Abstract
Background: Hypertension is a major cause of cardiovascular disease (CVD). In patients with hypertension, unawareness of the disease often results in poor blood pressure control and increases the risk of CVD. However, data in nationwide surveys regarding the proportion of unaware individuals and the implications of such on their clinical outcomes are lacking. We aimed to clarify the association between unawareness of being prescribed antihypertensive medications among individuals taking antihypertensive medications and the subsequent risk of developing CVD.
Methods and Results: This retrospective cohort study analyzed data from the JMDC Claims Database, including 313,715 individuals with hypertension treated with antihypertensive medications (median age 56 years). The primary endpoint was a composite of myocardial infarction, angina pectoris, stroke, heart failure, and atrial fibrillation. Overall, 19,607 (6.2%) individuals were unaware of being prescribed antihypertensive medications. During the follow-up period, 33,976 composite CVD endpoints were documented. Despite their youth, minimal comorbidities, and the achievement of better BP control with a reduced number of antihypertensive prescriptions, unawareness of being prescribed antihypertensive medications was associated with a greater risk of developing composite CVD. Hazard ratios of unawareness of being prescribed antihypertensive medications were 1.16 for myocardial infarction, 1.25 for angina pectoris, 1.15 for stroke, 1.36 for heart failure, and 1.28 for atrial fibrillation. The results were similar in several sensitivity analyses, including the analysis after excluding individuals with dementia.
Conclusions: Among individuals taking antihypertensive medications, assessing the awareness of being prescribed antihypertensive medications may help identify those at high risk for CVD-related events.
Hypertension is a major cause of cardiovascular disease (CVD) and one of the most frequently observed lifestyle-related diseases in the general population.1 In individuals with hypertension, characterized by systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure ≥90 mmHg, a lack of awareness of their condition often results in poor blood pressure control and increases the risk of developing CVD.2–6 Moreover, in clinical settings, patients with hypertension who are prescribed antihypertensive medications often remain unaware of their prescribed treatment regimen. However, data in nationwide surveys regarding the proportion of individuals who lack awareness of their antihypertensive prescriptions and the implications of such unawareness on their clinical outcomes are scarce. Using a nationwide health checkup and claims database, we aimed to determine the proportion of unawareness of antihypertensive prescriptions among individuals diagnosed with hypertension and prescribed such medications, and its association with cardiovascular outcomes.
Methods
Study Population
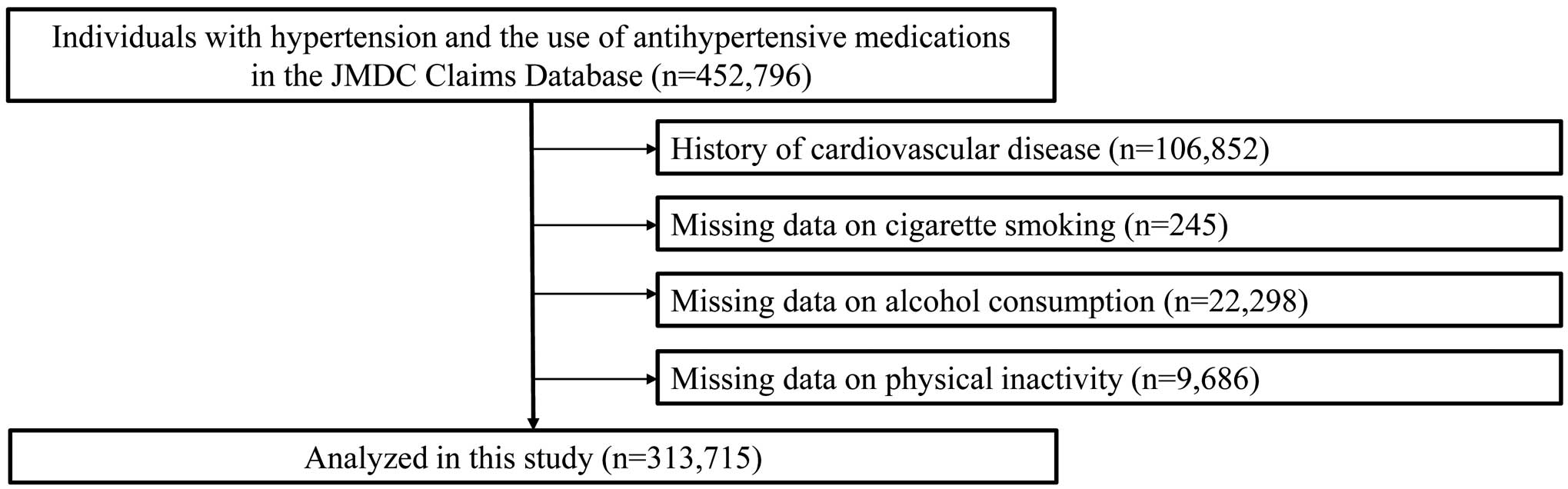
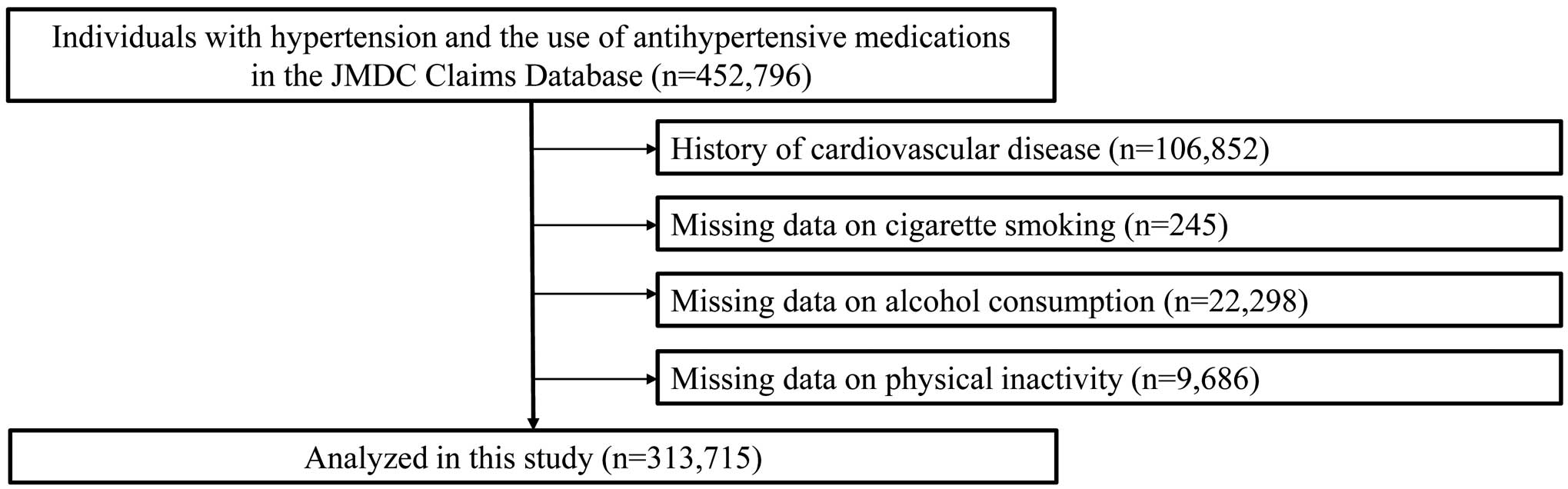
