Abstract
Background: In Japan, the implantation of implantable cardioverter defibrillators (ICD) for the primary prevention of sudden cardiac death (SCD) is not covered by insurance reimbursement, and the underuse of ICDs has been noted. Therefore, this study analyzed the medical costs incurred due to a lack of primary prevention ICD therapy for SCD.
Methods and Results: This retrospective cohort study analyzed data from 4 advanced critical care centers between January 2020 and December 2024. From a database of 3,606 cases of cardiac arrest, there were 348 patients with a documented rhythm at the time of arrest that could have been treated with an ICD. Of these patients, 43 (12.4%) had documented evidence of heart failure treatment and were eligible for ICD implantation before experiencing a cardiac arrest. The total mean (±SD) medical cost for these patients was US $11,679±14,666 (¥1,775,150±2,229,272).
Conclusions: In this multicenter retrospective analysis, we identified a subset of patients who were eligible for primary prevention ICD therapy but did not receive it prior to experiencing sudden cardiac arrest. These cases were associated with substantial post-arrest medical costs. Our findings highlight the potential clinical and economic impact of the underutilization of ICDs in Japan and suggest that broader implementation of guideline-directed ICD therapy for primary prevention may reduce both mortality and healthcare expenditure.
Reduced left ventricular (LV) function is strongly correlated with the incidence of sudden cardiac death (SCD). Implantable cardioverter defibrillator (ICD) therapy, including cardiac resynchronization therapy defibrillator (CRT-D) therapy, has been globally implemented because it reduces overall mortality in patients with heart failure and LV dysfunction, as well as the incidence of SCD.1–8 In Japan, the Nippon Storm Study demonstrated that the primary preventive effect of ICD therapy on SCD reduction is equivalent to its secondary preventive effect in patients with both ischemic and non-ischemic cardiomyopathy.9–13
The guidelines of the Japanese Circulation Society (JCS)/Japanese Heart Rhythm Society (JHRS), which are aligned with global ICD guidelines such as those published by the ESC/EHRA and ACC/AHA/HRS, adopt an LV ejection fraction (LVEF) of ≤35% as the criterion for ICD implantation for the primary prevention of SCD.14 However, in Japan, ICD implantation for the primary prevention of SCD is not covered by insurance reimbursement, and the underuse of ICDs has been noted.15,16 Moreover, the medical costs and social losses associated with the insufficient implementation of primary prevention ICD therapy have not been analyzed. Therefore, the aim of the present study was to analyze the medical costs and social losses incurred due to the lack of primary prevention ICD therapy for SCD.
Methods
Study Design and Setting
This was a retrospective cohort study using data from 4 critical care centers or equivalent facilities in Japan located in the Kanto region of Japan, conducted from January 2020 to December 2024. Using structured and linked clinical data, this study aimed to clarify the associated medical costs for patients estimated to have had a cardiac arrest prevented by ICDs, including CRT-D, and to capture their prognosis.
The study protocol was approved by the Ethics Committee of TXP Medical Co., Ltd., and the requirement for informed consent was waived due to the retrospective design of the study.
Data Source
All 4 facilities implemented the NEXT Stage ER (NSER; TXP Medical Co. Ltd., Tokyo, Japan). The NSER assists physicians in creating medical records, structuring recorded data, and developing databases for clinical research. The NSER serves as the user interface for electronic medical records software, enabling medical professionals to record chief complaints, present illness, medical history, physical evaluation, and emergency department (ED) diagnoses in designated fields.17 When a medical professional enters data into the chief complaint field, it is automatically categorized according to 231 chief complaint categories based on the Japan Triage and Acuity Scale (JTAS). Medical history and current medication information are also structured within the system, which records data on the course of events after arrival, treatment timelines, vital signs, and electrocardiogram (ECG) waveforms. In cases of cardiac arrest, detailed records of the initial ECG waveform and time of return of spontaneous circulation (ROSC) are included in the database.
In addition to the ED data from the NSER, various clinical test results, medical records, ordering information, and Diagnosis Procedure Combination (DPC) FF/EF data stored in TXP Medical’s data warehouse were used as data sources. Medical data were purchased by Medtronic Japan Co., Ltd. from TXP Medical Co., Ltd. and provided solely as statistical data.
Study Population
This study included patients aged ≥18 years who were transported to the ED with out-of-hospital cardiac arrest and had an initial ECG showing shockable rhythm (ventricular tachycardia [VT] and ventricular fibrillation [VF]) or whose automated external defibrillator (AED) was activated on-site or during emergency transport. This study initially identified patients with cardiac arrest to evaluate those who were indicated for primary prevention ICDs, and the following exclusion criteria were applied (see Figure 1): age <18 years, non-cardiac cause of cardiac arrest, unknown rhythm at the time of arrest, no prior history of cardiac disease, poor pre-arrest activities of daily living, and not indicated for primary prevention ICD based on medical record review.
