Abstract
Background: Epidemiological data on ruptured aortic aneurysms from large-scale studies are scarce. The aims of this study were to: clarify the clinical course of ruptured aortic aneurysms; identify aneurysm site-specific therapies and outcomes; and determine the clinical course of patients receiving conservative therapy.
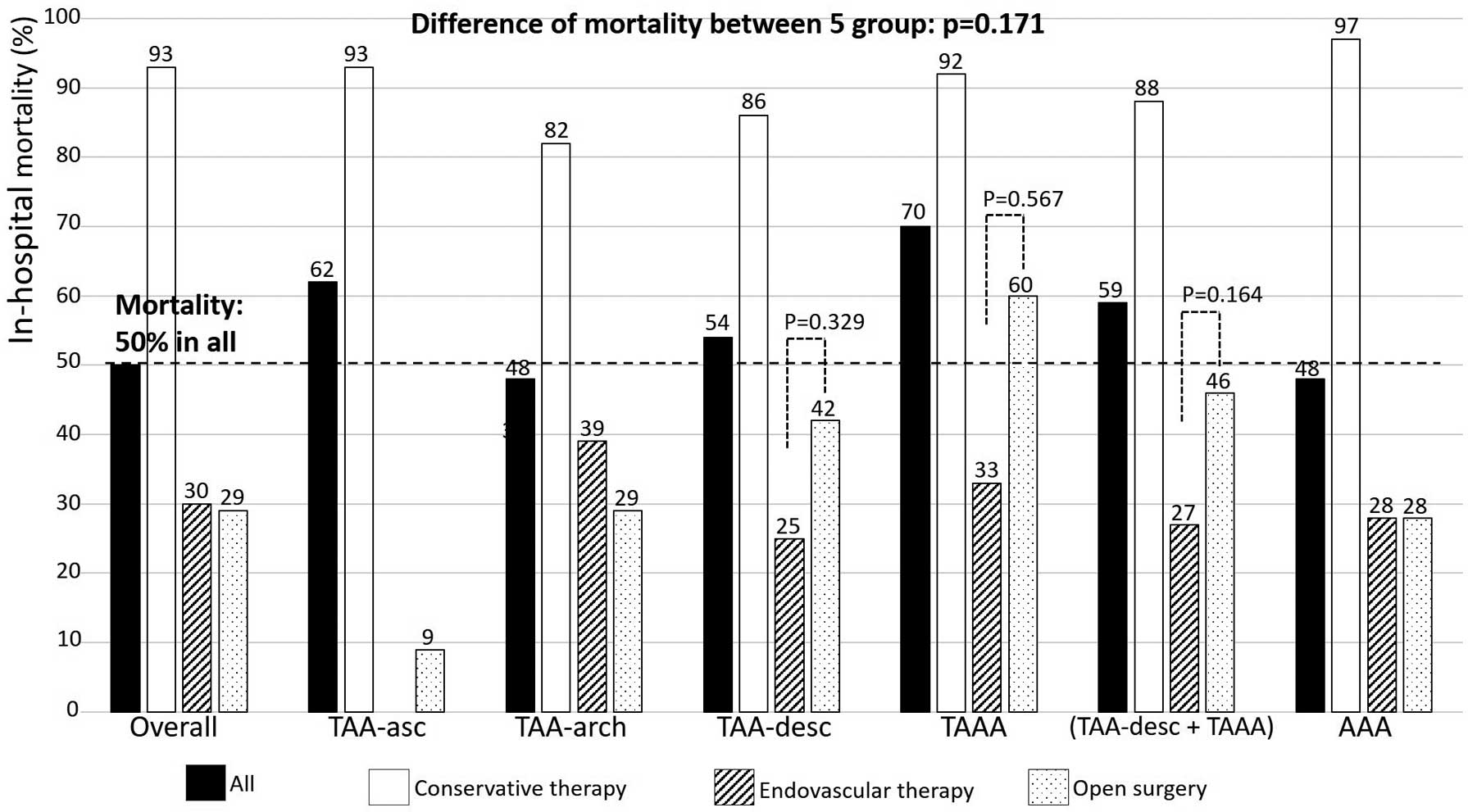
Methods and Results: Using the Tokyo Acute Aortic Super Network database, we retrospectively analyzed 544 patients (mean [±SD] age 78±10 years; 70% male) with ruptured non-dissecting aortic aneurysms (AAs) after excluding those with impending rupture. Patient characteristics, status on admission, therapeutic strategy, and outcomes were evaluated. Shock or pulselessness on admission were observed in 45% of all patients. Conservative therapy, endovascular therapy (EVT), and open surgery (OS) accounted for 32%, 23%, and 42% of cases, respectively, with corresponding mortality rates of 93%, 30%, and 29%. The overall in-hospital mortality rate was 50%. The prevalence of pulselessness was highest (48%) in the ruptured ascending AA group, and in-hospital mortality was the highest (70%) in the ruptured thoracoabdominal AA group. Multivariable logistic regression analysis indicated in-hospital mortality was positively associated with pulselessness (odds ratio [OR] 10.12; 95% confidence interval [CI] 4.09–25.07), and negatively associated with invasive therapy (EVT and OS; OR 0.11; 95% CI 0.06–0.20).
Conclusions: The outcomes of ruptured AAs remain poor; emergency invasive therapy is essential to save lives, although it remains challenging to reduce the risk of death.
Ruptured aortic aneurysms are a critical issue in emergency medicine, with reported mortality rates of 43–45%.1 However, epidemiological data from an overview of ruptured aortic aneurysms from large-scale studies are scarce. Furthermore, the treatment and outcomes of ruptured aortic aneurysms vary markedly depending on their location. This trend has become especially evident with advances in stent grafting. However, data on aneurysm site-specific clinical features of ruptured aortic aneurysms are lacking. In addition, most of the documented outcomes associated with ruptured aortic aneurysms are associated with invasive therapies, with limited reports on the outcomes of patients who did not undergo such interventions.
The purpose of this study was to clarify the clinical features, therapies, and outcomes of ruptured aortic aneurysms in patients after emergency transfer based on the Tokyo Acute Aortic Super Network (TAASN) registry database. Furthermore, we wanted to identify aneurysm site-specific therapies and outcomes and determine the clinical course of patients receiving conservative therapy.