This was a nationwide population-based retrospective cohort study using data retrieved from the JMDC Claims Database (JMDC, Tokyo, Japan).7–9 The JMDC Claims Database collects data on individual health insurance records and health checkups from more than 60 Japanese insurers (e.g., anthropometric measurements and blood tests results). The database stores data on inpatient and outpatient administrative claims; diagnoses are registered using the International Classification of Diseases Tenth Revision (ICD-10). We identified 452,796 individuals aged ≥18 years with hypertension (ICD-10 codes I10–I15) using antihypertensive medications (World Health Organization Anatomical Therapeutic Chemical codes: C02, C03, C04, C07, C08, and C09) from January 2005 to May 2022. Individuals were included if they were enrolled in the insurance for more than 1 year. Exclusion criteria were as follows: a prior history of CVD (n=106,852), such as myocardial infarction (MI), angina pectoris (AP), stroke, heart failure (HF) or atrial fibrillation (AF); missing data on cigarette smoking (n=245); missing data on alcohol consumption (n=22,298); or missing data on physical inactivity (n=9,686). Thus, 313,715 individuals were included in the present study (Figure 1).
Ethical Considerations
This study was approved by the Ethics Committee of The University of Tokyo (Approval no. 2018-10862) and was conducted in accordance with the Declaration of Helsinki. Because the JMDC Claims Database was anonymized, the requirement for informed consent was waived.
Awareness of Being Prescribed Antihypertensive Medications
Awareness of being prescribed antihypertensive medications was assessed by responses to the question “Do you use medications to lower your blood pressure?” in health checkups. “Unawareness” was defined as individuals with hypertension who were prescribed antihypertensive medications and answered “No” to the question.
Covariates
Information on covariates was retrieved from the initial health checkups and medication status in the database. Information on the number of antihypertensive medication prescriptions was also obtained. The number of prescriptions for antihypertensive medications was defined as the number of prescriptions for the following drug classes: renin–angiotensin system inhibitors, β-blockers, calcium channel blockers, mineralocorticoid receptor antagonists, diuretics, and other antihypertensive medications. Obesity was defined as a body mass index ≥25 kg/m2. Diabetes was defined as a fasting glucose concentration ≥126 mg/dL and/or having a prescription for antidiabetic medications (including insulin). Dyslipidemia was defined as low-density lipoprotein cholesterol ≥140 mg/dL, and/or a high-density lipoprotein cholesterol <40 mg/dL, and/or a triglyceride ≥150 mg/dL, and/or having a prescription for antihyperlipidemic medications. Smoking status (current or non-current/never) and the frequency of alcohol consumption (every day or not every day) were assessed using information from a self-administered questionnaire. Physical inactivity was defined as not exercising for 30 min ≥2 times/week or not walking for more than 1 h/day.
Outcomes
Data on clinical outcomes were collected between January 2005 and May 2022. The primary outcomes were composite CVD events, including MI (ICD-10 codes I210–I214 and I219), AP (ICD-10 codes I200, I201, I208, and I209), stroke (ICD-10 codes I630, I631–I636, I638, I639, I600–I611, I613–I616, I619, I629, and G459), HF (ICD-10 codes I500, I501, I509, and I110), and AF (ICD-10 codes: I480, I481, I482, I483, I484, and I489).8,10 The incidence of MI, AP, stroke, HF, and AF was analyzed separately as secondary outcomes. Individuals were censored at outcome occurrence, insurance withdrawal (including death), or on the final day of the study (May 2022).