Criteria for ICD-Eligible Patients
In this study, ICD-eligible patients were identified using the JCS/JHRS guidelines through a chart review conducted by 2 independent physicians (cardiologists or emergency physicians) who were not among the study authors.14 If discrepancies arose between the 2 reviewers, a third cardiologist provided the final assessment. Exclusion criteria were evaluated through a visual review of the NSER; if the information contained therein was insufficient, additional chart reviews were conducted. For primary prophylactic ICDs, patients with a complete medical history and pre-event echocardiographic data who were highly likely to meet ICD eligibility criteria, as well as those with missing pre-event test data or medical history but suspected of having heart disease based on medication information, suggesting potential ICD eligibility, were collectively classified as the “pre-arrest ICD indication group.” Patients for whom ICD eligibility was not clearly indicated were excluded.
In accordance with the JCS/JHRS guidelines, the specific criteria for determining ICD eligibility included the following, but were assessed comprehensively from a clinical perspective:
• LVEF ≤35% before the event
• exact pre-event LVEF value
• the presence of non-sustained VT (NSVT)
• history of heart disease, if applicable (e.g., prior percutaneous coronary intervention, coronary artery bypass graft, ischemic heart disease).
Medical Costs
Medical costs were calculated using the DPC EF file. These costs represent the sum of both the bundled payment (comprehensive fee) and fee-for-service components of the DPC payment system. The costs included all medical expenses incurred for the treatment of cardiac arrest, including the basic hospitalization fee and costs related to the procedures, such as the addition of hypothermia therapy. For patients who underwent ICD implantation, the direct costs associated with ICD implantation were excluded (whereas hospitalization costs were included). Costs presented in US dollars were calculated using an average exchange rate of US $1=¥152, based on the Bank of Japan›s official rate over the 12 months from February 2024 to March 2025.
Statistical Analysis
Summary statistics were used to characterize patient characteristics and outcomes. Continuous variables are presented as the mean±SD, whereas categorical variables, such as nominal variables, are presented as the number of patients and the percentage of total patients. Missing values for each data point were calculated and reported. Statistical analyses were performed using R version 4.2.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
In this study, we analyzed 348 patients from a database of 3,606 patients who experienced a cardiac arrest after excluding minors, patients with non-cardiogenic cardiopulmonary arrest, and patients in whom a clear shockable rhythm could not be identified. From this group, we ultimately analyzed 43 patients who were eligible for primary prevention ICD implantation before experiencing cardiac arrest but had not received an ICD. A study flowchart for emergency transportation is shown in Figure 1.
Clinical Characteristics of the Primary Prevention ICD-Eligible Patients
