
Many countries, including Japan, define the elderly population as those aged ≥65 years, but a clear medical or biological basis for this definition is lacking. In Japan, longitudinal studies on aging have shown that the physical and psychological functions of the elderly in recent years are clearly different from those in the past: gait speed, grip strength, serum albumin level, cognitive function, and other parameters have significantly improved. In addition, from various studies of the mental and physical health of the elderly, it is clear that the majority of people aged 65–74 years maintain their mental and physical health and can participate in social activities, which means that at least many of these individuals are now to be treated in the same way as young and middle-aged people.587
Aging is an independent risk factor for development of coronary artery disease (CAD).588 Nonetheless, considering the abovementioned change, we should not use chronological age to define the “elderly”; rather, we should use judgement for individual patients based on their biological and/or functional status at least for those aged 65–74 years when considering the primary prevention of CAD. Based on extensive evidence on lifestyle-related diseases in Japan, the general recommendation is to provide an individualized approach for older adults. Frailty, cognitive function, activities of daily living (ADL), nutritional status, and medication adherence, among other factors, have been reported as evaluation items necessary for the individual assessment of elderly patients.
1.1.1 Evaluation of Frailty
Frailty is “a state in which resilience to stress has declined due to age-dependent reduction in reserve capacity”. It is typically defined as follows: “Positioned as a pre-stage of a condition requiring long-term care, frailty is a high-risk condition that tends to lead to health problems, including disability and death, as it is likely to cause multifaceted issues, such as mental/psychological vulnerability, social vulnerability, and physical vulnerability”.589
Although various methods for evaluating frailty are available, they can be roughly classified according to the phenotypic model proposed by Fried et al,590 and the cumulative deficit model proposed by Rockwood et al.591 A typical evaluation method for the former is the Cardiovascular Health Study (CHS) criterion, which is convenient and suitable for evaluation in clinical practice. The Japanese CHS standards (J-CHS) have also been published (Table 24).592 The Frailty Index is a well-known assessment tool based on the latter method, and is primarily used in clinical research to evaluate severity and tracking changes over time. This index is, however, unsuitable for clinical settings due to its complexity.
Table 24.
Revised J-CHS Criteria (Cited From Healthy Longevity Net)
| Component |
Questions and measurements |
Answer |
| Shrinking |
Have you unintentionally lost 2 or more kg in the past 6 months? |
Yes=1 |
No=0 |
| Weakness |
Grip strength <28 kg in men or 18 kg in women |
Yes=1 |
No=0 |
| Exhaustion |
In the past 2 weeks, have you felt tired without a reason? |
Yes=1 |
No=0 |
| Slowness |
Gait speed <1.0 m/s |
Yes=1 |
No=0 |
| Low activity |
Do you engage in moderate levels of physical exercise or sports
aimed at health? |
No to both questions=1 |
| Do you engage in low levels of physical exercise aimed at health? |
Others=0 |
If three or more items apply, the patient is frail. If one or two items apply, the patient is pre-frail. If none of the items apply, the patient is healthy. (Adapted from Satake S, Arai H. Geriatr Gerontol Int 2020; 20(10): 992–993.592 John Wiley and Sons. © 2020 Japan Geriatrics Society.)
1.1.2 Evaluation of Cognitive Function and ADL
Evaluation of ADL includes basic and instrumental ADL. Basic ADL refers to basic activities such as locomotion, climbing stairs, bathing, using the toilet, eating, and dressing.593 Instrumental ADL refers to social activities that are more complex than basic ADL, such as shopping, meal preparation, medication management, money management, and using transportation for traveling outside the home.594 Both are also used as screening tools for frailty and, in the case of diabetes, can be used for categorization of glycemic control goals in older adults. To assess cognitive function, the Mini-Mental State Examination (MMSE) and the Revised Hasegawa Simplified Scale of Intelligence (HDS-R) are used.
1.1.3 Evaluation of Nutritional Status
Malnutrition should be suspected if these items are positive: “(unintentional) weight loss of 2–3 kg or more within 6 months” (in the J-CHS evaluation), and “body mass index (BMI) <18.5 kg/m2
” (in the basic checklist). The Malnutrition Screening Tool (MST),595 Malnutrition Universal Screening Tool (MUST),596 and the Mini Nutritional Assessment-Short Form (MNA-SF),597 among others, are used as screening tools. Malnutrition should be suspected in the elderly who respond as “not eating three meals a day properly” in the standard questionnaire designed by the Ministry of Health, Labour and Welfare, Japan to assess frailty for older adults aged ≥75 years.
1.1.4 Evaluation of Adherence to Medication
Both clinicians and patients tend to overestimate the actual rate of medication adherence. The average adherence rate to long-term lifestyle-related drugs is approximately 50%.598,599 Screening for the level of medication adherence is important because poor adherence is associated with adverse outcomes in the primary prevention of CAD. Several methods have been proposed to accurately assess medication adherence: (1) self-reporting by the patient, (2) reporting by family members, (3) evaluation by medical practitioners, such as questionnaires and structured interviews, (4) counting unused medications, and (5) drug concentration measurement in body fluids. However, at present, there is no criterion for determining the single most effective approach for screening. Currently, the accuracy of evaluation can be improved by using multiple methods in combination with a multidisciplinary approach. In addition, because older adults are less likely to adhere to medication for various reasons, multidisciplinary investigation of the causes and individualized approach are recommended.600
1.1.5 Hypertension601
Alteration in blood pressure (BP) is known to occur more often in older adults. Systolic hypertension, white-coat hypertension, nocturnal hypertension, orthostatic hypotension, and postprandial hypotension are frequent, so BP should be evaluated by home BP measurement, and attention should be paid to fluctuations in BP. We need to pay particular attention to older patients, because the BP tends to decrease due to reduced intake of food and water. The first choices of antihypertensive drugs are calcium-channel antagonists, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), and thiazide diuretics. The advantages and disadvantages of each drug should be considered before use. Falls and fractures are likely to occur in the early stages of treatment with antihypertensive drugs. Therefore, it is generally recommended for the elderly aged ≥75 years, in particular, to begin an antihypertensive drug at the half of the standard dose and increase it gradually over 1–3 months to achieve a gradual reduction of BP. In addition, when adherence to medication may worsen owing to a decline in cognitive function, methods such as one-dose packaging, the use of combination drugs, and provision of medication guidance to family members should be implemented.
1.1.6 Dyslipidemia602
Comprehensive management of not only lipids but also other atherosclerosis risk factors, such as hypertension and diabetes, is important for treating dyslipidemia. Improving lifestyle habits should be prioritized, especially for patients with obesity who need to prevent overeating and excessive sugar intake. However, excessive dietary restrictions may lead to unhealthy weight loss accompanied by a decrease in muscle mass and strength (i.e., sarcopenia) and may eventually cause physical deterioration, gait disturbance, and falls. Therefore, dyslipidemia should be managed while checking the physical condition and weight of the patient. With respect to the primary prevention of CAD for the elderly <75 years old, there is clear evidence that reducing the level of low-density lipoprotein cholesterol (LDL-C) level with statin treatment prevents CAD and non-cardiogenic cerebral infarction. In contrast, for the elderly aged ≥75 years the evidence supporting the effectiveness of lipid-lowering treatment is not clear. Therefore, individualized judgement is required. Keep in mind, however, that in a cohort study of the elderly aged ≥75 years, discontinuation of statin medication increased the risk of hospitalization for cardiovascular events by 33%.603 For this reason, we propose continuation of treatment among the elderly aged ≥75 years who are taking statins.
1.1.7 Diabetes604
Diabetes is a risk factor for sarcopenia, frailty, and dementia; hence, glycemic control in older adults is important. Conversely, the elderly are more likely to develop severe hypoglycemia, which is a risk factor for the development of cardiovascular disease (CVD), dementia, and death. Therefore, in aged people with diabetes, the appropriate goals of blood glucose control should be set after consideration of both the benefits and the risks of strict glycemic control. Based on this, in 2016 the Japan Geriatrics Society published their Blood Glycemic Control Targets (HbA1c Level) for Diabetes in the Aged (Table 25).604 Target values are set in consideration of the patient’s characteristics and health condition, especially patient categories I–III based on cognitive function and ADL, and the risk of hypoglycemia from the drugs being taken. In the elderly with diabetes, hypoglycemia induced by strict treatment needs to be avoided. When taking “drugs that may cause severe hypoglycemia”, such as insulin, sulfonylurea (SU) drugs, and glinide drugs, the target value of HbA1c is set marginally higher and a lower limit is set. Category I and II target values are HbA1c <7.0%, with no lower limit if not taking “drugs with potential for causing severe hypoglycemia”. In the case of “drugs that may cause severe hypoglycemia”, such as insulin, SU drugs, and some glinide drugs, the HbA1c target value should be set slightly higher. The Dementia Assessment Sheet for Community-based integrated care system-8 items (DASC-8) may be referred to when considering individual risk categorization.605
Table 25.
Glycemic Control Target (HbA1c Value) for Diabetes in Aged Individuals
| |
Category I |
Category II |
Category III |
Patient characteristics/health
conditionNote 1) |
(1) Normal cognitive function
and
(2) ADL independence |
(1) Mild cognitive
impairment to mild
dementia
or
(2) Instrumental ADL
decline, basic ADL
independence |
(1) Moderate or greater
dementia
or
(2) Decrease in the
basic ADL
or
(3) Many comorbidities
and functional
disorders |
Use of drugs that may
cause severe hypoglycemia
(insulin preparations, SU
drugs, and glinide drugs,
among other types) |
NoNote 2) |
<7.0% |
<7.0% |
<8.0% |
| YesNote 3) |
Age more than 65
years and less 75
years less than 7.5%
(lower limit 6.5%) |
Age more than 75
years less than 8.0%
(lower limit 7.0%) |
<8.0%
(lower limit 7.0%) |
<8.5%
(lower limit 7.5%) |
In addition to age, duration of illness, risk of hypoglycemia, and support system, treatment goals are individually set in consideration of cognitive function, basic ADL, instrumental ADL, and comorbidities in the elderly. However, the risk of severe hypoglycemia increases with age.
Note 1: For the evaluation of cognitive function, basic ADL (dressing, moving, bathing, and toilet use, among other activities), and instrumental ADL (IADL: shopping, meal preparation, medication management, and money management, among other activities), refer to the website of the Japan Geriatrics Society (https://www.jpn-geriat-soc.or.jp/). In end-of-life situations, treatment to prevent significant hyperglycemia and associated dehydration and acute complications is a priority.
Note 2: The target for complication prevention is less than 7.0%, even in elderly patients with diabetes. However, if it is achievable only with appropriate diet and exercise therapy, or if it is achievable without the side effects of drug therapy, the target should be less than 6.0%. If treatment intensification is difficult, the target should be less than 8.0%. No lower limit is present. A target of less than 8.5% is acceptable for Category III conditions if there are concerns about the adverse effects of multiple medications, serious comorbidities, and poor social support.
Note 3: Taking into consideration the duration of diabetes, if preventing the onset and progress of complications is prioritized, take measures to prevent severe hypoglycemia. Concurrently, individual targets and lower limits may be set for each elderly individual. If the patient has been under treatment with these drugs since <65 years and the blood glucose control status is below the target or lower limit in the table, maintain the status quo but pay close attention to severe hypoglycemia. Glinide drugs are occasionally classified as drugs that do not pose a risk of severe hypoglycemia, taking into consideration the type, amount used, blood sugar level, and other factors.
(Adapted from Geriatric Diabetes Guidelines 2017, P46. the Japan Geriatrics Society and the Japan Diabetes Society, Nankodo 2017.604)
1.1.8 Obesity606
The diagnosis of obesity in older adults is based on the same criteria as used for young and middle-aged individuals. Because BMI may not accurately reflect body fat mass, however, careful consideration is needed. Specifically, in the presence of edema or when height is shortened due to vertebral compression fracture, BMI becomes higher than actual body fat mass. In fact, there is no clear evidence that obesity in older adults is a risk factor for CVD. Conversely, a high waist-to-hip ratio and metabolic syndrome increase the risk of CVD in people aged <75 years. According to the “Diabetes Treatment Guidelines 2019”, an association between obesity (BMI >25 kg/m2) and increased mortality rate is not clear in people aged ≥75 years, in fact, some reports show that the mortality rate increases with BMI <22 kg/m2. Therefore, the Clinical Guideline for the Obese Elderly 2018, proposed by the Japan Geriatrics Society, suggests considering the current body weight and BMI 25 kg/m2
as a guide, with more focus on the prevention of sarcopenia and frailty.
