Article ID: CJ-66-0162
Article ID: CJ-66-0162
Dear Colleagues,
On behalf of the Editorial Team of Circulation Journal, I am pleased to announce the Circulation Journal Awards for the Year 2018.
The aim of these Awards is to recognize papers published in 2018, both clinical and experimental studies, that were highly appreciated by the Editorial Team. The selection process comprises 2 steps. In the first step, from 325 original papers published in the Journal in 2018, our 42 Japanese Associate Editors selected papers with a high scientific level in their respective fields, and in the second step, the 4 Associate Editorial Teams (10∼11 on 1 team) further evaluated the selected papers in terms of originality, contribution to cardiovascular science, manner of paper preparation, and future possibilities.
In the year of 2018, the following 7 papers have been selected for the Circulation Journal Awards.
First Place in the Clinical Investigation Section(Circ J 2018; 82: 2609–2618)1
| Clinical and Echocardiographic Impact of Tafazzin Variants on Dilated Cardiomyopathy Phenotype in Left Ventricular Non-Compaction Patients in Early Infancy Keiichi Hirono, Yukiko Hata, Makoto Nakazawa, Nobuo Momoi, Tohru Tsuji, Taro Matsuoka, Mamoru Ayusawa, Yuriko Abe, Tamaki Hayashi, Nobuyuki Tsujii, Tadaaki Abe, Heima Sakaguchi, Ce Wang, Asami Takasaki, Shinya Takarada, Mako Okabe, Nariaki Miyao, Hideyuki Nakaoka, Keijiro Ibuki, Kazuyoshi Saito, Sayaka Ozawa, Naoki Nishida, Neil E. Bowles, Fukiko Ichida (Department of Pediatrics (K.H., C.W., A.T., S.T., M.O., N. Miyao, H.N., K.I., K.S., S.O., F.I.), Legal Medicine (Y.H., N.N.), Graduate School of Medicine, University of Toyama, Toyama; Department of Pediatric and Lifelong Congenital Cardiology Institute, Southern Tohoku Research Institute for Neuroscience, Southern Tohoku General Hospital, Koriyama (M.N.); Department of Pediatrics, Fukushima Medical University, Fukushima (N. Momoi, T.T.); Department of Pediatrics, Toyonaka Municipal Hospital, Toyonaka (T.M.); Department of Pediatrics and Child Health, Nihon University School of Medicine, Tokyo (M.A., Y.A.); Department of Pediatrics, Nara Medical University, Kashihara (T.H., N.T.); Department of Pediatrics, Niigata City General Hospital, Niigata (T.A.); Department of Pediatric Cardiology, National Cerebral and Cardiovascular Center, Suita (H.S.), Japan; and Department of Occupational and Environmental Health and Safety, University of Utah, Salt Lake City, UT (N.E.B.), USA) |
 |
Background: Left ventricular non-compaction (LVNC) is a cardiomyopathy morphologically characterized by 2-layered myocardium and numerous prominent trabeculations, and is often associated with dilated cardiomyopathy (DCM). Variants in the gene encoding tafazzin (TAZ) may change mitochondrial function and cause dysfunction of many organs, but they also contribute to the DCM phenotype in LVNC, and the clinical and echocardiographic features of children with this phenotype are poorly understood.
Methods and Results: We enrolled 92 DCM phenotype LVNC patients and performed next-generation sequencing to identify the genetic etiology. Ten TAZ variants were identified in 15 male patients (16.3%) of the 92 patients, including 3 novel missense substitutions. The patients with TAZ variants had a higher frequency of early onset of disease (92.3% vs. 62.3%, P=0.0182), positive family history (73.3% vs. 20.8%, P=0.0001), and higher LV posterior wall thickness Z-score (8.55±2.60 vs. 5.81±2.56, P=0.0103) than those without TAZ variants, although the mortality of both groups was similar.
Conclusions: This study provides new insight into the impact of DCM phenotype LVNC and emphasizes the clinical advantages available for LVNC patients with TAZ variants.

(A) Left ventricular posterior wall (LVPW) and (B) compacted layer in the left ventricular posterior wall (LVPWC) thickness z-score in patients with dilated cardiomyopathy phenotype left ventricular non-compaction according to tafazzin (TAZ) variant status.