Methods
TAASN
The Tokyo Cardiovascular Care Unit Network (TCCUN), which covers the entire Tokyo metropolitan region except for the islands, is an emergency transfer system for patients with all types of cardiovascular disease.2 The TAASN is a component of the TCCUN. The TAASN database comprises data from emergency departments, including cardiovascular intensive care units, cardiovascular surgery sections, and emergency and critical care centers in 65 hospitals, including 26 hospitals with advanced critical centers. To improve transport efficiency, 14 first-line priority hospitals (which can accept patients at any time) and 28 second-line hospitals (which will accept patients if the first-line hospitals cannot) have been established across the entire Tokyo metropolitan area. After obtaining consent from each patient to use their data, the TAASN member facility sends the data and anonymously registers the patient details in the TAASN database, as described previously.3 The data comprise all treatments and outcomes of ruptured aortic aneurysms after emergency admission in a limited metropolitan area.
Study Population
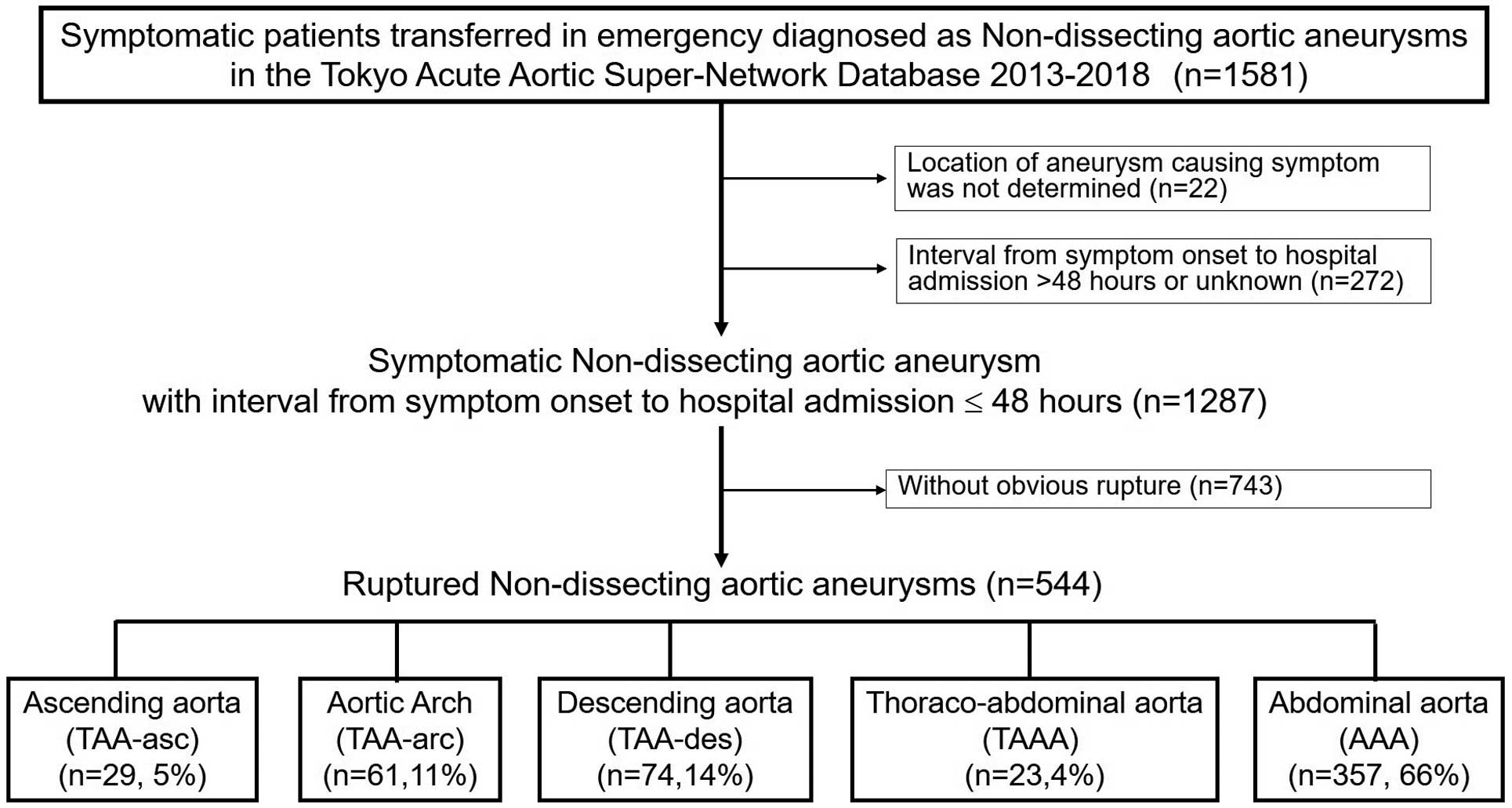
Figure 1 is a flow diagram of patient selection. We retrospectively analyzed 1,581 symptomatic patients with non-dissecting aortic aneurysms after emergency admission using the clinical records in the TAASN database for events between January 2013 and December 2018. We attempted to select suspected non-dissecting aortic aneurysms and excluded pseudoaneurysms and dissecting or infected aortic aneurysms as accurately as possible. Aortic aneurysms were diagnosed by physicians whose facilities participated in the TAASN. Of 1,581 registered patients with suspected non-dissecting aortic aneurysms during that period, we excluded 22 with an unknown lesion location and 272 who were admitted >48 h from symptom onset to focus on patients with evident symptoms without late admission. Of the remaining 1,287 patients with suspected symptoms of non-dissecting aortic aneurysms, 743 without obvious aortic ruptures were excluded. The excluded patients without obvious aortic rupture may be diagnosed with impending aortic rupture or chest or back pain not caused by an aortic aneurysm. Thus, 544 patients with obvious aortic rupture (i.e., so-called open rupture) were included in the present study. In this study, obvious aortic rupture was defined as obvious blood leakage from the aorta confirmed by imaging findings, including computed tomography (CT) or echocardiography.