In addition, sarcopenic obesity, which is a combination of obesity and sarcopenia, increases with ageing. The risk of CAD is reported to be higher in aged individuals with sarcopenic obesity than in those with obesity but without sarcopenia. However, the definition and diagnostic criteria for sarcopenic obesity are not established, so caution is needed when interpreting such reports.607 Energy restriction, adequate protein intake, and resistance exercise are recommended for the management of sarcopenic obesity.606
1.1.9 Lifestyle Modification
Even in older adults, exercise can be effective for the primary prevention of CAD through the prevention and improvement of lifestyle-related diseases. Exercise includes aerobic exercise for the improvement of cardiopulmonary function, balance exercise for preventing falls, and resistance exercise for improving muscle mass and strength. These exercises should be performed according to the motor function of the individual. In addition, particular attention is given to cardiopulmonary complications, orthopedic conditions such as those of joints and spine, risk of falls, BP and physical condition on the day of exercising to prevent accidents. Warm-up and cool-down sessions before and after exercise are also necessary. The exercise intensity, duration, and frequency should be as follows: moderate or higher intensity exercise for ≥30 min/day, 2–3 times/week, although individualized modification considering personal condition is necessary. Older adults should be instructed to perform the exercise at a level of effort that allows them to enjoy the process, in a manner that they can perform for long periods of time, and they should avoid overexercising and stop if they feel any pain.608,609 For older adults with malnutrition, excessive lifestyle intervention in diet and exercise might worsen frailty. Thus, individualized intervention is needed.
1.2 Pathologies That Require Specific Caution in the Primary Prevention of CAD in the Elderly
The prevention of CAD in the elderly also contributes to healthy life expectancy by preventing the transition to frailty through suppression of functional decline owing to the disease. Therefore, for the primary prevention of CAD in older adults, it is important to first comply with standard preventive measures indicated in clinical practice guidelines. Conversely, patients participating in the large-scale clinical studies that are the source of the guidelines are subject to various exclusion criteria, and the elderly and patients with comorbidities are largely excluded. Therefore, whether the efficacious treatments reported in clinical studies can be applied practically to aged people remains unclear. Not only will the expected effect not be obtained, but also the process may even cause adverse events. Typical conditions that require special attention in older adults include polypharmacy, frailty, dementia, and end of life.
1.2.1 Polypharmacy
In the treatment of older adults, multiple drug use is known to be a risk for frailty and an impediment to healthy life expectancy.610 In older adults with multiple comorbidities, the simple addition of drug treatments recommended in guidelines does not necessarily result in the best outcomes. Using related guidelines as a reference, a comprehensive and individualized judgement is necessary to decide the appropriateness of the final prescription.611
There is no strict definition of polypharmacy. In studies conducted in other countries, the prescription of ≥5 types of drugs is often considered to represent polypharmacy. In a Japanese study investigating the relationship between the number of drugs and adverse drug events in hospitalized older adults showed that the intake of ≥6 types of drugs increased the incidence of adverse drug events.612 In another study that investigated the relationship between the number of medications and falls in outpatients, ≥5 medications increased the incidence of falls.613 Based on these results, ≥5–6 drugs may be considered as polypharmacy requiring reevaluation for drug adherence support and prescription reviews to reduce adverse events owing to decreased drug adherence and drug interactions. Additionally, whether combination drugs should be considered as a single medication or as 2–3 medications is unclear, as evidence from previous research is unavailable. From a pharmacokinetic point of view, it is considered to be as 2 or 3 medications. However, from the viewpoint of medication adherence, it is considered to be as a single medication. At present, the optimal management of this problem is unclear.
The correction of polypharmacy in older adults has been reported to reduce the incidence of adverse drug events and death, and to reduce medical costs.614–616 CVD has a high morbidity rate among older adults, and cardiovascular drugs account for a large proportion of drug therapy in Japan, both in terms of the cost of medication and the number of drugs. Reducing polypharmacy in cardiovascular drugs is also important from the perspective of medical economics. At this stage, effective intervention measures are unclear, but experts recommend a multidisciplinary approach.
1.2.2 Frailty
Various evaluation methods are available for frailty, but we should note that the severity of frailty varies depending on the evaluation method used. Confirming that the severity of frailty documented in each clinical study matches the severity of the frailty of the patient in question is necessary. Subanalyses of the HYVET study617 and the SPRINT study77 for hypertension in frail older adults reported the effect of primary prevention of CAD with antihypertensive treatment. However, in both studies, frailty was evaluated using the Frailty Index, and almost no group evaluated as frail according to the CHS criteria (a group with slow walking speed and perceived fatigue) was included. Therefore, for the primary prevention of CAD, even among aged people with frailty, if an individual is relatively healthy, the management measures for young and middle-aged people may help improve prognosis. Concurrently, frailty should be evaluated on a case-by-case basis, as this strategy may worsen the prognosis in patients with severe physical impairment.
1.2.3 Dementia
CAD and dementia have common risk factors.77,618–621 Treatment for the primary prevention of CAD may affect the onset and course of dementia. Conversely, the presence of dementia may also affect the primary prevention of CAD. However, in Japan, there are limited studies that have reported the treatment provided for patients with dementia; hence, the effect of dementia on the treatment of other conditions is unclear. Evidence from international reports indicates that people with dementia are less likely to receive ACE inhibitors, cardiac catheterization, coronary angioplasty, and heart bypass surgery. This risk of undertreatment is present even in patients who did not indicate a rejection of “Do Not Resuscitate (DNR)” status.622 Many studies have reported that individuals with dementia are more likely to be undertreated than those without dementia, and that those with dementia are unlikely to receive the same treatment as those without dementia. In addition, even when drug treatment is initiated in the same manner used for non-dementia patients, it becomes difficult for those with dementia to manage medication from a relatively early stage. Not only can they not take medication, but they may also have an accident, such as unintentional overdose. Therefore, an environment that allows compliance with medication should be secured as necessary before drug therapy is initiated.623
At this stage, it is unclear how the primary prevention of CAD should be best managed in people with dementia. However, because evidence to the contrary has not been reported, compliance with standard criteria is recommended; however, attention should be paid to excessive hypotension, hypoglycemia, and medication status, and individual judgment should be given priority.
1.2.4 End of Life
There are various definitions of end-of-life status. The Japan Geriatrics Society defines the terminal stage as “The condition is irreversible and progressive. A state in which improvement of the condition or prevention of progression cannot be expected, even with the best possible treatment at that time. A state in which death in the near future becomes inevitable”. Most clinical trials on the primary prevention of CAD exclude aged people who are at the end of their life, and from the viewpoint of improving life prognosis, drugs for treating lifestyle-related diseases are of limited significance for such individuals. Drugs used to treat lifestyle-related diseases should be used only for pathological conditions, such as hypertensive emergencies and hyperosmotic hyperglycemia, or for controlling symptoms. The management target and the management methods should be determined on an individual basis based on the patient’s wishes, the wishes of their family members, and medical judgment, and the discontinuation of drug treatment should be proactively considered.
The Glycemic Control Goals for Diabetes in the Aged 2016 recommends that “at the end of life, treatment should be prioritized to prevent marked hyperglycemia and associated dehydration and acute complications”. According to the 2017 Guidelines for the Management of Hypertension in the Aged (Japan Geriatrics Society), “antihypertensive therapy for elderlies at the end of their life is not indicated for improving prognosis, and discontinuation of antihypertensive drugs should be actively considered (recommendation grade B)”. The “Clinical Guidelines for Geriatric Dyslipidemia 2017” (Japan Geriatrics Society) states that “It is safe to discontinue statin therapy in patients with a life expectancy of less than 1 year. It leads to QOL improvement and medical cost reduction (recommendation grade B)”.
2. Women (Table 26)
Table 26.
Recommendation and Level of Evidence for HRT in Women With Dyslipidemia
| |
COR |
LOE |
After confirming that HRT is not contraindicated or its careful administration is not required,
HRT should be considered for symptomatic menopausal women with dyslipidemia |
IIa |
A |
COR, class of recommendation; HRT, hormone replacement therapy; LOE, level of evidence.
2.1 Current Status of CAD in Japanese Women
Of the various types of CAD, myocardial infarction (MI) has been studied most frequently in the field of epidemiology. Women are reported to have lower incidence of MI compared with men worldwide.624 Nonetheless, the mortality rate after MI is recognized to be higher in women than in men in both the USA625–628 and Japan.629,630 In an epidemiological study conducted in Japan from the 1990s to the 2000s, the age-adjusted incidence of MI in women was 20–50% of that observed in men.6,8,631,632 The hospitalization rates for CAD increases in women after the age of 50 years but remains lower than those in men.633
In light of the increase in the incidence of CAD with aging,8 and the unprecedented rate of aging in the Japanese female population,634 measures in anticipation of an increase in the onset of and death from CAD in women are necessary. In fact, the absolute number of deaths and mortality rate in women showed that heart disease and cerebrovascular disease combined ranked higher than those from malignant neoplasms in the 2019 vital statistics.635
2.2 Association of Atherosclerosis Risk Factors With CAD in Women
2.2.1 Serum Lipids
The relationship between serum lipid levels and age differs considerably in men and women. Serum lipid levels change dramatically after menopause due to a decrease in estrogen level (as described in the following paragraph). Increase in LDL-C is considered to contribute the most to the increased incidence of CAD among postmenopausal women.
According to the 2019 National Health and Nutrition Survey report, the levels of LDL-C and non-high-density lipoprotein cholesterol (non-HDL-C) do not exhibit age-dependent changes in men. Conversely, in women, before the average menopause age of 50 years, average LDL-C and triglycerides (TG) levels are lower than those in men. However, after the age of 50, the average LDL-C levels in women are higher than in men. TG levels also increase and approach the levels in men after the age of 50. The level of HDL-C does not change with age in men or women and consistently remains higher among all age groups in women than in men.328
The United States Nurses’Health Study reported that high LDL-C and low HDL-C levels are predictors of incident CAD independent of other coronary risk factors among postmenopausal women.636 There are several prospective cohort studies conducted in Japan that have examined the association between serum lipids and the development of CAD in women. In JALS-ECC, the adjusted incidence of MI in the high total cholesterol (TC) group (Q4) was significantly higher than that in the low TC group (Q1).105 Furthermore, CIRCS showed that the multivariable-adjusted hazard ratio (HR) for the incidence of MI significantly increased 1.42-fold for every increase of 30 mg/dL in the LDL-C level.95 In EPOCH-JAPAN, the adjusted HRs for CAD mortality were significantly higher in women aged 40–69 years in the high TC group than in those in the low TC group.637 In NIPPON DATA80, women in the high TC group had a significantly higher multivariable-adjusted HR for death from heart disease than those in the low TC group.106 Both JALS-ECC and CIRCS have shown that elevated non-HDL-C levels are significantly associated with the incidence of CAD in Japanese women.105,107,129,132
Based on the findings from these studies, high levels of TC, LDL-C, TG, and non-HDL-C are considered to be risk factors for development of CAD in women.
Only a few large-scale clinical trials have been conducted on Japanese women to evaluate the effects of therapeutic interventions, especially statins. The MEGA study initially reported that pravastatin did not reduce the risk of CAD in women.151 However, a subanalysis subsequently showed reduction in the risk of major adverse cardiovascular events (MACE) incidence in women aged ≥55 years.638 In the JUPITER study, rosuvastatin reduced the risk of hospitalization for unstable angina and revascularization events in women but did not show clear preventive effects on MI events.639 In the CTT collaboration meta-analysis (for the primary prevention of CVD), a reduction in the LDL-C level by 1 mmol/L (38.7 mg/dL) was significantly associated with reduced cardiovascular risk in men; however, only a nonsignificant declining trend was observed in women.
Thus, the primary preventive effect of statins on CVD in Japanese women is not as clear as that in men. However, the effect of statins on CVD prevention were shown to be similar in men and in women globally in a meta-analysis for secondary prevention.640 Furthermore, in a meta-analysis of 27 randomized controlled trials (RCTs), both primary and secondary prevention, statins significantly reduced the risk of CVD in women, which was not significantly different from that observed in men.150 Considering these findings, the fact that the primary preventive effect of statins on CVD in Japanese women was not statistically significant is due to the low absolute risk, and it is reasonable to consider statins as an effective intervention in women as in men.
