Abstract
Background: Limited data exist regarding the prognostic implications of N-terminal pro-B-type natriuretic peptide (NT-proBNP) in patients with non-ST-elevation myocardial infarction (NSTEMI) who undergo percutaneous coronary intervention (PCI).
Methods and Results: Of 13,104 patients in the nationwide Korea Acute Myocardial Infarction Registry-National Institutes of Health, 3,083 patients with NSTEMI who underwent PCI were included in the present study. The primary endpoint was major adverse cardiovascular events (MACE) at 3 years, a composite of all-cause death, recurrent myocardial infarction, unplanned repeat revascularization, and admission for heart failure. NT-proBNP was measured at the time of initial presentation for the management of NSTEMI, and patients were divided into a low (<700 pg/mL; n=1,813) and high (≥700 pg/mL; n=1,270) NT-proBNP group. The high NT-proBNP group had a significantly higher risk of MACE, driven primarily by a higher risk of cardiac death or admission for heart failure. These results were consistent after confounder adjustment by propensity score matching and inverse probability weighting analysis.
Conclusions: In patients with NSTEMI who underwent PCI, an initial elevated NT-proBNP concentration was associated with higher risk of MACE at 3 years, driven primarily by higher risks of cardiac death or admission for heart failure. These results suggest that the initial NT-proBNP concentration may have a clinically significant prognostic value in NSTEMI patients undergoing PCI.
Non-ST-elevation myocardial infarction (NSTEMI) results in significant ischemic myocardial damage, caused primarily by a decrease in coronary blood flow, which requires revascularization.1 One of the treatment options for acute phase management to restore coronary blood flow and minimize ischemic myocardial damage is percutaneous coronary intervention (PCI).2 With recent advances in biomarker assays, such as high-sensitivity cardiac troponin for a working diagnosis of acute coronary syndrome (ACS), NSTEMI has become the predominant clinical presentation among the total ACS population.3,4
In this regard, there is a growing need to identify reliable prognostic biomarkers for risk stratification and long-term guidance of therapeutic decisions in NSTEMI patients undergoing PCI. Nevertheless, cardiac enzymes such as troponin and creatine kinase-myocardial band (CK-MB), commonly used in the diagnosis of acute myocardial infarction (MI), failed to demonstrate predictive value in long-term prognosis and risk stratification in NSTEMI patients.5–7 Although previous studies evaluated novel biomarkers associated with the prognosis of NSTEMI patients, the clinical utility of these biomarkers has not been fully validated as yet.8–10
N-terminal pro-B-type natriuretic peptide (NT-proBNP), a prohormone secreted by ventricular myocytes in response to myocardial stress and ventricular stretching, has been recognized as a promising biomarker for various cardiovascular diseases, including congestive heart failure (CHF), valvular heart disease, pulmonary hypertension, and cardiomyopathies.11–16 Although there have been few studies presenting the prognostic value of NT-proBNP in patients with NSTEMI,17,18 clinical evidence of NT-proBNP in NSTEMI patients who underwent PCI is still limited due to small sample sizes and limited follow-up durations of previous studies. In this regard, the aim of the present study was to evaluate the clinical relevance of NT-proBNP for predicting clinical outcomes among NSTEMI patients after PCI using a nationwide multicenter registry.
Methods
Study Protocol and Population Selection
The study population was derived from the nationwide multicenter prospective Korea Acute Myocardial Infarction Registry-National Institutes of Health (KAMIR-NIH). This dedicated registry consecutively enrolled patients with acute MI from 20 tertiary university hospitals in South Korea from November 2011 to December 2015. A detailed study protocol has been published previously.19,20 The protocol of KAMIR-NIH was approved by the ethics committees of each participating center and written informed consent was obtained from all participants. The registry protocol adhered to the tenets of the Declaration of Helsinki.
Of the 13,104 patients enrolled in KAMIR-NIH, we selected patients who underwent PCI for NSTEMI, which was defined as acute MI without newly detected ST-elevation in ≥2 contiguous leads measuring ≥0.1 mV or a new left bundle branch block on a 12-lead electrocardiogram (ECG), accompanied by an increase of at least 1 cardiac marker of necrosis.20 Patients with ST-elevation myocardial infarction (STEMI; n=6,325), those for whom NT-proBNP concentrations at the time of initial presentation were unavailable (n=2,202), those who did not undergo PCI (n=1,159), and those lost to follow-up in <1 year (n=335) were excluded from the study (Figure 1). Finally, 3,083 patients were included in the analysis and were classified into a low or high NT-proBNP group using an optimal cut-off value of 700pg/mL NT-proBNP, as determined by receiver operating characteristic (ROC) curve analysis (Supplementary Figure 1).
Patient Management, Data Collection, and Follow-up
Patients were treated according to current guidelines and coronary interventions were performed using standard techniques. The choice of treatment strategy, such as the type, diameter, length, and number of stents, the use of intravascular imaging devices, thrombus aspiration, or percutaneous cardiopulmonary support devices, as well as the selection of medications were left to the operator’s discretion. PCI was considered successful if the final residual stenosis was <30% with Thrombolysis in Myocardial Infarction (TIMI) Grade 3 flow. Complete revascularization was achieved when successful PCI was performed on all coronary arteries with significant stenosis during the index hospitalization. Following the index procedure, all patients were prescribed aspirin and a P2Y12
inhibitor for at least 12 months, unless contraindications were present. The choice of P2Y12
inhibitor was at the operator’s discretion in accordance with current guidelines and considering individual patient factors, such as bleeding risk. Additional medications, including renin-angiotensin-aldosterone system blockers, β-blockers, and statins, were also prescribed based on practice guidelines.21,22
Demographic features and cardiovascular risk factors were collected by detailed patient interview. NT-proBNP was measured at the time of initial presentation for the management of NSTEMI. During the index hospitalization, features of coronary angiography and specific procedural details of PCI, as well as information about complications and discharge medications, were documented. After discharge, patients were followed up at 6, 12, 24, and 36 months through outpatient clinic visits or telephone contact, and whenever any clinical event occurred. Independent clinical research coordinators collected all data using a web-based case report form on the internet-based Clinical Research and Trial management system (iCReaT), a data management system established by the Centers for Disease Control and Prevention, Ministry of Health and Welfare, Republic of Korea (iCReaT Study No. C110016).
