Article ID: CJ-24-0159
Article ID: CJ-24-0159
Heart failure (HF) is categorized into stages A–D based on structural changes and symptomatic manifestations,1 and this classification not only provides information on the progression of the disease but also can help elucidate the characteristics of individuals and populations. Stages A and B include patients without clinical symptoms; thus both are denoted as preclinical HF. The 2022 American Heart Association (AHA)/American College of Cardiology (ACC)/Heart Failure Society of America (HFSA) Guideline for the management of HF2 emphasizes the significance of primary prevention for individuals at risk of HF (Stage A) or with pre-HF (Stage B).
Article p ????
Identifying left ventricular (LV) abnormalities is imperative in patients with preclinical HF, and global longitudinal strain (GLS) is a sensitive marker of subtle LV functional abnormalities. Current guidelines stipulate that a GLS <16% should be construed as an LV structural abnormality.2–4 Indeed, the 2022 AHA/ACC/HFSA Guideline for the management of HF2 recommends thresholds, including GLS <16%, for diagnosing stage B with evidence of structural heart disease and heightened filling pressures. The use of GLS in patients with preclinical HF could facilitate early detection of subclinical LV dysfunction, thereby aiding the prevention of progression to clinical HF. However, not all echocardiographic instruments can measure GLS, and there is a paucity of studies examining whether medical history and echocardiographic parameters can predict a GLS <16%.
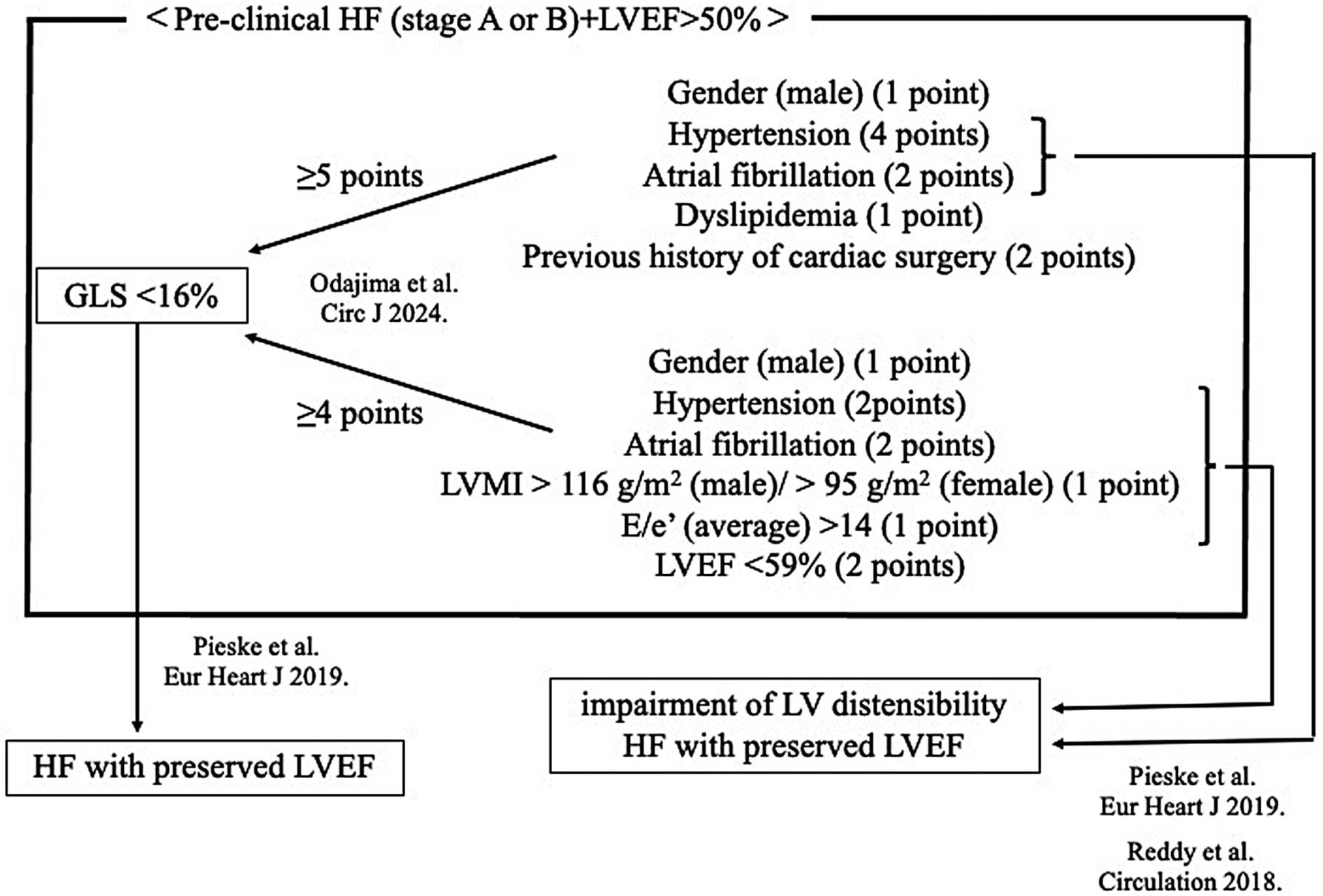
In this issue of the Journal, Odajima et al5 report the development of a scoring system for evaluating LV longitudinal myocardial dysfunction, which may prove beneficial for the risk stratification of patients with preclinical HF. They examined 853 patients with preclinical HF to devise a scoring system for predicting low GLS (<16%). Using Cox proportional hazards analysis, they assessed the associations of medical history and echocardiographic parameters with GLS <16% and constructed 2 models. In model 1 (based on medical history), a score ≥5 points predicted GLS <16% with 90.2% sensitivity and 62.9% specificity (male=1 point, hypertension=4 points, dyslipidemia=1 point, atrial fibrillation=2 points, and history of cardiac surgery=2 points). In model 2 (incorporating medical history and echocardiographic parameters), a score ≥4 points predicted GLS <16% with 80.3% sensitivity and 76.5% specificity (male=1 point, hypertension=2 points, atrial fibrillation=2 points, LV mass index [LVMI] >116 g/m2 (male) or >96 g/m2 (female)=1 point, LV ejection fraction [LVEF] <59%=2 points, and E/e′ >14=1 point).