Statistical Analysis
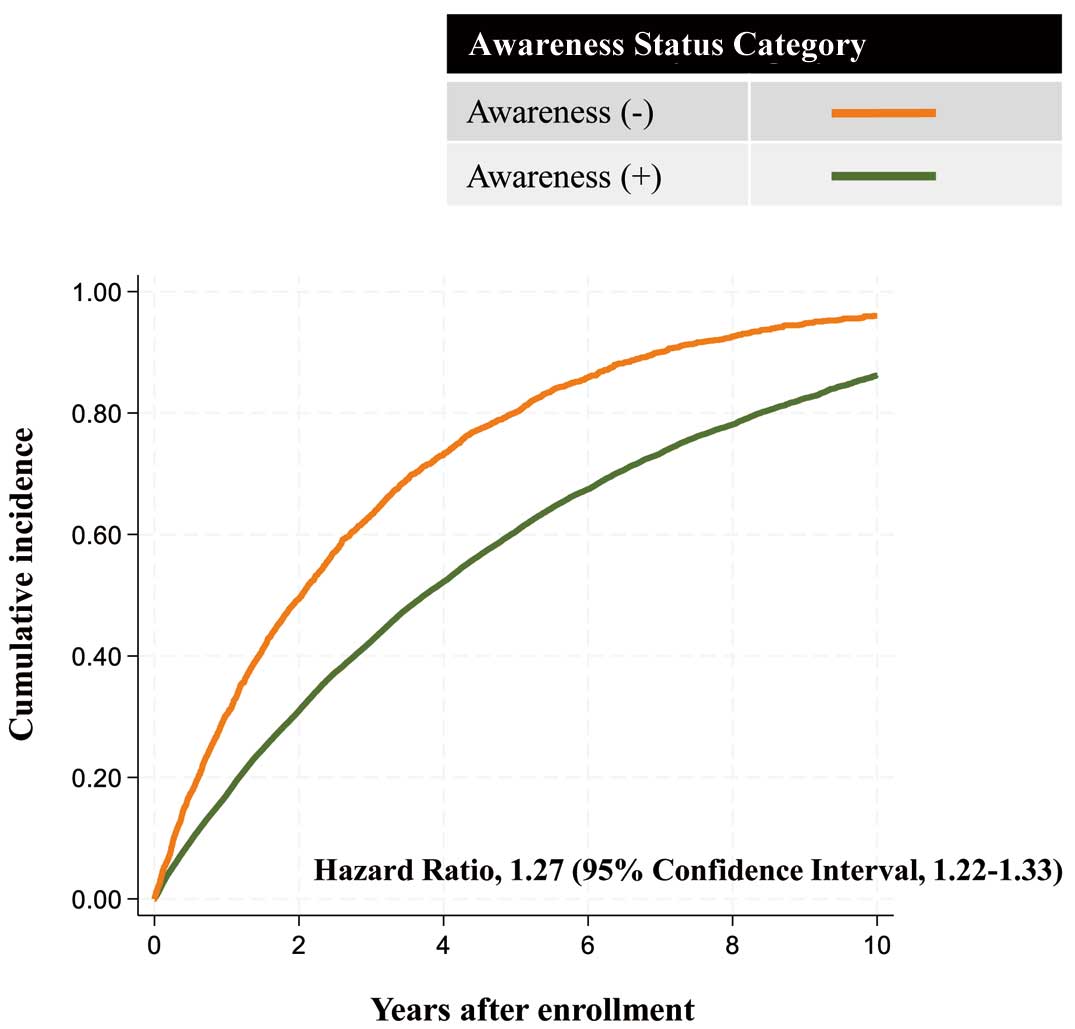
Baseline characteristics stratified by awareness of being prescribed antihypertensive medications were summarized using median value with the interquartile range (IQR) for continuous variables and numbers and percentages for categorical variables. The significance of differences was tested using the Mann-Whitney U test or Chi-squared test. Adjusted survival curves were used to compare the cumulative incidence of composite CVD events between individuals who were and who were not aware of being prescribed antihypertensive medications. The model was adjusted for age, sex, body mass index, SBP, number of prescriptions for antihypertensive medications, diabetes, dyslipidemia, cigarette smoking, alcohol consumption, and physical inactivity. Cox proportional hazards regression models were used to examine relationships between unawareness of being prescribed antihypertensive medications and the subsequent risk of developing CVD-related events. Model 1 was an unadjusted model. Model 2 was adjusted for age and sex, and Model 3 was adjusted for age, sex, body mass index, SBP, number of prescriptions for antihypertensive medications, diabetes, dyslipidemia, cigarette smoking, alcohol consumption, and physical inactivity.
Six sensitivity analyses were conducted. First, we extracted study participants with available estimated glomerular filtration rate (eGFR) data (n=166,689); a multivariate Cox proportional hazards regression model was used after adjusting for eGFR. Second, we repeated the primary analysis after excluding individuals with dementia (ICD-10 codes: F000–F002, F009, F010–F013, F018, F019, F03, G300–G309). Third, missing covariate data were imputed using multiple imputations with chained equations and 20 iterations. Fourth, analysis was performed among individuals with a follow-up period ≥1 year (i.e., induction period of 1 year). Fifth, we performed a subgroup analysis stratified by sex (male, female), age (≥50, <50 years), and SBP (≥130 [median], <130 mmHg). Sixth, we analyzed the relationship between unawareness of being prescribed antihypertensive medications and all-cause death. All statistical analyses were performed using Stata version 17 (StataCorp LLC, College Station, TX, USA). Statistical significance was set at two-tailed P<0.05.
Results
Baseline Characteristics
Baseline clinical characteristics of the study participants are presented in the Table. The median age of the participants was 56 years (IQR 50–61 years), 222,216 (70.8%) were male, and 19,607 (6.2%) individuals were unaware of being prescribed antihypertensive medications. Individuals who were unaware of their prescription of antihypertensive medications were younger than those who were aware of their prescription. The prevalence of obesity and dyslipidemia was lower in individuals who were unaware of being prescribed antihypertensive medications.
Table.