Study Outcomes
The primary outcome was a major adverse cardiovascular event (MACE), a composite of all-cause death, recurrent MI, unplanned repeat revascularization, and admission for heart failure, at 3 years. Secondary outcomes included the individual components of MACE and a composite of cardiac death or admission for heart failure at 3 years. Follow-up echocardiographic data were assessed among 1,054 patients with a left ventricular ejection fraction (LVEF) >50% at the index echocardiography and for whom both index and follow-up echocardiography data were available. Recurrent MI was defined as the recurrence of symptoms or the presence of electrocardiographic changes associated with a rise in cardiac biomarker concentrations above the upper limit of normal. Periprocedural MI was not included as a clinical outcome. Clinically driven revascularization that occurred after discharge from the index hospitalization was coded as an unplanned repeat revascularization event according to the Academic Research Consortium definitions.23 Clinical events that occurred within the 3-year follow-up period were analyzed in the present study. The median follow-up duration of the study was 1,062 days (interquartile range: 1,086.0–1,155.0 days).
Statistical Analysis
All discrete and categorical variables are presented as numbers and relative frequencies (percentages). Categorical data were compared using the Chi-squared test. Continuous variables are reported as the mean±SD and were compared using Student’s t-test. The cumulative incidence of clinical events was estimated by the Kaplan-Meier method and compared using the log-rank test. The Cox proportional hazards model was used to estimate hazard ratios (HRs) with 95% confidence intervals (CIs) for MACE. The assumption of proportionality was assessed by the Schoenfeld residuals and graphically by the log-log plot. A multivariable Cox model was fitted using all variables with P<0.1 from the univariable analyses and variables that could be clinically relevant. The final model included the following variables: age, sex, high Killip class (Class 3 or 4), hypertension, diabetes, end-stage renal disease, previous CHF, LVEF <50%, left ventricular (LV) end-diastolic diameter, atrial fibrillation, 3-vessel disease, and failure to achieve complete revascularization. A restricted cubic spline curve with 3 knots was used to evaluate the prognostic implications of NT-proBNP on MACE at 3 years as a continuous value.
For sensitivity analysis, propensity score matching and inverse probability treatment-weighting (IPTW) analyses were performed using the propensity score from a multivariable logistic regression model. The covariables of age, sex, body mass index (BMI), high Killip class (Class 3 or 4), hypertension, diabetes, dyslipidemia, end-stage renal disease, previous CHF, previous MI, previous cerebrovascular accident (CVA), LVEF, multivessel disease, Type B2 or C lesion according to the American College of Cardiology (ACC)/American Heart Association (AHA) classification,24 and failure to achieve complete revascularization were included in the model. The balance between the 2 groups after propensity score matching or IPTW adjustment was assessed by calculating percentage standardized mean differences, which were within 10% across all matched covariables, suggesting successful balance was achieved between the comparative groups by propensity score matching and IPTW adjustment (Supplementary Table 1). A subgroup analysis of the primary outcome was performed according to clinical and procedural factors of interest between the low and high NT-proBNP groups.
All probability values were 2-sided, and P<0.05 was considered statistically significant. Statistical analyses were performed using SPSS 27.0 for Windows (SPSS-PC, Chicago, IL, USA) and R version 4.3.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline Clinical Characteristics
Baseline clinical characteristics are summarized in Table 1. Among the total population, 1,813 (58.8%) patients were categorized in the low (<700 pg/mL) NT-proBNP group and 1,270 (41.2%) patients were classified in the high (≥700 pg/mL) NT-proBNP group. The mean age of the entire cohort was 64.5±12.0 years and 71.5% were male. Patients in the high NT-proBNP group were older, presented with higher Killip class (Class 3 or 4), and lower systolic and diastolic blood pressures than those in the low NT-proBNP group. In addition, patients in the high NT-proBNP group had a higher prevalence of major cardiovascular comorbidities, including hypertension, diabetes, end-stage renal disease, previous MI, angina, CVA, CHF, and atrial fibrillation, than those in the low NT-proBNP group. The high NT-proBNP group had lower LVEF (48.6±11.9% vs. 57.1±8.3%; P<0.001) and higher LV end-diastolic diameter (50.3±7.4 mm vs. 49.0±5.5 mm; P<0.001) than the low NT-proBNP group. Conversely, there was no significant difference in peak cardiac troponin-I concentrations between the 2 groups (Table 1).