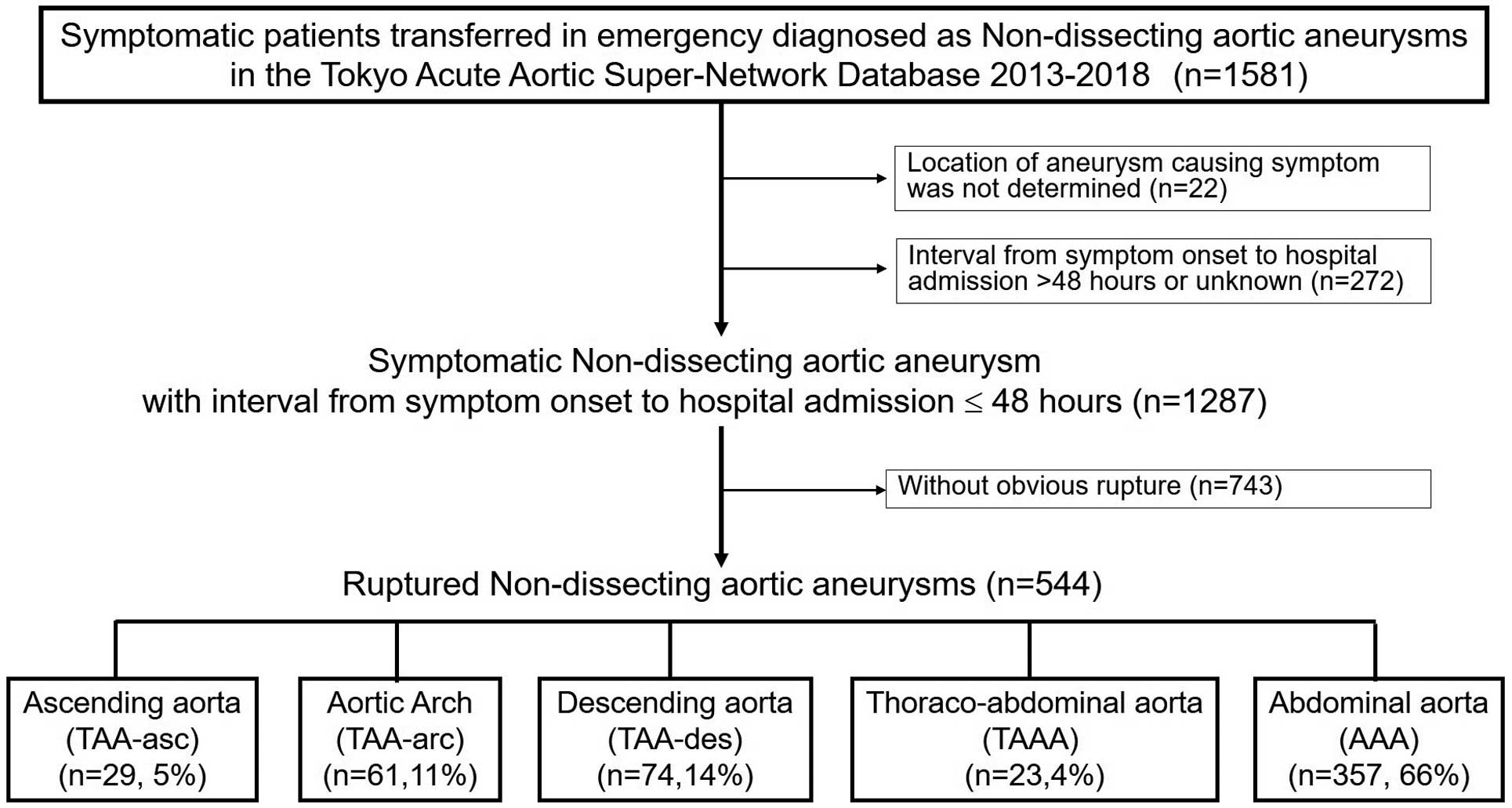
The 544 patients with ruptured aortic aneurysms were divided into 5 groups according to the segment where the aneurysm occurred: thoracic aortic aneurysm at the ascending aorta (TAA-asc; n=29 [5%]), aortic arch (TAA-arch; n=61 [11%]), or descending aorta (TAA-desc; n=74 [14%]); thoracoabdominal aorta aneurysm (TAAA; n=23 [4%]); and abdominal aorta aneurysm (AAA; n=357 [66%]). Patients with an aortic root aneurysm were included in the TAA-asc group. Patients with ≥2 aneurysms were classified into one of these 5 groups based on the CT findings and pain location.
Patient Characteristics
We collected patients’ background information on admission, including age, sex, body mass index, history of hypertension, dyslipidemia, and diabetes, and smoking history, and compared this among the 5 aneurysm groups.
Status on Admission
The status on admission, such as the time from symptom onset to admission, systolic blood pressure (SBP; in the case of measurable SBP), and hemoglobin (Hb) levels, were examined. SBP other than numeric data such as “pulseless”, including cardiac arrest, was collected and examined separately from numeric data. The status on admission was compared among the 5 aneurysm groups.
Subsequently, these data were compared between patients undergoing conservative (n=174; 32%) and invasive (n=356; 65%) therapy. Invasive therapy included endovascular therapy (EVT; n=125 [23%]) and open surgery (OS; n=231 [42%]).
Therapeutic Strategy and Outcome
The proportion of a selected therapy for each aneurysm site was compared among the 5 groups, and in-hospital mortality for each therapy was compared separately for each of the 5 aortic aneurysm sites. The number of in-hospital deaths among patients receiving conservative therapy and the days from admission to death were examined. We searched for the cause of death. Finally, we used multivariable logistic regression analysis to identify factors associated with in-hospital death.
Statistical Analysis
Continuous data are expressed as the mean±SD. Because data on SBP at admission and time from symptom onset to hospital admission were not normally distributed, they were tested using a non-parametric test and are expressed as the median with interquartile range (IQR). The significance of differences among continuous variables for the 5 groups of aortic aneurysm sites were calculated using Kruskal-Wallis tests with Dunnett correction. Categorical variables are expressed as numbers and percentages and were compared among the 5 groups of aortic aneurysm sites using Fisher’s exact tests with Dunnett correction. Factors associated with in-hospital death were identified using multivariable logistic regression analysis. The presence or absence of multicollinearity of explanatory variables in multivariate analysis was confirmed by a variance inflation factor (VIF) <3. P<0.05 was considered statistically significant. IBM SPSS for Windows version 27.0 (IBM Corp., Armonk, NY, USA) was used for all statistical analyses.
Results
Patient Characteristics
Patient characteristics according to the site of the aortic aneurysm are presented in Table 1. Of the 5 groups, AAA (66%) was the most prevalent. No differences in patient characteristics were observed among the 5 aortic aneurysm site groups. Furthermore, patient background did not differ between the broadly defined “TAA” group (comprising TAA-asc, TAA-arch, TAA-desc, and TAAA) and the AAA group.
Table 1.