Baseline Characteristics
| |
Total
(n=313,715) |
Awareness of being prescribed
antihypertensive medications |
P value |
| Yes (n=294,108) |
No (n=19,607) |
| SBP (mmHg) |
130 [121–140] |
130 [122–140] |
128 [118–139] |
<0.001 |
| DBP (mmHg) |
82 [75–89] |
82 [75–89] |
81 [72–88] |
<0.001 |
| No. prescriptions for antihypertensive medications |
| 1 |
189,075 (60.3) |
173,483 (59.0) |
15,592 (79.5) |
<0.001 |
| 2 |
96,097 (30.6) |
92,777 (31.5) |
3,320 (16.9) |
|
| 3 |
23,451 (7.5) |
22,845 (7.8) |
606 (3.1) |
|
| 4 |
4,396 (1.4) |
4,321 (1.5) |
75 (0.4) |
|
| 5 |
636 (0.2) |
623 (0.2) |
13 (0.1) |
|
| 6 |
60 (0.0) |
59 (0.0) |
1 (0.0) |
|
| Age (years) |
56 [50–61] |
56 [50–62] |
52 [46–59] |
<0.001 |
| Male sex |
222,216 (70.8) |
209,231 (71.1) |
12,985 (66.2) |
<0.001 |
| BMI (kg/m2) |
25.0 [22.6–27.8] |
25.0 [22.7–27.9] |
24.1 [21.6–27.1] |
<0.001 |
| Obesity |
157,513 (50.2) |
149,321 (50.8) |
8,192 (41.8) |
<0.001 |
| Diabetes |
60,341 (19.2) |
56,476 (19.2) |
3,865 (19.7) |
0.079 |
| Dyslipidemia |
207,719 (66.2) |
195,750 (66.6) |
11,969 (61.0) |
<0.001 |
| Cigarette smoking |
78,106 (24.9) |
73,117 (24.9) |
4,989 (25.4) |
0.067 |
| Alcohol consumption |
111,266 (35.5) |
106,176 (36.1) |
5,090 (26.0) |
<0.001 |
| Physical inactivity |
169,844 (54.1) |
159,351 (54.2) |
10,493 (53.5) |
0.071 |
| Glucose (mg/dL) |
100 [92–112] |
100 [92–112] |
97 [89–109] |
<0.001 |
| LDL-C (mg/dL) |
121 [102–140] |
121 [102–140] |
121 [101–142] |
0.036 |
| HDL-C (mg/dL) |
58 [48–69] |
57 [48–69] |
59 [49–71] |
<0.001 |
| Triglycerides (mg/dL) |
110 [78–160] |
111 [78–160] |
102 [71–153] |
<0.001 |
Unless indicated otherwise, data are given as n (%) or the median [interquartile range]. P values were calculated using a Chi-squared test for categorical variables and the Mann-Whitney U test for continuous variables. BMI, body mass index; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure.
Unawareness of Being Prescribed Antihypertensive Medications and CVD-Related Events
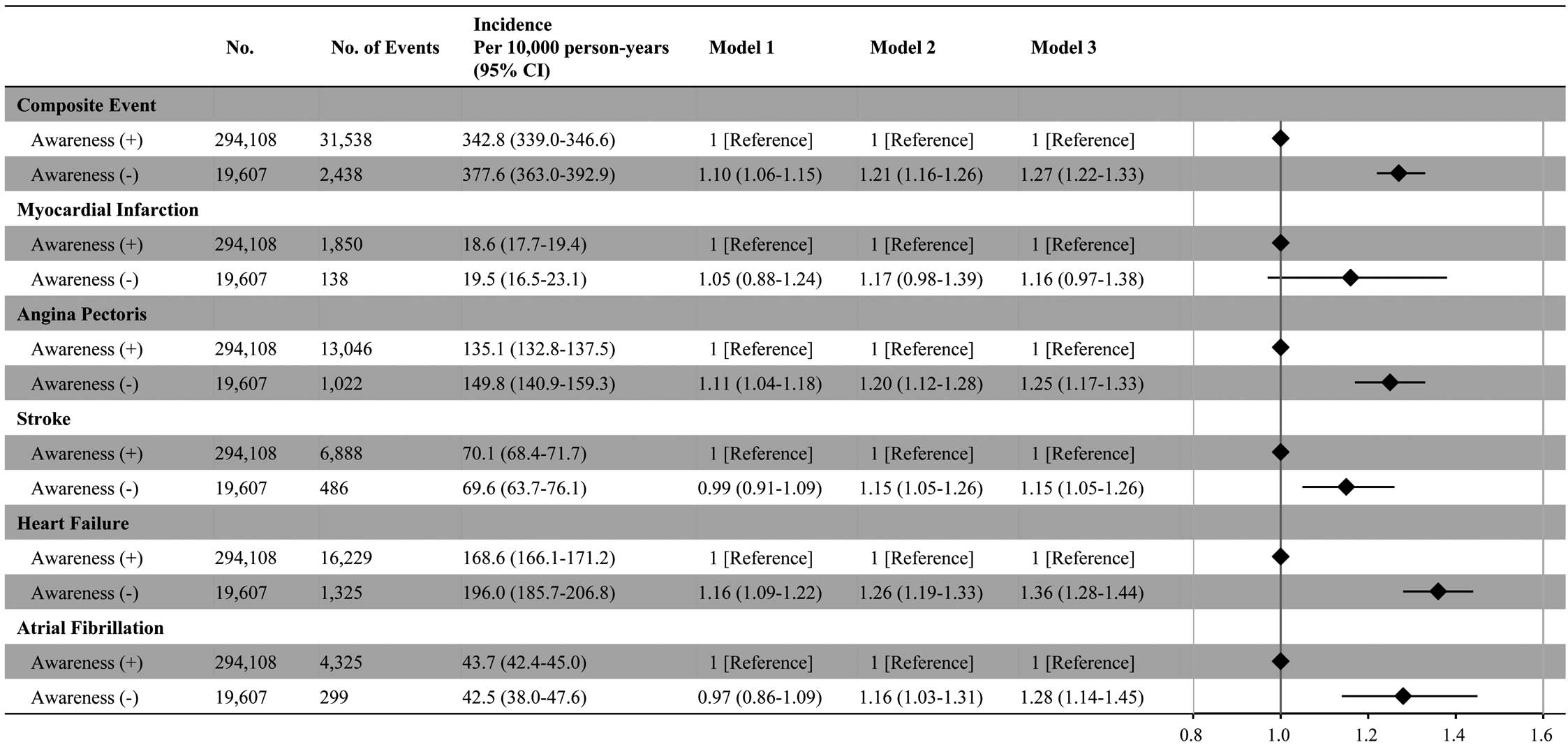
During a mean (±SD) observation period of 1,247±914 days, 33,976 composite CVD events were documented. Adjusted survival curves showed that the cumulative incidence of composite CVD events was higher in individuals who were unaware of being prescribed antihypertensive medications than in those who were aware of their prescription (Figure 2). Multivariable Cox regression analyses (Model 3) showed that unawareness of being prescribed antihypertensive medications was associated with a greater risk of developing composite CVD endpoints (hazard ratio [HR] 1.27; 95% confidence interval [95% CI] 1.22–1.33). HRs of unawareness of being prescribed antihypertensive medications were 1.16 (95% CI 0.97–1.38) for MI, 1.25 (95% CI 1.17–1.33) for AP, 1.15 (95% CI 1.05–1.26) for stroke, 1.36 (95% CI 1.28–1.44) for HF, and 1.28 (95% CI 1.14–1.45) for AF (Figure 3).
