Abstract
Background: Comprehensive management of acute coronary syndrome (ACS) requires seamless treatment across institutions, including intensive care centers and local clinics. However, maintaining guideline-directed medical therapy remains challenging. One promising option to improve the situation may be the implementation of regional collaborative clinical pathways. This study evaluated the prevalence and functionality of such pathways for ACS in Japan.
Methods and Results: A nationwide survey was conducted through questionnaires and web searches, targeting all 47 prefectural managers of Japanese Circulation Association (JCA) branches. The study focused on pathways managed at the prefectural or regional levels, excluding inactive or institutional pathways. In all, 18 pathways were identified: 11 (23%) prefecture wide and 4 (9%) region wide. Most pathways included risk factor targets such as low-density lipoprotein cholesterol (LDL-C), HbA1c, and blood pressure, but only 8 pathways set an LDL-C target of <70 mg/dL. Pathways updated between 2022 and 2024 and incorporating LDL-C management protocols were considered functional. In all, 45 JCA branches viewed future ACS pathways established by the government or academic societies as potentially useful resources.
Conclusions: Regional collaborative clinical pathways for ACS patients in Japan show variable implementation across prefectures, with approximately one-third of prefectures having established pathways. Future efforts should prioritize the establishment of comprehensive, sustainable, and standardized pathways to optimize ACS management and improve patient outcomes nationwide.
Comprehensive treatment through seamless medical collaboration is required for the treatment of acute coronary syndrome (ACS) because of high mortality and recurrence rates, including rapid emergency transportation, intensive care at core centers, and optimal secondary prevention at local hospitals and clinics.1 One of remaining issues regarding the prognosis of ACS is the incidence of non-culprit lesion-related cardiovascular events. Although the incidence of culprit lesion-related events has decreased owing to advances in percutaneous coronary intervention, including the improved performance of drug-eluting stents, the incidence of non-culprit lesion-related cardiovascular events remains high, reportedly approximately twice that of culprit lesion-related events.2 Because most non-culprit lesion-related cardiovascular events are thought to result from the rupture of unstable plaques located through coronary trees, it is necessary to consider rapid plaque stabilization by intensive pharmacotherapy in addition to the consideration of immediate revascularization.3 The central component of pharmacotherapy in patients with ACS is intensive lipid-lowering therapy, including maximum tolerated statin dose, ezetimibe, and proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors.4–6 Current guidelines in Japan recommend target low-density lipoprotein cholesterol (LDL-C) levels <70 mg/dL in patients with ACS, achieved with intensive lipid-lowering therapy and lifestyle modifications.7 However, the achievement rate of this target is reported only approximately 30% in daily clinical practice in Japan, suggesting that inadequate lipid management may be a contributing factor to non-culprit lesion-related cardiovascular events.8
Using clinical pathways is thought to be a promising measure to improve adherence to guideline-oriented medical therapy, including improving the achievement rate of target LDL-C levels in patients with ACS.9 The implementation of clinical pathways and discharge checklists designed for in-hospital use is relatively easy to establish and has been reported to contribute to stricter short-term lipid management.10 Conversely, to optimize longer-term secondary prevention, it is considered ideal to introduce unified clinical pathways within a certain geographic region, including cardiovascular experts in core medical centers and general physicians in local hospitals and clinics.11 However, the current state of implementation and practical use of regional collaborative clinical pathways for patients with ACS in Japan is unclear. Thus, the aim of the present study was to clarify the current status of collaborative clinical pathways for ACS using a nation-wide survey.