Of the 43 patients included in the study, the mean age was 68.3±18.0 years, and 38 (88.4%) were male (Table 1). Information on medical history, comorbidities, medications, initial waveform at the time of cardiac arrest, number of defibrillations, and laboratory test results are presented in Table 1. The percentage of bystanders who used an AED was 32.6%. Myocardial ischemia was the cause of cardiac arrest in 15 of 43 (34.9%) patients.
Table 1.
Patient Characteristics Among Patients With a Confirmed Pre-Arrest ICD Indication
| |
All patients
(n=43) |
Died in ED
(n=17) |
Admitted to hospital
(n=26) |
| Patient demographics |
| Age (years) |
68.3±18.0 |
65.6±23.3 |
70.0±14.8 |
| Male sex |
38 (88.4) |
14 (82.4) |
24 (92.3) |
| Presence of comorbidity/past medical history |
| Acute myocardial infarction |
14 (32.6) |
7 (41.2) |
7 (26.9) |
| Ischemic cardiomyopathy |
5 (11.6) |
2 (11.8) |
3 (11.5) |
| Percutaneous coronary intervention |
1 (2.3) |
0 (0.0) |
1 (3.9) |
| Coronary artery bypass graft |
4 (9.3) |
3 (17.7) |
1 (3.9) |
| Chronic kidney disease |
3 (7.0) |
1 (5.9) |
2 (7.7) |
| Atrial arrhythmia |
4 (9.3) |
0 (0.0) |
4 (15.4) |
| Ventricular arrhythmia including VT and VF |
4 (9.3) |
2 (11.8) |
2 (7.7) |
| Heart failure |
13 (30.2) |
4 (23.5) |
9 (34.6) |
| Valvular heart disease |
1 (2.3) |
0 (0.0) |
1 (3.9) |
| Stroke/transient ischemic attack |
6 (14.0) |
2 (11.8) |
4 (15.4) |
| Congenital heart disease |
2 (4.7) |
1 (5.9) |
1 (3.9) |
| Hypertension |
3 (7.0) |
2 (11.8) |
1 (3.9) |
| Pre-arrest NSVT |
| Yes |
6 (14.0) |
2 (11.8) |
4 (15.4) |
| No |
23 (53.5) |
8 (47.1) |
15 (57.7) |
| Unknown |
14 (32.6) |
7 (41.2) |
7 (26.9) |
| First documented rhythm at the scene |
| Shockable |
35 (81.4) |
12 (70.6) |
23 (88.5) |
| Non-shockable |
4 (9.3) |
4 (23.5) |
0 (0.0) |
| Presence of pulse |
4 (9.3) |
1 (5.9) |
3 (11.5) |
| AED use by bystanders |
| Yes |
14 (32.6) |
3 (17.7) |
11 (42.3) |
| No |
26 (60.5) |
12 (70.6) |
14 (53.9) |
| Unknown |
3 (7.0) |
2 (11.8) |
1 (3.9) |
| No. shocks delivered |
| Prehospital setting |
| 0 |
7 (16.3) |
5 (29.4) |
2 (7.7) |
| 1 |
8 (18.6) |
3 (17.7) |
5 (19.2) |
| 2 |
7 (16.3) |
5 (29.4) |
2 (7.7) |
| 3 |
6 (14.0) |
0 (0.0) |
6 (23.1) |
| ≥4 |
13 (30.2) |
4 (23.5) |
9 (34.6) |
| Unknown |
2 (4.7) |
0 (0.0) |
2 (7.7) |
| In-hospital setting |
| 0 |
21 (48.8) |
7 (41.2) |
14 (53.9) |
| 1 |
4 (9.3) |
1 (5.9) |
3 (11.5) |
| 2 |
8 (18.6) |
4 (23.5) |
4 (15.4) |
| 3 |
2 (4.7) |
0 (0.0) |
2 (7.7) |
| ≥4 |
4 (9.3) |
2 (11.8) |
2 (7.7) |
| Unknown |
4 (9.3) |
3 (17.7) |
1 (3.9) |
| Laboratory data |
| Creatinine on hospital admission (mg/dL) |
1.4±0.5 |
1.3±0.2 |
1.5±0.4 |
| eGFR on hospital admission (mL/min/1.73 m2) |
54.3±20.1 |
65.0±11.9 |
54.2±18.9 |
| BNP on hospital admission (pg/mL) |
635.3±934.3 |
194.1±284.3 |
660.7±822.4 |
| Detailed cause of arrests |
Acute myocardial infarction or ischemic heart
disease |
15 (34.9) |
6 (35.3) |
9 (34.6) |
| Other |
28 (65.1) |
11 (64.7) |
17 (65.4) |
Continuous data are presented as the mean±SD; categorical data are presented as n (%). AED, automated external defibrillator; BNP, B-type natriuretic peptide; ED, emergency department; eGFR, estimated glomerular filtration rate; ICD, implantable cardioverter defibrillator; NSVT, non-sustained ventricular tachycardia; VF, ventricular fibrillation; VT, ventricular tachycardia.
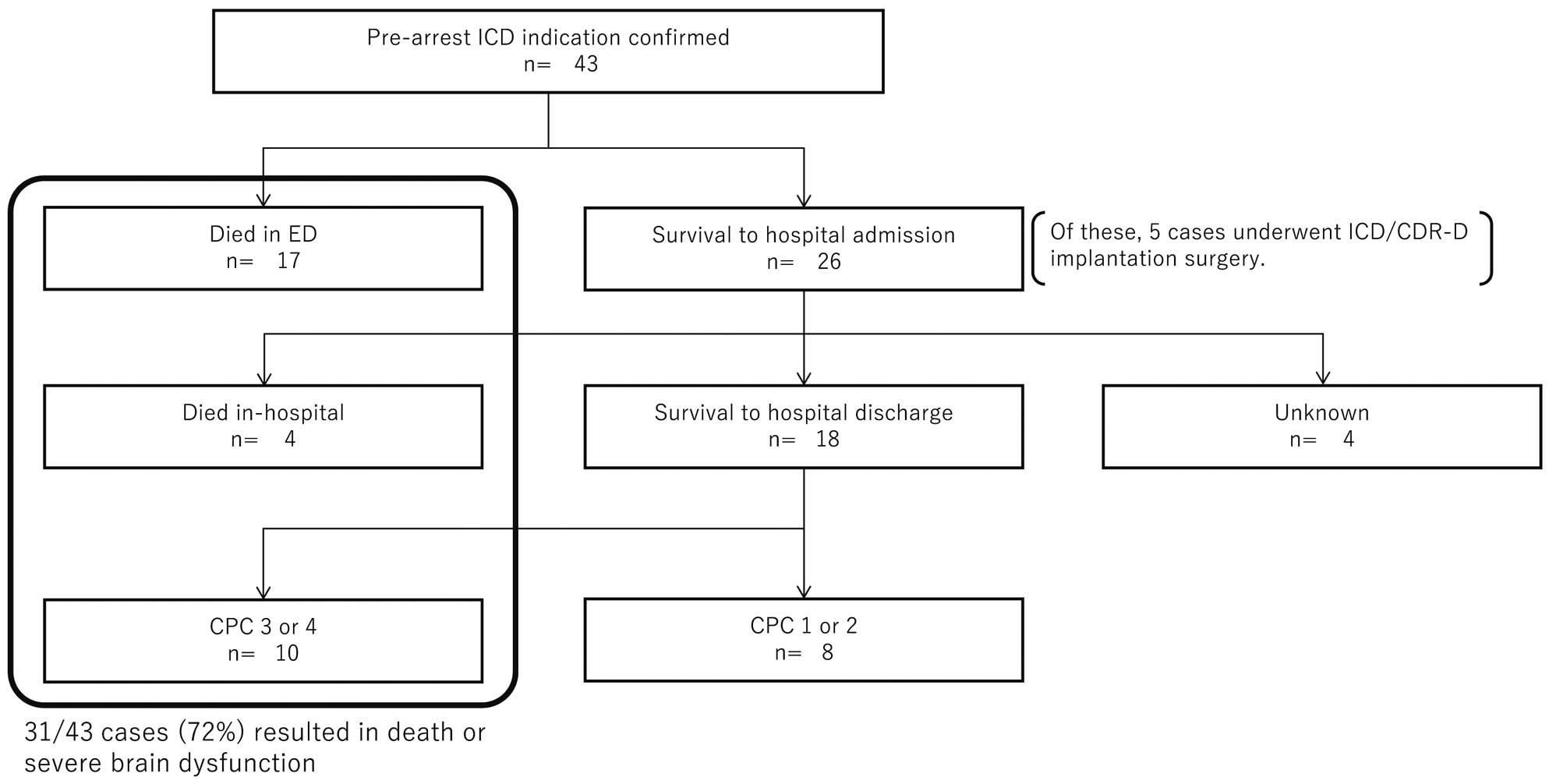