Sensitivity Analyses
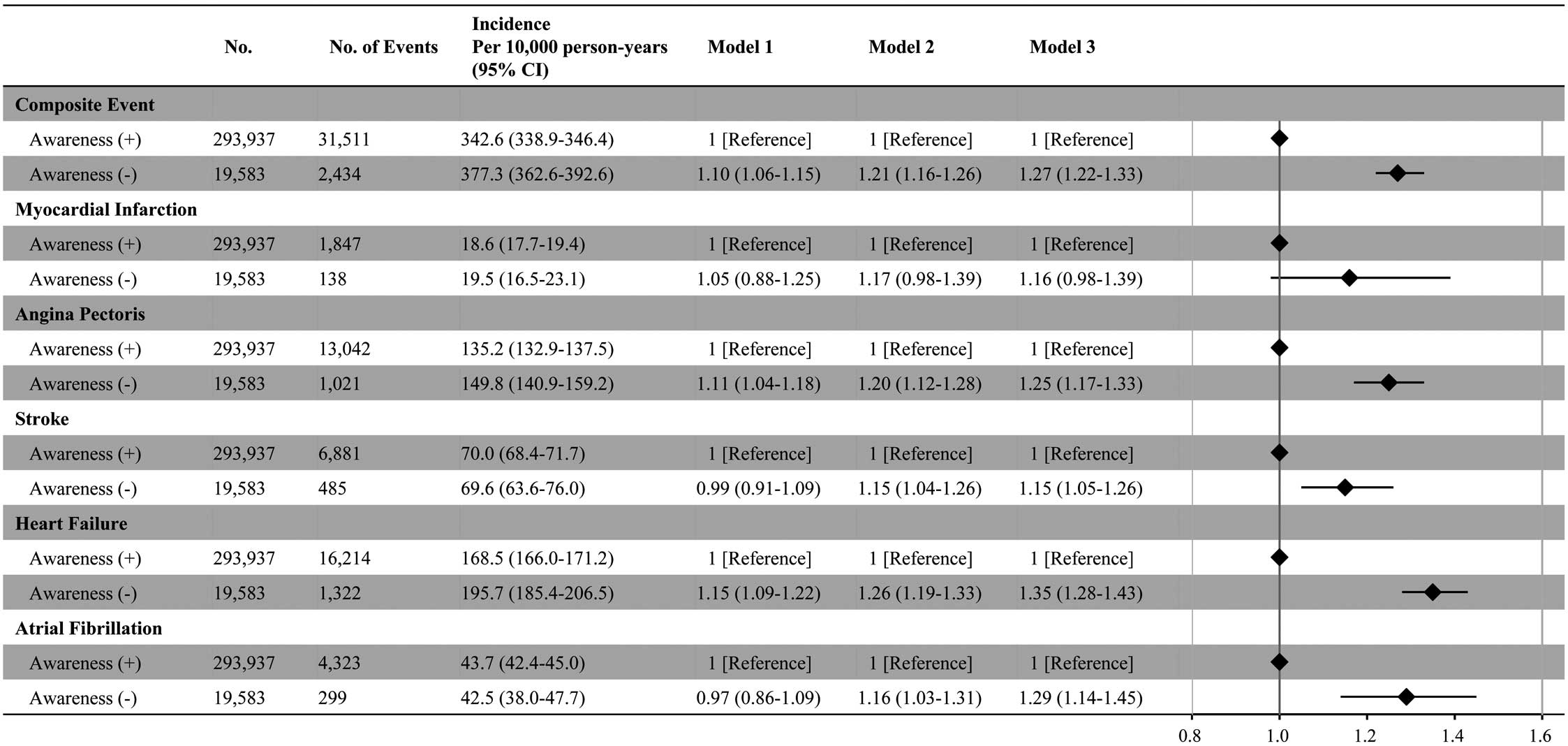
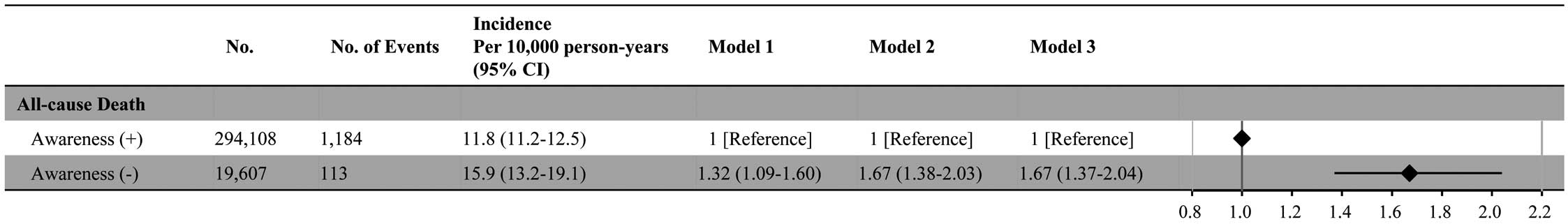
Six sensitivity analyses were conducted. First, 166,689 individuals for whom eGFR data were available were evaluated. Unawareness of being prescribed antihypertensive medications was associated with a higher risk of developing composite CVD endpoints, even after adjusting for eGFR (Supplementary Figure 1). Second, our main findings remained unchanged, even after excluding individuals with dementia (Figure 4). Third, primary analyses were performed after imputing missing data, including cigarette smoking, alcohol consumption, and physical inactivity, using multiple imputations. The positive association between unawareness of being prescribed antihypertensive medications and the risk of composite CVD endpoints was similar (Supplementary Figure 2). Fourth, we confirmed the robustness of the primary findings among individuals with a follow-up period of ≥1 year (Supplementary Figure 3). Fifth, a positive association between unawareness of being prescribed antihypertensive medications and the risk of the composite CVD endpoint was observed in all subgroups stratified by sex, age, and SBP (Figure 5). Sixth, unawareness of being prescribed antihypertensive medications was associated with a greater risk of all-cause death (Figure 6).