In addition, more aggressive treatment should be considered for patients at a high risk, such as those with familial hypercholesterolemia (FH; see Chapter III.3 for details). Although there are case reports641,642 describing the possibility of congenital anomalies caused by statin administration in early pregnancy, a different cohort study has shown that the incidence of congenital anomalies did not differ with or without statin use.643 However, owing to an insufficient number of studies evaluating the risk for breastfeeding, statins are contraindicated in pregnant and lactating women. For other specific management policies for dyslipidemia, refer to Chapter II.3.
2.2.2 Diabetes
According to the 2019 National Health and Nutrition Survey Report, the percentage of women strongly suspected to have diabetes is as low as 10.8%, as compared with 19.7% in men.328 However, a Japanese cohort study showed that presence of diabetes in women significantly increases the HRs for the incidence of and death from CAD.644–646 In JACSS, a multicenter case–control study of MI, patients with diabetes had odds ratios for incident MI as high as 2.90 in men and 6.12 in women.647 A meta-analysis of 64 cohort studies including 858,507 participants also showed that the risk ratio of development of CAD in patients with diabetes was as high as 2.63 in women compared with 1.85 in men.648 Based on these findings, diabetes is a significant risk factor for CAD that affects women to a greater degree.
2.2.3 Cigarette Smoking
According to the 2019 National Health and Nutrition Survey report, the cigarette smoking rate is as low as 7.6% in women, compared with 27.1% in men.328 However, the JPHC Study Cohort I and Suita Study showed that Japanese women with a smoking habit have a relative risk (RR) of 3–8-fold higher than those who do not smoke for developing MI.518,649 In addition, HRs for CAD death were higher in women with a smoking habit, in 2 studies from combined Japanese cohorts.650,651 In addition, a meta-analysis, including the studies mentioned above, has shown that the RR for incidence of CAD is greater in female than in male smokers.652 Similarly, in JACSS, the odds ratio of smoking to the onset of MI was 4.00 for men and 8.22 for women.647
Based on these findings, smoking should be regarded as an important risk factor for CAD, especially in women.
2.2.4 BP
According to the 2019 National Health and Nutrition Survey Report, the mean systolic BP (SBP) was 132.0 mmHg for men and 126.5 mmHg for women.328 The percentage of men and women with SBP ≥140 mmHg was 29.9% and 24.9%, respectively. In other words, women showed lower BP values.328 In healthy individuals without any comorbidities, the association between BP and CAD risk can be described as “lower the better”, with lower BP corresponding to lower risk for the incidence of CAD until the SBP/diastolic BP (DBP) reaches the lower boundary of 115/75 mmHg, regardless of sex. This relationship has been confirmed in a large integrated cohort study (with ≈958,000 participants, of whom 10% were from Japan or China).67 This finding was consistent with reports from EPOCH-JAPAN and the Suita Study (refer to Chapter II.2 for specific treatment and management of high BP).
2.3 Primary Prevention of CAD
The foundation of CAD primary prevention is lifestyle modification. The Nurses’ Health Study, which was a cohort of American women aged 30–55 years, reported that greater adherence to preventive lifestyle factors (healthy eating habits, no smoking habit, moderate or good exercise habit, proper weight maintenance, and alcohol restriction, among others) was associated with lower risk ratio for the incidence of CAD and sudden cardiac death.653,654 Even for women, the maintenance of a healthy lifestyle from a young age is the cornerstone of atherosclerosis prevention.
Diabetes is an important risk factor for CAD, and is especially important in women. According to a meta-analysis of 14 clinical trials with 28,614 patients with type 2 diabetes, strict glycemic control was associated with a reduced risk ratio for MI at 0.85 [0.76–0.95],655 and greater benefit was observed for reducing microangiopathies.182 Because the risk of hypoglycemia also increases with strict glycemic control, it is necessary to intensify treatment while considering the patient’s condition.656
As mentioned earlier, smoking is an important risk factor for CAD, especially in women. A cohort study of Japanese men and women showed that the risk ratio of CAD death in women who quit smoking was not significantly different from that in those who had never smoked.657 Considering that smoking during pregnancy increases the risk of congenital abnormalities,658 it is important to raise awareness from a young age about the harmful effects of smoking.
2.4 Hormone Replacement Therapy (HRT)
HRT, which is used to treat symptoms associated with menopause and osteoporosis during and after menopause among women, gained popularity in Europe and the USA during the 1960s. As noted before, in postmenopausal women the increase in serum LDL-C levels in response to the decrease in estrogen levels may contribute substantially to the increase in the incidence of CAD after menopause. Therefore, HRT was expected to exert a preventive effect on the incidence of CAD, and many studies have been conducted on this topic since then.
According to the findings of a meta-analysis of 16 observational studies published in the 1990s, the risk ratio for the incident CAD in previous HRT users was 0.70 [0.63–0.77] and 0.50 [0.45–0.59] for current HRT users when compared with non-HRT users.659 However, in the Women’s Health Initiative study, an RCT conducted in postmenopausal women (average age: 63 years) to verify the preventive effect of HRT on CAD, the incidence was significantly higher in the HRT group, with a HR of 1.29 [1.02–1.63] compared with the placebo group.660
Various subanalyses were performed to examine the discrepancy between the results obtained from observational studies and the Women’s Health Initiative study. In a 2015 Cochrane meta-analysis that integrated data from 19 RCTs, stratification by years after menopause revealed that women who received HRT more than 10 years after menopause showed a risk ratio of 1.07 [0.96–1.20] for CAD development, but those received HRT less than 10 years after menopause demonstrated a risk ratio of 0.52 [0.29–0.96].661 Based on this finding a “timing hypothesis” was proposed: early initiation of HRT during transition into menopause when atherosclerosis has not progressed acts preventively against CAD by taking effect on lipid profiles and the intima. In contrast, estrogen administration in older individuals with established plaque formation may increase the risk of CAD by promoting plaque rupture and arterial thrombus formation. A 2×2, double-blinded, placebo-controlled RCT published in 2016 (Early vs Late Intervention Trial with Estradiol study662) reported findings that were consistent with this hypothesis. The trial recruited women less than 6 years after menopause (mean age: 55 years) and more than 10 years after menopause (mean age: 65 years) and either HRT or placebo were administered to both age groups. The primary endpoint was set as carotid intima–media thickness (IMT) progression at 5 years. Women more than 10 years after menopause in both HRT and placebo groups showed similar progression in IMT, but in women less than 6 years after menopause, IMT progression was significantly reduced in the HRT group. The findings suggested that HRT initiated at an earlier phase after menopause suppresses the development of atherosclerosis.662
Based on these findings, the 2017 HRT Guidelines by the Japanese Society of Obstetrics and Gynecology and Japanese Society for Menopause and Women’s Health do not recommend the use of HRT in women with a history of MI or coronary atherosclerotic lesions, and it is a contraindication of the treatment. Furthermore, the guideline warrants extra caution for HRT initiation if any of the following apply: obesity, age ≥60 years, initial HRT administration ≥10 years after menopause, history of coronary spasm and microvascular angina, severe hypertriglyceridemia, or uncontrolled diabetes or hypertension.663 In addition to higher age, the risk of adverse events is known to differ depending on the type, dose, administration route, and administration method of estrogen and progestin. A Dutch cohort study of 698,098 women reported comparable risk for incident MI in oral estrogen users but significantly lower risk for transdermal estrogen users when compared with nonusers.664 Reportedly, the risk of venous thromboembolism did not increase with transdermal estrogen administration,665 and the risk of breast cancer did not increase with natural progesterone.666
The Japanese Society for Menopause and Women’s Health has developed a Guidance Statement for the prevention of the onset of atherosclerosis in women that complies with the Japan Atherosclerosis Society Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2017. The guideline statement recommends that symptomatic menopausal women with dyslipidemia should undergo HRT concurrently with lifestyle modification.667
3. Familial Hypercholesterolemia (FH; Table 27)
Table 27.
Recommendations and Levels of Evidence for Primary Prevention of CAD in Patients With FH
| |
COR |
LOE |
In addition to early diagnosis and rigorous treatment, family screening (cascade screening)
should be performed to prevent CAD |
I |
C |
Lipid management should be strictly maintained with statins as the first-line drug, with the goal of
achieving LDL-C levels <100 mg/dL |
I |
C |
FH homozygotes should be treated with aggressive LDL-C-lowering therapy, including LDL
apheresis, PCSK9 inhibitors, and MTP inhibitors |
I |
C |
All homozygous FH patients, and heterozygous FH patients who are refractory to drug therapy,
children, pregnant women, and women who wish to have children should be referred to a specialist |
I |
C |
CAD, coronary artery disease; COR, class of recommendation; FH, familial hypercholesterolemia; LDL-C, low-density lipoprotein cholesterol; LOE, level of evidence.
3.1 Overview
FH is a hereditary autosomal dominant metabolic disease and characterized by high serum LDL-C level, tendon xanthoma/cutaneous nodular xanthoma (including Achilles tendon thickening), and early-onset CAD. Patients with FH have high LDL-C levels since birth and develop coronary atherosclerosis at a young age. Therefore, FH is an extremely high-risk disease for CAD. Untreated men often develop CAD between the ages of 30 and 50 years, and untreated women between the ages of 50 and 70 years.668 The proportion of FH in patients with acute coronary syndrome (ACS) in Japan is 2.7–5.7%, which is significantly higher than that in the general population (approximately 0.33%), and the proportion of FH in younger patients with ACS is even higher (≈8%).669,670 In addition, untreated heterozygous FH patients show a 13-fold risk increase.671 A study in Japan reported that untreated heterozygous FH patients had a 15-year earlier onset of CAD than those without FH; however, the onset can be delayed by lipid-lowering treatment with statins.672 Therefore, it is essential to always keep the possibility of FH in mind when examining a patient with elevated LDL-C.
Consistent with other countries, approximately 1 in 300 Japanese people have heterozygous FH, and the absolute number of patients with FH in Japan is estimated to be >400,000.673 Although reports from Japan on the accurate diagnosis rate of heterozygous FH are lacking, it is presumed to be low; hence, improving the diagnosis rate of FH is an urgent issue. Notably, when one patient with FH is diagnosed, family screening and early initiation of treatment for family members who are also diagnosed with FH can reduce the incidence of CAD and premature death.
3.2 Genetics of FH
Although genetic testing is not required for the diagnosis of FH, a definite diagnosis can be made if pathogenic mutations in the following LDL receptor-related genes are found in patients with high LDL-C levels. Family members of genetically confirmed FH patients with high LDL-C can be diagnosed with FH as well. From April 2022, genetic testing for patients with suspected FH is covered by insurance in Japan. However, a limited number of domestic facilities can perform genetic testing as of October 2022.
Mutations in the LDL receptor (LDLR), apolipoprotein B-100 (APOB), and the gain-of-function mutation in proprotein convertase subtilisin/kexin type 9 (PCSK9) genes are known to cause FH. Variants of these 3 genes have been confirmed in 60–80% of patients clinically diagnosed with heterozygous FH.674,675 Homozygous FH is defined as having abnormalities in the LDLR, APOB, or gain-of function PCSK9 in both alleles. Autosomal recessive hypercholesterolemia (ARH) is a hereditary disease caused by a pathogenic mutation in the LDLR adaptor protein 1 (LDLRAP1) gene. Individuals with ARH demonstrate clinical features as in homozygous FH, thus they are classified as homozygous FH.
3.3 Diagnosis of FH
3.3.1 Diagnostic Criteria
Table 28 shows the diagnostic criteria for adult patients (age ≥15 years) with FH proposed in “the Japan Atherosclerosis Society Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2022”.39 Family history is important because Achilles tendon thickening may not be prominent, especially in young patients. In addition, because the level of serum LDL-C may decrease temporarily during the acute phase of MI, physical examination of the Achilles tendons and taking a thorough family medical history are important when examining patients with MI.
Table 28.