Table 1.
Baseline Clinical Characteristics
| |
Total population
(n=3,083) |
NT-proBNP |
P value |
| Low (n=1,813) |
High (n=1,270) |
| Age (years) |
64.5±12.0 |
60.8±11.3 |
69.8±11.0 |
<0.001 |
| Male sex |
2,203 (71.5) |
1,509 (83.2) |
694 (54.6) |
<0.001 |
| BMI (kg/m2) |
24.1±3.3 |
24.5±3.1 |
23.4±3.5 |
<0.001 |
| Killip class |
|
|
|
<0.001 |
| Class 1 |
2,492 (80.8) |
1,640 (90.5) |
852 (67.1) |
|
| Class 2 |
283 (9.2) |
116 (6.4) |
167 (13.1) |
|
| Class 3 |
265 (8.6) |
43 (2.4) |
222 (17.5) |
|
| Class 4 |
43 (1.4) |
14 (0.8) |
29 (2.3) |
|
| Hemodynamic data |
| SBP (mmHg) |
135.8±26.6 |
138.1±25.7 |
132.6±27.6 |
<0.001 |
| DBP (mmHg) |
81.3±15.7 |
82.8±15.2 |
79.1±16.3 |
<0.001 |
| Heart rate (beats/min) |
79.2±17.7 |
75.6±15.5 |
84.3±19.4 |
<0.001 |
| Cardiovascular risk factors |
| Hypertension |
1,650 (53.5) |
854 (47.1) |
796 (62.7) |
<0.001 |
| Diabetes |
943 (30.6) |
444 (24.5) |
499 (39.3) |
<0.001 |
| Current smoking |
1,141 (37.0) |
832 (45.9) |
309 (24.3) |
<0.001 |
| Dyslipidemia |
351 (11.4) |
246 (13.6) |
105 (8.3) |
<0.001 |
| End-stage renal disease |
63 (2.0) |
1 (0.1) |
62 (4.9) |
<0.001 |
| Previous MI |
256 (8.3) |
133 (7.3) |
123 (9.7) |
0.024 |
| Previous angina |
351 (11.4) |
171 (9.4) |
180 (14.2) |
<0.001 |
| Previous CVA |
207 (6.7) |
82 (4.5) |
125 (9.8) |
<0.001 |
| Previous CHF |
47 (1.5) |
11 (0.6) |
36 (2.8) |
<0.001 |
| Family history of IHD |
19 (0.6) |
16 (0.9) |
3 (0.2) |
0.043 |
| Cardiac enzyme level |
| Peak CK-MB (ng/mL) |
56.8±85.9 |
62.7±90.9 |
48.3±77.4 |
<0.001 |
| Peak troponin-I (ng/mL) |
21.0±42.2 |
20.8±42.6 |
21.2±41.6 |
0.824 |
| Laboratory data |
| Hemoglobin (g/dL) |
13.6±2.1 |
14.3±1.6 |
12.6±2.2 |
<0.001 |
| Creatinine (mg/dL) |
1.1±1.0 |
0.9±0.3 |
1.4±1.5 |
<0.001 |
| Total cholesterol (mg/dL) |
178.0±45.7 |
184.3±44.6 |
169.0±45.7 |
<0.001 |
| HDL-C (mg/dL) |
42.9±11.5 |
43.0±10.8 |
42.7±12.6 |
0.584 |
| LDL-C (mg/dL) |
111.9±38.1 |
116.5±36.6 |
105.2±39.1 |
<0.001 |
| HbA1c (%) |
6.5±1.5 |
6.4±1.4 |
6.7±1.6 |
0.001 |
| Medications at discharge |
| Aspirin |
3,077 (99.8) |
1,810 (99.8) |
1,267 (99.8) |
0.981 |
| Clopidogrel |
2,439 (79.1) |
1,375 (75.8) |
1,064 (83.8) |
<0.001 |
| Prasugrel |
354 (11.5) |
255 (14.1) |
99 (7.8) |
<0.001 |
| Ticagrelor |
709 (23.0) |
441 (24.3) |
268 (21.1) |
0.040 |
| RAAS blocker |
2,555 (82.9) |
1,504 (83.0) |
1,051 (82.8) |
0.923 |
| β-blocker |
2,657 (86.2) |
1,577 (87.0) |
1,080 (85.0) |
0.137 |
| Statin |
2,931 (95.1) |
1,746 (96.3) |
1,185 (93.3) |
<0.001 |
| Oral anticoagulant |
88 (2.9) |
14 (0.8) |
74 (5.8) |
<0.001 |
| Echocardiographic data |
| LVEF (%) |
53.6±10.8 |
57.1±8.3 |
48.6±11.9 |
<0.001 |
| LVEDd (mm) |
49.5±6.4 |
49.0±5.5 |
50.3±7.4 |
<0.001 |
| Atrial fibrillation |
136 (4.4) |
39 (2.2) |
97 (7.6) |
<0.001 |
Unless indicated otherwise, data are presented as the mean±SD or n (%). BMI, body mass index; CHF, congestive heart failure; CK-MB, creatine kinase-myocardial band; CVA, cerebrovascular accident; DBP, diastolic blood pressure; HDL-C, high density lipoprotein cholesterol; IHD, ischemic heart disease; LDL-C, low density lipoprotein cholesterol; LVEDd, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NT-proBNP, N-terminal pro-B-type natriuretic peptide; RAAS, renin-angiotensin-aldosterone system; SBP, systolic blood pressure.
Procedural Characteristics
Table 2 presents the procedural characteristics in the study population. The high NT-proBNP group had a higher prevalence of left main artery disease and 3-vessel disease than the low NT-proBNP group. More extensive coronary artery disease in the high NT-proBNP group resulted in lower achievement of complete revascularization during the index hospitalization than in the low NT-proBNP group (64.9% vs. 72.2%; P<0.001). Pre- and post-PCI TIMI flow did not differ significantly between the 2 groups. Intravascular imaging was more commonly used in the low NT-proBNP group than high NT-proBNP group (23.3% vs. 18.0%, respectively; P<0.001), whereas mechanical hemodynamic support was more frequently used in the high NT-proBNP group than low NT-proBNP group (1.4% vs. 0.4%, respectively; P=0.007).
Table 2.
Baseline Procedural Profiles
| |
Total population
(n=3,083) |
NT-proBNP |
P value |
| Low (n=1,813) |
High (n=1,270) |
| Angiographic disease extent |
| Single vessel disease |
1,399 (45.4) |
898 (49.5) |
501 (39.4) |
<0.001 |
| Three-vessel disease |
583 (18.9) |
286 (15.8) |
297 (23.4) |
<0.001 |
| Left main artery disease |
157 (5.1) |
71 (3.9) |
86 (6.8) |
0.001 |
| Culprit-only PCI at index procedure |
2,287 (74.2) |
1,386 (76.4) |
901 (70.9) |
0.001 |
| Complete revascularization during index hospitalization |
2,133 (69.2) |
1,309 (72.2) |
824 (64.9) |
<0.001 |
| Culprit lesion location |
|
|
|
<0.001 |
| Unprotected left main artery |
75 (2.4) |