A study flowchart for emergency transport is shown in Figure 2. Of the 43 patients in the study, 17 (39.5%) died in the ED. Of the remaining 26 patients (60.5%) who were hospitalized, 4 died during hospitalization, with 2 classified as cardiac deaths and the remaining 2 as non-cardiac deaths. Eighteen patients were discharged alive; however, 10 had severe neurological sequelae classified as a Cerebral Performance Category Scale (CPC) of 3 or 4. The CPC classifications are as follows: CPC 1, consciousness with normal function or mild disability; CPC 2, consciousness with moderate disability; CPC 3, consciousness with severe disability; CPC 4, coma or vegetative state; and CPC 5, brain death. We established a good outcome as a CPC of 1 or 2 and a poor outcome as a CPC of 3–5 at discharge.18–20 Data were missing for the remaining 4 patients.
In-Hospital Procedures
Of the 26 patients who survived to hospital admission with a confirmed pre-arrest ICD indication, 12 (46.2%) required circulatory support with extracorporeal membrane oxygenation (Table 2). To stabilize hemodynamics, catheter ablation was performed in 2 (7.7%) patients, and percutaneous coronary intervention was performed in 4 (15.4%). Ultimately, 5 (19.2%) patients underwent ICD or CRT-D implantation during hospitalization for secondary prevention of SCD.
Table 2.
In-Hospital Procedures for Patients Who Survived to Hospital Admission With Pre-Arrest ICD Indication Confirmed
| |
Survived to hospital
admission (n=26) |
| Hemodialysis/CRRT |
5 (19.2) |
| Mechanical ventilation |
19 (73.1) |
| Electrophysiology study/ablation |
2 (7.7) |
| Percutaneous coronary intervention |
4 (15.4) |
| Circulatory support |
| Impella |
3 (11.5) |
| ECMO |
12 (46.2) |
| IABP |
4 (15.4) |
| ICD or CRT-D implantation |
5 (19.2) |
Data are presented as n (%). CRRT, continuous renal replacement therapy; CRT-D, cardiac resynchronization therapy with a defibrillator; ECMO, extracorporeal membrane oxygenation; IABP, intra-aortic balloon pump; ICD, implantable cardioverter defibrillator.
Outcomes After Hospital Admission
Of the 26 patients who survived to hospital admission with confirmed pre-arrest ICD indications, 18 (69.2%) were discharged alive, 4 (15.4%) died during hospitalization, and data were missing for 4 (15.4%). The mean length of hospitalization was 12.6±11.7 days, with a mean stay in the intensive care unit of 4.2±4.9 days. Of the 18 (69.2%) patients who were discharged alive, 13 (50%) were discharged home, with the remaining 5 (19.2%) transferred to another hospital or admitted to a care facility (Table 3).
Table 3.
Outcomes Among Patients Who Survived to Hospital Admission With Pre-Arrest ICD Indication Confirmed
| |
Survived to hospital
admission (n=26) |
| Outcome |
| Survival to hospital discharge |
18 (69.2) |
| Death (in-hospital mortality) |
4 (15.4) |
| Unknown |
4 (15.4) |
| Hospitalization outcomes |
| Length of hospital stay (days) |
12.6±11.7 |
| Length of ICU stay (days) |
4.2±4.9 |
| Destination after hospitalization |
| Home |
13 (50.0) |
| Other healthcare facility |
5 (19.2) |
Continuous data are presented as the mean±SD; categorical data are presented as n (%). ICD, implantable cardioverter defibrillator; ICU, intensive care unit.
Total Medical Costs
Among the 32 patients with available data, the mean total medical cost was US $11,679±14,666 (¥1,775,150±2,229,272; Table 4). For patients who survived to hospital admission, the mean total medical cost was US $15,879±16,044 (¥2,413,683±2,438,717). In contrast, for patients who were transported but died in the ED, the total medical cost was US $2,437±1,489 (¥370,379±226,400).