Diagnostic Criteria for FH in Adults (Age ≥15 Years)
| 1. Serum LDL-C level ≥180 mg/dL |
2. Xanthoma of the tendons (back of the hand, elbow, or knee, among other areas, or thickening of the Achilles tendon) or
cutaneous nodular xanthomas |
| 3. Family history of FH or early-onset CAD (in 1st-degree relative) |
| • Diagnosis is confirmed after excluding other primary/secondary lipid disorders |
| • If the patient is already on medication, the lipid measurement prior to medication use should be referred to upon diagnosis |
• Achilles tendon thickening is based on the following measurements: radiography: ≥8.0 mm for men and ≥7.5 mm
for women; ultrasound: ≥6.0 mm for men and ≥5.5 mm for women |
| • Cutaneous nodular xanthoma does not include eyelid xanthelasma |
• Early-onset coronary artery disease is defined as coronary artery disease that develops in men aged <55 years and
women aged <65 years |
| • FH is diagnosed if ≥2 conditions are met |
• Even if ≥2 conditions are not met, FH is strongly suspected if the LDL-C level is >250 mg/dL or if criterion 2 or 3 is met and
the LDL-C level is >160 mg/dL |
| • FH is diagnosed if a FH pathogenic mutation is detected |
• If homozygous FH is suspected, genetic testing is recommended. Genetic testing is also useful for suspected heterozygous
FH, which is difficult to diagnose |
| • This diagnostic criterion also applies to homozygous FH |
| • If a patient is diagnosed with FH, family screening (cascade screening) is recommended |
CAD, coronary artery disease; FH, familial hypercholesterolemia; LDL-C, low-density lipoprotein cholesterol. (Adapted from Japan Atherosclerosis Society. 2022.39)
The majority of patients with homozygous FH present with a serum TC level ≥600 mg/dL, skin/tendon xanthomas and atherosclerotic disease observed from childhood, and parents with heterozygous FH. Xanthomas in patients with homozygous FH often occur in areas of the body that receive mechanical stimulus such as flexion or friction (e.g., fingers, elbows, knee joints, and buttocks). Because patients with homozygous FH are difficult to distinguish from patients with severe heterozygous FH, genetic testing is recommended for definitive diagnosis.
A change from the diagnostic criteria in the 2017 edition of the guideline is the cutoff value for Achilles tendon thickness. On X-ray imaging, the conventional cutoff of 9 mm (for both men and women) had a high specificity but low sensitivity, which was a major concern for FH diagnosis. In 2021, a new cutoff value (male: 7.6 mm, female: 7.0 mm) was reported in Japan based on findings from the analysis of 986 patients, including 485 genetically diagnosed FH.676 Therefore, the cutoff value has been changed to 8.0 mm for men and 7.5 mm for women in the updated guideline to maintain specificity while enhancing sensitivity. In 2017, the cutoff values for ultrasound Achilles tendon measurements were proposed (male: 6.0 mm, female: 5.5 mm).677 The measurement values for ultrasound Achilles tendon have been also included in the updated 2022 guideline, owing to the progress of its standardized measurement method in recent years.678 Additionally in the updated guideline, patients with either cutaneous/tendon xanthomas or a family history of FH are diagnosed as “suspected FH” if they have an LDL-C level ≥160 mg/dL.
Table 32 (see Chapter III.5.2, in page 52) shows the FH diagnostic criteria for children (aged <15 years) as defined in the Pediatric FH practice guidelines 2022.679 During childhood, the majority of the individuals affected with heterozygous FH exhibit very few physical symptoms; thus, the diagnosis is confirmed based on serum LDL-C level and family history. Furthermore, the new criteria set “probable FH”, different from the Guidance for Pediatric Familial Hypercholesterolemia 2017. Patients are categorized as “FH” or “probable FH” depending on the presence of family history of FH or either a high level of serum LDL or early-onset CAD. The LDL-C cutoff value of 140 mg/dL corresponds to approximately the 95th percentile of all children. Multiple measurements are recommended because LDL-C levels fluctuate during puberty.
3.3.2 Other Primary / Secondary Dyslipidemias to Consider for Differential Diagnosis
In addition to FH, primary dyslipidemias with tendon xanthomas and a high risk of CAD include sitosterolemia680 and cerebrotendinous xanthomatosis.681 Cholesteryl ester storage disease (lysosomal acid lipase deficiency)682 is a lysosomsal storage disease that also present with high level of serum LDL and a high risk of CAD. These 3 conditions should be considered when the parents of the patient are not FH because they are all autosomal recessive disorders.
Diabetes mellitus (DM), hypothyroidism, nephrotic syndrome, cholestatic liver disease, obesity, and drug-induced hypercholesterolemia (e.g., steroids) should also be excluded as conditions that may cause high serum LDL-C concentrations.
3.4 Treatment of Patients With Heterozygous FH (Adults: Aged ≥15 Years) (Figure 7)39
3.4.1 Target LDL-C Level
Because patients with FH are at an extremely high risk for developing CAD, their risk is considered to correspond to secondary prevention for non-FH patients. Therefore, the target LDL-C level for primary prevention among patients with heterozygous FH is set as <100 mg/dL.671 Moreover, because patients with heterozygous FH in secondary prevention are at an even higher risk, the target LDL-C level is set as <70 mg/dL.671 Since it is ethically unacceptable to conduct clinical trials without lipid-lowering treatment in FH, there is no clear evidence for the setting of these control target values.
3.4.2 Lifestyle Modification
It is important for patients with FH to maintain their body weight, quit smoking, and improve their dietary habits. Exercise therapy should be indicated after screening for atherosclerosis prior to initiation.
3.4.3 Medical Therapy
Medical therapy should be initiated at the timing of FH diagnosis because it is difficult for patients with heterozygous FH to achieve the target LDL-C level by lifestyle modification alone. Statins are the first-line agents. A retrospective study of 329 patients with heterozygous FH in Japan showed the association of statin administration and delayed onset of CAD.672 If statins administered at regular doses are ineffective for achieving the target LCL-C level, statin titration as well as the addition of ezetimibe should be considered. If the treatment effect remains insufficient, a PCSK9 inhibitor, anion exchange resin (resin) or probucol should be considered. Reportedly, the additive administration of a PCSK9 inhibitor in patients with heterozygous FH treated with the maximum tolerated dose of statin (+ezetimibe) lowered the LDL-C level by ≈60%.683,684 The LDL-C-lowering effect of PCSK9 inhibitors used among statin-intolerant heterozygous FH patients is reported to be ≈35%.685 Patients who do not achieve the target LDL-C level even after treatment with PCSK9 inhibitors in addition to the maximum tolerated statins should be referred to a specialist immediately, as they may have homozygous FH.
3.4.4 LDL Apheresis (Lipoprotein Apheresis)
In patients with heterozygous FH, LDL apheresis and referral to a specialist should be considered when the TC level is not <250 mg/dL despite treatment with lifestyle modification and rigorous medical therapy.
3.5 Treatment of Patients With Homozygous FH (Figure 8)39
3.5.1 Target LDL-C Level
The risk for the incidence of CAD in patients with homozygous FH is even higher than in those with heterozygous FH. Therefore, aggressive LDL-C lowering treatment as quickly as possible is necessary. The target LDL-C level for primary prevention is <100 mg/dL, and that for secondary prevention is <70 mg/dL; however, these levels are often unattainable in homozygous FH patients. If a patient is suspected of having homozygous FH, it is recommended to consult with or refer to a specialist.
3.5.2 Lifestyle Modification
Maintaining an ideal body weight, smoking cessation, and improving dietary habits are the foundations of treatment even for homozygous FH patients. Screening for atherosclerosis should be performed before guiding exercise therapy because patients may already have CAD, valvular disease (particularly aortic stenosis or supraventricular stenosis), or aortic aneurysm.
3.5.3 Medical Therapy
More aggressive and rapid LDL-C-lowering therapy is necessary in patients with homozygous FH than in those with heterozygous FH. However, since the mechanism of action of most LDL-C-lowering drugs is to enhance LDL receptor activity, it is difficult to achieve sufficient efficacy in FH homozygotes. While LDL-C-lowering effect could be expected, albeit inadequately, in the defective type with some residual LDL receptor activity, almost all conventional lipid-lowering drugs were ineffective in the negative (null) type with almost no residual activity.686,687 Therefore, from a healthcare economics point of view, PCSK9 inhibitors should not be continuously administered to patients in whom the LDL-C level does not decrease after several doses. In contrast, a retrospective study reported that statin treatment for homozygous FH contributed to a reduction in mortality rate.688 Microsomal triglyceride transfer protein (MTP) inhibitors have been shown to reduce LDL-C levels by ≈50% regardless of LDL receptor-activity status.689,690 It should be noted that strict diet therapy and avoidance of alcohol are required to reduce side effects, such as gastrointestinal symptoms and liver dysfunction. Notably, homozygous FH is certified as a designated intractable disease (Notification No. 79) and will receive coverage for the majority of medical expenses, such as PCSK9 inhibitors, MTP inhibitors, and LDL apheresis.
3.5.4 LDL Apheresis (Lipoprotein Apheresis)
In FH homozygotes, LDL-C control targets cannot be reached in most cases, even with aggressive treatment with currently available drugs. Therefore, it is often necessary to undergo LDL apheresis therapy every 1-2 weeks. The earlier LDL apheresis therapy is initiated, the greater the benefit. However, it is safe and realistic to start at age 4-6, when they can lie quietly on the bed.
3.6 Treatment of Children (Aged <15 Years) With Heterozygous FH
Immediately after diagnosis, guidance on improving lifestyle habits should be provided. Pediatric FH patients should be advised never to smoke cigarettes for their entire lives. In addition, it is important that all family members living in the same house not smoke or quit smoking. If lifestyle modification does not reduce LDL-C levels to <180 mg/dL, medical therapy should be considered for patients aged ≥10 years, regardless of sex. Statins are the first-line drug. In Japan, pitavastatin (but not the generic brand) is indicated for FH in children aged ≥10 years of age. The initial dose of pitavastatin is 1 mg and can be titrated up to 2 mg/day. The target LDL-C level is <140 mg/dL; however, this is often difficult to achieve in practice. In patients with a family history of early-onset CAD or sudden cardiac death, or with coexisting DM, aggressive LDL-C-lowering treatment should be administered. For probable FH cases, statins should be administered if the LDL-C level is continuously ≥180 mg/dL. If the diagnosis or treatment cannot be confirmed or is uncertain, patients should be referred to a specialist.
3.7 Treatment for Women With Childbearing Desire
For female patients with FH who wish to become pregnant, preconception evaluation of atherosclerosis, including carotid artery ultrasonography, echocardiography, and adequate preconception counseling (such as the need for a planned pregnancy and medications to be discontinued) are recommended to ensure safe continuation of the pregnancy and delivery. With the exception of resins, other cholesterol-lowering medications are regarded as teratogenic and should be avoided during pregnancy. The same applies to breastfeeding.
Pregnancy in patients with homozygous FH requires further caution regarding pregnancy planning and atherosclerosis assessment using carotid ultrasound and exercise electrocardiogram (ECG). LDL apheresis is recommended during pregnancy because of the marked increase in LDL-C levels and cardiovascular stress during late pregnancy and childbirth. LDL apheresis can be safely performed in pregnant patients with homozygous FH.691
4. Chronic Kidney Disease (CKD; Table 29)
Table 29.
Recommendations and Levels of Evidence for CKD
| |
COR |
LOE |
| CKD stage should be assessed according to the CKD-CGA classification |
I |
C |
| Blood pressure targets |
| CKD with diabetes: <130/80 mmHg (with or Without proteinuria) |
I |
B |
| CKD without diabetes: <140/90 mmHg (for A1 category) |
I |
A |
CKD without diabetes: <130/80 mmHg may be Considered for A2/3 category (to be determined
along with CKD stage) |
IIb |
B |
| Antihypertensive therapy |
CKD regardless of with or without diabetes A1
Category: Any of the following can be considered as the first-line drugs: RAS inhibitors (ARBs
and ACEIs), CCBs, and thiazide diuretics (in the case of eGFR: ≥30 mL/min/1.73 m2) |
IIa |
C |
CKD regardless of with or without diabetes A2/A3: Administer RAS inhibitors (ARBs or ACEIs)
as the first-line drug |
I |
A |
| Lipid-lowering therapy |
CKD with dyslipidemia (hypercholesterolemia): Consider treating with statins alone or in
combination with ezetimibe |
IIa |
B |
CKD with severely decreased kidney function and hypertriglyceridemia may be carefully
treated with pemafibrate, which is primarily excreted via the liver. However, other fibrates are
contraindicated in these CKD patients |
III
(Harm) |
C |
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin-receptor blocker; CCB, calcium-channel blocker; CKD, chronic kidney disease; COR, class of recommendation; LOE, level of evidence; RAS, renin-angiotensin system.