Methods
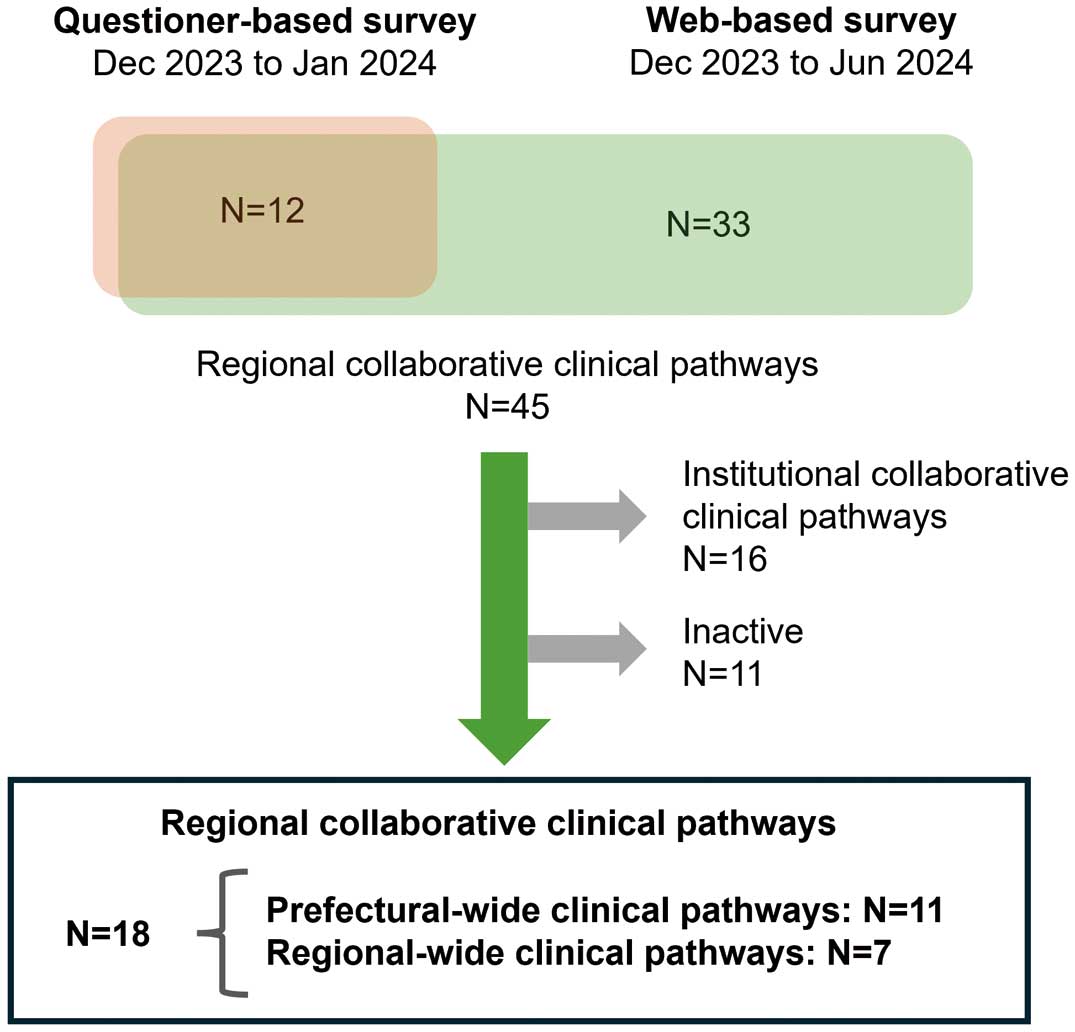
This study is based on 2 types of surveys, a questionnaire survey and a web-based survey (Figure 1).
Questionnaire Survey
A survey was conducted from December 2023 to January 2024 by sending a questionnaire to the prefectural managers of all Japanese Circulation Association (JCA) branches. The purpose of this survey was to clarify the current status and prospects of regional collaborative clinical pathways for patients with ACS in each geographic region. All questions in this questionnaire survey are listed in the Supplementary Table. Responses to the questionnaire were obtained from all 47 prefectural branches. The present study included some of those questions and analyzed their responses to identify pathways, evaluate the functional status of pathways in daily practice, and clarify physicians’ expectations for future ideal pathways. The method for evaluating whether the clinical pathways were functional was left to the discretion of each JCA branch. Based on this survey, 12 clinical pathways for patients with ACS were identified.
Web-Based Survey
The purpose of the web-based survey was to complement the questionnaire survey and identify any regional collaborative clinical pathways for patients with ACS in each geographic region, as well as to thoroughly investigate the structures and items in each pathway. The web-based survey was conducted from December 2023 to June 2024 by searching the websites of the clinical pathways using several terms, including the name of the prefecture, “ACS,” “myocardial infarction,” “clinical pathway,” and “regional collaboration,” to access the digital form of the pathway. The survey was conducted using Google (https://www.google.co.jp/) and Yahoo Japan (http://search.yahoo.co.jp). Based on this survey, 33 additional clinical pathways for patients with ACS were identified.