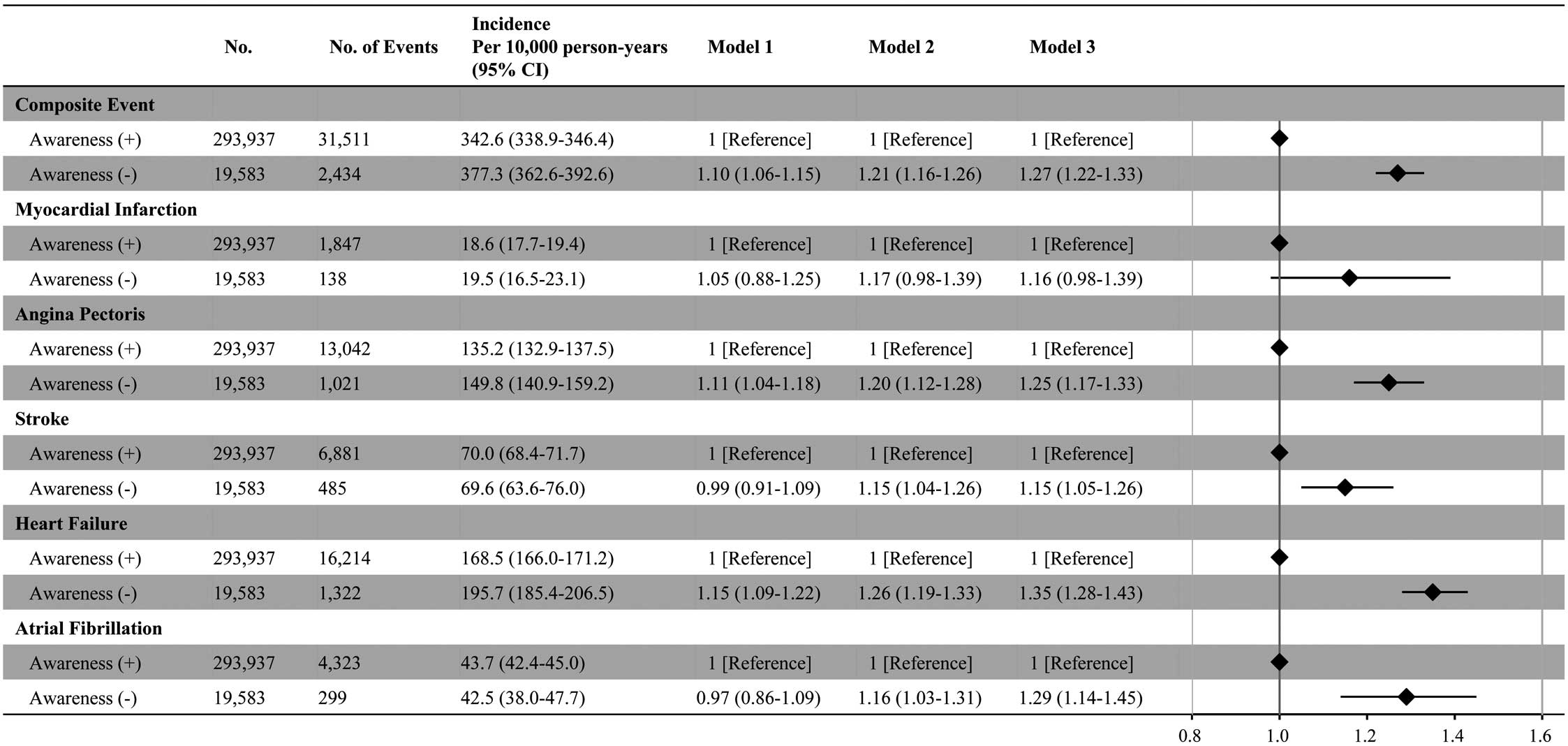
Discussion
In our nationwide study, which included 313,715 individuals with hypertension using antihypertensive medications, those who were unaware of being prescribed antihypertensive medications had a greater risk of developing subsequent CVD events than those who were aware of their prescription, even though they are young, have fewer additional comorbidities, and manage to maintain lower BP levels with a fewer number of prescribed antihypertensive medications. We confirmed the robustness of our primary findings using various sensitivity analyses. This is the first study to use a large-scale population-based cohort to demonstrate the relationship between unawareness of being prescribed antihypertensive medications and the risk of developing CVD events.