31 (1.7) |
44 (3.5) |
|
| LAD |
1,304 (42.3) |
710 (39.2) |
594 (46.8) |
|
| LCX |
799 (25.9) |
521 (28.7) |
278 (21.9) |
|
| RCA |
905 (29.4) |
551 (30.4) |
354 (27.9) |
|
| ACC/AHA Type B2/C lesionA |
2,602 (84.4) |
1,492 (82.3) |
1,110 (87.4) |
<0.001 |
| Transradial approach |
1,597 (51.8) |
997 (55.0) |
600 (47.2) |
<0.001 |
| Glycoprotein IIb/IIIa inhibitor |
242 (7.8) |
152 (8.4) |
90 (7.1) |
0.211 |
| Thrombus aspiration |
425 (13.8) |
281 (15.5) |
144 (11.3) |
0.001 |
| Treatment modalities |
|
|
|
0.813 |
| Drug-eluting stent |
2,189 (71.0) |
1,284 (70.8) |
905 (71.3) |
|
| Plain balloon angioplasty |
252 (8.2) |
153 (8.4) |
99 (7.8) |
|
| Others |
642 (20.8) |
376 (20.7) |
266 (20.9) |
|
| Stent diameter (mm) |
3.10±0.43 |
3.12±0.44 |
3.06±0.41 |
<0.001 |
| Total stent length (mm) |
30.01±15.60 |
28.95±14.54 |
31.51±16.87 |
<0.001 |
| Total no. stents implanted |
1.11±0.55 |
1.08±0.53 |
1.13±0.57 |
0.016 |
| Pre-PCI TIMI flow |
|
|
|
0.356 |
| Grade 0 |
877 (28.4) |
509 (28.1) |
368 (29.0) |
|
| Grade 1 |
373 (12.1) |
232 (12.8) |
141 (11.1) |
|
| Grade 2 or 3 |
1,833 (59.5) |
1,072 (59.1) |
761 (59.9) |
|
| Post-PCI TIMI flow |
|
|
|
0.641 |
| Grade 0 |
7 (0.2) |
3 (0.2) |
4 (0.3) |
|
| Grade 1 |
6 (0.2) |
4 (0.2) |
2 (0.2) |
|
| Grade 2 or 3 |
3,070 (99.6) |
1,806 (99.6) |
1,264 (99.5) |
|
| Intravascular imaging |
650 (21.1) |
422 (23.3) |
228 (18.0) |
<0.001 |
| IVUS |
573 (18.6) |
364 (20.1) |
209 (16.5) |
0.013 |
| OCT |
92 (3.0) |
66 (3.6) |
26 (2.0) |
0.014 |
| Mechanical hemodynamic support |
26 (0.8) |
8 (0.4) |
18 (1.4) |
0.007 |
| IABP |
24 (0.8) |
8 (0.4) |
16 (1.3) |
0.019 |
| ECMO |
3 (0.1) |
0 (0.0) |
3 (0.2) |
0.138 |
Unless indicated otherwise, data are presented as the mean±SD or n (%). AType B2 or C lesions according to American College of Cardiology (ACC)/American Heart Association (AHA) classification.24 ECMO, extracorporeal membrane oxygenation; IABP, intra-aortic balloon pump; IVUS, intravascular ultrasound; LAD, left anterior descending artery; LCX, left circumflex artery; NT-proBNP, N-terminal pro-B-type natriuretic peptide; OCT, optical coherence tomography; PCI, percutaneous coronary intervention; RCA, right coronary artery; TIMI, Thrombolysis in Myocardial Infarction.
Clinical Outcomes According to NT-proBNP Concentration
A comparison of clinical outcomes between the 2 groups is presented in Table 3 and Figure 2. The risk of MACE at 3 years was significantly higher in the high than low NT-proBNP group (29.5% vs. 12.3%, respectively; adjusted [a] HR 1.68; 95% CI 1.37–2.05; P<0.001). The higher risk of MACE in the high NT-proBNP group was primarily driven by a higher risk of cardiac death or admission for heart failure in this group (15.6% vs. 2.2%; aHR 2.86; 95% CI 1.94–4.21; P<0.001). The high NT-proBNP group had a significantly higher risk of all-cause death, cardiac death, recurrent MI, and admission for heart failure than the low NT-proBNP group. Conversely, there was no significant difference in the risk of unplanned revascularization between the 2 groups (Table 3; Supplementary Figure 2). There was a significant association between the NT-proBNP concentration and risk of MACE at 3 years as a continuous value (P<0.001; Supplementary Figure 3).
Table 3.
Clinical Outcomes at 3 Years According to Baseline NT-proBNP Concentration
| |
NT-proBNP |
Univariable analysis |
Multivariable analysisA |
Low
(n=1,813) |
High
(n=1,270) |
HR |
95% CI |
P value |
HR |
95% CI |
P value |
| MACEB |
216 (12.3) |
359 (29.5) |
2.63 |
2.23–3.12 |
<0.001 |
1.68 |
1.37–2.05 |
<0.001 |
| All-cause death |
44 (2.5) |
153 (12.8) |
5.30 |
3.79–7.42 |
<0.001 |
2.12 |
1.44–3.10 |
<0.001 |
| Cardiac death |
24 (1.4) |
87 (7.5) |
5.54 |
3.53–8.70 |
<0.001 |
1.88 |
1.13–3.16 |
0.016 |
| Recurrent MI |
31 (2.2) |
58 (6.3) |
2.91 |
1.88–4.50 |
<0.001 |
1.88 |
1.12–3.16 |
0.017 |
Unplanned repeat
revascularization |
159 (9.0) |
143 (12.3) |
1.34 |
1.08–1.70 |
0.008 |
1.27 |
0.96–1.67 |
0.089 |
| Admission for HF |
14 (0.8) |
115 (9.6) |
12.63 |
7.25–21.99 |
<0.001 |
4.74 |
2.60–8.66 |
<0.001 |
Cardiac death or
admission for HF |
38 (2.2) |
186 (15.6) |
7.71 |
5.44–10.92 |
<0.001 |
2.86 |
1.94–4.21 |
<0.001 |
Unless indicated otherwise, data are shown as n (%). The cumulative incidence of clinical outcomes is presented as Kaplan-Meier estimates over a median follow-up of 1,062 days. AThe adjusted variables included in the multivariable analysis were age, sex, high Killip class (Class 3 or 4), hypertension, diabetes, end-stage renal disease, previous CHF, LVEF <50%, LVEDd, atrial fibrillation, 3-vessel disease, and failure to achieve complete revascularization. BMajor adverse cardiovascular events (MACE) were defined as a composite of all-cause death, recurrent MI, unplanned repeat revascularization, or admission for heart failure (HF). CI, confidence interval; HR, hazard ratio. Other abbreviations as in Table 1.

