Abstract
Background:
We sought to explore the effects of previous heart failure (HF) hospitalization on mortality in patients hospitalized for acute decompensated HF (ADHF) in a large Japanese contemporary observational database.
Methods and Results:
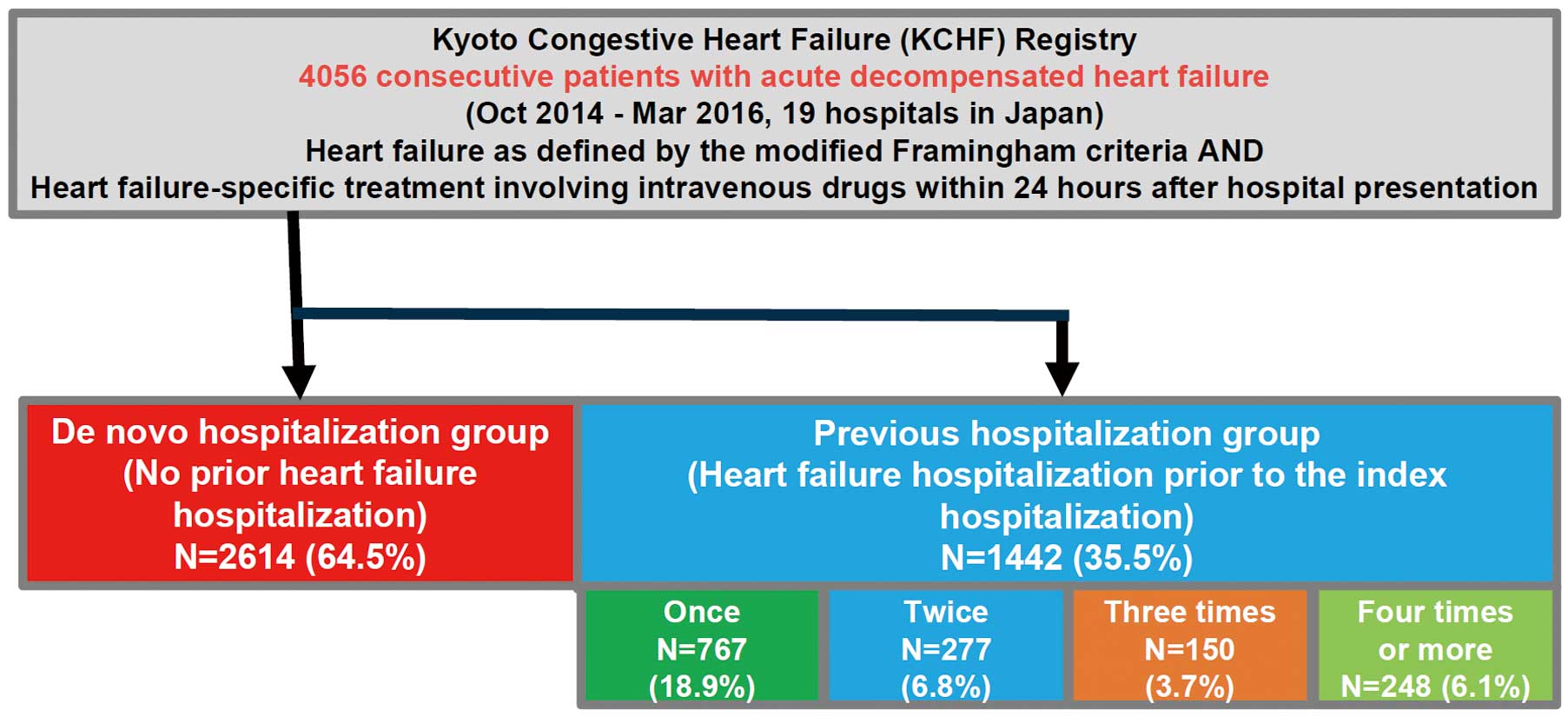
We prospectively enrolled consecutive patients with ADHF in 19 participating hospitals between October 2014 and March 2016. Of 4,056 patients, 1,442 patients (35.4%) had at least 1 previous HF hospitalization (previous hospitalization group), while 2,614 patients (64.5%) did not have a history of HF hospitalization (de novo hospitalization group). Patients with previous hospitalization were older and more often had comorbidities such as anemia, and renal failure than those without. The cumulative 1-year incidence of all-cause death was significantly higher in the previous hospitalization group than in the de novo hospitalization group (28% vs. 19%, P<0.001). After adjusting confounders, the excess risk of the previous hospitalization group relative to the de novo hospitalization group for all-cause death remained significant (HR, 1.28; 95% CI: 1.10–1.50, P=0.001). The excess risk was significant in patients without advanced age, anemia, or renal failure, but not significant in patients with these comorbidities, with significant interaction. Increase in the number of hospitalizations was associated with an increased risk for mortality.