(Circ J 2018; 82: 874–885)2
| Acute Heart Failure in Patients With Severe Aortic Stenosis ― Insights From the CURRENT AS Registry ― Kazuya Nagao, Tomohiko Taniguchi, Takeshi Morimoto, Hiroki Shiomi, Kenji Ando, Norio Kanamori, Koichiro Murata, Takeshi Kitai, Yuichi Kawase, Chisato Izumi, Makoto Miyake, Hirokazu Mitsuoka, Masashi Kato, Yutaka Hirano, Shintaro Matsuda, Tsukasa Inada, Tomoyuki Murakami, Yasuyo Takeuchi, Keiichiro Yamane, Mamoru Toyofuku, Mitsuru Ishii, Eri Minamino-Muta, Takao Kato, Moriaki Inoko, Tomoyuki Ikeda, Akihiro Komasa, Katsuhisa Ishii, Kozo Hotta, Nobuya Higashitani, Yoshihiro Kato, Yasutaka Inuzuka, Chiyo Maeda, Toshikazu Jinnai, Yuko Morikami, Naritatsu Saito, Kenji Minatoya, Takeshi Kimura on behalf of the CURRENT AS Registry Investigators (Department of Cardiovascular Center, Osaka Red Cross Hospital, Osaka (K.N., T. Inada); Department of Cardiovascular Medicine (T.T., H.S., S.M., N.S., T. Kimura), Department of Cardiovascular Surgery (K. Minatoya), Kyoto University Graduate School of Medicine, Kyoto; Department of Clinical Epidemiology, Hyogo College of Medicine, Nishinomiya (T. Morimoto); Department of Cardiology, Kokura Memorial Hospital, Kitakyusyu (K.A.); Division of Cardiology, Shimada Municipal Hospital, Shimada (N.K.); Department of Cardiology, Shizuoka City Shizuoka Hospital, Shizuoka (K. Murata); Department of Cardiovascular Medicine, Kobe City Medical Center General Hospital, Kobe (T. Kitai); Department of Cardiovascular Medicine, Kurashiki Central Hospital, Kurashiki (Y. Kawase); Department of Cardiology, Tenri Hospital, Tenri (C.I., M.M.); Division of Cardiology, Nara Hospital, Kinki University Faculty of Medicine, Ikoma (H.M.); Department of Cardiology, Mitsubishi Kyoto Hospital, Kyoto (M.K.); Department of Cardiology, Kinki University Hospital, Osakasayama (Y.H.); Department of Cardiology, Koto Memorial Hospital, Higashiomi (T. Murakami); Department of Cardiology, Shizuoka General Hospital, Shizuoka (Y.T.); Department of Cardiology, Nishikobe Medical Center, Kobe (K.Y.); Department of Cardiology, Japanese Red Cross Wakayama Medical Center, Wakayama (M.T.); Department of Cardiology, National Hospital Organization Kyoto Medical Center, Kyoto (M. Ishii); Cardiovascular Center, The Tazuke Kofukai Medical Research Institute, Kitano Hospital, Osaka (E.M.-M., T. Kato, M. Inoko); Department of Cardiology, Hikone Municipal Hospital, Hikone (T. Ikeda); Department of Cardiology, Kansai Electric Power Hospital, Osaka (A.K., K.I.); Department of Cardiology, Hyogo Prefectural Amagasaki General Medical Center, Amagasaki (K.H.); Department of Cardiology, Japanese Red Cross Otsu Hospital, Otsu (N.H., T.J.); Department of Cardiology, Saiseikai Noe Hospital, Osaka (Y. Kato); Department of Cardiology, Shiga Medical Center for Adults, Moriyama (Y.I.); Department of Cardiology, Hamamatsu Rosai Hospital, Hamamatsu (C.M.); and Department of Cardiology, Hirakata Kohsai Hospital, Hirakata (Y.M.), Japan) |
 |
Background: Clinical profiles of acute heart failure (AHF) complicating severe aortic stenosis (AS) remain unclear.
Methods and Results: From a Japanese multicenter registry enrolling consecutive patients with severe AS, 3,813 patients were categorized into the 3 groups according to the symptom of heart failure (HF); No HF (n=2,210), chronic HF (CHF) (n=813) and AHF defined as hospitalized HF at enrolment (n=790). Median follow-up was 1,123 days with 93% follow-up rate at 2 years. Risk factors for developing AHF included age, female sex, lower body mass index, untreated coronary artery stenosis, anemia, history of HF, left ventricular ejection fraction <50%, presence of any combined valvular disease, peak aortic jet velocity ≥5 m/s and tricuspid regurgitation pressure gradient ≥40 mmHg, and negative risk factors included dyslipidemia, history of percutaneous coronary intervention and hemodialysis. Respective cumulative 5-year incidences of all-cause death and HF hospitalization in No HF, CHF and AHF groups were 37.1%, 41.8% and 61.8% (P<0.001) and 20.7%, 33.8% and 52.3% (P<0.001). Even in the initial aortic valve replacement (AVR) stratum, AHF was associated with excess 5-year mortality risk relative to No HF and CHF (adjusted hazard ratio [HR] 1.64; 95% confidence interval [CI]: 1.14–2.36, P=0.008; adjusted HR 1.47; 95% CI: 1.03–2.11, P=0.03, respectively).
Conclusions: AHF complicating severe AS was associated with an extremely dismal prognosis, which could not be fully resolved by AVR. Careful management to avoid the development of AHF is crucial.

Cumulative incidences of the primary outcome measures among the AHF, CHF, and No HF groups. (A) All-cause death, and (B) HF hospitalization. Abbreviations as in Figure 1.