Patient Characteristics
| |
All |
TAA-asc |
TAA-arch |
TAA-desc |
TAAA |
TAA/TAAA |
AAA |
P value |
TAA/TAAA
vs. AAA |
Among 5
groups |
| No. patients (%) |
544 |
29 (5) |
61 (11) |
74 (14) |
23 (4) |
187 (34) |
357 (66) |
|
|
| Age (years) |
78±10 |
76±10 |
78±10 |
78±9 |
79±7 |
78±9 |
77±11 |
0.433 |
0.774 |
| Male sex |
383 (70) |
21 (72) |
43 (70) |
46 (62) |
15 (65) |
125 (67) |
258 (72) |
0.199 |
0.488 |
| BMI (kg/m2) |
22.5±3.8
(n=395) |
22.4±2.5
(n=17) |
22.1±4.0
(n=50) |
22.6±4.3
(n=51) |
23.4±4.5
(n=18) |
22.4±4.0
(n=136) |
22.5±3.7
(n=259) |
0.664 |
0.661 |
| Hypertension |
341/532
(64) |
13/27
(48) |
43/61
(70) |
52/73
(71) |
15/23
(65) |
122/187
(66) |
219/348
(63) |
0.638 |
0.214 |
| Dyslipidemia |
191/534
(36) |
5/27
(19) |
15/61
(25) |
29/73
(40) |
10/23
(43) |
59/184
(32) |
132/350
(38) |
0.217 |
0.067 |
| Diabetes |
62/534
(12) |
3/27
(11) |
10/60
(17) |
5/73
(7) |
4/23
(17) |
22/183
(12) |
40/351
(11) |
0.887 |
0.379 |
| Smoking history |
173/426
(41) |
8/20
(40) |
21/54
(39) |
24/62
(39) |
6/20
(30) |
59/156
(38) |
114/270
(42) |
0.413 |
0.861 |
Unless indicated otherwise, data are given as the mean±SD, n (%), or n/N (%). AAA, abdominal aorta aneurysm; BMI, body mass index; TAA-arch, thoracic aortic aneurysm at the aortic arch; TAA-asc, thoracic aortic aneurysm at the ascending aorta; TAA-desc, thoracic aortic aneurysm at the descending aorta; TAAA, thoracoabdominal aorta aneurysm.
Status on Admission
The status of patients on admission according to aortic aneurysm site is presented in Table 2. The overall percentage of hemodynamically unstable patients, including those with shock vital signs (measurable blood pressure <90 mmHg) or pulselessness, was 45%. TAA-asc was the most critical segment on admission compared with the other sites. In this cohort, although measurable SBP did not differ significantly, pulselessness (48%) and cardiac tamponade (31%) were the most prevalent, and the Hb value was the highest (11.9±2.2 g/L) on admission among the 5 groups.
Table 2.
Patient Status on Admission
| |
All |
TAA-asc |
TAA-arch |
TAA-desc |
TAAA |
TAA/TAAA |
AAA |
P value |
TAA/TAAA
vs. AAA |
Among 5
groups |
| No. patients (%) |
544 |
29 (5) |
61 (11) |
74 (14) |
23 (4) |
187 (34) |
357 (66) |
|
|
Time from symptom onset
to hospital admission (min) |
184
[75–380] |
111
[44–215] |
185
[66–380] |
198
[61–386] |
170
[110–310] |
169
[65–377] |
189
[80–380] |
0.660 |
0.540 |
| SBP measurable (mmHg) |
109±35
(n=428) |
119±40
(n=14) |
117±33
(n=54) |
111±33
(n=69) |
111±42
(n=20) |
114±35
(n=181) |
106±35
(n=278) |
0.025 |
0.190 |
| Shock or pulselessness |
241/532
(45) |
18/29
(62) |
15/60
(25)A |
23/69
(33) |
11/23
(48) |
67/181
(37) |
174/351
(50) |
0.006 |
<0.001 |
| Pulselessness |
104/533
(20) |
14/29
(48) |
6/61
(10)B |
9/69
(13)C |
3/23
(19)D |
32/182
(18) |
72/351
(21)E |
0.489 |
<0.001 |
| Cardiac arrest |
72 (14) |
11 (38) |
6 (10)F |
9 (12)G |
2 (9) |
28 (15) |
44 (12)H |
0.423 |
0.010 |
| Hemoglobin (g/dL) |
10.0±2.7
(n=510) |
11.9±2.2
(n=28) |
10.7±2.6
(n=58) |
10.3±2.7I
(n=65) |
9.2±2.2J
(n=23) |
10.5±2.6
(n=174) |
9.8±2.7K
(n=336) |
0.002 |
<0.001 |
| Hemoglobin <7.0 g/dL |
65/510
(13) |
1/28
(4) |
5/58
(9) |
6/65
(9) |
5/23
(22) |
17/174
(10) |
48/336
(14) |
0.163 |
0.211 |
| Cardiac tamponade |
17 (3) |
9 (31) |
4 (7)L |
4 (5)M |
0 (0)N |
17 (9) |
– |
– |
<0.001 |
Unless indicated otherwise, data are given as the mean±SD, median [interquartile range], n (%), or n/N (%). Post hoc comparisons with Dunnett correction vs. the thoracic aortic aneurysm at the ascending aorta (TAA-asc) group: AP=0.004; BP<0.001; CP=0.002; DP=0.034; EP=0.007; FP=0.012; GP=0.021; HP=0.003; IP=0.017; JP<0.001; KP<0.001; LP=0.015; MP=0.005; NP=0.013. SBP, systolic blood pressure. Other abbreviations as in Table 1.
Table 3 shows the status on admission of each therapeutic strategy subgroup. Comparing patient characteristics and status on admission between patients receiving conservative therapy and those receiving invasive therapy (EVT or OS), the former presented at older age (82±9 vs. 75±10 years; P<0.001) and had lower Hb concentrations (9.5±2.5 vs. 10.3±2.7 g/dL; P=0.002), a higher prevalence of pulselessness (40% vs. 9%; P<0.001), and higher in-hospital mortality (93% vs. 29%; P<0.001).
Table 3.
Characteristics and Status on Admission of Each Therapeutic Strategy Subgroup
| |
EVT |
OS |
EVT or OS |
Conservative
therapy |
P value
EVT or OS vs.
conservative therapy |
| No. patients |
125 (23) |
231 (42) |
356 (65) |
174 (32) |
|
| Age (years) |
76±11 |
75±9 |
75±10 |
82±9 |
<0.001 |
| Male sex |
82 (66) |
178 (77) |
260 (73) |
114 (66) |
0.085 |
| Measurable SBP (mmHg) |
119±35
(n=114) |
104±34
(n=203) |
110±35
(n=317) |
106±37
(n=102) |
0.341 |
| Shock or pulseless |
32 (26)
(n=113) |
93 (41)
(n=225) |
125 (36)
(n=338) |
107 (63)
(n=170) |
<0.001 |
| Hb (g/dL) |
10.4±2.8
(n=117) |
10.2±2.7
(n=218) |
10.3±2.7
(n=335) |
9.5±2.5
(n=162) |
0.002 |
| Hb <7.0 g/dL |
12 (10) |
27 (12) |
39 (12) |
25 (15) |
0.254 |
| Pulselessness |
9 (9)
(n=123) |
22 (10)
(n=225) |
31 (9)
(n=348) |
68 (40)
(n=171) |
<0.001 |
| Cardiac arrest |
2 (2) |
10 (4) |
12 (3) |
55 (32) |
<0.001 |
| In-hospital death |
37 (30) |
67 (29) |
104 (29) |
162 (93) |
<0.001 |
Unless indicated otherwise, data are given as the mean±SD or n (%). EVT, endovascular therapy; Hb, hemoglobin; OS, open surgery; SBP, systolic blood pressure; shock, SBP <90 mmHg.
