Article ID: CJ-24-0187
Article ID: CJ-24-0187
Heart failure (HF) is considered as both a pressing global health concern and a pandemic, with its prevalence expected to rise significantly in the coming decades due to the aging of populations.1 A universal definition and classification of HF has proposed stages of HF as: at risk for HF (stage A), pre-HF (stage B), symptomatic HF (stage C), and advanced HF (stage D).2 These stages of HF are associated with progressively worsening 5-year survival rates: stage A 97.0%, stage B 95.7%, stage C 74.6%, and stage D 20.0%. Therefore, it is important to accurately diagnose asymptomatic early-stage HF (stages A and B) and prevent progression to symptomatic stage C through early treatment. However, diagnosing asymptomatic early-stage HF is challenging for general practitioners in primary care settings.
Article p ????
In this issue of the Journal, Fujimoto and colleagues3 shed light on the critical role of B-type natriuretic peptide (BNP) in the early detection of preclinical HF (early-stage HF), particularly in primary care settings. They demonstrate that increasing BNP concentrations are significantly associated with the prevalence of preclinical HF in Japan, an association that remained robust even after adjusting for various clinical parameters. As the BNP concentration increased, left atrial volume index (LAVI), left ventricle mass index (LVMI), and the early diastolic velocity/early diastolic velocity (E/e′) ratio increased, while the left ventricular ejection fraction (LVEF) and global longitudinal strain (GLS) decreased on echocardiography. These findings highlight the importance of proactive screening measurement of BNP.
The notable strength of this study is that echocardiographic data are available for all the patients with BNP measurement. There is little data on echocardiography in patients with suspected HF and BNP <35 pg/mL because HF guidelines in Europe and the USA recommend that echocardiography should be performed only in patients with BNP ≥35 pg/mL.4,5 A universal definition of preclinical HF is yet to be established, so in their study Fujimoto et al applied their novel structural heart disease (SHD) criteria (LAVI ≥34 mL/m2 in sinus rhythm or ≥40 mL/m2 in atrial fibrillation (AF); LVMI ≥149 g/m2 in men or ≥122 g/m2 in women; LVEF <50%; GLS <16%; E/e′ ≥15) or evidence of significant valvular heart disease. Results demonstrated that the prevalence of preclinical HF diagnosed with these new criteria consistently increases as BNP concentration increases. However, the authors indicate that the appropriateness of their definition of SHD requires further validation in other studies.
These considerations and the study’s results tell us that BNP assessment is an easy-to-use method for predicting preclinical HF in primary care settings, but with several issues that need to be resolved. First, in which patients should we measure BNP to diagnose preclinical HF accurately and efficiently among asymptomatic patients? Preclinical HF is defined as patients with SHD, but without current or previous symptoms/signs of HF.4,5 Although clinicians need to suspect preclinical HF before measuring BNP, it is challenging to suspect HF in asymptomatic patients. BNP could be measured in all patients with stage A HF, but it is too costly (Figure). Therefore, it is desirable to identify the specific patient population to undergo BNP measurement. A previous study proposed a new risk score (BASE-CH score) to predict NT-proBNP ≥125 pg/mL in preclinical HF patients, based on routinely available clinical and laboratory variables,6 and this could prompt clinicians to suspect HF in asymptomatic patients. Second, which patients with preclinical HF and elevated BNP will develop stage C HF is to be determined. BNP concentration is influenced by both cardiac and non-cardiac factors such as inflammation, infection, age, and anemia, which might reduce diagnostic accuracy.5 The absolute risks of progression to HF were 8.4 per 100 person-years in a previous study.7 Therefore, we need to develop a risk score that identifies asymptomatic patients likely to progress to stage C HF, using clinical and laboratory variables that clinicians can use routinely. Finally, how should we treat patients with preclinical HF? A meta-analysis showed that intensive blood pressure control was associated with 36% reduction in HF events.8 Several randomized controlled trials (RCTs) have shown that SGLT2 inhibitors prevent HF hospitalizations in patients with type 2 diabetes and at risk for, or with established cardiovascular disease (CVD) or at high risk for CVD, or chronic kidney disease.9–11 In addition, multiple RCTs of patients with a recent myocardial infarction and LVEF ≤40% have shown that angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, β-blockers, and statins prevent symptomatic HF and reduce mortality rates.12–15 However, there is no established treatment that is common to the various underlying diseases or LVEF to prevent the progression of preclinical HF patients to symptomatic stage C HF. Therefore, further investigations to clarify interventions targeting prevention of the progression to stage C HF from preclinical HF are needed.