Conclusions:
In a contemporary ADHF cohort in Japan, repeated hospitalization was associated with an increasing, higher risk for 1-year mortality.
Acute decompensated heart failure (ADHF) might be recognized as a “multi-event disease” with a high morbidity, mortality, and social burden.1,2
The natural history of heart failure (HF) included multiple occurrences of decompensated failure both symptomatically and hemodynamically, finally leading to death.3
Observational studies or subanalyses in randomized trial settings from the late 1990 s to the early 2000 s illustrated the impact of previous hospitalization on long-term mortality in patients hospitalized for HF in Western countries.4–6
Rapid relief of symptoms, however, could be achieved once volume overload and/or excessive afterload were managed successfully in the acute decompensated phase. In addition, the recent advances in the management of HF and optimal guideline-recommended therapies often led clinicians to misunderstand that the patients have returned to their compensated state and some of these patients would tolerate repeated admissions; these patients were called “frequent flyers”.7
The aim of the current study was to explore the effects of previous HF hospitalization on mortality in patients hospitalized for ADHF in a large Japanese contemporary observational database.
Methods
The Kyoto Congestive Heart Failure (KCHF) registry is a physician-initiated, prospective, observational, multicenter cohort study that enrolled consecutive patients hospitalized due to ADHF for the first time between October 2014 and March 2016 in 19 secondary and tertiary hospitals, including rural and urban areas, and large and small hospitals, in Japan. The details of the design and patient enrolment in the KCHF registry have been described previously.8,9
Briefly, we enrolled patients with ADHF as defined by the modified Framingham criteria who were admitted to the participating centers, and those who underwent HF-specific treatment requiring i.v. drugs ≤24 h after presenting to hospital. We did not exclude those patients with ADHF associated with acute coronary syndrome (ACS). We collected not only the medical and laboratory data, but also the social and economic data. The study protocol was approved by the institutional review board of each participating center. Patient records were anonymized prior to analysis. A waiver of written informed consent from each patient was approved, because it was allowed in the Japanese ethics guidelines for epidemiological studies.10
Clinical follow-up data at 1 year were collected in October 2017. No patients refused to participate in the study when contacted for follow-up. The attending physicians or research assistants at each participating hospital collected the data for clinical events after the index hospitalization from the hospital charts, or by contacting patients, their relatives, and/or their referring physicians. In the present analysis, we sought to compare the clinical outcomes between patients with or without a previous history of HF hospitalization at the time of the index hospitalization for ADHF (Figure 1).