Therapeutic Strategies and Outcomes by Aneurysm Site
The therapeutic strategies according to aortic aneurysm site are shown in Figure 2. Among all patients with ruptured aortic aneurysms, 32% were treated with conservative therapy, whereas 23% and 42% were treated with EVT and OS, respectively. Among patients with TAA-desc and TAAA, EVT (33% and 26%, respectively) was more frequently selected than OS (26% and 22%, respectively). EVT was selected the least frequently in patients with AAA (21%), even less frequently than in patients with TAA-desc (33%; P=0.030). OS was most frequently selected for patients with AAA (50%), significantly more frequently than for patients with TAAA (22%; P=0.009).

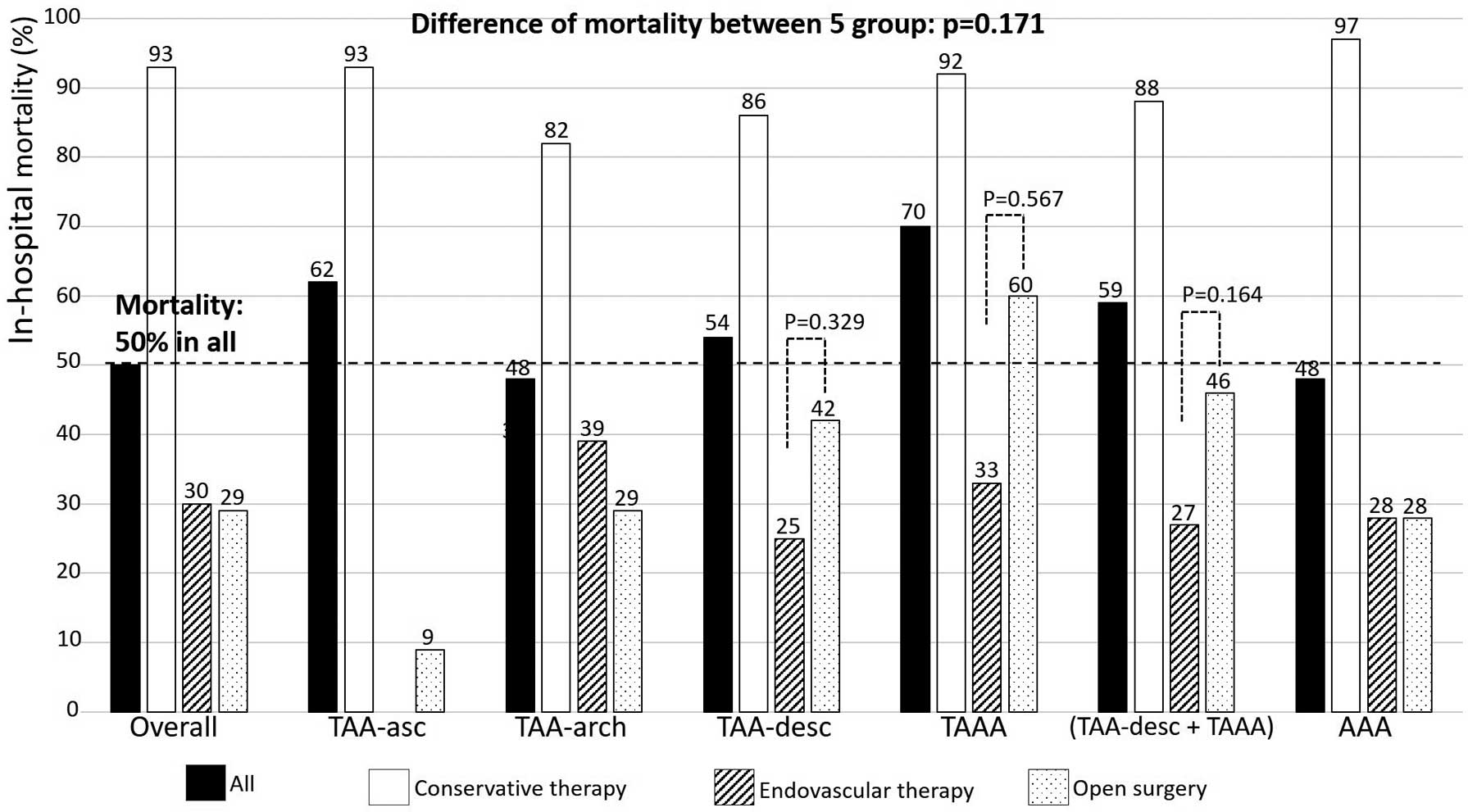
The in-hospital mortality rates according to aneurysm site are shown in Figure 3. The overall in-hospital mortality was 50%, without any differences among the 5 groups (P=0.171). The in-hospital mortality rates of patients with cardiac arrest and pulselessness were 97% and 90%, respectively. According to therapeutic strategy, the mortality rates of conservative therapy, EVT, and OS were 93%, 30%, and 29%, respectively. Among the 5 sites, the mortality rate was highest in for TAAA (70%) and lowest for AAA (48%) and TAA-arch (48%). In the case of TAA-desc, TAAA, and “TAA-desc or TAAA”, the mortality rate was lower for patients treated with EVT (25%, 33%, and 27%, respectively) than those treated with OS (42% [P=0.329], 60% [P=0.567], and 46% [P=0.164], respectively), although the differences were not statistically significant. In the case of patients with AAA, the mortality for those treated with EVT and OS was similar (28% and 28%, respectively; P=1.000). Comparing the TAA/TAAA subgroup with the AAA group, the mortality attributed to OS was 32% and 28% (P=0.693), respectively, and that of EVT was 32% and 28% (P=0.612), respectively.