Table 4.
Total Costs in Patients With Pre-Arrest ICD Indication Confirmed
| |
NA |
Total costs |
| USD |
JPY |
| Patients with pre-arrest ICD indication confirmed |
32 |
11,679±14,666 |
1,775,150±2,229,272 |
| Patients who survived to hospital admission |
22 |
15,879±16,044 |
2,413,683±2,438,717 |
| Hospital stay ≤1 day |
5 |
6,299±2,045 |
957,456±310,821 |
| Hospital stay 2–7 days |
8 |
15,541±12,573 |
2,362,254±1,911,047 |
| Hospital stay ≥8 days |
9 |
21,753±10,534 |
3,306,431±1,601,100 |
| Died in ED |
10 |
2,437±1,489 |
370,379±226,400 |
Unless indicated otherwise, data are presented as the mean±SD. ANumber of patients used in the calculation. ED, emergency department; ICD, implantable cardioverter defibrillator; JPY, Japanese yen; USD, US dollars.
Discussion
The major findings of this study are as follows:
1. Of the 348 patients with cardiogenic cardiac arrest and a clearly documented shockable rhythm at the time of arrest, 43 (12.4%) had documented evidence of receiving heart failure treatment and were eligible for primary prevention ICD implantation before experiencing a cardiac arrest.
2. Among these 43 patients, 17 (39.5%) died in the ED.
3. Of the 26 (60.5%) patients who survived hospitalization, 4 (15.3%) died during hospitalization. In addition, among those who survived until discharge (18 patients), 10 (55.6%) were discharged with severe neurological sequelae classified as CPC 3 or CPC 4.
4. Among the patients who survived to hospital admission, the mean total medical cost, excluding the cost of ICD implantation, was US $15,879±16,044 (¥2,413,683±2,438,717).
In summary, among cardiac arrest patients who were eligible for primary prevention ICD implantation and received heart failure treatment before cardiac arrest, approximately half died in hospital and approximately one-quarter were discharged with severe neurological impairment. To the best of our knowledge, this is the first study in Japan to analyze medical costs using a database of patients who experienced cardiac arrest. Among the patients who should have been treated with an ICD for the primary prevention of SCD, only a limited number were able to achieve social reintegration despite experiencing cardiac arrest with a shockable rhythm.
Proportion of Cardiac Arrest Patients With a Shockable Rhythm
In this study we analyzed only the patients in whom a clear shockable rhythm was documented after cardiac arrest, accounting for approximately 10% of patients in the database. However, in recent years, reports have emerged suggesting that shockable rhythms during cardiac arrest may be more common than previously thought.21 Previous reports have shown that among 14,065 cases of out-of-hospital cardiac arrest, 43% of patients had VF recorded on the initial ECG. However, the estimated incidence of VF at the time of onset of cardiac arrest is reported to be 60–70% overall and 80–85% in patients with underlying heart disease.22 These discussions are also consistent with recent data suggesting that even in patients in whom VT or VF was not documented during out-of-hospital cardiac arrest, the majority still had shockable rhythms.23–25 Consequently, preventive and therapeutic interventions targeting ventricular arrhythmia, as represented by the use of ICDs for the primary prevention of SCD, should continue to be a key focus in future clinical practice.
Underuse of ICD
In Japan, the use of ICDs for primary prevention is limited owing to restricted insurance coverage, leading to what is referred to as an “underuse” situation. This restriction has hindered the widespread adoption of ICDs among patients at a high risk of SCD, raising concerns about the potential increase in preventable deaths and complications.
The CHART-2 study by Satake et al. highlighted the low implantation rate of ICDs for primary prevention in patients with heart failure in Japan.26 That study analyzed 2,778 patients with New York Heart Association Class II–III chronic heart failure (80.9% with ischemic heart disease) and classified them into 3 groups based on LVEF ≤35% and the presence of NSVT. The results revealed that only 30.4% of patients with Class I indications and 6.6% with Class IIa indications underwent ICD implantation.26 Furthermore, the risk of lethal arrhythmic events was significantly higher in those with Class I and Class II indications (9.89- and 4.95-fold higher) relative to those without an ICD indication (LVEF >35%),26 supporting the validity of risk stratification based on the guidelines.
Together with the present study, these previous findings indicate that ICDs for primary prevention are underutilized in Japan. Potential contributing factors include limitations in insurance coverage, a lack of awareness among healthcare providers, and insufficient patient education. Promoting guideline-based ICD implantation is essential for improving patient outcomes. The Nippon Storm Study, the largest registry in Japan, demonstrated that the primary prevention effect of ICDs in Japanese patients was equivalent to the secondary prevention effect for both ischemic cardiomyopathy and non-ischemic cardiomyopathy.10,11 Furthermore, the recently conducted Japanese Heart Failure and Sudden Cardiac Death Prevention Trial (HINODE) showed that the rate of appropriate ICD therapy for primary prevention in Japan is comparable to that in Western countries.27 In addition, HINODE confirmed the validity of SCD risk stratification using LVEF ≤35% and NSVT,27 as recommended by the JCS/JHRS guidelines. This finding also suggests that the absence of ICD implantation leads to SCD.