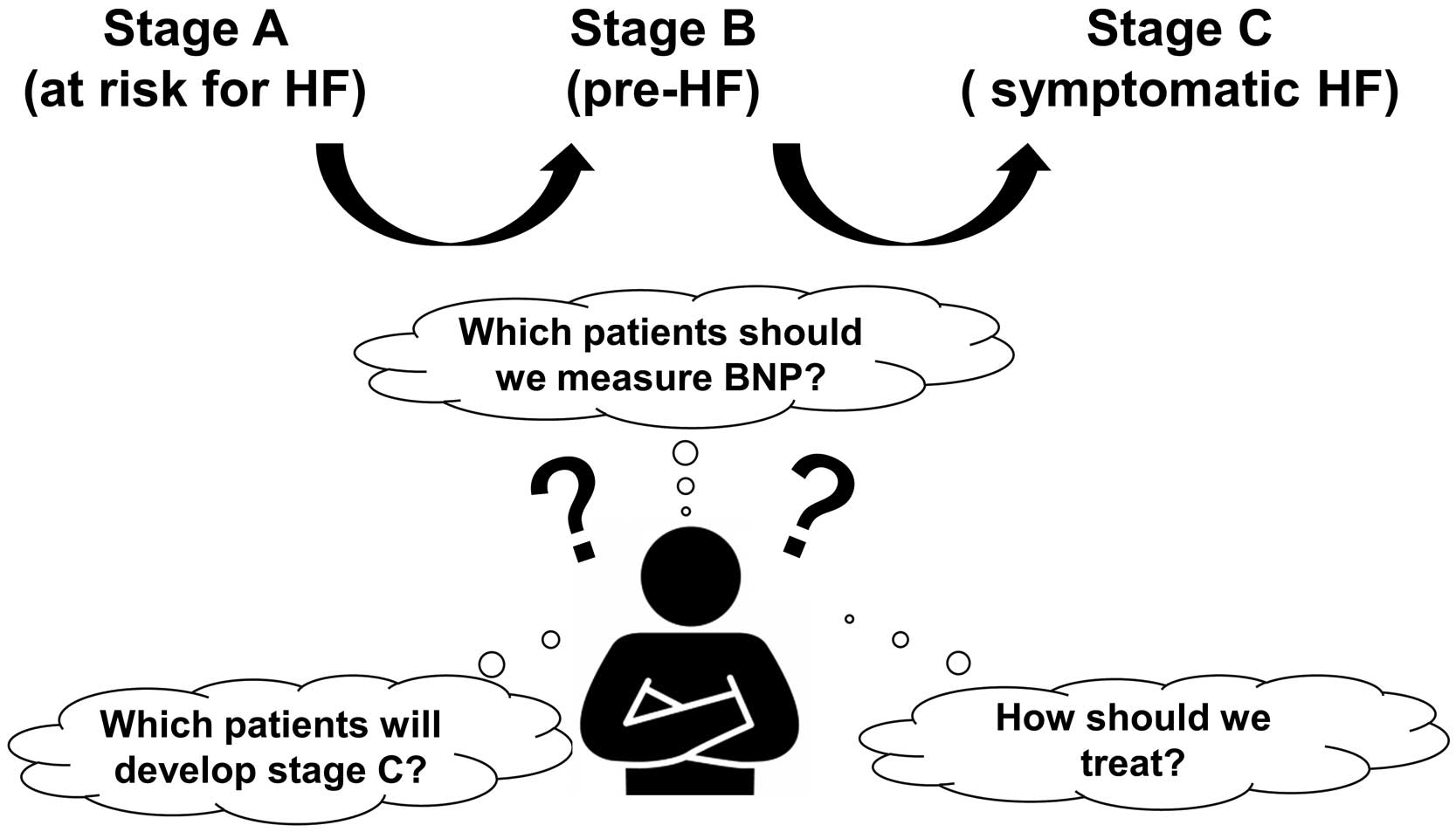
Heart failure (HF) stages and what we should consider. BNP, B-type natriuretic peptide.
In conclusion, the present study underscores the value of proactive screening using BNP in primary care settings to address the impending HF pandemic. It can assist clinicians in the early detection of preclinical HF, the “invisible enemy”.
The authors have no conflicts of interest relevant to the content of this article.