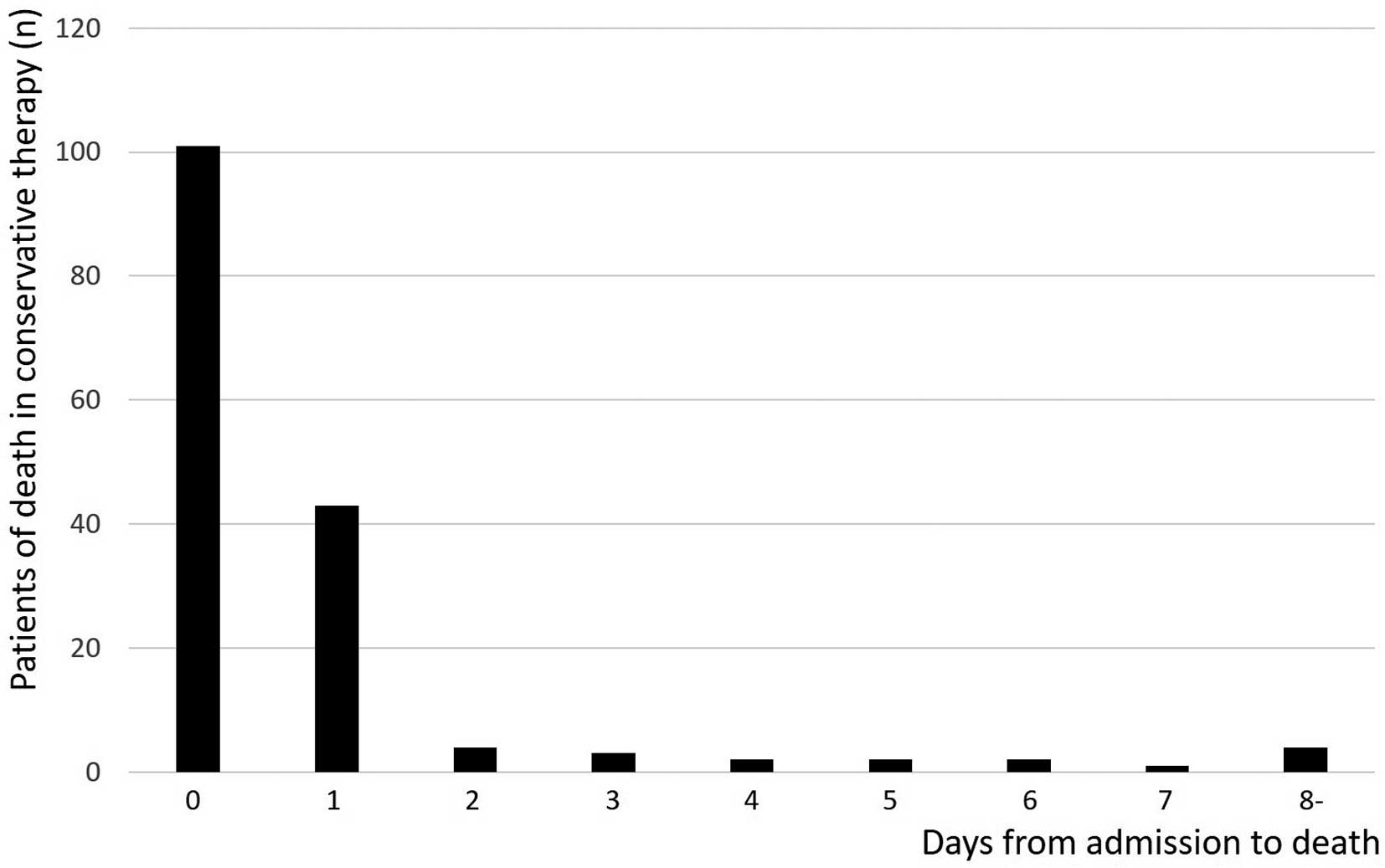
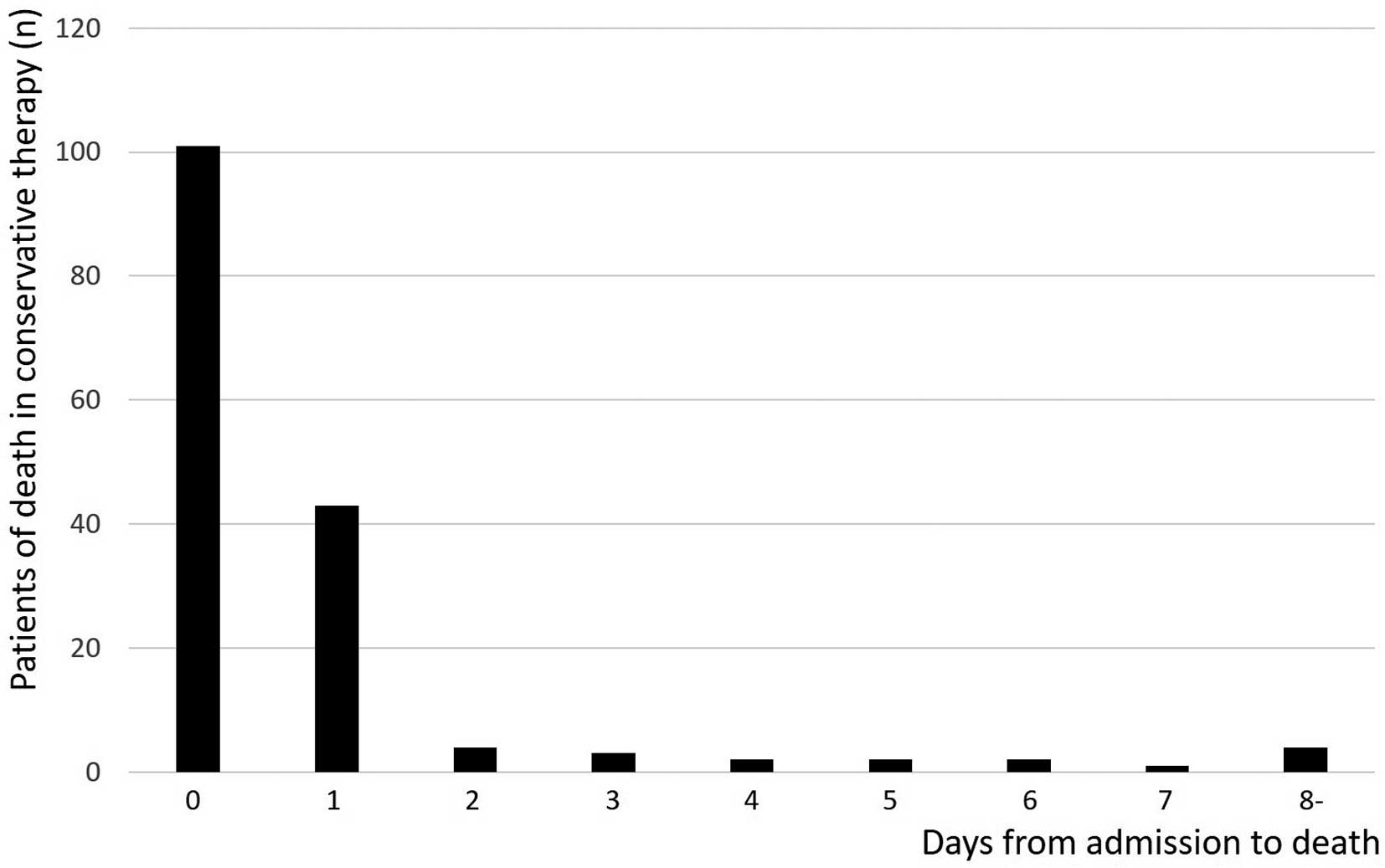
The mortality rates of patients receiving conservative therapy and the number of days from admission to death are shown in Figure 4. Within the first 2 days after admission, 89% of patients on conservative therapy died, which increased to 98% within 1 week. The primary cause of death at each rupture site was hemorrhage: TAA-asc, 67%; TAA-arch, 86%; TAA-desc, 90%; TAAA, 94%; and AAA, 89% (P=0.106). Other causes of death were cardiac tamponade (22% of patients with TAA-asc), infection (10% of patients with TAA-arch), and mesenteric ischemia (4% of patients with AAA).