4.1 Definition of CKD
CKD is defined clinically as a pathological condition characterized by persistent kidney damage or decreased kidney function.692 Several clinical studies conducted in Japan and overseas have shown that CKD increases the risk of CVD, such as MI, stroke, heart failure, and death (e.g., cardiorenal linkage). CKD is widely recognized as an important target for the primary prevention of CAD.692–694 In July 2018, the Governmental Policy Statement for CKD (https://www.mhlw.go.jp/stf/shingi2/0000172968_00002.html) was released by the Ministry of Health, Labour and Welfare with the cooperation of academic societies including the Japanese Society of Nephrology, Japanese Circulation Society, Japan Diabetes Society, Japan Medical Association, and municipality and patients’ association. Based on this statement, awareness-raising activities regarding the importance of early detection and early treatment of CKD are being carried out. CKD progresses to end-stage kidney disease (ESKD), which requires dialysis and kidney transplantation. The number of patients requiring chronic dialysis in Japan was ≈348,000 at the end of 2020, with an upward trend. Additionally, the population requiring dialysis is aging each year.695
The estimated number of patients with CKD in Japan is ≈13.3 million,692 which corresponds to 1 in 8 adults having CKD. The prevalence of CKD is particularly high among the elderly.692 There are few subjective symptoms but it can be diagnosed using blood and urine tests. Therefore, early diagnosis of CKD via examinations and laboratory tests at medical institutions is important. The progression of CKD and the onset of CVD should be prevented by providing evidence-based management.692
Notes on the CKD Definition
• Currently, CKD is characterized by the following laboratory test results: (1) urinary abnormalities (the presence of proteinuria is particularly important) and imaging, hematological, and pathological evidence of kidney failure, (2) estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2, or both results, persisting for ≥3 months.
• In clinical practice, the glomerular filtration rate (GFR) in Japanese adults is generally evaluated as the eGFR using the Japanese GFR estimation formula, based on the individual’s serum creatinine (Cr) concentration, age, and sex.692
• The Japanese Society of Nephrology “Evidence-based CKD clinical practice guidelines 2018”692 recommend calculating the GFR using the MDRD (Modification of Diet in Renal Disease) estimation formula developed for Japanese individuals (the MDRD formula was developed primarily for Japanese patients with impaired kidney function and is calculated from the serum Cr concentration, sex, and age).696
• The CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) formula has also been developed for Japanese individuals.697 In a prospective cohort study of the general Japanese population, in which most of them were considered to have normal kidney function, eGFR by the CKD-EPI formula predicted the risk of all-cause death better than the eGFR by the MDRD formula.698
• In addition, in the case of extremely low muscle mass, such as emaciation or amputated lower limbs, the eGFR formula based on the serum cystatin C (Cys-C) level is recommended.699
• Use of Cr clearance (CCr) value alone is discouraged in the evaluation of CKD.
4.2 CKD and CVD Risk: Cardiorenal Linkage
Kidney damage due to CKD increases the risk of ESKD, which requires dialysis and transplantation, and accelerates arteriosclerosis, which increases the risk of CVD (e.g., cardiorenal linkage).692 For example, in a study assessing the risk of death and ESKD according to the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (K/DOQI) stages in a general population of the USA, the risk of death was considerably higher than the risk of progression to ESKD, even in the predialysis stage of CKD.700 In Japan, where the frequency of CVD is said to be lower than in Europe and the USA, a large-scale epidemiological study (the Hisayama study), demonstrated that, in the CKD group (GFR <60 mL/min/1.73 m2), the incidence of CVD was higher than that in the normal kidney function group, and this was in line with the findings from Europe and the USA.701 In a meta-analysis of 14 cohort studies including 105,872 general local residents, the presence of CKD, defined as GFR <60 mL/min/1.73 m2, was associated with the increased risk of CVD and all-cause death. Furthermore, the lower the GFR, the higher the RR.702 Albuminuria is also an important risk factor for CVD and all-cause death independent of kidney function. The risk of CVD and all-cause death is shown to increase with higher levels of albuminuria.702
4.3 Severity Classification for CKD
Historically, the definition of CKD has focused on decreased kidney function (i.e., GFR). In recent years, however, the presence of albuminuria and proteinuria has attracted attention as indicators of kidney structural abnormalities, and both have been shown to be independent risk factors for not only ESKD but also CVD (the higher the albuminuria/proteinuria and lower the GFR, the higher the risk, and the combination of the 2 increases the risk additively).
In the KDIGO 2012 Clinical Practice Guideline for the evaluation and management of CKD703 by the Kidney Disease Improving Global Outcome (KDIGO) group, and in the 2018692 the CKD clinical practice guideline by the Japanese Society of Nephrology, the CKD-CGA severity classification was used to evaluate the risk of not only ESKD but also CVD by combining underlying disease (Cause: C), kidney function (GFR: G), and proteinuria (albuminuria: A). The CKD-CGA grading system uses color coding to indicate the risk of ESKD, CVD, and all-cause death. Green indicates the lowest risk condition as a baseline, and yellow, orange, and red indicate a higher risk of ESKD, CVD, and all-cause death.692
Despite these recommendations, the evaluation of the degree of kidney injury based on glomerular structural abnormalities using albuminuria and proteinuria is yet to be popularized in clinical settings compared with evaluation of the degree of kidney function using the eGFR, particularly among non-nephrologists. Nevertheless, both evaluations are essential for CKD diagnosis and CKD severity assessment (CVD and ESKD risk assessment).704
In the KDIGO guidelines, the use of spot urine urinary albumin determination : urine albumin-to-creatinine ratio (UACR; mg/gCr) is recommended, by which relatively simple and valid measurement values can be obtained. In Japan, the current insurance coverage criterion for the evaluation of albuminuria and proteinuria in patients with diabetes is:
“In patients with diabetes or early diabetic nephropathy, if microalbuminuria is suspected (limited to stage 1 or stage 2 diabetic nephropathy), it can only be calculated once every 3 months.”
Therefore, in Japan, the UACR is recommended in patients with diabetes or early diabetic nephropathy who are suspected to have microalbuminuria (30–299 mg/gCr). The CKD Clinical Practice Guidelines 2018 state that “the presence of proteinuria of 0.15 g/gCr or higher (albuminuria of 30 mg/gCr or higher) is particularly important” for evaluating the degree of kidney impairment. Patients without diabetes are evaluated using the urinary protein-to-creatinine ratio (g/gCr).692 Importantly, urinary protein testing by the dipstick method is not recommended because of the difficulty in evaluating urinary protein when the urine sample is concentrated or diluted.692
4.4 Treatment According to CKD Severity Classification
The risk of ESKD and CVD in patients with CKD steadily increases as the severity of CKD-CGA increases, but the degree of risk differs depending on the underlying disease. For example, according to the findings of the Miyagi Gonryo CKD cohort study conducted in Japan among patients with CKD, if diabetes (diabetic nephropathy) or hypertension (nephrosclerosis) is the primary disease, the risk of CVD (angina pectoris, MI, congestive heart failure, stroke and CVD death) was approximately 5.9- or 3.3-fold greater, respectively, compared with CKD patients with nephritis as the primary disease.705 Therefore, to reduce the risk of CVD in patients with CKD, both direct treatment to suppress CKD progression, and treatment of the risk factors for CKD progression and CVD development are necessary.
4.4.1 Treatment for CKD Progression/Risk Factors of CVD
The management of coronary risk factors, such as hypertension, diabetes, dyslipidemia, and smoking, for the primary prevention of CAD remains important in CKD patients as it does in the non-CKD patients. Among the treatments for hypertension, diabetes, dyslipidemia, hyperuricemia, mineral and bone disorders (MBDs), and kidney anemia in patients with CKD, the appropriate treatment for hypertension is recommended in particular for the primary prevention of CAD.
a. BP Management (Figure 9)
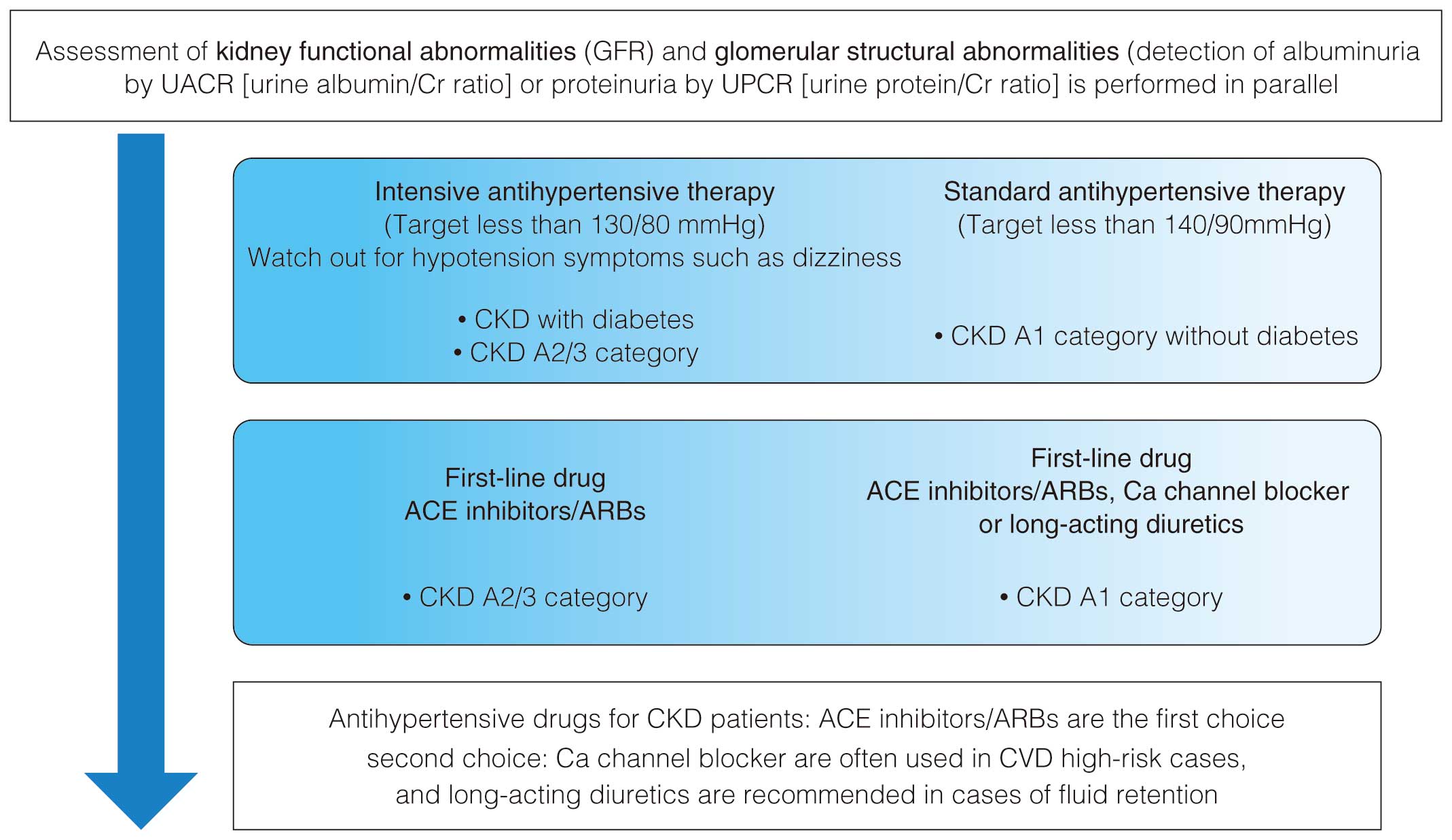
Among RCTs comparing strict vs. standard antihypertensive therapies in CKD patients with respect to BP goals, the STEP study of 8,511 hypertensive patients, aged 60–80 years (mean age: 66.2 years), most of whom had normal kidney function, was conducted in China. A strict antihypertensive group (SBP 110–130 mmHg; mean age 66.2 years; 24.1% participants aged 70–80 years; 2.4% kidney dysfunction) and a standard antihypertensive group (SBP 130–150 mmHg; mean age 66.3 years; 24.2% participants aged 70–80 years; 2.3% kidney dysfunction) were compared.81 In that study, the incidence of primary composite outcome (stroke, ACS [acute myocardial infarction (AMI) and hospitalization for unstable angina], acute decompensated heart failure, coronary revascularization, atrial fibrillation, or death from cardiovascular causes) was lower (HR 0.74 [95% confidence interval (CI) 0.60–0.92]) in the strict antihypertensive group, during a median observation period of 3.34 years.81 Hypotension was more common in the strict antihypertensive group, but no difference was observed between groups with respect to other side effects and renal composite outcomes (decreased kidney function and progression to ESKD).704 To summarize, in the STEP study, strict antihypertensive treatment for hypertension in elderly patients aged 60–80 years led to a CVD-protective effect, whereas a CKD-protective effect was not clearly observed.81
Following the STEP study, the SPRINT trial studied 9,361 nondiabetic high-risk hypertensive patients (average age 67.9 years, 28.2% patients aged >75 years, 28.3% patients with CKD [excluding eGFR <20], 20.0% patients with a history of CVD). In a subanalysis in the final report, a comparison was made between the strict antihypertensive group (SBP <120 mmHg) and the standard antihypertensive group (SBP <140 mmHg) over an integrated observation period (median 3.88 years), which included the initial intervention period (median 3.33 years) and the post-trial follow-up period.80 During the intervention period, both the incidence of primary composite outcomes (cerebrovascular disease, acute heart failure, and cardiovascular death) and all-cause death were significantly lower in the strict antihypertensive group: The primary composite outcome was 1.77% in the strict antihypertensive group and 2.40% in the standard antihypertensive group (HR 0.73; 95% CI 0.63–0.86), and the all-cause death was 1.06% in the strict antihypertensive group and 1.41% in the standard antihypertensive group (HR 0.75; 95% CI 0.61–0.92). A similar reduction in the primary composite outcome and all-cause death was also observed over the integrated observation period: The primary composite outcome was 1.84% in the strict antihypertensive group and 2.43% in the standard antihypertensive group (HR 0.76; 95% CI 0.65–0.88), and all-cause death was 1.23% in the strict antihypertensive group and 1.55% in the standard antihypertensive group (HR 0.79; 95% CI 0.66–0.94).80 Conversely, acute kidney injury (AKI) was more common in the strict antihypertensive group during the consolidation period: 1.3% in the strict antihypertensive group and 0.8% in the standard antihypertensive group (HR 1.69; 95% CI 1.37–2.10). A significant increase was also observed in the incidence of kidney dysfunction (≥30% decline in the eGFR persisting for ≥90 days) in hypertensive patients with normal kidney function: 1.29% in the strict antihypertensive group and 0.39% in the standard antihypertensive group (HR 3.34; 95% CI 2.44–4.66).80 This evidence indicates that strict antihypertensive treatment may increase the risk of AKI while reducing CVD and all-cause death.80
Considering the evidence, with respect to the target BP for patients with CKD with hypertension, from the perspective of suppressing ESKD progression and CVD incidence, the following are recommended:74,692
• CKD with diabetes:
<130/80 mmHg with or without proteinuria
• CKD without diabetes:
<140/90 mmHg for proteinuria A1 (by the CKD-CGA severity classification)
<130/80 mmHg for proteinuria A2/A3 (the CKD-CGA severity classification).