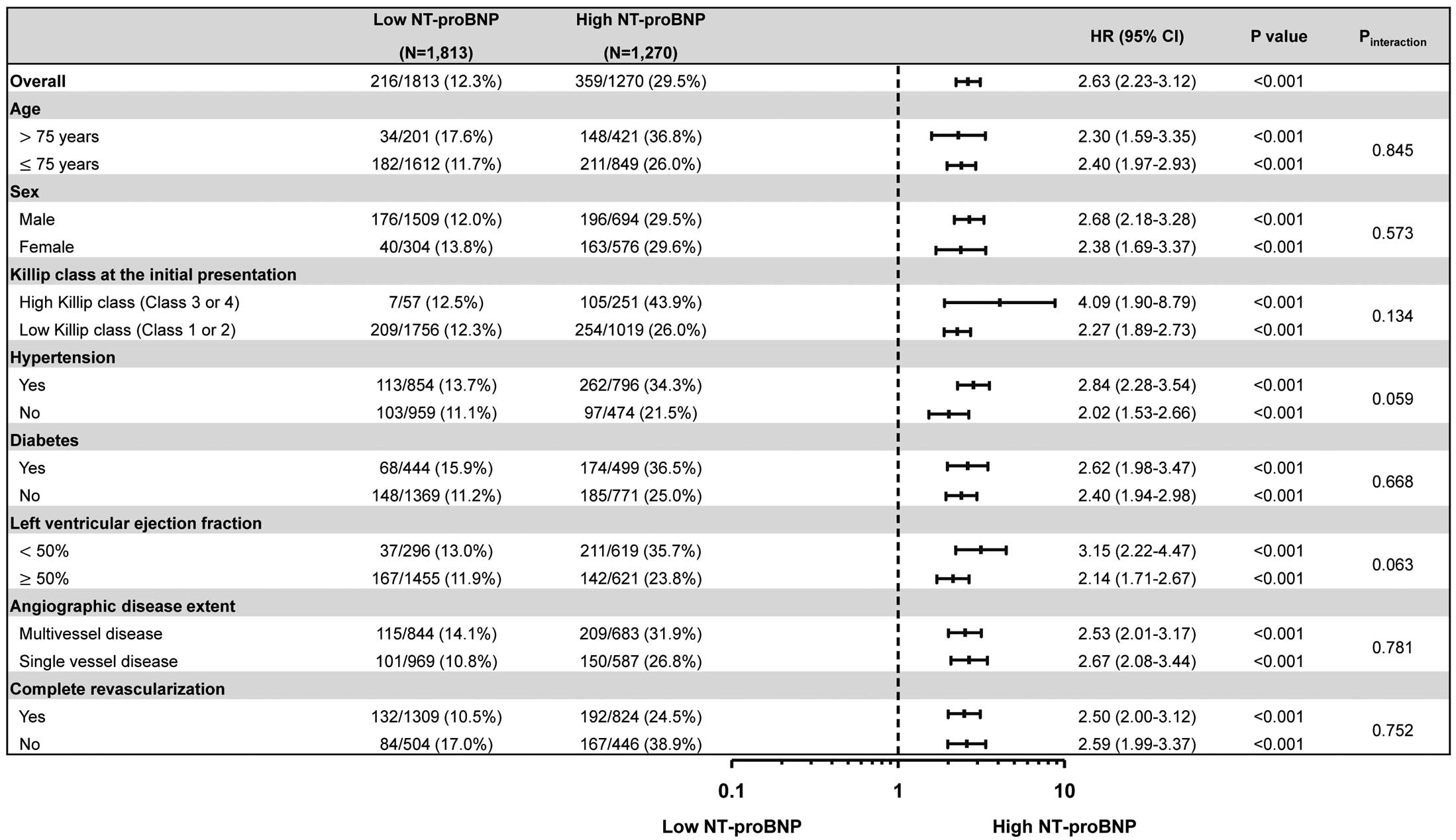
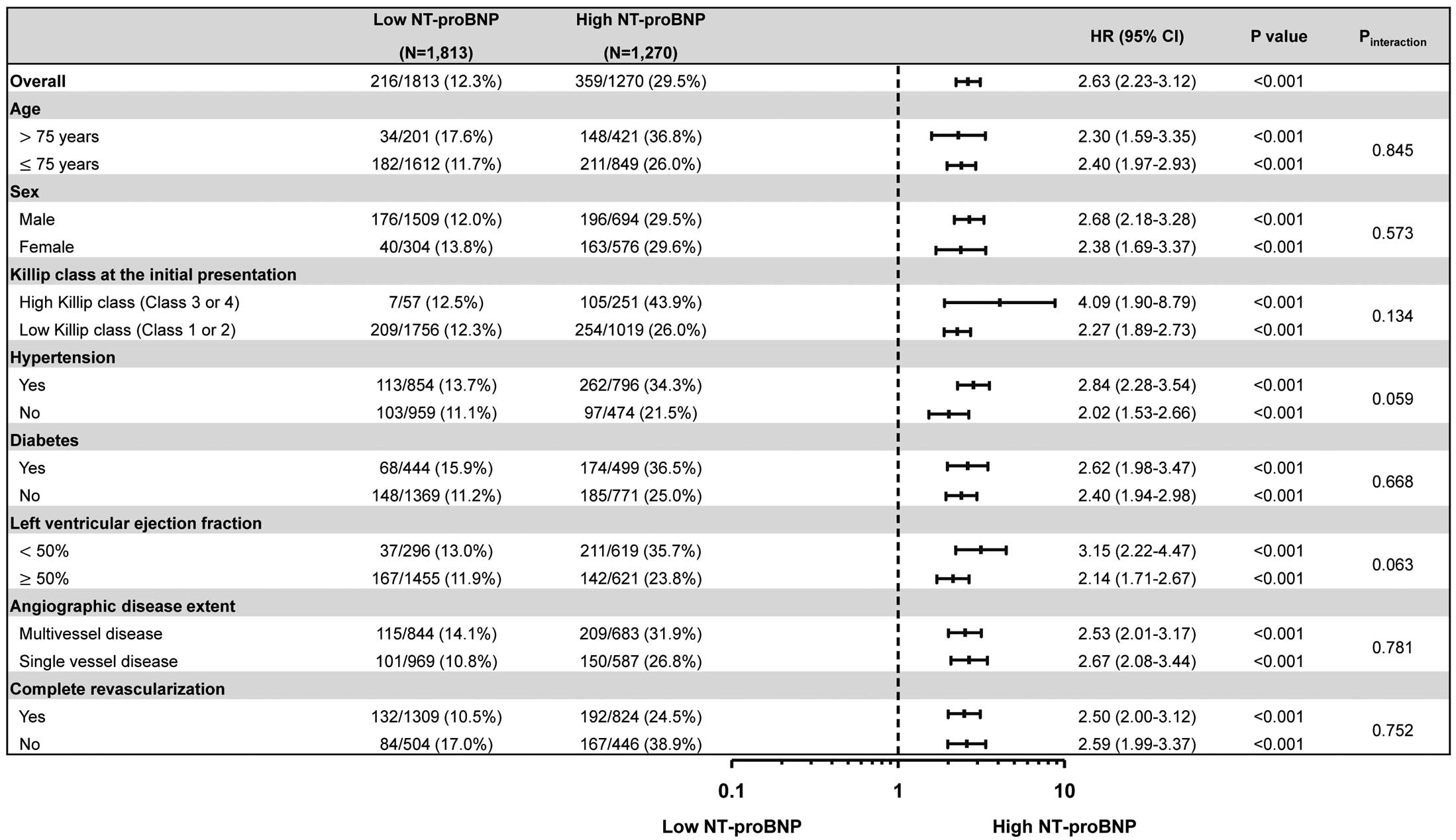
Sensitivity analysis was performed using propensity score matching and IPTW analyses to adjust for differences in baseline characteristics. Both propensity score matching and IPTW analyses constantly showed a significantly higher risk of 3-year MACE in the high NT-proBNP group than in the low NT-proBNP group (Supplementary Table 2). Patients with elevated initial NT-proBNP showed a consistently higher risk of MACE across various subgroups without significant interaction (Figure 3). In addition, the higher risk of MACE in the high NT-proBNP group was consistently observed, regardless of target vessels (Supplementary Figure 4).