Estimated Medical Costs for Patients With Severe Brain Damage
Of the cardiac arrest patients with shockable rhythm, 43 were identified as potential candidates for primary prevention ICD implantation prior to the onset of their cardiac arrest. Of these 43 patients, 17 died in the ED and 26 were hospitalized. Of those who were hospitalized, 10 were discharged with severe disabilities (classified as CPC 3 or CPC 4) and 4 died during hospitalization. Patients with disabilities classified as CPC 3 were unable to live independently and required daily assistance with basic activities. Although some individuals may retain limited communication abilities, they may also experience significant cognitive impairment. In contrast, patients classified as CPC 4 are unconscious or unable to communicate, and although they be able to breath spontaneously, they are entirely dependent on caregivers for feeding and toileting.
We examined the post-discharge costs of patients with CPC 3–4 (n=10). According to previous studies, the distribution of the modified Rankin Scale (mRS) scores for CPC 3 and CPC 4 patients at discharge are 2% mRS3, 90.8% mRS4, and 7.2% mRS5 for those classified as CPC 3 and 100% mRS5 for those classified as CPC 4.28–30 Based on prior research, the estimated annual costs for each mRS category were US $34,733 (¥5,279,416) for mRS3, US $37,571 (¥5,710,792) for mRS4, and US $41,830 (¥6,358,160) mRS5.31 By estimating the proportion of patients classified as CPC 3 among all CPC 3–4 patients (n=10) in scenarios ranging from 10% to 90%, the total projected annual post-discharge cost for this group with a poor prognosis ranged from US $382,218 to US $414,291 (¥58,097,135–62,972,215). In addition, we estimated the survival duration until death for all 10 patients based on the 1-year survival rates of patients classified as CPC 3 and CPC 4 reported previously of 63.9% and 28%, respectively.32 When these rates were applied to scenarios where the proportion of CPC 3 patients ranged from 10% to 90%, the estimated time to death for all patients was a maximum of 4 years. These findings suggest that medical and long-term care costs are expected to last for several years in this population with a poor prognosis.
Cost Analysis and Potential Benefits of Primary Prevention ICDs in Shockable Cardiac Arrest
The life expectancy of patients with a CPC of 3 or 4 is generally approximately 4 years after discharge. In addition, among the 10 patients with severe neurological sequelae, the medical costs were incurred over a maximum of 4 years were approximately US $410,000 (¥63,000K). This means that, on average, the cost incurred was US $41,000 (¥6,300K) per patient. Based on this, the total estimated medical cost per patient from the cardiac arrest event to emergency transport was approximately US $16,000 (¥2,400,000); combined with the US $41,000 (¥6,300,000) post-discharge cost, the total estimated medical expense per patient was US $57,000 (¥8,700,000). For comparison, the total medical costs for a typical ICD implantation were calculated as US $27,000 (¥4,000,000) based on the clinical pathway of Chiba University Hospital, which was chosen as a reference because it maintains detailed cost data and follows standardized ICD implantation protocols that are representative of current clinical practice in Japan.
Estimating the Number Needed to Treat Based on a Fixed Relative Risk Reduction
To estimate the number needed to treat using a fixed relative risk reduction, we used data from the Improve SCA Study33 and followed 4 steps, as outlined in the Supplementary Figure. In the Improved SCA Study, the 3-year mortality rate was 19.5% in the non-ICD group and 12.9% in the ICD group. Based on these results, we assumed that ICD implantation leads to a 34% relative reduction in mortality. Applying this effect to our study population with a 3-year mortality rate of 48.8%, the resulting absolute risk reduction is 16.6%. Therefore, the estimated number needed to treat is approximately 6, meaning that implanting ICDs in 6 patients would prevent 1 death over a 3-year period.
Study Limitations
This study has several limitations. First, the generalizability of the results is limited because of the small number of cases included in the analysis. This is because only a small number of patients had an initial VT or VF rhythm (shockable rhythm) recorded after cardiac arrest. Unfortunately, this may be due to the low rate of AED use in witnessed cardiac arrest cases among those analyzed in this study. In addition, some patients without recorded shockable rhythms may have originally presented with shockable rhythms that were not captured, probably because of delayed witnessing. Second, data on pre-arrest medical history and medication use were not available, making it difficult to determine the ICD eligibility of some patients. Third, our dataset did not include patients who had an ICD implanted prior to cardiac arrest, because such patients were excluded from the database. Therefore, we were unable to evaluate outcomes or hospitalization costs in this specific subgroup, such as patients with ICDs for primary prevention. Fourth, medical costs were analyzed using statistical data extracted from the NSER database, making it impossible to analyze detailed individual patient data. Fifth, this study focuses solely on cases of cardiac arrest. However, to properly evaluate the cost-effectiveness of primary prevention ICD implantation, it is necessary to include patients who did not experience cardiac arrest. In the future, a large-scale cost-effectiveness analysis of ICD implantation for primary prevention should be conducted in Japan.