The results of the multivariable regression analysis of factors associated with in-hospital death are presented in Table 4. Multicollinearity was determined to be absent because the VIF for all explanatory variables was <3 (1.224 for age ≥85 years, 1.056 for male sex, 1.173 for onset to admission ≥120 min, 1.033 for Hb <7.0 g/dL, 1.225 for pulselessness on admission, 1.043 for TAA-asc, 1.029 for TAA-desc, 1.019 for TAAA, and 1.468 for EVT or OS). The analysis indicated that in-hospital mortality was positively associated with age ≥85 years (odds ratio [OR] 3.29; 95% confidence interval [CI] 1.92–5.64), male sex (OR 2.17; 95% CI 1.31–3.60), and pulselessness (OR 10.12; 95% CI 4.09–25.07), TAAA (OR 4.29; 95% CI 1.25–14.81), and negatively associated with invasive therapy (EVT and OS; OR 0.11; 95% CI 0.06–0.20).
Table 4.
Factors Associated With In-Hospital Death
| |
OR |
95% CI |
P value |
| Age ≥85 years |
3.289 |
1.918–5.640 |
<0.001 |
| Male sex |
2.172 |
1.310–3.602 |
0.003 |
| Onset to admission ≥120 min |
1.118 |
0.648–1.927 |
0.689 |
| Hemoglobin <7.0 g/dL |
1.925 |
0.894–4.146 |
0.094 |
| Pulselessness on admission |
10.120 |
4.085–25.072 |
<0.001 |
| TAA-asc |
0.663 |
0.184–2.397 |
0.531 |
| TAA-desc |
1.509 |
0.695–3.275 |
0.298 |
| TAAA |
4.293 |
1.245–14.806 |
0.021 |
| EVT or OS |
0.113 |
0.064–0.201 |
<0.001 |
CI, confidence interval; OR, odds ratio. Other abbreviations as in Tables 1,3.
Discussion
We have documented the detailed clinical course of 544 patients with ruptured aortic aneurysms after emergency admission in a metropolitan area. The in-hospital mortality rate of ruptured aortic aneurysms was 50% in the overall cohort and 93% among patients receiving conservative therapy. Among all aortic aneurysm sites, TAA-asc presented the most unstable hemodynamic condition. Advanced age and pulselessness on admission were positively associated with in-hospital mortality; invasive therapy (EVT and OS) was negatively associated with mortality.
Our data demonstrate an in-hospital mortality rate of ruptured aortic aneurysms of 50% overall, which is still high in the stent graft era. Recent studies reported overall mortality rates of ruptured TAA and AAA of 43–44%1,4 and 40–45%,1,5 respectively. The mortality rate in the present study seems to be a little higher than in previous reports. One possible reason for this is that our data on aortic rupture only included open rupture, not impending rupture. Second, other studies occasionally calculated mortality rates without including conservative therapy, resulting in a lower mortality rate. Third, the infrequent use stent grafts may be related to the higher mortality in the present study.
Data from the US in 2015 indicated an increasing use of EVT (55%) for ruptured AAA and predominance over OS (45%), and lower mortality when treated with EVT (21%) than with OS (36%).6 The characteristic feature of treatment for ruptured AAA in the Tokyo area in the present study was the more common use of OS than EVT. One possible reason for this is that our data do not include those with impending rupture, so hemodynamics may have been more unstable in many cases, resulting in more patients treated with OS than with stent graft. Another reason is that hospitals belonging to the TAASN do not always stock all types and sizes of stent grafts. Similarly, in the case of ruptured TAA, treatment with EVT is more common than with OS, and the mortality rate with EVT is lower than that with OS.7–9 In the present study, EVT was used more than in OS for patients with ruptured TAA-desc and TAAA, but the difference was smaller than expected, and in-hospital mortality rates for patients treated by EVT were not significantly superiority to those for patients treated by OS.
Our study demonstrated that patients with TAA-asc were most likely to present in a hemodynamically unstable condition, probably due to cardiac tamponade, because their mean Hb level did not decrease. However, patients with TAA-asc had the second worst mortality rate (62%) after those with TAAA (70%). A previous study had reported that among patients with ruptured TAA, prehospital death was highest for TAA-asc.10
We could not find any significant differences in patient characteristic between the 5 groups of aortic aneurysms, and between the broadly defined TAA group (TAA and TAAA) and AAA group. A recent study reported that AAA was more strongly associated with atherosclerosis than TAA.11 Higher age, male sex, smoking, and hypertension are all known risk factors for AAA.12,13 However, in the present study, the AAA group did not have more factors contributing to atherosclerosis than the TAA group. This may be due to an insufficient sample size.
We presented patient characteristics and the clinical course of the patients with ruptured aortic aneurysms according to type of therapy: invasive and conservative therapy. It is important to note that 32% of patients with ruptured aortic aneurysms were treated without invasive therapy. Not surprisingly, patients treated conservatively were in poorer general condition on admission than patients treated invasively. Approximately 90% of all patients with ruptured aortic aneurysms under conservative therapy died within 2 days of admission, and almost all patients died within 1 week. These findings are consistent with previous studies reporting that 76% of patients with ruptured TAA without surgery died within 24 h of symptom onset.14
The multivariable regression analysis showed that older age and pulselessness on admission were strongly associated with in-hospital death, and that invasive therapy was negatively associated with mortality, as expected. These findings suggested optimization of patient selection for invasive therapy, especially among elderly patients. Thus, aggressive invasive therapy with appropriate patient selection is required to save lives.