(Circ J 2018; 82: 1623–1631)3
| The Unraveled Link Between Antiviral Therapy and Heart Failure Hospitalization in Chronic Hepatitis C Virus Infection ― A Nationwide Cohort Study ― Ming-Shyan Lin, Chang-Min Chung, Ming-Ling Chang, Mei-Yen Chen, Shih-Tai Chang, Pao-Hsien Chu, Tien-Hsing Chen, Wey-Yil Lin, Tung-Jung Huang, Yu-Sheng Lin (Department of Cardiology (M.-S.L.), Department of Pulmonary Disease and Critical Care (T.-J.H.), Chang Gung Memorial Hospital, Yunlin; Department of Cardiology, Heart Failure Center, Chang Gung Memorial Hospital, Chiayi (M.-S.L., C.-M.C., S.-T.C., Y.-S.L.); Liver Research Center and Division of Hepatology, Department of Gastroenterology and Hepatology, Chang Gung Memorial Hospital, Taoyuan (M.-L.C.); College of Nursing & Graduate Institute of Nursing, Chang Gung University of Science and Technology, Chiayi (M.-Y.C.); Department of Nursing (M.-Y.C.), Department of Cardiology, Heart Failure Center, Chang Gung Memorial Hospital, College of Medicine (P.-H.C.), Chang Gung University, Taoyuan; Department of Cardiology, Chang Gung Memorial Hospital, Keelung (T.-H.C.); and Department of Neurology, Landseed Hospital, Taoyuan (W.-Y.L.), Taiwan) |
 |
Background: Although hepatitis C virus (HCV) is a known risk factor for cardiovascular disease, whether antiviral therapy (AVT) can reduce heart failure (HF) hospitalizations is unknown.
Methods and Results: In this population-based cohort study, we used data from the Taiwan National Health Insurance Research Database to evaluate the effect of interferon-based therapy (IBT) on cardiovascular events in patients with chronic HCV infection. Clinical outcomes evaluated included HF hospitalizations; a composite of acute myocardial infarction, ischemic stroke, and peripheral artery disease; all-cause death; and cardiovascular death. Of 83,229 eligible patients with chronic HCV infection, we compared 16,284 patients who received IBT with untreated subjects after propensity score matching. Patients who received IBT were less likely to be hospitalized for HF compared with untreated subjects (incidence density.ID, 0.9 vs. 1.5 events per 103 person-years; hazard ratio.HR, 0.58; 95% confidence interval.CI, 0.42–0.79; P=0.001). Compared with untreated subjects, the treated group had significantly lower risk of composite vascular events (ID, 3.7 vs. 5.0 events per 103 person-years; P<0.001), all-cause death (ID, 5.6 vs. 17.2 events per 103 person-years; P<0.001), and cardiovascular death (ID, 0.2 vs. 0.6 events per 103 person-years; P=0.001).
Conclusions: AVT for chronic HCV infection might offer protection against HF hospitalizations, critical vascular events, and cardiovascular death beyond known beneficial effects.

Incidence densities of heart failure hospitalizations (A) and composite vascular events (B) between treated and untreated groups after 1:2 matching.
(Circ J 2018; 82: 2707–2714)4
| Clinical Manifestations and Long-Term Mortality in Lamin A/C Mutation Carriers From a Japanese Multicenter Registry Kenzaburo Nakajima, Takeshi Aiba, Takeru Makiyama, Suguru Nishiuchi, Seiko Ohno, Koichi Kato, Yuta Yamamoto, Takahiro Doi, Satoshi Shizuta, Kenji Onoue, Nobue Yagihara, Taisuke Ishikawa, Ichiro Watanabe, Hiroshi Kawakami, Yasushi Oginosawa, Nobuyuki Murakoshi, Akihiko Nogami, Kazutaka Aonuma, Yoshihiko Saito, Takeshi Kimura, Satoshi Yasuda, Naomasa Makita, Wataru Shimizu, Minoru Horie, Kengo Kusano (Department of Cardiovascular Medicine (K.N., T.A., S.Y., K. Kusano), Department of Advanced Arrhythmia and Translational Medical Science (T.A.), National Cerebral and Cardiovascular Center, Suita; Department of Advanced Cardiovascular Medicine, Graduate School of Medical Sciences Kumamoto University, Kumamoto (K.N., S.Y., K. Kusano); Department of Cardiovascular Medicine, Kyoto University Graduate School of Medicine, Kyoto (T.M., S.N., Y.Y., T.D., S.S., T.K.); Department of Cardiovascular and Respiratory Medicine, Shiga University of Medical Science, Otsu (S.O., K. Kato, M.H.); Department of Cardiovascular Medicine, Nara Medical University, Kashihara (K.O., Y.S.); Department of Cardiovascular Biology and Medicine, Niigata University Graduate School of Medical and Dental Sciences, Niigata (N.Y.); Department of Molecular Physiology, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki (T.I., N. Makita); Division of Cardiology, Department of Medicine, Nihon University School of Medicine, Tokyo (I.W.); Department of Cardiology, Pulmonology, Hypertension and Nephrology, Ehime University Graduate School of Medicine, Toon (H.K.); The Second Department of Internal Medicine, University of Occupational and Environmental Health, Kitakyushu (Y.O.); Cardiovascular Division, Faculty of Medicine, University of Tsukuba, Tsukuba (N. Murakoshi, A.N., K.A.); and Department of Cardiovascular Medicine, Nippon Medical School, Tokyo (W.S), Japan) |
 |
Background: Mutation in the lamin A/C gene (LMNA) is associated with several cardiac phenotypes, such as cardiac conduction disorders (CCD), atrial arrhythmia (AA), malignant ventricular arrhythmia (MVA) and left ventricular dysfunction (LVD), leading to sudden cardiac death (SCD) and/or end-stage heart failure. We investigated how these phenotypes are associated with each other and which of them are most important for total mortality.