The recommendations are in accordance with the BP reduction goals of the CKD clinical practice guideline 2018 and hypertension treatment guideline 2019 (JSH2019). Further, it should also be noted that the SBP and DBP values measured at home are 5 mmHg lower than the BP values measured in the clinic.74
With respect to the low limit of BP targets, findings from the Gonryo study, a prospective CKD cohort study in Japan, observed that the risks of CVD (including cerebrovascular disease) and all-cause death before initiating renal replacement therapy (kidney transplantation, peritoneal dialysis, and hemodialysis) were higher in patients with BP <110/70 mmHg than in the patients with BP 130–139/80–89 mmHg.706 From the perspective of AKI prevention, the 2018 Clinical Practice Guidelines for CKD proposes to avoid lowering the SBP to <110 mmHg, regardless of the presence or absence of diabetes and the CKD stage.692 However, older people are particularly varied in their medical conditions and should be judged individually. For this reason, a specific low BP goal is not prescribed for older people.
As for the nonpharmacological therapeutic strategies for lowering BP, the CKD Clinical Practice Guidelines 2018 recommend restricting salt intake to <6 g/day for controlling hypertension and proteinuria and preventing CVD in patients with CKD. However, the excessive reduction in salt intake may be harmful; hence, setting an individualized low limit for salt intake is recommended with a limit of 3 g/day as a guide.692 From the pharmacotherapeutic perspective, the CKD Clinical Practice Guidelines 2018 and JSH2019 recommend the following:74,692
• In proteinuria A1 with or without diabetes, one of the following drugs should be administered as the first-line drug: renin–angiotensin system inhibitors (angiotensin-receptor blockers or ACE inhibitor inhibitors), calcium-channel blockers, or thiazide diuretics (eGFR ≥30 mL/min/1.73 m2).
• Administration of renin–angiotensin system inhibitors (angiotensin-receptor blockers or ACE inhibitor inhibitors), as the first-line drug for proteinuria A2/A3, regardless of the absence or presence of diabetes.
b. Lipid Management
Lipid-lowering therapy with statins alone and in combination with ezetimibe has been reported to suppress the deterioration of proteinuria and kidney function and prevent CVD incidence in patients with CKD and dyslipidemia. These drugs are recommended in the CKD Clinical Practice Guidelines 2018.692 Thus, CKD with dyslipidemia (hypercholesterolemia) should be treated with statins alone or in combination with ezetimibe.
On the other hand, CKD with severely decreased kidney function and hypertriglyceridemia may be carefully treated with pemafibrate, a selective peroxisome proliferator-activated receptor-α modulator (SPPARMα) primarily excreted via the liver. However, other conventional fibrates are renally excreted, and thus contraindicated in such CKD patients. Additional evidence of pemafibrate regarding its effectiveness and safety in CKD patients is expected from future studies.
4.4.2 New Drugs for CKD Treatment
a. Sodium Glucose Cotransporter 2 (SGLT2) Inhibitors
Currently, the efficacy of SGLT2 inhibitors in patients with CKD without diabetes and proteinuria is not supported by sufficient evidence. Conversely, the Japanese Society of Nephrology recommends SGLT2 inhibitors as a treatment for patients with diabetic kidney disease (DKD) and eGFR ≥25 mL/min/1.73 m2. However, this is a recommendation for improving and maintaining kidney function, and the evidence regarding the primary preventive effect on CAD is insufficient, as detailed below.
At present, early-stage clinical research on therapeutic drugs for CKD is being conducted in both Japan and overseas. In the DAPA-CKD study, 4,304 patients with or without type 2 diabetes (eGFR 25–75 mL/min/1.73 m2, UACR 200–5,000 mg/gCr) (386 centers including Japan and 21 other countries) were studied. The effects of treatment with 10 mg of the SGLT2 inhibitor dapagliflozin administered once daily were investigated.707 The Data Monitoring Committee determined a clear efficacy in the dapagliflozin group compared with the placebo group, and the trial was terminated early. The primary composite endpoint [≥50% eGFR decline + ESKD (maintenance dialysis initiation, kidney transplantation, eGFR <15 mL/min/1.73 m2) + death from kidney disease + cardiovascular death] at a median duration of 2.4 years occurred in 197 (9.2%) individuals in the dapagliflozin group and 312 (14.5%) individuals in the placebo group [HR 0.61 (95% CI 0.51–0.72, P<0.001); NNT (number needed to treat) = 19 (95% CI 15–27)].707 Similar results were obtained in a subgroup analysis limited to G4 patients with severe kidney function impairment.707,708
The HR for the secondary composite endpoint (cardiovascular death + hospitalization for heart failure) in the dapagliflozin group (vs. placebo group) was 0.71 (95% CI 0.55–0.92, P=0.009). All-cause death occurred in 101 (4.7%) individuals in the dapagliflozin group and 146 (6.8%) individuals in the placebo group [HR 0.69 (95% CI 0.53–0.88, P=0.004)]. Dapagliflozin treatment reduced the risk of both ESKD and CVD, including heart failure, in patients with CKD in the DAPA-CKD trial.707 The reduction in the primary composite endpoint [50% or more eGFR decline + ESKD (maintenance dialysis initiation, kidney transplantation, eGFR <15 mL/min/1.73 m2) + death from kidney disease + cardiovascular death] in the dapagliflozin arm was similar to that in CKD patients with or without type 2 diabetes.707,708 Based on the evidence from the study, the US Food and Drug Administration approved the expanded indication of the SGLT2 inhibitor dapagliflozin for CKD. In Japan, the use of dapagliflozin was approved for additional indications for “chronic kidney disease (excluding end-stage kidney failure or patients undergoing dialysis)”, regardless of the presence or absence of type 2 diabetes.
Currently, dapagliflozin is the only SGLT2 inhibitor that has been shown to be effective in treatment for CKD, and thus covered by health insurance, regardless of the presence or absence of type 2 diabetes. As a treatment for improving and maintaining kidney function against CKD, it is considered a treatment option for patients with CKD and eGFR ≥25 mL/min/1.73 m2.707 However, in the DAPA-CKD trial, a reduction was observed only in the composite endpoint of cardiovascular death and hospitalization due to heart failure, but not in isolated cardiovascular death.707 Therefore, the primary preventive effect of dapagliflozin for CAD in patients with CKD cannot be confirmed. At this point of time, therefore, the administration of SGLT2 inhibitors, such as dapagliflozin, is not recommended for the purpose of primary prevention of CAD in patients with CKD.
Detailed usage of SGLT2 inhibitors for CKD is provided in the Japan Diabetes Society’s Recommendations for proper use of sglt2 inhibitors (http://www.jds.or.jp/modules/important/index.php?content_id=48).709 However, when using such a reference, careful consideration is required when administrating the drug to the elderly, frail patients, and patients with impaired consciousness and communication problems, who are at a high risk of dehydration. Also, in the DAPA-CKD trial, the exclusion criteria were as follows: type 1 diabetes, polycystic kidney disease, lupus nephritis, antineutrophil cytoplasmic antibody-associated vasculitis, and immunotherapy for primary/secondary kidney disease within the past 6 months. Attention should be paid to these conditions as well.707
b. Nonsteroidal Selective Mineralocorticoid Receptor Antagonists (MRAs)
For the MRA finerenone, in integrated clinical trials (FIGARO-DKD, FIDELIO-DKD, and prespecified pooled analysis FIDELITY) in CKD patients with type 2 diabetes, including Japanese, improvements were observed in primary composite endpoints of kidney condition (endstage kidney failure, eGFR decline by ≥40%, and kidney death) and cardiovascular conditions (cardiovascular death, non-fatal MI, non-fatal stroke, and hospitalization for heart failure) in patients with CKD with type 2 diabetes, regardless of CKD severity or the concomitant use of SGLT2 inhibitors. Therefore, in March 2022, finerenone was approved for manufacturing and marketing in Japan with an indication for CKD with type 2 diabetes.710–712 The most commonly reported adverse reactions include hyperkalemia, hypotension, and decreased GFR (increased blood Cr). However, in both the FIGARO-DKD and FIDELIO-DKD trials, hospitalization for heart failure was the only cardiovascular composite endpoint (among cardiovascular death, non-fatal MI, non-fatal stroke, and hospitalization for heart failure) that demonstrated a significant reduction. No significant protective effects were observed for the other components (cardiovascular death, non-fatal MI, and non-fatal stroke) in the finerenone-treated group.710–712 Therefore, the primary preventive effect of finerenone in CAD in patients with CKD is yet to be confirmed. At present, the administration of MRAs, such as finerenone, is not recommended for the primary prevention of CAD in patients with CKD.
5. Children
Preface
Pathological studies of the coronary arteries in children and young adults have shown that atherosclerosis can be observed from childhood. In autopsy cases of children, the greater the number of prenatal cardiovascular risk factors, the larger the area of atherosclerotic lesions.713 The key to the prevention of CAD is a combination of a healthy lifestyle, performing appropriate screening tests for pediatric lifestyle-related diseases, and providing early intervention for patients with signs of atherosclerotic development.714 In Japan, many children are born with a low birth weight that is associated with higher risk for developing noncommunicable diseases, such as obesity and ischemic heart disease, later in life.715,716 Furthermore, it is necessary to improve our understanding of diseases such as FH, in which atherosclerosis progresses from childhood, and anomalous coronary arteries, which can cause coronary artery events in children.