Definition of Regional Collaborative Clinical Pathways for Patients With ACS
Based on the questionnaire and web-based surveys, 45 regional collaborative clinical pathways were identified. Of these, 18 pathways (11 prefecture-wide pathways and 7 region-wide pathways) included in the present analysis after the exclusion of 16 institutional collaborative pathways and 11 inactive pathways (Figure 1).
A prefecture-wide pathway was defined as a unified clinical pathway designed to be used in multiple core centers and clinics through the prefecture (Table 1). A region-wide pathway was defined as a unified clinical pathway used in multiple core centers and clinics within a specific medical region within the prefecture or implemented in a specific region although its use was not limited within the region. An institutional collaborative pathway was defined as a clinical pathway established by a specific institute to be used by that institute in collaboration with clinics. Although we acknowledge the importance of institutional clinical pathways, because they may be synonymous with regional collaborative clinical pathways in certain areas, it was not feasible to comprehensively screen all existing pathways to clarify their actual prevalence and functional status within the framework of this project. Therefore, we decided to exclude institutional clinical pathways from the present study and focus exclusively on regional collaborative clinical pathways. A pathway was judged as inactive and excluded from the study due to inaccessibility issues, including “outdated links” and “not found,” despite the existence of the link to the pathway or the website. The exclusive targeting of patients with ACS was not a requirement for inclusion in the present analysis. This means that some of pathways included in this study focus on the wider population, including patients with other heart diseases in addition to ACS.
Table 1.
Definitions of Collaborative Clinical Pathways
| Term |
Definition |
| Type |
| Institutional |
Established by a core center to be used in collaborations between the center and local clinics |
| Prefecture wide |
Designed to be used in multiple core centers and clinics throughout the entire prefecture |
| Region wide |
Designed to be used in multiple core centers and clinics within a specific region, or implemented in a specific region
although its use is not limited within the region |
| Structure |
| Circulating |
Designed to share medical conditions and treatment plans between a GP and a core center with the intention of
regularly rotating between them
Circulating pathways describe the specific timing and conditions for referring a patient back to a core center |
| Unidirectional |
Designed to smoothly transfer medical conditions and treatment plans from a core center to the GP and other
medical staff after intensive treatment at a core center |
| Communication tools |
| Status sheet |
Intended to share medical conditions and treatment plans among a GP, a core center, and other medical staff |
| Handy notebook |
Designed mainly for patients to understand treatment plans, record their medical conditions themselves, and learn
about their own disease
Some handy notebooks are designed with the same intent as a communication sheet |
| Protocol sheet |
Designed to share specific treatment strategies (e.g., LDL-C-lowering therapy) to achieve guideline-recommended
treatment goals |
GP, general physician at a local clinic; LDL-C, low-density lipoprotein cholesterol.
The year of the most recent update, the basic type of pathway, its structure (circulating or unidirectional), and the communication tools were investigated for all pathways using the website for each pathway and its digital form. The organizations that established and managed the pathways were also investigated. The definitions of pathway structure (i.e., circulating or unidirectional) and communication tools (status sheet, handy notebook, and protocol sheet) are provided in Table 1.
Items in Pathways
The items described and mentioned in each pathway were investigated using the website for each pathway and its digital form. Items included target levels for risk factors, medications, and routine examinations through clinical follow-up.
Statistical Analysis
Continuous variables were analyzed using t-tests. Categorical variables are reported as counts and percentages, and were compared using the Chi-squared test. Statistical analyses were performed using SPSS version 24.0 (IBM, Armonk, NY, USA).
Results
Prevalence of Regional Collaborative Pathways for ACS Patients in Japan
Eighteen pathways for ACS management were identified. Of the 47 prefectures in Japan, 11 (23%) have prefecture-wide pathways and 4 (9%) have region-wide pathways (Figure 2). Details of all pathways identified are presented in Table 2.

Table 2.