Methods and Results: A multicenter registry included 110 LMNA mutation carriers (age, 43±15 years, male: 62%) from 60 families. After genetic diagnosis of LMNA mutation (missense: 27%, non-missense: 73%), patients or subjects were followed to evaluate the manifestations of their phenotypes and the risk of total mortality; 90 patients could be followed (median: 5 [0–35] years). Prevalence of the 4 clinical phenotypes was significantly increased during follow-up. Among these phenotypes, AA was significantly associated with MVA. CCD was significantly associated with LVD. LVD, meanwhile, was significantly associated with CCD and MVA. Male sex was significantly associated with MVA. Furthermore, during follow-up, 17 patients died: 12 end-stage heart failure, 4 SCD and 1 stroke. LVD was the only independent predictor for all-cause death (OR: 41.7, 95% CI: 4.1–422.3; P=0.0016).
Conclusions: Several cardiac phenotypes were age-dependently increased in LMNA mutation carriers, suggesting that ICD or CRT-D could suppress SCD after middle age; however, LVD leading to end-stage heart failure was the only independent predictor for total mortality.
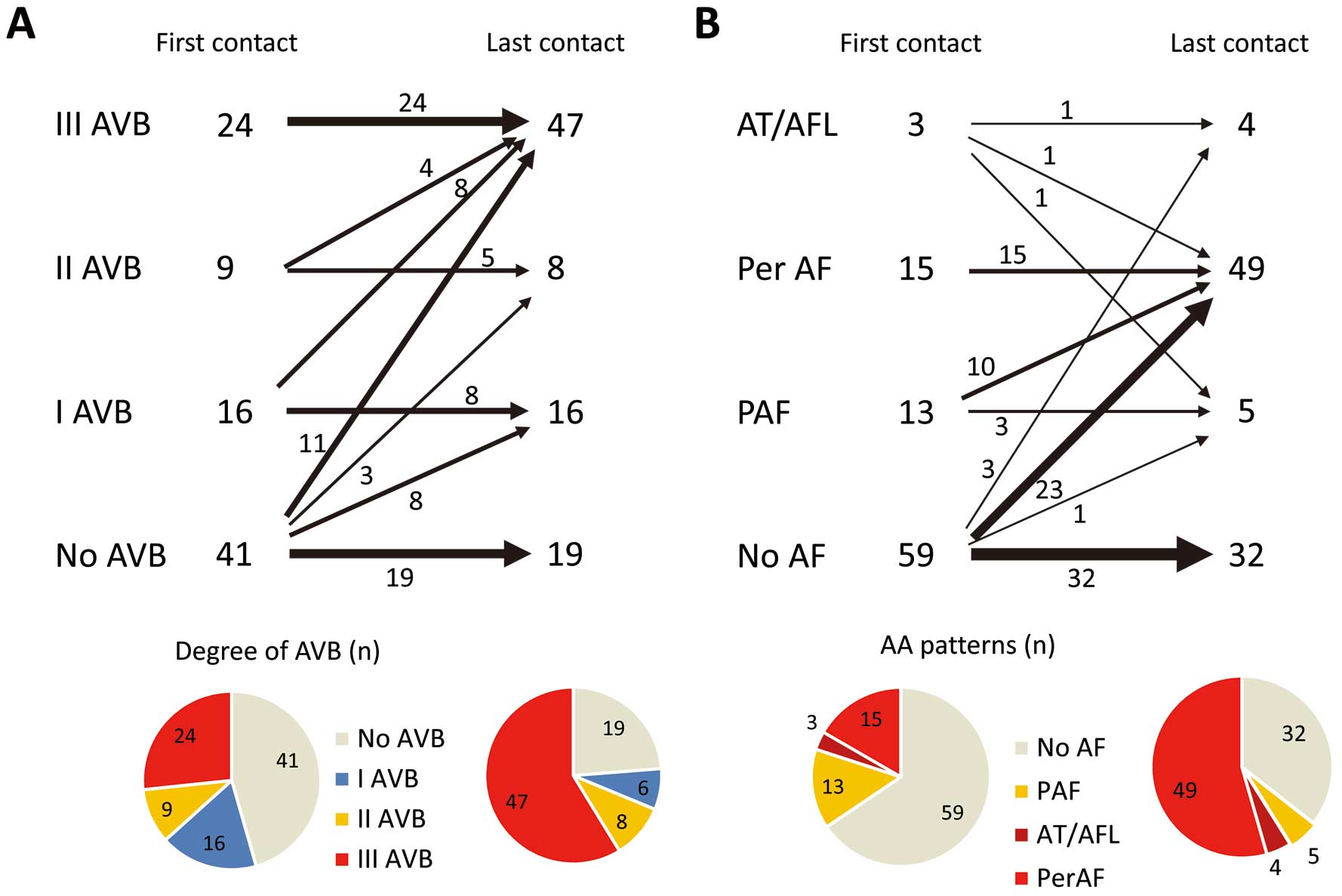
(A) Serial change in the severity of AVB and (B) change in AA pattern during follow-up of LMNA mutation carriers (n=90). AA, atrial arrhythmias; AVB, atrioventricular block; AT, atrial tachycardia; AFL, atrial flutter; PAF, paroxysmal atrial fibrillation; Per AF, persistent atrial fibrillation.