Patient’s awareness of major risk factors for CVD, such as hypertension, is pivotal in its prevention and management.3,6 An unawareness of CVD risk factors may lead to decreased motivation in seeking appropriate medical treatment and healthy behaviors for reducing the risk of CVD onset.11 A previous population-based study, which compared the epidemiology of hypertension among Asian Indians living in Singapore and India, revealed that the proportion of individuals aware of hypertension was higher among Indians living in urban Singapore than in rural India (72.4% vs. 25.3%).6 In addition, among Indians living in Singapore, most individuals who were aware of their condition were prescribed antihypertensive medications.6 These findings suggest that socioeconomic status may affect awareness of hypertension. Unawareness of hypertension may lead to poor adherence to antihypertensive treatment, which is associated with an increased risk of CVD. For example, previous epidemiological studies showed that the risk of poor blood pressure control and the development of CVD decreased progressively as adherence to antihypertensive medications increased.12–17 However, in our analysis, individuals who were unaware of being prescribed antihypertensive medications had lower blood pressure values. Furthermore, they possessed baseline characteristics that would typically classify them as low risk (younger age, lower number of prescriptions for antihypertensive medications, and lower prevalence of obesity or dyslipidemia). Indeed, a significant association between unawareness of being prescribed antihypertensive medications and CVD was not observed in the unadjusted analysis (Model 1). Nevertheless, in the analysis adjusted for baseline characteristics, unawareness of being prescribed antihypertensive medications was significantly associated with a higher risk of CVD. Therefore, in clinical practice, it is important to avoid overlooking unawareness of being prescribed antihypertensive medications. This study has clinical implications in that it identified an independent risk factor for CVD (i.e., unawareness of being prescribed antihypertensive medications) in a population that initially may not be considered high risk.
There are several potential explanations for the results of this study that have clinical implications. Among patients unaware of their antihypertensive medications prescription, there is a possibility of decreased long-term adherence to pharmacotherapy and subsequent poor blood pressure control, leading to an increased risk of developing CVD.12–14 Conversely, it should be noted that baseline blood pressure was lower in patients lacking awareness of their antihypertensive prescription. Further data need to be accumulated to identify the way in which unawareness of antihypertensive prescriptions could affect long-term adherence to pharmacotherapy and clinical outcomes. In addition, patients unaware of being prescribed antihypertensive medication may have underlying factors, such as cognitive impairment, that could serve as confounding variables. However, the main findings in the present study remained unchanged even after excluding individuals with dementia. Because this study was retrospective and observational, a causal relationship between the lack of awareness of antihypertensive prescriptions and the increased risk of subsequent CVD development cannot be established. Future prospective studies regarding educational interventions are needed to clarify whether improving patient awareness of being prescribed antihypertensive medications could lead to improved prognosis in patients with hypertension receiving antihypertensive treatment. At the very least, in clinical practice, physicians should be aware that approximately 6% of patients with hypertension being prescribed antihypertensive medications are unaware of their prescription, and such lack of awareness may be associated with an elevated risk of developing CVD at an earlier stage. Further, differences in survival curves between individuals who were and were not aware of being prescribed antihypertensive medications were observed from the beginning of the follow-up period. Such “awareness” among physicians could potentially contribute to improved quality of care and prognosis in patients with hypertension.
This study has several limitations, most of which are due to the use of the health checkup and administrative claims dataset, as described previously.8,18–20 The incidence of CVD events in our dataset is comparable to that in other epidemiological datasets in Japan,21,22 and previous studies have demonstrated high accuracy for recorded diagnoses (including CVD) in administrative claims databases in Japan.23,24 Therefore, we believe that our study could represent the current epidemiological condition. Nevertheless, because documented diagnoses in the claims database are generally less thoroughly validated, we acknowledge that uncertainty remains regarding the accuracy of CVD diagnoses. Furthermore, even after correcting for multiple covariates, the potential for residual confounding due to unmeasured variables (e.g., mental stress, socioeconomic status) remains, which could have influenced our primary findings. Individuals who lack prescribing awareness may also lack awareness of their hypertension. Unfortunately, this has not been assessed in health checkups, and therefore there is no information on this point in the JMDC Claims Database.
Conclusions
The present study, using a large-scale claims database, showed that individuals who were unaware of being pre-scribed antihypertensive medications had a greater risk of developing various CVD events than those who were aware of being prescribed antihypertensive medications, despite their younger age, the presence of fewer comorbidities, and the attainment of better BP control with a reduced regimen of antihypertensive medications. These results emphasize the importance of providing individuals with hypertension treated using antihypertensive medications with an accurate understanding of their treatment status and of patient education from healthcare providers.
Sources of Funding
This work was supported by grants from the Ministry of Health, Labour and Welfare, Japan (21AA2007) and the Ministry of Education, Culture, Sports, Science and Technology, Japan (20H03907, 21H03159, 21K08123, and 22K21133). The funding sources played no role in the present study.
Disclosures
H.K. and K.F. report having received research funding and scholarship funds from Medtronic Japan Co., Ltd, Boston Scientific Japan Co., Ltd, Biotronik Japan, Simplex QUANTUM Co., Ltd, and Fukuda Denshi, Central Tokyo Co., Ltd. I.K., K.N., and H.M. are members of Circulation Journal’s Editorial Team. The remaining authors have no conflicts of interest to disclose.
Author Contributions
Conception and design: H.K., Y.S., A.O., J.K., A.N., Y.Y., K.N., and I.K.; Analysis of data: Y.S., A.O., K.F., T.J., and H.Y.; Interpretation of data: H.K., A.O., K.F., H.M., K.N., H.Y., and I.K.; Drafting of the manuscript: H.K., A.O., Y.S., N.T., and H.M.; Critical revision for important intellectual content: N.T., H.M., Y.Y., H.Y., and I.K.; Final approval of the submitted manuscript: All authors.
IRB Information
This study was approved by the Clinical Research Review Board of The University of Tokyo (2018-10862). Because this retrospective study using the JMDC Claims Database involved analysis of deidentified data, individuals did not need to provide informed consent.
Data Availability
The JMDC Claims Database is available for purchase from JMDC Inc. (https://www.jmdc.co.jp/en/).