Regional Collaborative Clinical Pathways for Patients With Acute Coronary Syndrome in Japan
| Area |
UpdateA |
Initiative |
Target |
Pathway
structure |
Communication
tools |
| Prefecture-wide pathways |
| Tochigi |
2013 |
Prefectural medical association |
AMI |
Circulating |
Handy notebook |
| Gunma |
2023 |
Regional healthcare council |
ACS, CCS |
Circulating |
Status sheet, protocol sheet |
| Chiba |
2010 |
Prefectural government |
AMI |
Circulating |
Status sheet |
| Fukui |
2022 |
Regional healthcare council |
AMI, AP, HF |
Circulating |
Status sheet, protocol sheet |
| Nara |
2011 |
Prefectural government |
AMI, AP |
Circulating |
Handy notebook, status sheet |
| Okayama |
2023 |
Prefectural government |
AMI |
Circulating |
Handy notebook, status sheet,
protocol sheet |
| Hiroshima |
2016 |
Regional healthcare council |
MI, HF |
Circulating |
Handy notebook |
| Tokushima |
2024 |
Regional healthcare council |
AMI |
Circulating |
Status sheet |
| Kagawa |
2023 |
Prefectural government |
AMI |
Circulating |
Handy notebook, status sheet,
protocol sheet |
| Nagasaki |
2022 |
Regional healthcare council |
AMI |
Unidirectional |
Status sheet, protocol sheet |
| Kagoshima |
2022 |
University hospital |
ACS |
Circulating |
Protocol sheet |
| Region-wide pathways |
| Tsuruoka (Yamagata) |
2013 |
Regional healthcare council |
AMI |
Circulating |
Handy notebook, status sheet |
| Okitama (Yamagata) |
2017 |
PCI center |
AMI, AP |
Circulating |
Status sheet |
| Niikawa (Toyama) |
2016 |
Regional healthcare council |
AMI |
Circulating |
Status sheet |
| Toyono (Osaka) |
2010 |
PCI center, regional medical association |
AMI |
Circulating |
Handy notebook |
| Tobu (Tottori) |
2014 |
Regional medical association |
MI |
Circulating |
Status sheet |
| Chubu (Tottori) |
2013 |
Regional medical association |
AMI |
Circulating |
Status sheet |
| Seibu (Tottori) |
2020 |
Regional medical association |
ACS |
Circulating |
Status sheet |
AThe year the most recent version was released. ACS, acute coronary syndrome; AMI, acute myocardial infarction; AP, angina pectoris; CCS, chronic coronary syndrome; HF, heart failure; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Prefecture-Wide Pathways
Ten of 11 prefecture-wide pathways were established and managed by prefecture-wide organizations, including the prefectural government, prefectural medical association, or the council of regional healthcare. Three pathways have not been updated in 10 years and all except 1 pathway are circulating pathways (Table 2). Six recently developed pathways include a protocol sheet describing how to titrate lipid-lowering drugs to achieve target LDL-C levels (Table 2).
Region-Wide Pathways
Four of 7 pathways were established and are managed by regional medical associations (Table 2). Four pathways have not been updated in 10 years, and 5 of the 7 region-wide pathways comprise a sole status sheet (Table 2).
Items Included in Regional Collaborative Pathways
Items described by the pathways are shown in Figure 3. Seventeen of 18 pathways describe risk factor target levels, including LDL-C (n=16), HbA1c (n=16), and blood pressure (n=14). Of the 16 pathways describing LDL-C targets, only 8 include the currently recommended LDL-C level (<70 mg/dL). Seventeen of 18 pathways mention medications, including statins (n=14) and PCSK9 inhibitors (n=8). Coronary angiograms are described by 10 pathways as routine follow-up examinations, whereas a limited number of pathways mention coronary computed tomography angiography or scintigraphy as follow-up examinations (Figure 3).
Functional Status of Regional Collaborative Pathways
Based on responses to the questionnaire survey about the functional status of the pathways obtained from 12 prefectural JCA branches with any type of regional collaborative clinical pathway, 5 pathways were judged as functional (i.e., they had been updated between 2022 and 2024 and incorporated LDL-C management protocols) and 5 pathways were judged as non-functional. All functional pathways were prefecture-wide pathways (Figure 4) and had been updated between 2022 and 2024. Compared with non-functional pathways, the functional pathways tended to have a protocol sheet and specified target LDL-C <70 mg/dL.