(Circ J 2018; 82: 2485–2492)5
| Activation of the AKT Pathway in the Ascending Aorta With Bicuspid Aortic Valve Yuichiro Hirata, Hiroki Aoki, Takahiro Shojima, Kazuyoshi Takagi, Tohru Takaseya, Kohji Akasu, Satoru Tobinaga, Yoshihiro Fukumoto, Hiroyuki Tanaka (Division of Cardiovascular Surgery, Department of Surgery (Y.H., T.S., K.T., T.T., K.A., S.T., H.T.), Division of Cardiovascular Medicine, Department of Internal Medicine (Y.F.), Kurume University School of Medicine, Kurume; Cardiovascular Research Institute, Kurume University, Kurume (H.A.), Japan) |
 |
Background: Dilatation of the ascending aorta affects those patients with bicuspid aortic valve (BAV), even after valvular surgery, possibly due to tissue fragility. The goal of the study was the molecular characterization of aorta with BAV compared to that with normal tricuspid aortic valve (TAV).
Methods and Results: The subjects were patients who underwent surgery for aortic valve stenosis in 2013 and 2014. Nine patients with BAV and 13 with TAV were examined. There was no difference in the clinical characteristics or grade of aortic valve stenosis, but the diameters of the ascending aorta were significantly higher in the BAV group. The ascending aortic specimens were subjected to transcriptome analyses, which revealed the changes in receptor tyrosine kinase (RTK) pathway-related genes between TAV and BAV samples. Immunohistochemical study revealed higher staining of phosphorylated AKT (pAKT) in the media of the ascending aorta in the BAV group, regardless of the size of ascending aorta, whereas total AKT did not show such a difference. Immunofluorescence staining revealed the AKT activation was mainly in the medial vascular smooth muscle cells.
Conclusions: The results showed that the RTK-AKT pathway in the medial layer of the ascending aorta is activated in aortae with BAV. Activation of this pathway may be associated with fragility and dilatation of the ascending aorta with BAV.
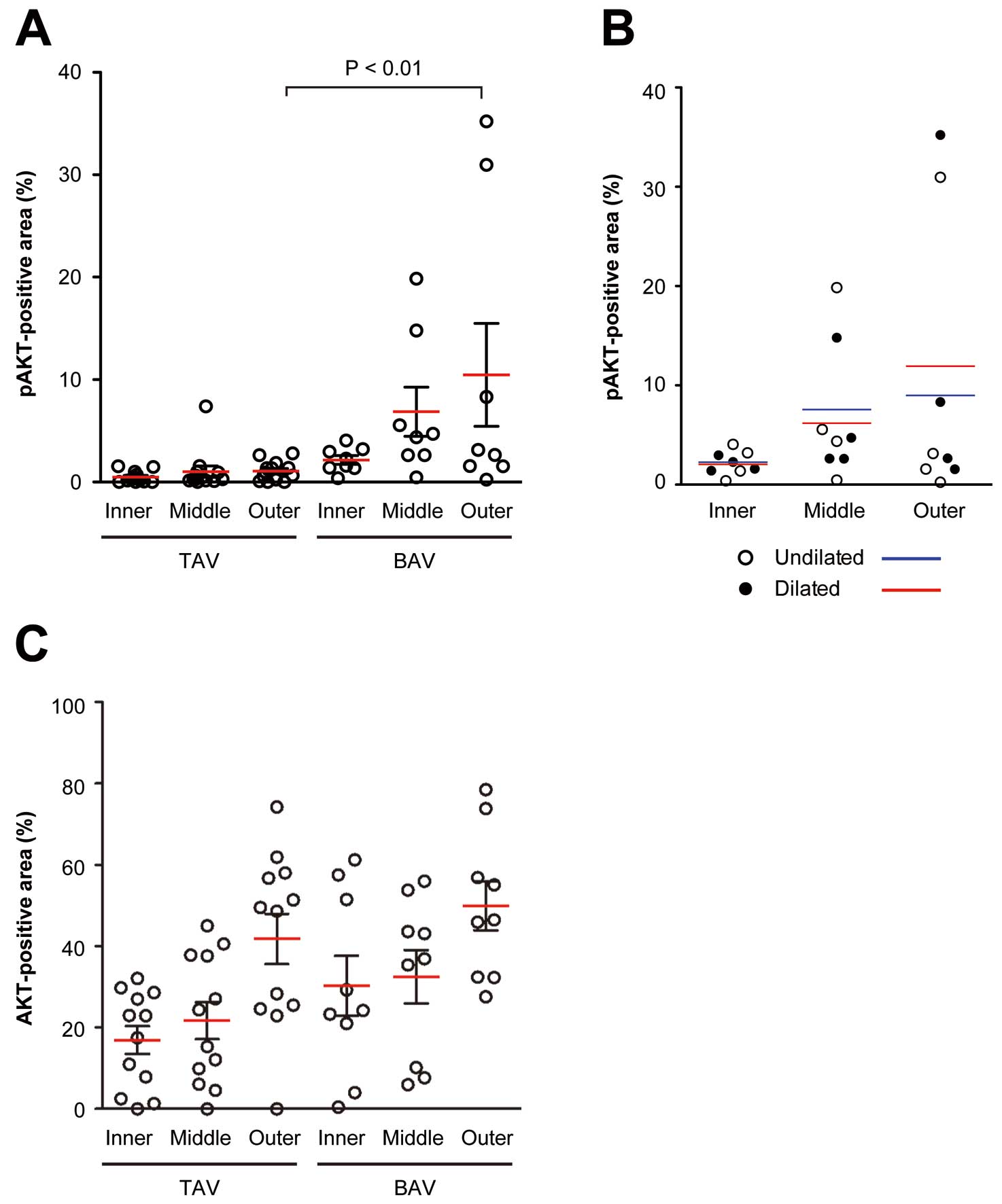
pAKT-positive area in the aortic wall samples. (A) The graph shows the pAKT-positive area in the inner, middle, and outer zones of the medial layer in the aortic samples with tricuspid aortic valve (TAV) and bicuspid aortic valve (BAV). Red and black bars indicate means and standard errors respectively. (B) The graph shows the pAKT-positive area in the inner, middle, and outer zones of the medial layer in the aortic samples with BAV. Open symbols and blue bars indicate individual data and means respectively, for samples without ascending aorta dilation. Closed symbols and red bars indicate those samples with ascending aorta dilation, as defined by the diameters of more than 45 mm. (C) The graph shows the AKT-positive area in the inner, middle, and outer zones of the medial layer in the aortic samples with TAV and BAV. Red and black bars indicate means and standard errors respectively.