Hypertension emerged as the most significant risk factor for HF development in model 1, with long-term elevated blood pressure potentially contributing to LV myocardial damage. Thus, hypertension serves as a crucial surrogate marker for predicting GLS <16%, and its management may constitute a component of comprehensive HF care. In model 2, the inclusion of conventional echocardiographic parameters, including LVMI, LVEF, and E/e′, together with medical history augmented the accuracy of the GLS <16% prediction.
GLS is a more precise and sensitive parameter than conventional cardiac functional indices across all HF stages, with an abnormal GLS correlating with the occurrence of cardiovascular events.6–9 Although GLS <16% is undeniably a pivotal indicator, predicting GLS <16% solely based on LV appearance on transthoracic echocardiography is challenging without confirming the actual measured values of GLS. Nevertheless, this study sheds light on the elusive condition of GLS <16% by elucidating the predictive factors and reaffirms the significance of these predictors (hypertension, atrial fibrillation, high LVMI, low LVEF, and E/e′ >14) in indicating GLS <16%. Therefore, continued attention to factors such as hypertension, atrial fibrillation, high LVMI, low LVEF, and E/e′ >14 leads to the recognition of GLS <16%. However, confirming the singular importance of GLS <16% in individuals with LVEF >50% and preclinical HF (Stage A or B) remains a future task.
Furthermore, understanding the significance of GLS <16% in individuals with LVEF >50% and preclinical HF (Stage A or B) is essential. Initially, GLS mirrors LV contractility; nevertheless, hypertension, atrial fibrillation, high LVMI, and E/e′ >14, linked with LV distensibility, emerged as factors indicative of GLS <16% in this study (Figure).3,10 Thus, GLS <16% reflects not only LV contractility but also LV distensibility, in line with previous reports,3 and can serve as a pivotal indicator, reflecting both LV contractility and distensibility in individuals with LVEF >50% and preclinical HF (Stage A or B), as reaffirmed by the findings of the study of Odajima et al.