Expectations for Future ACS Pathways
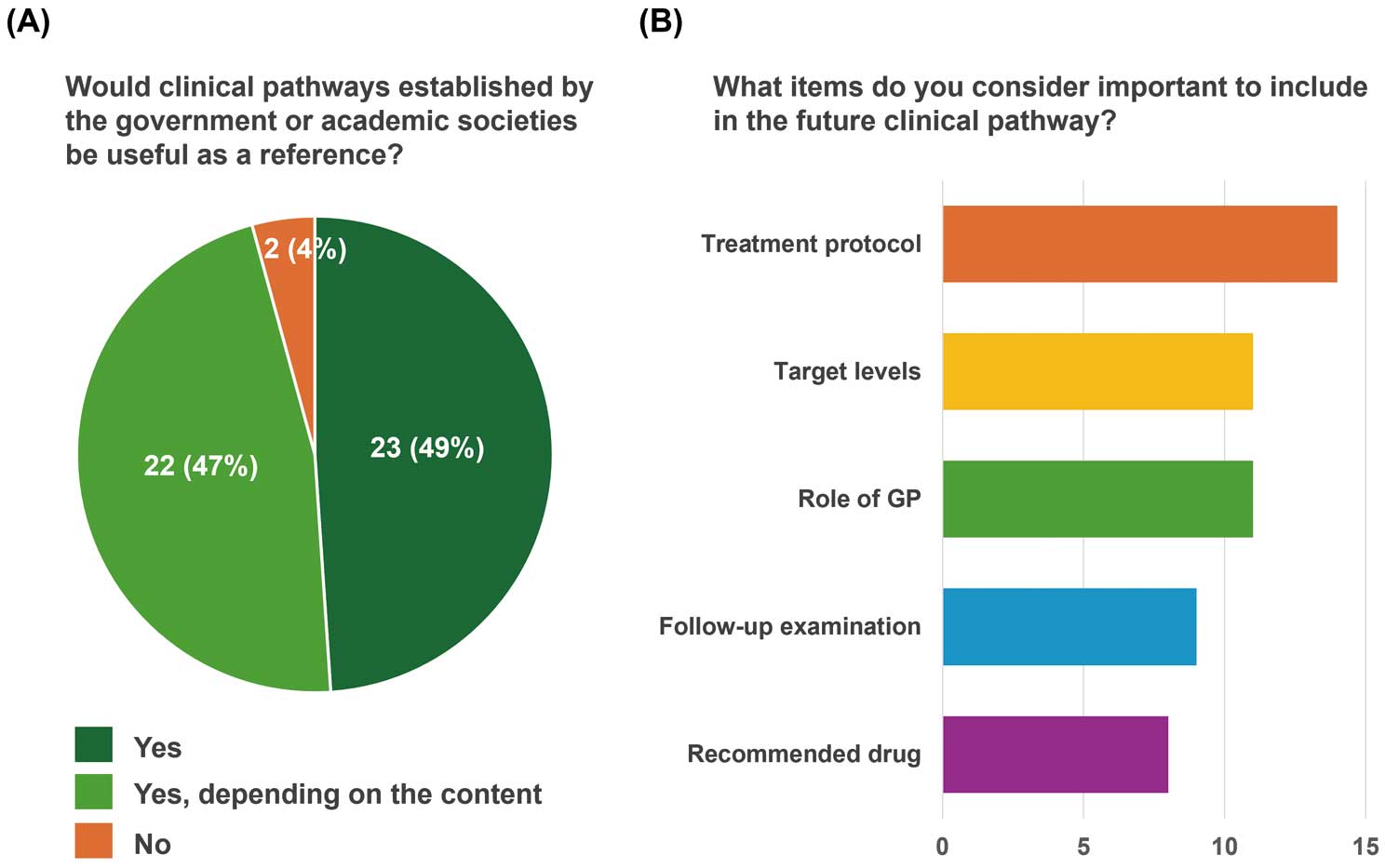
The results of the questionnaire survey about expectations for future ACS collaborative pathway are shown in Figure 5. Forty-five of 47 prefectural JCA branches responded positively to future ACS collaborative pathways established by the government or academic societies, viewing them as potentially useful resources (Figure 5A). Among potential items in the future pathways, treatment protocol, target risk factor levels, and descriptions of the role of general physicians were primarily considered important.