(Circ J 2018; 82: 2861–2871)6
| MicroRNA-377 Inhibits Atherosclerosis by Regulating Triglyceride Metabolism Through the DNA Methyltransferase 1 in Apolipoprotein E-Knockout Mice Ling-Yan Chen, Xiao-Dan Xia, Zhen-Wang Zhao, Duo Gong, Xiao-Feng Ma, Xiao-Hua Yu, Qiang Zhang, Si-Qi Wang, Xiao-Yan Dai, Xi-Long Zheng, Da-Wei Zhang, Wei-Dong Yin, Chao-Ke Tang (Institute of Cardiovascular Research, Key Laboratory for Atherosclerology of Hunan Province, Medical Research Center, Hunan Province Cooperative Innovation Center for Molecular Target New Drug Study (L.-Y.C., X.-D.X., Z.-W.Z., D.G., X.-H.Y., Q.Z, S.-Q.W., W.-D.Y, C.-K.T.), Department of Internal Medicine-Cardiovascular, Nanhua Hospital (X.-F.M.), University of South China, Hengyang, Hunan; Key Laboratory of Molecular Target & Clinical Pharmacology, School of Pharmaceutical Sciences & the Fifth Affiliated Hospital, Guangzhou, Medical University, Guangzhou (X.-Y.D.), China; Department of Biochemistry and Molecular Biology, Libin Cardiovascular Institute of Alberta, Cumming School of Medicine, University of Calgary, Health Sciences Center, Calgary, Alberta (X.-L.Z.); and Department of Pediatrics and Group on the Molecular and Cell Biology of Lipids, University of Alberta, Alberta (D.-W.Z.), Canada) |
Background: Lipoprotein lipase (LPL) plays an important role in triglyceride metabolism. It is translocated across endothelial cells to reach the luminal surface of capillaries by glycosylphosphatidylinositol-anchored high-density lipoprotein binding protein 1 (GPIHBP1), where it hydrolyzes triglycerides in lipoproteins. MicroRNA 377 (miR-377) is highly associated with lipid levels. However, how miR-377 regulates triglyceride metabolism and whether it is involved in the development of atherosclerosis remain largely unexplored.
Methods and Results: The clinical examination displayed that miR-377 expression was markedly lower in plasma from patients with hypertriglyceridemia compared with non-hypertriglyceridemic subjects. Bioinformatics analyses and a luciferase reporter assay showed that DNA methyltransferase 1 (DNMT1) was a target gene of miR-377. Moreover, miR-377 increased LPL binding to GPIHBP1 by directly targeting DNMT1 in human umbilical vein endothelial cells (HUVECs) and apolipoprotein E (ApoE)-knockout (KO) mice aorta endothelial cells (MAECs). In vivo, hematoxylin-eosin (H&E), Oil Red O and Masson’s trichrome staining showed that ApoE-KO mice treated with miR-377 developed less atherosclerotic plaques, accompanied by reduced plasma triglyceride levels.
Conclusions: It is concluded that miR-377 upregulates GPIHBP1 expression, increases the LPL binding to GPIHBP1, and reduces plasma triglyceride levels, likely through targeting DNMT1, inhibiting atherosclerosis in ApoE-KO mice.