Supplementary Files
Please find supplementary file(s);
https://doi.org/10.1253/circj.CJ-24-0039
References
- 1.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2224–2260.
- 2.
Fenech G, Vallée A, Cherfan M, Kab S, Goldberg M, Zins M, et al. Poor awareness of hypertension in France: The CONSTANCES population-based study. Am J Hypertens 2020; 33: 543–551.
- 3.
Man REK, Gan AHW, Fenwick EK, Gan ATL, Gupta P, Sabanayagam C, et al. Prevalence, determinants and association of unawareness of diabetes, hypertension and hypercholesterolemia with poor disease control in a multi-ethnic Asian population without cardiovascular disease. Popul Health Metr 2019; 17: 17.
- 4.
Liew SJ, Lee JT, Tan CS, Koh CHG, Van Dam R, Müller-Riemenschneider F. Sociodemographic factors in relation to hypertension prevalence, awareness, treatment and control in a multi-ethnic Asian population: A cross-sectional study. BMJ Open 2019; 9: e025869.
- 5.
Owolabi EO, Goon DT, Adeniyi OV, Seekoe E. Social epidemiology of hypertension in Buffalo City Metropolitan Municipality (BCMM): Cross-sectional study of determinants of prevalence, awareness, treatment and control among South African adults. BMJ Open 2017; 7: e014349.
- 6.
Yip W, Wong TY, Jonas JB, Zheng Y, Lamoureux EL, Nangia V, et al. Prevalence, awareness, and control of hypertension among Asian Indians living in urban Singapore and rural India. J Hypertens 2013; 31: 1539–1546.
- 7.
Kaneko H, Itoh H, Kamon T, Fujiu K, Morita K, Michihata N, et al. Association of cardiovascular health metrics with subsequent cardiovascular disease in young adults. J Am Coll Cardiol 2020; 76: 2414–2416.
- 8.
Kaneko H, Yano Y, Itoh H, Morita K, Kiriyama H, Kamon T, et al. Association of blood pressure classification using the 2017 American College of Cardiology/American Heart Association Blood Pressure guideline with risk of heart failure and atrial fibrillation. Circulation 2021; 143: 2244–2253.
- 9.
Suzuki Y, Kaneko H, Okada A, Matsuoka S, Fujiu K, Michihata N, et al. Kidney outcomes in patients with diabetes mellitus did not differ between individual sodium–glucose cotransporter-2 inhibitors. Kidney Int 2022; 102: 1147–1153.
- 10.
Kaneko H, Yano Y, Okada A, Itoh H, Suzuki Y, Yokota I, et al. Age-dependent association between modifiable risk factors and incident cardiovascular disease. J Am Heart Assoc 2023; 12: e027684.
- 11.
Langellier BA, Garza JR, Glik D, Prelip ML, Brookmeyer R, Roberts CK, et al. Immigration disparities in cardiovascular disease risk factor awareness. J Immigr Minor Health 2012; 14: 918–925.
- 12.
Herttua K, Tabák AG, Martikainen P, Vahtera J, Kivimäki M. Adherence to antihypertensive therapy prior to the first presentation of stroke in hypertensive adults: Population-based study. Eur Heart J 2013; 34: 2933–2939.
- 13.
Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation 2009; 120: 1598–1605.
- 14.
Degli Esposti L, Saragoni S, Benemei S, Batacchi P, Geppetti P, Di Bari M, et al. Adherence to antihypertensive medications and health outcomes among newly treated hypertensive patients. Clinicoecon Outcomes Res 2011; 3: 47–54.
- 15.
Caro JJ, Salas M, Speckman JL, Raggio G, Jackson JD. Persistence with treatment for hypertension in actual practice. CMAJ 1999; 160: 31–37.
- 16.
Shea S, Misra D, Ehrlich MH, Field L, Francis CK. Correlates of nonadherence to hypertension treatment in an inner-city minority population. Am J Public Health 1992; 82: 1607–1612.
- 17.
Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Levin R, Avorn J. Compliance with antihypertensive therapy among elderly Medicaid enrollees: The roles of age, gender, and race. Am J Public Health 1996; 86: 1805–1808.
- 18.
Kaneko H, Itoh H, Yotsumoto H, Kiriyama H, Kamon T, Fujiu K, et al. Association of isolated diastolic hypertension based on the cutoff value in the 2017 American College of Cardiology/American Heart Association blood pressure guidelines with subsequent cardiovascular events in the general population. J Am Heart Assoc 2020; 9: e017963.
- 19.
Matsuoka S, Kaneko H, Okada A, Morita K, Itoh H, Michihata N, et al. Age modified relationship between modifiable risk factors and the risk of atrial fibrillation. Circ Arrhythm Electrophysiol 2022; 15: e010409.
- 20.
Suzuki Y, Kaneko H, Yano Y, Okada A, Itoh H, Matsuoka S, et al. Interaction of blood pressure and glycemic status in developing cardiovascular disease: Analysis of a nationwide real-world database. J Am Heart Assoc 2023; 12: e026192.
- 21.
Miura K, Nakagawa H, Ohashi Y, Harada A, Taguri M, Kushiro T, et al. Four blood pressure indexes and the risk of stroke and myocardial infarction in Japanese men and women: A meta-analysis of 16 cohort studies. Circulation 2009; 119: 1892–1898.
- 22.
Saito I, Yamagishi K, Kokubo Y, Yatsuya H, Iso H, Sawada N, et al. Association between mortality and incidence rates of coronary heart disease and stroke: The Japan Public Health Center-based prospective (JPHC) study. Int J Cardiol 2016; 222: 281–286.
- 23.
Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol 2017; 27: 476–482.
- 24.
Fujihara K, Yamada-Harada M, Matsubayashi Y, Kitazawa M, Yamamoto M, Yaguchi Y, et al. Accuracy of Japanese claims data in identifying diabetes-related complications. Pharmacoepidemiol Drug Saf 2021; 30: 594–601.