Discussion
The main findings of this study were as follows. First, of the 47 prefectures in Japan, 11 have prefecture-wide pathways and 4 have region-wide pathways for ACS patients, with most pathways managed by prefectural or regional medical associations and a significant number not updated in the past 10 years. Second, most pathways describe risk factor targets, including LDL-C, HbA1c, and blood pressure, but only 8 pathways specified the target LDL-C as <70 mg/dL. Third, all functional pathways are all prefecture wide pathways, recently updated, and include treatment protocols. Fourth, expectations for future ACS pathways emphasized the need for them to be developed by government or academic societies and for them to include details regarding the implementation of treatment protocols, as well as updated target levels.
Development of Regional Collaborative Pathways for ACS Patients in Japan
Enhanced regional medical collaboration, including the use of clinical pathways, is positioned as a fundamental aspect of achieving a system that provides safe, secure, and high-quality medical care. The Ministry of Health, Labour and Welfare of Japan has identified the establishment of this system as a policy issue, and each prefecture is required to develop a plan to reinforce collaboration among local institutions for patient treatment and care. The fifth revision of the Medical Care Act in 2007 identified acute myocardial infarction as a disease for which a regional medical collaboration system should be established through the implementation of collaborative clinical pathways. This led to the creation and operation of regional collaborative clinical pathways for acute myocardial infarction in various medical institutions or regions. However, in the management of patients with ACS, the rate of achieving target LDL-C levels remains low.12 One potential reason for the low achievement rate is considered insufficient regional collaboration, indicating a need for more effective regional collaboration for ACS patients, including intensive care centers and general physicians in local clinics.13
Current Status of Regional Collaborative Pathways in Japan
The results of this survey revealed that regional collaborative clinical pathways for ACS patients are available in approximately one-third of prefectures in Japan (Figure 6). This suggests that there may be many regions where continuous and consistent treatment for ACS patients based on adequate collaboration between medical institutions is insufficient. The reasons for the limited penetration of regional collaborative pathways are unclear; however, one potential reason may be the difficulty in establishing pathways. Establishing a unified regional collaborative pathway requires the consolidation of opinions and intentions from physicians at various medical institutions, cooperation with administrative organizations and medical associations, and significant human and economic resources, all of which can be major barriers to the development of pathways. The present survey also showed that many of the unified prefecture-wide pathways were established by cooperative councils organized by core hospitals, medical associations, and administrative organizations, and were recently revised and updated based on the latest guidelines. Conversely, most region-wide pathways were primarily established by local medical associations and have not been revised for many years. These results indicate that, for the implementation of regional collaborative pathways, it is crucial to also establish a system to sustain their operation.

Structure and Functionality of the Pathways
Although most pathways included target LDL-C, HbA1c, and blood pressure levels, it was found that most pathways did not include the most recent updated levels or recommended medications. In addition, more than half the pathways specified coronary angiography as a routine follow-up examination, even though the latest guideline does not recommend its use for patients without symptoms or ischemic findings.14 Some prefecture-wide pathways included target LDL-C levels and specific treatment protocols for lipid-lowering therapy based on current guidelines, which are expected to standardize treatment and improve clinical outcomes for patients. Conversely, most region-wide pathways used status sheets with a large number of blank cells that were to be filled with vital signs, laboratory findings, and medications, suggesting that they require considerable operational effort. Thus, minimizing and selecting items by focusing on practical efficacy are future challenges. From the results of the questionnaire survey, it became clear that the characteristics of functional pathways included being prefecture wide, incorporating specific treatment protocols, and having updated target risk factors levels and recommended medications. These findings suggest that it is important to update the contents of pathways in accordance with the latest guidelines for the sustainable operation of regional collaborative pathways.15
Prospects for Regional Collaborative Pathways for ACS Patients
This study revealed that regions with existing and adequately functioning regional collaborative pathways for ACS patients are limited. Conversely, there is significant expectation for future pathways established by administrative organizations and academic societies, suggesting a need to reinforce regional collaboration through these pathways. It is also recognized that including practical content, such as specific treatment protocols, target levels, and the roles of general physicians, is important for ideal pathways. Given the significant barriers to establishing pathways in each region, an ideal approach may be for academic societies to take the initiative in creating exemplary unified pathways, which can then be adapted to fit the specific characteristics of each region.