Conclusions
In this multicenter retrospective analysis, we identified a subset of patients who were eligible for primary prevention ICD therapy but did not receive it prior to experiencing sudden cardiac arrest. These cases were associated with substantial post-arrest medical costs. Our findings highlight the potential clinical and economic impacts of the underutilization of ICDs in Japan and suggest that broader implementation of guideline-directed ICD therapy for primary prevention may reduce both mortality and healthcare expenditure.
Sources of Funding
This study did not receive any specific funding.
Disclosures
Y. Kondo has received lecture fees from Daiichi-Sankyo, Bayer, Abbott Medical Japan, Biotronik Japan, Boston Scientific, Japan Lifeline, and Medtronic, as well as research funds from Daiichi-Sankyo and Boston Scientific. T.G. is an employee of TXP Medical. J.A.C. is an employee of Medtronic, Plc., and S.O. is an employee of Medtronic Japan. Y. Kobayashi has received lecture fees from Abbott Medical Japan, Bayer Japan, Bristol-Myers Squibb, Boehringer Ingelheim, and Daiichi-Sankyo, as well as scholarship funds from Takeda Pharmaceutical, Abbott Medical Japan, Terumo, Otsuka Pharmaceutical, Boehringer Ingelheim, Astellas, Daiichi-Sankyo, Win International, Japan Lifeline, and Nipro. H.T. has received honoraria for lectures and speaker bureaus from Daiichi Sankyo, Novartis Pharma, Medtronic Japan, Biotronik Japan, Bristol Myers Squibb, and Boston Scientific Japan, and has received grants (investigator-initiated study unrelated to this review topic) from Abbott Medical Japan, Daiichi Sankyo Company, Nippon Boehringer Ingelheim, Otsuka Pharmaceutical, Eli Lilly Japan, and Marubun Tsusyo. Y. Kobayashi is a member of Circulation Journal’s Editorial Team. H.T. is an Associate Editor of Circulation Journal. The remaining authors have no conflicts of interest to disclose.
IRB Information
This study was approved by the Ethics Committee of TXP Medical (Approval no. TXPREC-028).
Data Availability
The data generated in this study will not be shared.
Supplementary Files
Please find supplementary file(s);
https://doi.org/10.1253/circj.CJ-25-0195
References
- 1.
Desai AS, Fang JC, Maisel WH, Baughman KL. Implantable defibrillators for the prevention of mortality in patients with nonischemic cardiomyopathy: A meta-analysis of randomized controlled trials. JAMA 2004; 292: 2874–2879.
- 2.
Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005; 352: 225–237.
- 3.
Barakat AF, Saad M, Elgendy AY, Mentias A, Abuzaid A, Mahmoud AN, et al. Primary prevention implantable cardioverter defibrillator in patients with non-ischaemic cardiomyopathy: A meta-analysis of randomised controlled trials. BMJ Open 2017; 7: e016352.
- 4.
Poole JE, Olshansky B, Mark DB, Anderson J, Johnson G, Hellkamp AS, et al. Long-term outcomes of implantable cardioverter-defibrillator therapy in the SCD-HeFT. J Am Coll Cardiol 2020; 76: 405–415.
- 5.
Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. N Engl J Med 1996; 335: 1933–1940.
- 6.
Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002; 346: 877–883.
- 7.
Greenberg H, Case RB, Moss AJ, Greenberg H, Case RB, Moss AJ, et al. Analysis of mortality events in the Multicenter Automatic Defibrillator Implantation Trial (MADIT-II). J Am Coll Cardiol 2004; 43: 1459–1465.
- 8.
Goldenberg I, Gillespie J, Moss AJ, Hall WJ, Klein H, McNitt S, et al. Long-term benefit of primary prevention with an implantable cardioverter-defibrillator: An extended 8-year follow-up study of the Multicenter Automatic Defibrillator Implantation Trial II. Circulation 2010; 122: 1265–1271.
- 9.
Noda T, Kurita T, Nitta T, Chiba Y, Furushima H, Matsumoto N, et al. Significant impact of electrical storm on mortality in patients with structural heart disease and an implantable cardiac defibrillator. Int J Cardiol 2018; 255: 85–91.
- 10.
Sasaki S, Noda T, Okumura K, Nitta T, Aizawa Y, Ohe T, et al. Effectiveness of implantable cardioverter defibrillator in patients with non-ischemic heart failure with systolic dysfunction: Subanalysis of the Nippon Storm Study. Circ J 2022; 87: 92–100.
- 11.
Kondo Y, Noda T, Sato Y, Ueda M, Nitta T, Aizawa Y, et al. Comparison of 2-year outcomes between primary and secondary prophylactic use of defibrillators in patients with coronary artery disease: A prospective propensity score-matched analysis from the Nippon Storm Study. Heart Rhythm O2 2021; 2: 5–11.
- 12.
Kondo Y, Noda T, Takanashi Y, Sasaki S, Sato Y, Nitta T, et al. Two-year outcomes of primary prophylactic use of defibrillators for ischemic and non-ischemic cardiomyopathy: Propensity score-matched analysis from the Nippon Storm Study. Circ J 2024; 88: 1107–1114.
- 13.