5.1 Hypertension
In children, normal BP varies according to the individual’s age, sex, and height. In the 2019 Japanese Society of Hypertension Guidelines for the management of hypertension (JSH2019), the criterion for pediatric hypertension has been set by age and sex category (Table 30).74 The JSH2019 guideline defined new BP categories for adults: “high normal BP” (SBP 120–129 and DBP <80 mmHg using office BP measurement) and “elevated BP” (SBP 130–139 and/or DBP 80–89) given the elevated risk for cardiocerebrovascular deaths among adults. However, the same categorization has not been set for children. Considering the tracking of pediatric BP to adults (i.e., elevated BP in childhood is associated with hypertension in adulthood),717 it is necessary to establish a pediatric “prehypertension” criteria for the primary prevention of CAD in Japan.
Table 30.
Hypertension Criteria for Children by Age Group and Sex
| |
Systolic blood
pressure (mmHg) |
Diastolic blood
pressure (mmHg) |
| Pre-school children |
≥120 |
≥70 |
| Elementary school |
|
|
| First to third graders |
≥130 |
≥80 |
| Fourth to sixth graders |
≥135 |
≥80 |
| Junior high-school |
|
|
| Boys |
≥140 |
≥85 |
| Girls |
≥135 |
≥80 |
| High-school |
≥140 |
≥85 |
(Adapted from “The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH2019)”.74)
BP measurement for children is recommended to be performed ≥3 times using an appropriate-size cuff. However, because there are limited opportunities for measuring BP during childhood, it is important for school cardiac examinations and well-child visits to be able to screen for children with high BP to prevent CAD.
Evidence for the Pediatric Hypertension Criteria
• In children, it is difficult to establish specific BP levels based on the future risk of CVD development. In Europe and the USA, BP levels are set at the 90th/95th percentile or greater for each age from birth as “high normal BP”/“hypertension”, respectively, and are recommended for close follow-up.718,719
• The 95th percentile values in a pediatric epidemiological study of BP in Japan (Mitsuke study) were 10–15 mmHg lower than the values defining “hypertension” for children in the JSH2019. The 90th percentile (in mmHg), a reference for the “high normal BP”, were approximately 105/60, 115/60, 130/70, and 125/70 for children in lower grades of elementary school, upper grades of elementary school, junior high school boys, and junior high school girls, respectively. According to the JSH2004 criteria (same as the JSH2019), the frequency of hypertension in all children ranges from 0.1% to 3%, and that in children with obesity ranges from 3% to 5%.720,721
Hypertension causes carotid intima–media thickening and left ventricular hypertrophy even in children.722,723 Low birth weight is associated with the development of hypertension, which is thought to be caused by decreased number of nephrons and increased insulin resistance.724,725 The basic treatment of essential hypertension in children includes body weight reduction for overweight/obese children and lifestyle-modification, such as an adherence to healthy diet and exercise. High dietary salt intake is associated with elevated BP, and reduction in salt intake is important.726 The antihypertensive medications indicated for use in children are some of the following: calcium-channel blockers, ACE inhibitors, and angiotensin-receptor blockers.74
5.2 Dyslipidemia
Blood cholesterol levels vary by age and sex, and they temporarily decrease among boys during puberty. The criterion for dyslipidemia in Japanese children is based on the 95th percentile (mg/dL) value in the national pediatric serum lipid survey: a TC level ≥220 mg/dL, a LDL-C level ≥140 mg/dL, a triglyceride level ≥140 mg/dL, a HDL-C level <40 mg/dL, and a non-HDL-C level ≥150 mg/dL.727,728
Pediatric dyslipidemia causes early coronary atherosclerosis in adolescents to young adults, so it is considered an important risk factor in the primary prevention of CAD.729 For dyslipidemia associated with childhood obesity and metabolic syndrome, lifestyle-modifications such as adherence to healthy diet, exercise, and anti-obesity measures are the basic recommendations. With increasing awareness of the importance of early diagnosis, the guidelines for pediatric FH were first established in Japan in 2017. Our recommendation on pediatric FH is shown in Table 31. The diagnostic criteria for pediatric FH in the revised Pediatric familial hypercholesterolemia treatment guide 2022 recommend the diagnosis be based solely on cholesterol level regardless of FH family history for suspected cases (Table 32).679,730,731 In addition to conventional cascade screening, diagnosis by universal screening is gaining importance.731 In Japan, medical examinations for the prevention of pediatric lifestyle-related diseases are an important opportunity for universal screening of dyslipidemia and FH. Reportedly, in medical examinations for 4th graders (children aged 9–10 years), the frequency of children with an LDL-C concentration ≥180 mg/dL (“suspected FH” even without other criteria being met) is 0.3–0.4%.732,733 Limited evidence is available to indicate that early diagnosis and treatment of FH during childhood reduces incident CAD at the population level.734,735 However, early treatment should be considered for the primary prevention of CAD at the individual level (see Table 31 for recommendation). Statins are the first-line drug used in children.736 In Japan, since 2015, pitavastatin has been indicated for children aged ≥10 years, and its safety and efficacy have been reported737 (see also Chapter III.3 for more information).
Table 31.
Recommendation and Level of Evidence for Pediatric FH Treatment
| |
COR |
LOE |
For cases of pediatric FH with a strong family history of early-onset coronary artery disease
or a persistent LDL-C level ≥180 mg/dL, treatment is considered from the age of 10
years, at which point statins are indicated |
IIa |
C |
COR, class of recommendation; FH, familial hypercholesterolemia; LDL-C, low-density lipoprotein cholesterol; LOE, level of evidence.
Table 32.
Diagnostic Criteria for FH in Children (Age <15 Years)
| 1. High serum LDL-C level (LDL-C ≥140 mg/dL prior to medical treatment, confirmed multiple times) |
| 2. Family history of FH (parents or siblings) |
| 3. LDL-C level ≥180 mg/dL observed in the individual’s parents or family history of premature CAD (in grandparents or parents) |
| First, exclude other primary and secondary causes of high serum LDL-C level |
| If criteria 1 and 2 are present, FH is confirmed |
| If criteria 1 and 3 are present, FH is suspected. Diagnose FH if the patient’s LDL-C level is ≥180 mg/dL |
| Even if only criterion 1 is present, diagnose FH for an LDL-C level ≥250 mg/dL, and probable FH for an LDL-C level ≥180 mg/dL |
| • If the LDL-C level is ≥250 mg/dL or xanthomas are present, differentiate the condition from homozygous FH |
• Diagnose FH if the patient has a FH pathogenic mutation. If the FH pathogenic mutation is identified in the patient’s parents or
siblings, add this information to the family history (criterion 2) |
| • Early-onset CAD is defined as CAD that develops in men aged <55 years and women aged <65 years |
| • Probable FH cases require further scrutiny and lipid-lowering therapy |
CAD, coronary artery disease; FH, familial hypercholesterolemia; LDL-C, low-density lipoprotein cholesterol.
(Adapted from Japan Pediatric Society, Japan Atherosclerosis Society. Guidelines for the Diagnosis and Treatment of Pediatric Familial Hypercholesterolemia 2022. [in Japanese],679 Japan Atherosclerosis Society, Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2022 [in Japanese], Japan Atherosclerosis Society, 2022.731)
5.3 Obesity and Metabolic Syndrome
In addition to hypertension, dyslipidemia, and diabetes, which are typical cardiovascular risk factors, childhood obesity is gaining much attention as a risk factor.738 Excessive visceral fat accumulation, causes hypertension, dyslipidemia, abnormal glucose metabolism, blood coagulation, and systemic chronic inflammation through modulation of the adipocytokine balance.739 Further, childhood obesity increases the risk of CAD in adulthood.740
In Japan, obesity is traditionally defined based on the calculation formula developed by Murata et al (percentage of overweight = {(measured weight-standard weight) / standard weight} × 100), and not the formula used to calculate BMI among adults. Using the percentage of overweight calculated from this formula, the infant age group is judged as “obese” if the percentage of overweight is +15% (115% of the standard weight) or higher, and the age group between 6 and 18 years old is judged as “obese” if the percentage of overweight is +20% (120% of the standard weight) or higher. In Europe and the USA, BMI percentile values and Z-scores are used to determine obesity in children.
In Japan, the gold standard for visceral fat obesity in children is defined as visceral fat area ≥60 cm2
at the umbilical level on abdominal CT.741 Waist circumference at the umbilicus level (umbilical circumference) is used as a simple method to assess abdominal obesity. Abdominal obesity is diagnosed when the waist–height ratio = umbilical circumference (cm) / height (cm) is ≥0.5 after the age of 6 years if the waist circumference is ≥75 cm in students in elementary school or ≥80 cm in students in junior high school.742 However, it is important to assess child physical development over time using growth curves from their height and weight, and an obesity curve to estimate changes in physical constitution and the effects of interventions.743
The criteria for childhood obesity disease were established in 2002 after the establishment of the criteria for adult obesity disease in 2000.744 The diagnostic criteria revised in 2014 are currently used (Table 33).745 Similarly, the diagnostic criteria for metabolic syndrome in children and adults are shown in Table 34.231,746 The key common pathophysiology in pediatric obesity and metabolic syndrome is excessive visceral fat accumulation. Association between increased common carotid artery (CCA) stiffness and excessive visceral fat accumulation at 10 years of age, and increased CCA intima–media thickening after 21 years of follow-up and greater number of coronary risk factors detected at 12–18 year of age have been reported.747,748
Table 33.
Diagnostic Criteria for Pediatric Obesity
Definition of obesity in
children |
≥20% obesity and significantly high body fat percentage
*Significantly increased body fat percentage in:
Boys: >25% at any age; Girls: >30% at age <11 years, >35% at age >11 years |
| Definition of obesity |
A medical condition in which health impairments (medical abnormalities) either caused by or associated with
obesity are present and medical attention to reduce obesity is necessary. It is treated as an illness |
| Applicable age range |
6 years 0 months to 18 years |
| Diagnosis of obesity |
(1) Individuals with ≥1 condition from A
(2) Individuals with obesity >50% and ≥1 condition from B
(3) Individuals with obesity <50% and ≥2 conditions from B
(≥2 items from the Reference section are to be treated as 1 condition from B) |
Health impairments
associated with obesity
included in the
diagnostic criteria |
A:
1) Hypertension
2) Respiratory impairment, including sleep apnea
3) Type 2 diabetes/impaired glucose tolerance
4) Visceral fat obesity
5) Early-onset atherosclerosis
B:
1) Nonalcoholic fatty liver disease (NAFLD)
2) Hyperinsulinemia and/or acanthosis nigricans
3) HyperTCemia and/or hyper non-HDL-cholesterolemia
4) Hyper-triglyceridemia and/or low HDL-cholesterolemia
5) Hyperuricemia |
Reference items
1) Dermatological findings, including streaking on
the skin
2) Motor organ impairment caused by obesity
3) Dysmenorrhea
4) Truancy, bullying related to obesity
5) Low or high birth weight of infants
Refer to the supplement to “Table C. Health
impairments necessary for the diagnosis of pediatric
obesity” available on the homepage of the Japan
Society for the Study of Obesity for specific cutoff
values for health impairments necessary for diagnosis* |
*http://www.jasso.or.jp/data/magazine/pdf/pediatricobesityguidelines2017_chart_C.pdf
(Modified from Childhood Obesity Practice Guidelines 2017 [in Japanese], Japan Society for the Study of Obesity, 2017.745)
Table 34.
Diagnostic Criteria for Metabolic Syndrome in Adults and Children
| |
Adults |
Children |
Joint Committee of
8 Societies (2005) |
Health, Labour and Welfare
Sciences Research (2007) |
| (1) Waist circumference |
≥85 cm (male)
≥90 cm (female) |
≥80 cm (both sexes)
Note: waist-height ratio is ≥0.5
For elementary school students, a minimum of
75 cm meets the criteria |
| (2) Serum lipids |
TG ≥150 mg/dL
and/or
HDL-C <40 mg/dL |
TG ≥120 mg/dL
and/or
HDL-C <40 mg/dL |
| (3) Blood pressure |
SBP ≥130 mmHg
and/or
DBP ≥85 mmHg |
SBP ≥125 mmHg
and/or
DBP ≥70 mmHg |
| (4) Fasting blood glucose |
≥110 mg/dL |
≥100 mg/dL |
Metabolic syndrome is diagnosed when (1) is a required item and at least 2 of (2), (3), or (4) is present.