Assessing the effectiveness of regional collaborative pathways is an important issue for the future. Regional collaborative pathways are believed to enhance treatment standardization and optimization by fostering collaboration among institutions, addressing therapeutic inertia and knowledge gaps among physicians, enhancing patient adherence to hospital visits and medications, and expanding educational opportunities for patients.15 Consequently, these pathways are expected to further improve clinical outcomes. In the future, it will be essential to determine appropriate indicators and establish sustainable systems for the continuous evaluation of the anticipated effects of these clinical pathways.
Study Limitations
This study has several limitations. First, it is possible that some pathways were overlooked, despite our efforts to comprehensively identify regional collaborative pathways through questionnaire and web-based surveys. Second, this study may not have fully captured the status of clinical pathways for ACS patients in Japan because institutional pathways were excluded from the analysis due to challenges in comprehensively detecting and assessing their operational status, despite their potential significant impact in specific regions. Third, the evaluation method for determining the functionality of clinical pathways was left to the discretion of each JCA branch, potentially compromising objectivity.
Conclusions
Regional collaborative clinical pathways for ACS patients in Japan show variable implementation across prefectures, with approximately one-third of prefectures having established pathways. The structure and operational status of these pathways highlight the need for appropriate updates and sustained regional cooperation to optimize patient outcomes. Future efforts should prioritize establishing sustainable pathways, including treatment protocols and updated treatment targets, and enhancing regional collaboration to address ongoing challenges in ACS management.
Acknowledgments
The authors extend their sincere gratitude to all prefectural managers of JCA branches (https://j-circ-assoc.or.jp/branches/list/) who contributed their time and insights by completing the questionnaire. The authors also express their appreciation to Tomo Inoue of 3ROCK K.K. for his contributions to data collection. During the preparation of this manuscript, the authors used ChatGPT-4 (OpenAI) to enhance the quality of English language expression.
Sources of Funding
This study was conducted as part of the Open Call Project of the Japanese Circulation Association, which is funded by Amgen K.K.
Disclosures
Y.M. has received remuneration from Amgen K.K. and Novartis Pharma K.K. H.S. has received remuneration from Medtronic Japan Co., Ltd and Novartis Pharma K.K.; research funding from JIMRO Co., Ltd, Nippon Boehringer Ingelheim Co., Ltd, Medtronic Japan Co., Ltd, Daiichi Sankyo Co., Ltd, Japan Lifeline Co., Ltd, Abbott Medical Japan LLC, Amgen Astellas BioPharma K.K., Novartis Pharma K.K., and the Japan Heart Foundation; and scholarship funds and donations from Ono Pharmaceutical Co., Ltd, JCT Co., Ltd, Pfizer Japan Inc., and Abbott Medical Japan LLC. J.A. has received remuneration from Amgen K.K., Novartis Pharma K.K., Nippon Boehringer Ingelheim Co., Ltd, Daiichi Sankyo Co., Ltd, Ono Pharmaceutical Co., Ltd, Bayer Yakuhin, Ltd., Kowa Pharmaceutical Co. Ltd., and Mochida Pharmaceutical Co. Ltd. Y.S. has received remuneration from Otsuka Pharmaceutical Co., Ltd. and Novartis Pharma K.K., as well as research funding from Otsuka Pharmaceutical Co., Ltd. and Novartis Pharma K.K. I.K. has received remuneration from AstraZeneca K.K. and Novo Nordisk Pharma Ltd, as well as scholarship fund from Idorsia Pharmaceuticals Japan Ltd. I.K. is affiliated with a department endowed by Idorsia Pharmaceuticals Japan K.K., Novo Nordisk Pharma Ltd., Toa Eyo Company, Ltd., Takara Bio Inc., Nippon Boehringer Ingelheim Co., and BioStream, Inc. Y.I., J.A., Y.J.A., and I.K. are members of Circulation Journal’s Editorial Team.
IRB Information
The Japanese Circulation Association granted an exemption from requiring ethics approval.
Supplementary Files
Please find supplementary file(s);
https://doi.org/10.1253/circj.CJ-24-0714
References
- 1.
Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC guidelines for the management of acute coronary syndromes: Developed by the Task Force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J 2023; 44: 3720–3826.