Hanada K, Sasaki S, Kinjo T, Shikanai S, Yamazaki K, Kato T, et al. Incidence and predictors of appropriate implantable cardioverter defibrillator therapy in Japanese ischemic heart disease patients. Circ J 2025; 89: 354–363.
- 14.
Nogami A, Kurita T, Abe H, Ando K, Ishikawa T, Imai K, et al. JCS/JHRS 2019 guideline on non-pharmacotherapy of cardiac arrhythmias. Circ J 2021; 85: 1104–1244.
- 15.
Iwasaki Y, Noda T, Akao M, Fujino T, Hirano T, Inoue K, et al. JCS/JHRS 2024 guideline focused update on management of cardiac arrhythmias. Circ J 2025, doi:10.1253/circj.CJ-24-0073.
- 16.
Kitai T, Kohsaka S, Kato T, Kato E, Sato K, Teramoto K, et al. JCS/JHFS 2025 guideline on diagnosis and treatment of heart failure. Circ J 2025, doi:10.1253/circj.CJ-25-0002.
- 17.
Goto T, Hara K, Hashimoto K, Soeno S, Shirakawa T, Sonoo T, et al. Validation of chief complaints, medical history, medications, and physician diagnoses structured with an integrated emergency department information system in Japan: The Next Stage ER system. Acute Med Surg 2020; 7: e554.
- 18.
Phelps R, Dumas F, Maynard C, Silver J, Rea T. Cerebral performance category and long-term prognosis following out-of-hospital cardiac arrest. Crit Care Med 2013; 41: 1252–1257.
- 19.
Jennett B, Bond M. Assessment of outcome after severe brain damage: A practical scale. Lancet 1975; 1: 480–484.
- 20.
Kim TJ, Kim JM, Lee JS, Park SH, Jeong HB, Choi JK, et al. Prognostication of neurological outcome after cardiac arrest using wavelet phase coherence analysis of cerebral oxygen. Resuscitation 2020; 150: 41–49.
- 21.
Maury P, Marimpouy N, Beneyto M. What’s the cardiac rhythm at the time of cardiac arrest? Disputed dogma or true fact? Europace 2024; 27: euae299, doi:10.1093/europace/euae299.
- 22.
Holmberg M, Holmberg S, Herlitz J. Incidence, duration and survival of ventricular fibrillation in out-of-hospital cardiac arrest patients in Sweden. Resuscitation 2000; 44: 7–17.
- 23.
Andersson A, Arctaedius I, Cronberg T, Levin H, Nielsen N, Friberg H et al. In-hospital versus out-of-hospital cardiac arrest: Characteristics and outcomes in patients admitted to intensive care after return of spontaneous circulation. Resuscitation 2022; 176: 1–8.
- 24.
Inoue A, Hifumi T, Sakamoto T, Okamoto H, Kunikata J, Yokoi H, et al. Extracorporeal cardiopulmonary resuscitation in adult patients with out-of-hospital cardiac arrest: A retrospective large cohort multicenter study in Japan. Crit Care 2022; 26: 129.
- 25.
Okada Y, Kiguchi T, Irisawa T, Yamada T, Yoshiya K, Park C, et al. Development and validation of a clinical score to predict neurological outcomes in patients with out-of-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation. JAMA Netw Open 2020; 3: e2022920.
- 26.
Satake H, Fukuda K, Sakata Y, Miyata S, Nakano M, Kondo M, et al. Current status of primary prevention of sudden cardiac death with implantable cardioverter defibrillator in patients with chronic heart failure: A report from the CHART-2 Study. Circ J 2015; 79: 381–390.
- 27.
Aonuma K, Ando K, Kusano K, Asai T, Inoue K, Inamura Y, et al. Primary results from the Japanese Heart Failure and Sudden Cardiac Death Prevention Trial (HINODE). ESC Heart Fail 2022; 9: 1584–1596.
- 28.
Rittenberger JC, Raina K, Holm MB, Kim YJ, Callaway CW. Association between Cerebral Performance Category, Modified Rankin Scale, and discharge disposition after cardiac arrest. Resuscitation 2011; 82: 1036–1040.
- 29.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988; 19: 604–607.
- 30.
Shibahashi K, Konishi T, Ohbe H, Yasunaga H. Cost-effectiveness analysis of termination-of-resuscitation rules for patients with out-of-hospital cardiac arrest. Resuscitation 2022; 180: 45–51.
- 31.
Hattori N, Hirayama T, Katayama Y. Medical care for chronic-phase stroke in Japan. Neurol Med Chir (Tokyo) 2012; 52: 175–180.
- 32.
Phelps R, Dumas F, Maynard C, Silver J, Rea T. Cerebral Performance Category and long-term prognosis following out-of hospital cardiac arrest. Crit Care Med 2013; 41: 1252–1257.
- 33.
Zhang S, Ching CK, Huang D, Liu YB, Rodriguez-Guerrero DA, Hussin A, et al. Utilization of implantable cardioverter-defibrillators for the prevention of sudden cardiac death in emerging countries: Improve SCA clinical trial. Heart Rhythm 2020; 17: 468–475.