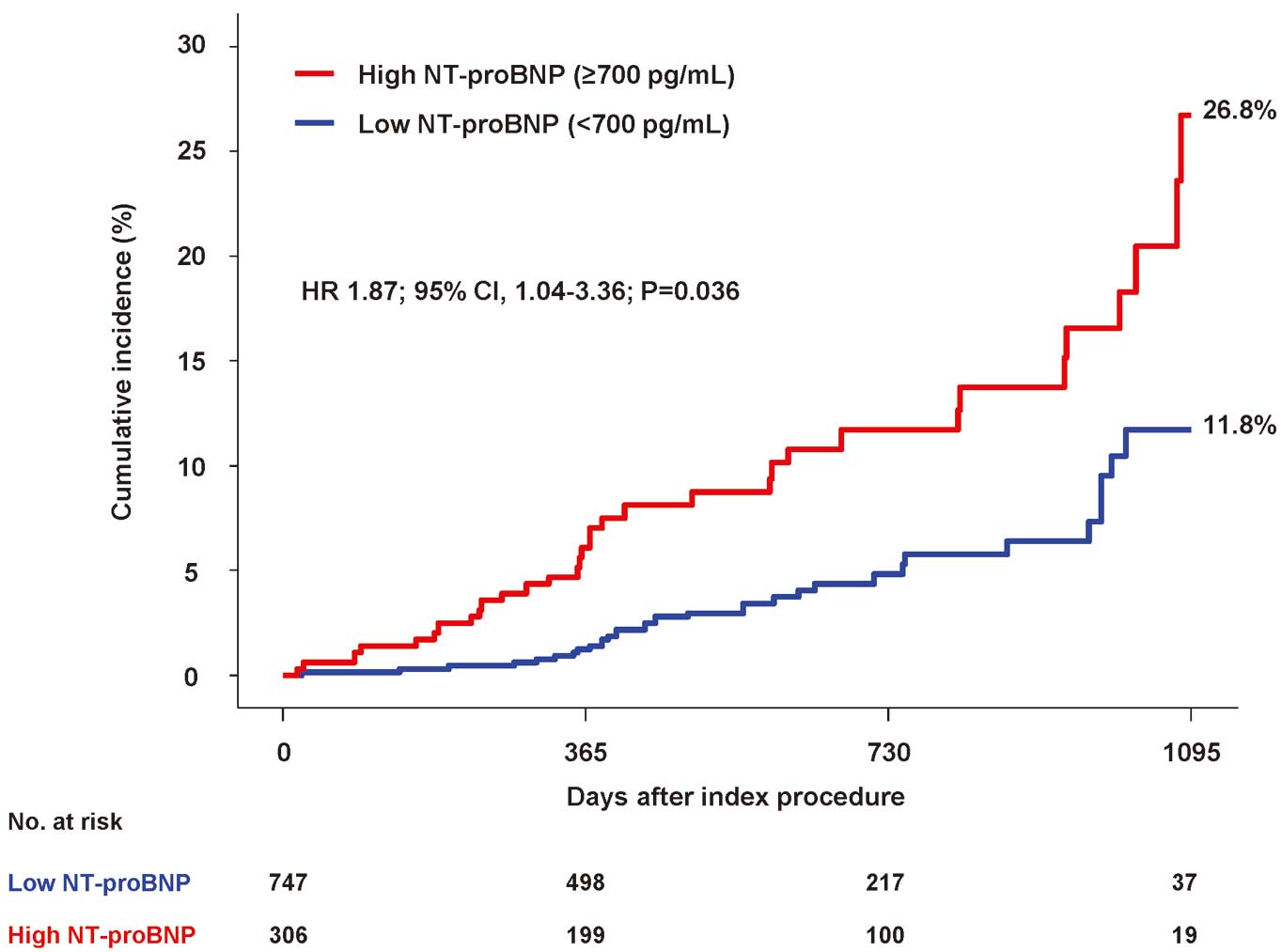
When evaluating follow-up echocardiographic data among 1,053 patients with an LVEF >50% at index echocardiography and for whom both index and follow-up echocardiograms were available, the cumulative incidence of LVEF decline to <50% at 3 years was significantly higher in the high than low NT-proBNP group (26.8% vs. 11.8%; aHR 1.87; 95% CI 1.040–3.365; P=0.036; Figure 4).
Discussion
The present study compared clinical outcomes at 3 years according to the initial NT-proBNP concentration in patients with NSTEMI who underwent PCI. The main findings are as follows. First, approximately 40% of NSTEMI patients had high NT-proBNP concentrations (>700 pg/mL) and this group had a higher prevalence of major cardiovascular risk factors and more extensive coronary artery disease. Second, the high NT-proBNP group had an increased risk of MACE at 3 years compared with the low NT-proBNP group, driven primarily by an increased risk of cardiac death or admission for heart failure. The prognostic implications of NT-proBNP were consistent after propensity score matching and IPTW analysis. In the subgroup analysis, high NT-proBNP was associated with worse clinical outcomes across various subgroups. Third, patients in the high NT-proBNP group had a significantly higher cumulative incidence of LVEF decline to <50% compared with those in the low NT-proBNP group during the 3 years of follow-up.