- 2.
Erlinge D, Maehara A, Ben-Yehuda O, Bøtker HE, Maeng M, Kjøller-Hansen L, et al. Identification of vulnerable plaques and patients by intracoronary near-infrared spectroscopy and ultrasound (PROSPECT II): A prospective natural history study. Lancet 2021; 397: 985–995.
- 3.
Minami Y, Ako J, Tsujita K, Yokoi H, Ikari Y, Morino Y, et al. Drug intervention as an emerging concept for secondary prevention in patients with coronary disease. Cardiovasc Interv Ther 2024; 39: 223–233.
- 4.
Yoshikawa M, Honda A, Arashi H, Shibahashi E, Otsuki H, Kawada-Watanabe E, et al. Addition of ezetimibe to intensive lipid-lowering therapy is associated with a lower incidence of heart failure in patients with acute coronary syndrome. Circ J 2024; 88: 1819–1824, doi:10.1253/circj.CJ-24-0536.
- 5.
Watanabe H, Morimoto T, Yamamoto K, Obayashi Y, Natsuaki M, Yamaji K, et al. Prevalence and effects of high-intensity statins for Japanese patients presenting with acute coronary syndrome: A post hoc secondary analysis of STOPDAPT-2 ACS. Circ J 2023; 87: 657–668.
- 6.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med 2018; 379: 2097–2107.
- 7.
Okamura T, Tsukamoto K, Arai H, Fujioka Y, Ishigaki Y, Koba S, et al. Japan Atherosclerosis Society (JAS) guidelines for prevention of atherosclerotic cardiovascular diseases 2022. J Atheroscler Thromb 2024; 31: 641–853.
- 8.
Nakamura M, Ako J, Arai H, Hirayama A, Nohara A, Murakami Y, et al. Lipid management and 2-year clinical outcomes in Japanese patients with acute coronary syndrome: EXPLORE-J. J Atheroscler Thromb 2021; 28: 1307–1322.
- 9.
Nakao S, Ishihara T, Tsujimura T, Iida O, Hata Y, Toyoshima T, et al. Effectiveness of hospital lipid-lowering protocol of intensive lipid-lowering therapy for patients with acute coronary syndrome. J Cardiol 2022; 79: 391–399.
- 10.
Okada K, Haze T, Kikuchi S, Kirigaya H, Hanajima Y, Tsutsumi K, et al. Early, intensive and persistent lipid-lowering therapy for secondary prevention of acute coronary syndrome. J Atheroscler Thromb 2024; 31: 1748–1762, doi:10.5551/jat.64988.
- 11.
Kageyama S, Murata K, Nawada R, Onodera T, Maekawa Y. Unique referral system contributes to long-term net clinical benefits in patients undergoing secondary prevention therapy after percutaneous coronary intervention. PLoS One 2020; 15: e0242707, doi:10.1371/journal.pone.0242707.
- 12.
Mitani H, Suzuki K, Ako J, Iekushi K, Majewska R, Touzeni S, et al. Achievement rates for low-density lipoprotein cholesterol goals in patients at high risk of atherosclerotic cardiovascular disease in a real-world setting in Japan. J Atheroscler Thromb 2023; 30: 1622–1634.
- 13.
Crawshaw J, Bartoli-Abdou JK, Weinman J, McRobbie D, Stebbins M, Brock T, et al. The transition from hospital to home following acute coronary syndrome: An exploratory qualitative study of patient perceptions and early experiences in two countries. Int J Pharm Pract 2021; 29: 61–69.
- 14.
Virani SS, Newby LK, Arnold SV, Bittner V, Brewer LC, Demeter SH, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease: A report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2023; 148: e9–e119.
- 15.
Krychtiuk KA, Ahrens I, Drexel H, Halvorsen S, Hassager C, Huber K, et al. Acute LDL-C reduction post ACS: Strike early and strike strong: From evidence to clinical practice. A clinical consensus statement of the Association for Acute CardioVascular Care (ACVC), in collaboration with the European Association of Preventive Cardiology (EAPC) and the European Society of Cardiology Working Group on Cardiovascular Pharmacotherapy. Eur Heart J Acute Cardiovasc Care 2022; 11: 939–949.