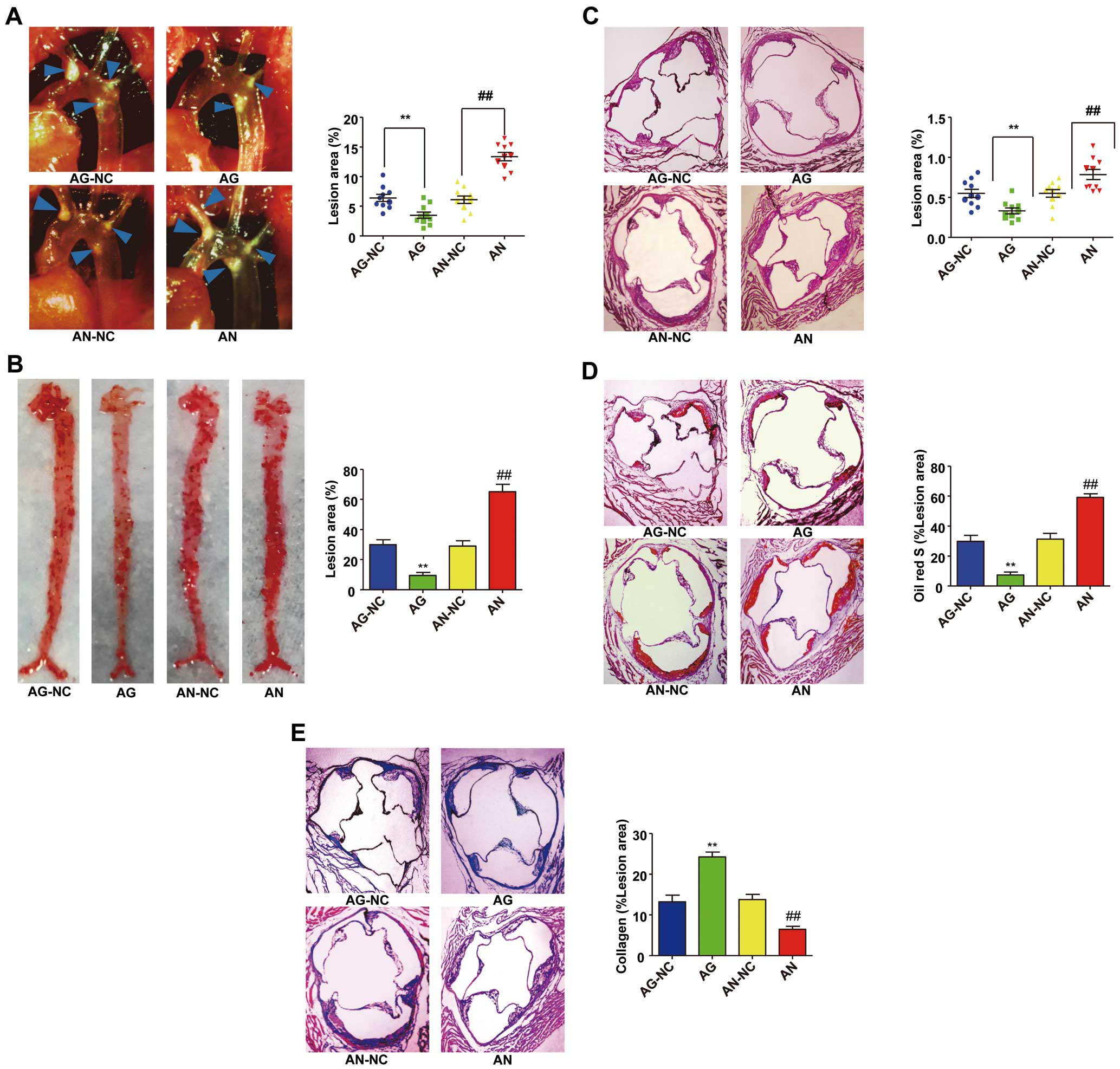
MicroRNA-377 (miR-377) ameliorates the development of atherosclerosis. Atherosclerotic lesions were examined in 12-week-old apolipoprotein E (ApoE)-knockout (KO) mice that were treated with miR-377 agomir negative control (AG-NC), miR-377 agomir (AG), miR-377 antagomir negative control (AN-NC), or miR-377 antagomir (AN) through tail vein injections. ApoE-KO mice were fed with high fat/high cholesterol diet. (A) Representative images of plaques (blue arrows) in aortic arches and thoracic aortas of ApoE-KO mice. (B) Representative images and quantification of atherosclerotic lesion areas in the en face analysis of the entire aorta with Oil Red O staining. (C) Representative micrographs of hematoxylin-eosin staining in the aortic sinus. (D) Characterization of aortic sinus in atherosclerotic lesion areas by Oil Red O staining. (E) Representative microscopic images and quantification of atherosclerotic plaque collagen content in the aortic sinus by Masson’s trichrome staining. Representative images of sections from each group are accompanied by graphs summarizing the data. (Original magnification×104 [C–E]). Data are presented as the mean±SEM, n=10. **P<0.01 vs. AG-NC and ##P<0.01 vs. AN-NC.
(Circ J 2018; 82: 739–746)7
| Increased Prognostic Value of Query Amyloid Late Enhancement Score in Light-Chain Cardiac Amyloidosis Ke Wan*, Jiayu Sun, Yuchi Han, Hong Liu, Dan Yang, Weihao Li, Jie Wang, Wei Cheng, Qing Zhang, Zhi Zeng, Yucheng Chen (Department of Cardiology (K.W., H.L., D.Y., W.L., J.W., Q.Z., Z.Z., Y.C.), Department of Radiology (J.S., W.C.), West China Hospital, Sichuan University, Chengdu, Sichuan Province, China; Department of Medicine (Cardiovascular Division), University of Pennsylvania, Philadelphia, PA (Y.H.), USA) *Current affiliation: Department of Geriatrics, West China Hospital, Sichuan University, Chengdu, Sichuan Province, China |
 |
Background: Late gadolinium enhancement (LGE) pattern is a powerful imaging biomarker for prognosis of cardiac amyloidosis. It is unknown if the query amyloid late enhancement (QALE) score in light-chain (AL) amyloidosis could provide increased prognostic value compared with LGE pattern.