(Sources: Prepared based on findings from the Definition and the diagnostic standard for metabolic syndrome. [in Japanese] Nihon Naika Gakkai Zasshi 2005; 94: 794–809,231 and the Cohort study on the establishment of the concept, pathophysiology, and diagnostic criteria of metabolic syndrome in childhood and effective intervention by the Ministry of Health, Labour, and Welfare research group.746)
Based on the childhood obesity diagnostic criteria revised in 2014, the prevalence of abdominal obesity was the highest among other coronary risk factors during health check-up in 2019 among 2,630 elementary school students in Suginami ward, Tokyo, with hypertension at 1.7%, dyslipidemia at 8.2%, high HbA1c at 2.1% and abdominal obesity at 11.9%.749
The implementation of anti-obesity measures from childhood onwards is crucial for the prevention of CAD.
5.4 Abnormal Glucose Metabolism/Type 2 Diabetes (Table 35)
Table 35.
Recommendation and Level of Evidence for Abnormal Glucose Metabolism/Diabetes in Children
| |
COR |
LOE |
Prevention of childhood obesity and type 2 diabetes and appropriate treatment
management should be considered to prevent CAD |
IIa |
B |
CAD, coronary artery disease; COR, class of recommendation; LOE, level of evidence.
The incidence of childhood-onset type 2 diabetes, which is strongly associated with obesity, is increasing worldwide.750 In Tokyo, according to the results of universal screening using a urine examination system in schools, the number of children with type 2 diabetes had more than tripled in 20 years (since 1974) in parallel with the increase in the number of children with obesity.751 Similar to adult diabetes, the diagnoses of pediatric diabetes can be categorized as: (1) diabetes, (2) borderline diabetes, and (3) normal according to the fasting plasma glucose (FPG) level, 2-h value in the oral glucose tolerance test (OGTT), random blood glucose level, and HbA1c level.752 Of note, if the FPG level is in the range of 100 to <110 mg/dL, it is considered a high normal value in adults; however, according to the childhood metabolic syndrome diagnostic criteria, an FPG level ≥100 mg/dL indicates fasting hyperglycemia and further assessment with OGTT is recommended.
Type 2 diabetes in children is strongly associated with obesity, and such children are also more likely to have hypertension and dyslipidemia. Persistent hyperglycemia increases the risk of CAD and stroke, as well as retinopathy, nephropathy, and neuropathy. A study of American children showed that the prognosis of childhood-onset type 2 diabetes patients after 15 years was worse than that of type 1 diabetes patients, with cardiovascular events reported in 3.7 per 1,000 patients.753 The prevention of obesity/diabetes from childhood and appropriate treatment management are necessary (Class IIa, Level B).
5.5 Pediatric Conditions That May Cause Sudden Cardiac Death
5.5.1 Kawasaki Disease (Table 36)
Table 36.
Recommendations and Levels of Evidence for Kawasaki Disease
| |
COR |
LOE |
Aspirin should be administered to patients with residual coronary artery aneurysm or a history of
moderate or large aneurysm as sequelae of Kawasaki disease |
I |
C |
Warfarin should be administered in patients with a large aneurysm, a history of acute myocardial
infarction, or a left ventricular thrombus |
I |
C |
| Statins or ACEIs may be considered for patients with coronary aneurysms |
IIb |
C |
ACEI, angiotensin-converting enzyme inhibitor; COR, class of recommendation; LOE, level of evidence.
Kawasaki disease is a systemic medium-sized vasculitis of unknown cause that most frequently affects children before preschool age. The prognosis of Kawasaki disease patients largely depends on the formation of coronary aneurysms due to the strong inflammation in the coronary arteries. Once a coronary aneurysm is formed, vascular remodeling continues until adulthood. Evidence shows that the larger the diameter of the aneurysm, the higher the risk of cardiac events.754 Even when the size of the aneurysm does not change or when the aneurysm regresses, a patient with a history of moderate to large (Z score ≥5.0) coronary aneurysm will require lifelong follow-up.755
The effects of Kawasaki disease on the cardiovascular system in the remote stage include (1) ACS due to thrombotic occlusion, (2) coronary artery stenosis/occlusion owing to long-term vascular remodeling, and (3) risk of early atherosclerosis progression. Therefore, the primary prevention of coronary artery events should be provided by antiplatelet therapy with aspirin (Class I, Level C). Anticoagulant therapy with warfarin is administered to those patients with a large aneurysm, a history of AMI or intra-aneurysm thrombus (Class I, Level C). Thrombosis also may be prevented with direct oral anticoagulants (DOACs), although no evidence is available.
In addition, the use of ACE inhibitors and ARBs for suppressing vascular remodeling has been reported, although the long-term prognosis with this treatment is unknown. Owing to the risk of early atherosclerosis development, lifestyle-modification is recommended to suppress atherosclerosis risk factors. Based on the large body of evidence on anti-atherosclerosis treatment in adults, the USA and Japanese guidelines for Kawasaki disease recommend the use of ACE inhibitors and statins (Class IIb, Level C) in patients with coronary aneurysms.755,756 However, currently, clear evidence to indicate the ideal time for treatment initiation or conditions that necessitate ACE inhibitor or statin therapy is unavailable.
Kawasaki disease needs to be medically managed continuously from pediatrics to internal medicine. However, interruption of regular follow-up or “drop-out” is a major issue associated with the treatment of this disease. General physicians should both check for patients with a history of Kawasaki disease-induced coronary aneurysm so they do not to miss regular follow-up and encourage referral of patients to appropriate medical institutions in such cases.
5.5.2 Congenital Coronary Anomalies
a. Congenital Coronary Anomalies as the Cause of Sudden Death
i. Sudden Cardiac Death in School Children and Young Individuals
The annual incidence of sudden death in children in schools in Japan is approximately 0.2 per 100,000 students.757–760 Among such cases, sudden cardiac death accounts for 75% of sudden deaths occurring during exercise.760,761
ii. Congenital Coronary Anomalies and Their Classification
Hypertrophic cardiomyopathy and congenital coronary anomalies are the most common causative conditions of pediatric sudden cardiac death.758,759 In congenital coronary anomalies, especially those in which the coronary artery originates from the contralateral coronary sinus, the central side of the coronary artery may run intramurally through the aortic wall. It may also be present between the pulmonary artery and aorta. The increased internal pressure and dilation of both large vessels during exercise compress the coronary arteries running abnormally, causing sudden cardiac death due to myocardial ischemia. Because the first symptom of this condition may be sudden cardiac death, it can be difficult to evaluate the risk based on pre-event symptoms or by performing an exercise stress test. The risk of sudden death is considered to be high when the orifice of the coronary artery is slit-like and narrow or when the coronary artery travels a long intramural course through the aortic wall.762
b. Limitations of Detection in School Heart Disease Screening
i. Limitations of ECG Screening
Most resting ECGs in patients with anomalous coronary arteries yield normal findings, so it is difficult to detect these abnormalities using the school heart disease screening system.763,764
ii. Imaging Diagnosis (Table 37)
Table 37.
Recommendations and Levels of Evidence for Congenital Coronary Anomalies
| |
COR |
LOE |
| Transthoracic echocardiography is recommended as a screening test |
I |
B |
| Coronary CT angiography is recommended if echocardiography is insufficient as a diagnostic measure |
IIa |
B |
COR, class of recommendation; CT, computed tomography; LOE, level of evidence.
Transthoracic echocardiography is recommended as a screening test.765,766 Coronary CT angiography is recommended if echocardiography is insufficient as a diagnostic measure.765–767
5.6 Cigarette Smoking (Table 38)
Table 38.
Recommendation and Level of Evidence for Smoking Prevention/Antismoking Education for Children
| |
COR |
LOE |
Early education for smoking prevention should be considered for children at the
pre-smoking stage to reduce the rate of adult smokers |
IIa |
B |
COR, class of recommendation; LOE, level of evidence.
The effects of parental smoking on children are first induced during the fetal period. Smoking by pregnant women and secondhand smoke lead to inhibition of fetal growth by the vasoconstrictive action of nicotine and lowering of oxygen levels due to the presence of carbon monoxide. It may lower birth weight, which can increase the risk of lifestyle-related diseases in the future.768,769
Evidence Related to the Effects of Smoke Inhalation on Blood Vessels in Childhood
• Passive smoking in infants and children decreases the HDL-C level, increases the carotid IMT, decreases vascular endothelial function, and promotes early atherosclerosis.770,771
• In younger people, an earlier age of smoking initiation is associated with a more rapid development of nicotine dependence, and a greater frequency and duration of smoking is associated with a greater risk of CAD.772,773
Although the rate of cigarette smoking is declining in young people, the increasing use of new types of tobacco-related product, such as heat-not-burn tobacco and electronic cigarettes, is a growing concern.774–776 Smoking prevention and cessation education for young individuals will help reduce the proportion of persons who start smoking. However, it will not reduce the proportion of current smokers who will stop smoking.777 Table 38 lists the recommendations for early smoking prevention education as a primary preventive measure for CAD.
5.7 Other Lifestyle Habits (Diet / Exercise / Sleep)
5.7.1 Diet
With respect to dietary habits in childhood, the age, sex, and physical activity of children should be considered, as well as the intake of appropriate energy and nutrients. Limiting excess fat, simple carbohydrates, and sodium should be considered. In particular, the essentials of an appropriate diet for children are given in reference to the estimated energy requirements according to the Japanese Dietary Intake Standards 2020 (Dietary Intake Standards 2020): the total amount of energy should be determined, and a distribution of 20% protein, 20–30% fat, and 50–60% carbohydrate should be followed.778
• The type of fat ingested is also important. Excessive intake of saturated fatty acids (SFAs), primarily present in meat, raises the LDL-C level in the blood. The ingestion of polyunsaturated fatty acids (PUFAs) in plant seeds and blue-backed fish reduces the LDL-C level.
• The physiological action differs depending on the type of PUFA ingested. n-6 PUFAs are pro-inflammatory, whereas n-3 PUFAs are anti-inflammatory (a negative correlation has been reported between the n-3/n-6 ratio and carotid stiffness β, which is an index of early atherosclerosis, in children with obesity).779
• In recent years, in Japan the dietary fat intake has increased with westernization of food habits. Therefore, in the Dietary Intake Standard 2020, target quantities of SFAs were added for children aged 3–17 years: ≤10% for boys and girls aged 3–14 years and ≤8% for children aged 15–17 years.
Japanese food is rich in variety, low in fat, and high in fiber. If the high salt content is reduced, it may be considered a healthy diet. As a preventive measure for CAD from childhood, the intake of a Japanese diet with fish as the main protein and a healthy portion of vegetables, seaweed, and soybean products is recommended.780
5.7.2 Exercise
For children, moderate exercise is effective for: healthy mental and physical development; controlling obesity, abnormal glucose metabolism, and abnormal lipid metabolism; and improving vascular endothelial function. Additionally, exercise exerts a positive effect on mental wellbeing, such as positivity and competence. With respect to the effect of exercise therapy, in an intervention study targeting children with obesity in Japan, the group that completed ≥10,000 steps while on holidays showed greater improvement in obesity compared with the group in which screen time was restricted on holidays, and to the group that performed only behavior recording781 (Class IIa, Level B).
With respect to the type of exercise, exercise play should be the focus in early childhood, and aerobic exercises in school-going children. After puberty, resistance exercises should also be performed.782 The physical activity guidelines for children in Japan do not set specific exercise intensities, but recommend daily exercise for ≥60 min.783 A sedentary lifestyle is the universal cause of obesity. Therefore, limiting the time spent watching TV and using computer and game displays in a seated position (“screen time”) to ≤2 h/day is recommended.784
5.7.3 Sleep
Sufficient amount of sleep is necessary because sleep deprivation is an important factor in obesity. Sekine et al examined the causes of obesity in Japanese 1st-graders and showed that children in the group with <8 h of sleep were 2.87-fold more likely to develop obesity than those in the group with ≥10 h sleep785 (Level B). A reduction in blood leptin levels and increase in ghrelin levels have been reported as potential mechanisms by which sleep deprivation leads to obesity (ghrelin is known to promote hunger). Staying up late may lead to the skipping of breakfast the following morning, which increases the risk of developing obesity and diabetes and leads to the onset of CAD in the future. According to the American Society of Sleep Research, based on the age group, school children require 9–13 h of sleep and adolescents require 8–10 h of sleep.786