Recently, with advancements in biomarkers used for the working diagnosis of ACS, such as high-sensitivity cardiac troponin,25 the incidence of NSTEMI has steadily increased, establishing its predominance among all ACS patients.3,4 Although the overall prognosis of NSTEMI patients has improved, there remains a residual risk of mortality even after successful revascularization. Indeed, NSTEMI reports a 1-year mortality rate of approximately 6% and is known to leave sustained sequelae, such as ischemic cardiomyopathy and CHF.3,6 Consequently, there is a growing need for reliable prognostic biomarkers for risk stratification and long-term management in patients with NSTEMI. Several studies have investigated biomarkers associated with the prognosis of NSTEMI patients. Hjort et al conducted a study on various cardiovascular biomarkers using blood samples extracted from patients during the acute phase of STEMI and NSTEMI.9 However, the pathophysiologic pattern of biomarkers in the NSTEMI patient group was heterogeneous, and failed to demonstrate the prognostic value of NT-proBNP for mortality and MACE.9 Zelniker et al reported that C-terminal telopeptide was associated with the prognosis of cardiac death and heart failure in NSTEMI patients; however, C-terminal telopeptide, known as a biomarker of collagen turnover, showed limited cardiac specificity.8 Furthermore, previous studies showed limited prognostic value of CK-MB or galectin-3 in NSTEMI patients.6,10
NT-proBNP has been established as a reliable biomarker for predicting prognosis in various heart diseases, especially CHF.11,12 However, only a few studies have investigated the prognostic value of NT-proBNP in patients with NSTEMI. Schellings et al showed that elevated NT-proBNP was a prognostic factor predicting 30-day mortality among 1,324 NSTEMI patients.18 Similarly, Takahashi et al evaluated 218 NSTEMI patients without elevation of creatine kinase and reported that a higher BNP concentration (>100pg/mL) was associated with an increased risk of adverse clinical events at 3 years.17 However, the results of these previous studies should be interpreted with caution. Although coronary revascularization by PCI or bypass surgery is the dominant treatment in contemporary practice, revascularization was performed in less than two-thirds of the study populations: 54.1% in the study of Takahashi et al17 and 67.0% in the study of Schellings et al.18 As a result, there is limited evidence regarding the long-term prognostic implications of NT-proBNP in patients with NSTEMI who have undergone PCI in large study populations with long-term follow-up. In this regard, the present study assessed the prognostic implications of NT-proBNP among 3,083 NSTEMI patients treated by PCI during index hospitalization and evaluated clinical outcomes during a median follow-up of 2.9 years using data from the large-scale nationwide KAMIR-NIH registry.
In the present study, the risk of MACE at 3 years was significantly higher in the high compared with low NT-proBNP group, driven primarily by an increased risk of cardiac death or admission for heart failure. It should be noted that the high NT-proBNP group had a higher prevalence of cardiovascular comorbidities and more extensive and complex coronary artery disease than the low NT-proBNP group. Regarding procedural results, the total length and number of implanted stents were higher, and the rate of complete revascularization was lower in the high compared with low NT-proBNP group. However, even after adjusting for various clinical factors that showed significant differences between the 2 groups through sensitivity analyses, the risk of MACE at 3 years remained significantly higher in the high NT-proBNP group. Furthermore, the risk of MACE at 3 years increased proportionally with the NT-proBNP concentration, showing the prognostic value of NT-proBNP concentrations for patients with NSTEMI who underwent PCI.
In addition, the high NT-proBNP group had a higher cumulative incidence of LVEF decline to <50% than the low NT-proBNP group. These results suggest that patients with elevated NT-proBNP concentrations would have a higher risk of developing LV systolic dysfunction and the onset of heart failure, even if the LVEF at index hospitalization is within the normal range. Another plausible explanation of the prognostic association between initial NT-proBNP concentrations and long-term clinical outcomes is that some acute MI patients presented with pre-existing elevated LV filling pressure.26 Elevated LV filling pressure indicates underlying structural and functional abnormalities of cardiac diastolic dysfunction before the acute MI event and is associated with clinical outcomes. Considering the limited evidence regarding reliable prognostic biomarkers in NSTEMI patients, the findings of the present study suggest that NT-proBNP may be a reliable prognostic indicator in NSTEMI patients treated with PCI.
Study Limitations
Some study limitations should be addressed. First, the study population was derived from prospective observational data. Although we tried to adjust for confounding variables through various statistical methods, there remains the risk of unintentional bias. Second, the optimal cut-off value of NT-proBNP (>700 pg/mL) for predicting MACE for NSTEMI patients was determined based on ROC analysis of the study population. Therefore, external validation of this cut-off value would be needed. Third, a high NT-proBNP concentration was associated with decreased LV systolic function during follow-up. However, diastolic function could not be assessed according to NT-proBNP concentrations because data pertaining to diastolic function were not collected in the KAMIR-NIH registry. Fourth, guideline-directed medical treatment including up-titration of β-blockers may influence NT-proBNP concentrations, but the current registry data did not systematically collect detailed information regarding medical treatment, especially during the follow-up period.
Conclusions
In patients with NSTEMI who underwent PCI, an elevated initial NT-proBNP concentration was associated with a higher risk of MACE at 3 years, driven primarily by the higher risk of cardiac death and admission for heart failure. The results of the present study suggest that the NT-proBNP concentration at the time of initial presentation may have a clinically significant prognostic value in NSTEMI patients undergoing PCI.
Sources of Funding
This research was supported by funds from the Research of Korea Centers for Disease Control and Prevention (2016-ER6304-01).
Disclosures
J.M.L. has received institutional research grants from Abbott Vascular, Boston Scientific, Philips Volcano, Terumo Corporation, MicroPort, Zoll Medical, Donga-ST, and Yuhan Pharmaceutical. J.-Y. Hahn has received institutional research grants from National Evidence-based Healthcare Collaborating Agency, Ministry of Health and Welfare, Korea, Abbott Vascular, Biosensors, Boston Scientific, Daiichi Sankyo, Donga-ST, Hanmi Pharmaceutical, and Medtronic Inc. H.-C.G. has received institutional research grants from Boston Scientific, Genoss, and Medtronic Inc. H.-S.K. is a member of Circulation Journal’s Editorial Team (International Associate Editor). All other authors have no competing interests to declare.