Methods and Results: Seventy-eight consecutive patients with AL amyloidosis underwent contrast-enhanced cardiovascular magnetic resonance imaging. Patients with cardiac involvement were grouped by LGE pattern and analyzed using QALE score. Receiver operating characteristic curve was used to identify the optimal cut-off for QALE score in predicting all-cause mortality. Survival of these patients was analyzed with the Kaplan-Meier method and multivariate Cox regression. During a median follow-up of 34 months, 53 of 78 patients died. The optimal cut-off for QALE score to predict mortality at 12-month follow-up was 9.0. On multivariate Cox analysis, QALE score ≥9 (HR, 5.997; 95% CI: 2.665–13.497; P<0.001) and log N-terminal pro-brain natriuretic peptide (HR, 1.525; 95% CI: 1.112–2.092; P=0.009) were the only 2 independent predictors of all-cause mortality. On Kaplan-Meier analysis, patients with subendocardial LGE can be further risk stratified using QALE score ≥9.
Conclusions: The QALE scoring system provides powerful independent prognostic value in AL cardiac amyloidosis. QALE score ≥9 has added value to differentiate prognosis in AL amyloidosis patients with a subendocardial LGE pattern.
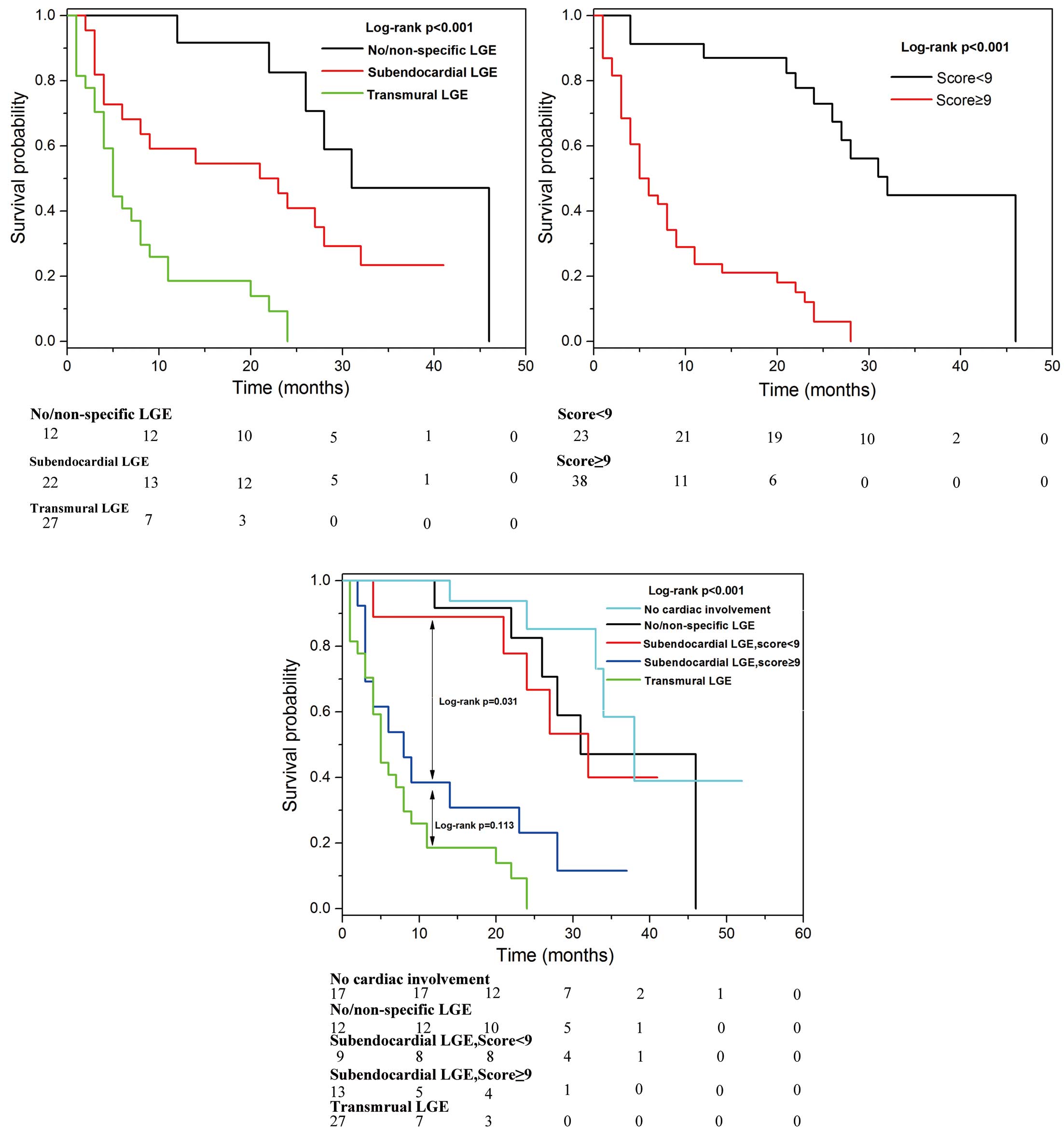
Survival curves according to (A) cardiac involvement in amyloid light-chain amyloidosis (P<0.001); (B) query amyloid late enhancement (QALE) score (P<0.001); and (C) cardiac involvement combined with QALE score (P<0.001).
Awards will be presented to the 7 research groups during the 83rd Annual Scientific Meeting of the Japanese Circulation Society, and will also be announced on the Society website. We look forward to receiving manuscripts with high scientific impact for publication in Circulation Journal in 2019.