Our study has several limitations. First, this study is based on registry data from the TASSN database. As such, some relevant variables were lacking: the diameter of the aortic aneurysm on admission, aneurysm morphology (fusiform or saccular; one aneurysm or some aneurysms/mega-aorta), the number of patients with multiple rupture points, where and by whom the CT images of each patient with ruptured aneurysm were analyzed, the exact time of death, the exact time of initiating EVT or OS, and the frequency of connective tissue disorders such as Marfan syndrome. Furthermore, we could not directly confirm the CT images of each patient with a ruptured aortic aneurysm. Second, instead of contrast-enhanced CT, echocardiography was used for diagnosis in certain cases. Consequently, aortic aneurysms, especially those involving dissection, may not have been conclusively excluded in these cases. Third, the lack of significant differences in mortality and background among the 5 subgroups may be due to the limited sample size of each subgroup. Fourth, detailed surgical procedures were not recorded for each open surgery. However, the details of the surgical repair were not the main purpose of this study. Fifth, determining therapeutic strategies was not uniform for all patients but was based on the policies and therapeutic skills available at each hospital. However, our results demonstrated the current treatment trends and outcomes of open ruptured aortic aneurysms in a limited metropolitan area. Sixth, the proportion of patients with AAA in critical condition may have been overestimated. Patients with mild symptoms may have been transferred to general surgery wards and they may not have been registered in the TAASN database. Thus, patients in a more severe condition may have been more likely to be included in our study. In contrast, those with TAA and TAAA may have been underestimated because these patients are occasionally transferred with cardiopulmonary arrest and die before a definitive diagnosis. Regardless of the location of the rupture, certain patients with ruptured aortic aneurysms died at the time of ambulance arrival and were not necessarily transferred to hospitals. Therefore, the results of this study only pertain to patients who arrived at hospital in critical condition and are not representative of the overall patient profile for ruptured aortic aneurysms.
Conclusions
Our data demonstrate that the outcome of ruptured aortic aneurysms remains poor, even with advances in surgical techniques and the widespread use of stent grafts, and conservative therapy can barely rescue patients with ruptured aortic aneurysms. Invasive therapy for ruptured aortic aneurysms is essential to save lives, although it remains challenging in many aspects to reduce the risk of death.
Acknowledgments
The authors thank the participating hospitals and leading members of TCCUN and TAASN. The authors also thank Kozue Murayama and Nobuko Yoshida for their assistance in maintaining the TAASN database.
Sources of Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Data collection and maintenance of the TCCUN registry is financially supported by the Tokyo Metropolitan Government, which had no role in the execution of this study or the interpretation of the results.
Disclosures
H.Y. is a member of Circulation Journal’s Editorial Team. The remaining authors have no conflicts of interest to disclose.
IRB Information
The Institutional Review Board of the Nippon Medical School approved this study (B-2022-528).
Data Availability
The deidentified participant data will not be shared.
References
- 1.
Groves EM, Khoshchehreh M, Le C, Malik S. Effects of weekend admission on the outcomes and management of ruptured aortic aneurysms. J Vasc Surg 2014; 60: 318–324.
- 2.
Yamamoto T, Otsuka T, Yoshida N, Kobayashi Y, Komiyama N, Hara K, et al. Hospital performance in a large urban acute myocardial infarction emergency care system: Tokyo Cardiovascular Care Unit network. J Cardiol 2021; 78: 177–182.
- 3.
Akutsu K, Yoshino H, Shimokawa T, Ogino H, Kunihara T, Takahashi T, et al. Is systolic blood pressure high in patients with acute aortic dissection on first medical contact before hospital transfer? Heart and Vessels 2019; 34: 1748–1757.
- 4.
Trenner M, Kuehnl A, Salvermoser M, Reutersberg B, Geisbuesch S, Schmid V, et al. Editor’s choice - High annual hospital volume is associated with decreased in hospital mortality and complication rates following treatment of abdominal aortic aneurysms: Secondary data analysis of the nationwide German DRG statistics from 2005 to 2013. Eur J Vasc Endovasc Surg 2018; 55: 185–194.
- 5.
Ultee KHJ, Zettervall SL, Soden PA, Buck DB, Deery SE, Shean KE, et al. The impact of endovascular repair on management and outcome of ruptured thoracic aortic aneurysms. J Vasc Surg 2017; 66: 343–352.
- 6.
Dansey KD, Varkevisser RRB, Swerdlow NJ, Li C, de Guerre LEVM, Liang P, et al. Epidemiology of endovascular and open repair for abdominal aortic aneurysms in the United States from 2004 to 2015 and implications for screening. J Vasc Surg 2021; 74: 414–424.
- 7.
Jonker FH, Trimarchi S, Verhagen HJ, Moll FL, Sumpio BE, Muhs BE. Meta-analysis of open versus endovascular repair for ruptured descending thoracic aortic aneurysm. J Vasc Surg 2010; 51: 1026–1032, 1032.e1–1032.e2.
- 8.
Ultee KHJ, Zettervall SL, Soden PA, Buck DB, Deery SE, Shean KE, et al. The impact of endovascular repair on management and outcome of ruptured thoracic aortic aneurysms. J Vasc Surg 2017; 66: 343–352.e1.
- 9.
Salsano A, Salsano G, Spinella G, Zaottini F, Mavilio N, Perocchio G, et al. Endovascular versus open surgical repair for ruptured descending aortic pathologies: A systematic review and meta-analysis of observational studies. Cardiovasc Intervent Radiol 2021; 44: 1709–1719.
- 10.
Pál D, Szilágyi B, Berczeli M, Szalay CI, Sárdy B, Oláh Z, et al. Ruptured aortic aneurysm and dissection related death: An autopsy database analysis. Pathol Oncol Res 2020; 26: 2391–2399.
- 11.
Ito S, Akutsu K, Tamori Y, Sakamoto S, Yoshimuta T, Hashimoto H, et al. Differences in atherosclerotic profiles between patients with thoracic and abdominal aortic aneurysms. Am J Cardiol 2008; 101: 696–969.
- 12.
Baumgartner I, Hirsch AT, Abola MT, Cacoub PP, Poldermans D, Steg PG, et al. Cardiovascular risk profile and outcome of patients with abdominal aortic aneurysm in out-patients with atherothrombosis: Data from the Reduction of Atherothrombosis for Continued Health (REACH) Registry. J Vasc Surg 2008; 48: 808–814.
- 13.
Lee AJ, Fowkes FG, Carson MN, Leng GC, Allan PL. Smoking, atherosclerosis and risk of abdominal aortic aneurysm. Eur Heart J 1997; 18: 671–676.
- 14.
Johansson G, Markström U, Swedenborg J. Ruptured thoracic aortic aneurysms: A study of incidence and mortality rates. J Vasc Surg 1995; 21: 985–988.