IRB Information
This study was approved by the Institutional Review Board of the Samsung Medical Center (Approval no. 2011-10-080).
Data Availability
The deidentified participant data will not be shared.
Supplementary Files
Please find supplementary file(s);
https://doi.org/10.1253/circj.CJ-24-0129
References
- 1.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2019; 40: 237–269.
- 2.
Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J 2023; 44: 3720–3826.
- 3.
Kim RB, Kim JR, Hwang JY. Epidemiology of myocardial infarction in Korea: Hospitalization incidence, prevalence, and mortality. Epidemiol Health 2022; 44: e2022057.
- 4.
Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet 2017; 389: 197–210.
- 5.
Tjora HL, Steiro OT, Langørgen J, Bjørneklett R, Nygård OK, Skadberg Ø, et al. Cardiac troponin assays with improved analytical quality: A trade-off between enhanced diagnostic performance and reduced long-term prognostic value. J Am Heart Assoc 2020; 9: e017465.
- 6.
Ishihara M, Nakao K, Ozaki Y, Kimura K, Ako J, Noguchi T, et al. Long-term outcomes of non-ST-elevation myocardial infarction without creatine kinase elevation: The J-MINUET study. Circ J 2017; 81: 958–965.
- 7.
Lim KD, Yan AT, Casanova A, Yan RT, Mendelsohn A, Jolly S, et al. Quantitative troponin elevation does not provide incremental prognostic value beyond comprehensive risk stratification in patients with non-ST-segment elevation acute coronary syndromes. Am Heart J 2008; 155: 718–724.
- 8.
Zelniker TA, Jarolim P, Scirica BM, Braunwald E, Park JG, Das S, et al. Biomarker of collagen turnover (C-terminal telopeptide) and prognosis in patients with non-ST-elevation acute coronary syndromes. J Am Heart Assoc 2019; 8: e011444.
- 9.
Hjort M, Eggers KM, Lindhagen L, Baron T, Erlinge D, Jernberg T, et al. Differences in biomarker concentrations and predictions of long-term outcome in patients with ST-elevation and non-ST-elevation myocardial infarction. Clin Biochem 2021; 98: 17–23.
- 10.
Mitić B, Jovanović A, Nikolić VN, Stokanović D, Andrejić OM, Vučić RM, et al. Trend of galectin-3 levels in patients with non-ST-elevation and ST-elevation myocardial infarction. Medicina (Kaunas) 2022; 58: 286, doi:10.3390/medicina58020286.
- 11.
de Lemos JA, McGuire DK, Drazner MH. B-type natriuretic peptide in cardiovascular disease. Lancet 2003; 362: 316–322.
- 12.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022; 145: e895–e1032.
- 13.
Hutt E, Mentias A, Alashi A, Wadhwa R, Fava A, Lever HM, et al. Prognostic value of age-sex adjusted NT-proBNP ratio in obstructive hypertrophic cardiomyopathy. Prog Cardiovasc Dis 2022; 74: 11–18.
- 14.
Bergler-Klein J. NT-proBNP as a cornerstone for prognosis in valve disease: All we need is blood. J Am Coll Cardiol 2020; 75: 1673–1675.
- 15.
Stämpfli SF, Erhart L, Hagenbuch N, Stähli BE, Gruner C, Greutmann M, et al. Prognostic power of NT-proBNP in left ventricular non-compaction cardiomyopathy. Int J Cardiol 2017; 236: 321–327.
- 16.
Gan CT, McCann GP, Marcus JT, van Wolferen SA, Twisk JW, Boonstra A, et al. NT-proBNP reflects right ventricular structure and function in pulmonary hypertension. Eur Respir J 2006; 28: 1190–1194.
- 17.
Takahashi N, Ogita M, Suwa S, Nakao K, Ozaki Y, Kimura K, et al. Prognostic impact of B-type natriuretic peptide on long-term clinical outcomes in patients with non-ST-segment elevation acute myocardial infarction without creatine kinase elevation. Int Heart J 2020; 61: 888–895.
- 18.
Schellings DA, Adiyaman A, Dambrink JE, Gosselink AM, Kedhi E, Roolvink V, et al. Predictive value of NT-proBNP for 30-day mortality in patients with non-ST-elevation acute coronary syndromes: A comparison with the GRACE and TIMI risk scores. Vasc Health Risk Manag 2016; 12: 471–476.
- 19.
Kim JH, Chae SC, Oh DJ, Kim HS, Kim YJ, Ahn Y, et al. Multicenter cohort study of acute myocardial infarction in Korea: Interim analysis of the Korea Acute Myocardial Infarction Registry-National Institutes of Health registry. Circ J 2016; 80: 1427–1436.
- 20.
Lee JM, Rhee TM, Hahn JY, Kim HK, Park J, Hwang D, et al. Multivessel percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction with cardiogenic shock. J Am Coll Cardiol 2018; 71: 844–856.
- 21.
Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022; 145: e18–e114.
- 22.
Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J 2023; 44: 3720–3826.
- 23.
Garcia-Garcia HM, McFadden EP, Farb A, Mehran R, Stone GW, Spertus J, et al. Standardized end point definitions for coronary intervention trials: The Academic Research Consortium-2 consensus document. Eur Heart J 2018; 39: 2192–2207.
- 24.
Ryan TJ, Bauman WB, Kennedy JW, Kereiakes DJ, King SB 3rd, McCallister BD, et al. Guidelines for percutaneous transluminal coronary angioplasty. A report of the American Heart Association/American College of Cardiology Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Committee on Percutaneous Transluminal Coronary Angioplasty). Circulation 1993; 88: 2987–3007.
- 25.
Vasile VC, Jaffe AS. High-sensitivity cardiac troponin for the diagnosis of patients with acute coronary syndromes. Curr Cardiol Rep 2017; 19: 92.
- 26.
Lee SH, Choi KH, Yang JH, Song YB, Lee JM, Park TK, et al. Association between preexisting elevated left ventricular filling pressure and clinical outcomes of future acute myocardial infarction. Circ J 2022; 86: 660–667.