The primary outcome measure in the current analysis was all-cause death after the index admission for ADHF. We used the laboratory data at the time of the index admission. Renal failure was defined as estimated glomerular filtration rate (eGFR) <30 mL/min/1.73 m2
based on the chronic kidney disease grades. Anemia was defined using the World Health Organization criteria (hemoglobin <12.0 g/dL in women and <13.0 g/dL in men). Physical activity before admission was classified by mobility status based on the definition of Japanese long-term care insurance into ambulatory (including those patients using any aid such as a stick), use of wheelchair (outdoor only and indoor and outdoor), and bed-ridden state.8,9
Public financial assistance was defined as the public assistance system provided by the Japanese Government.11
Patients with occupation were defined as those who were in a job or profession. Medical adherence was a dichotomous rating based on the self-report by patients or family members and reports by clinicians without rigorous quantitative definitions.12,13
Statistical Analysis
Categorical variables are presented as n (%), and were compared using the chi-squared test. Continuous variables are expressed as mean±SD or median (IQR), and were compared using the Student’s t-test when normally distributed or Wilcoxon rank-sum test when not normally distributed. Cumulative incidences were estimated using the Kaplan-Meier method and compared using the log-rank test. We regarded the date of admission as time zero for clinical follow-up. We compared baseline characteristics and mortality on the basis of the presence or absence of a previous HF hospitalization. We estimated the effects of previous HF hospitalization relative to no previous HF hospitalization for all-cause death as hazard ratios (HR) with 95% CI on multivariable Cox proportional hazard modeling. To adjust for the confounders, we simultaneously included previous HF hospitalization together with the 25 clinically relevant risk-adjusting variables in the multivariable Cox proportional hazards models in the entire cohort and in the subgroups (Table 1), after proportional hazard assumptions were assessed on the plots of log (time) vs. log [−log (survival)] stratified by the variables and were verified to be acceptable. For the multivariable analyses, continuous variables were dichotomized using clinically meaningful reference values or medians: age >80 years based on the median; left ventricular ejection fraction (LVEF) <40%; body mass index (BMI) ≤22 kg/m2; eGFR <30 mL/min/1.73 m2; decreased albumin (serum albumin <3.0 g/dL); and hyponatremia (serum sodium <135 mEq/L) according to the previous study.14
Post-hoc subgroup analyses were conducted as stratified by age, LVEF, prior myocardial infarction (MI), anemia, and renal failure.
Table 1.
ADHF Patient Characteristics
| Variables |
Previous hospitalization group
(n=1,442, 35.5%) |
De novo hospitalization group
(n=2,614, 64.5%) |
P-value |
| Clinical characteristics |
| Age (years) |
81 (74–86) |
80 (71–86) |
0.001 |
| Age >80 years† |
821 (56.9) |
1,326 (50.7) |
<0.001 |
| Men† |
787 (54.6) |
1,451 (55.5) |
0.58 |
| BMI (kg/m2) |
22.5 (20.0–25.2) |
21.8 (19.6–24.8) |
<0.001 |
| BMI <22 kg/m2 † |
718 (51.5) |
1,069 (43.9) |
<0.001 |
| Etiology |
|
|
<0.001 |
| Cardiomyopathy |
250 (17.3) |
358 (13.7) |
|
| Dilated cardiomyopathy |
171 (11.9) |
263 (10.1) |
|
| Valvular heart disease |
313 (21.7) |
506 (19.3) |
|
| Hypertensive |
289 (20.0) |
696 (26.6) |
|
| Ischemic |
492 (34.1) |
835 (32.0) |
|
| Associated with ACS† |
33 (2.3) |
206 (7.9) |
|
| Not associated with ACS |
459 (31.8) |
629 (24.1) |
|
| Arrhythmia-related |
40 (2.7) |
148 (5.7) |
|
| Others |
58 (4.0) |
71 (4.0) |
|
| Medical history |
| AF or Afl† |
756 (52.4) |
925 (35.4) |
<0.001 |
| Hypertension† |
1,009 (70.0) |
1,900 (72.7) |
0.07 |
| DM† |
599 (41.5) |
911 (34.9) |
<0.001 |
| Dyslipidemia |
625 (43.3) |
924 (35.4) |
<0.001 |
| Prior MI† |
441 (30.6) |
467 (17.9) |
<0.001 |
| Prior stroke† |
245 (17.0) |
417 (16.0) |
0.40 |
| Prior PCI or CABG |
535 (37.1) |
485 (18.6) |
<0.001 |
| Current smoking† |
130 (9.2) |
346 (13.5) |
<0.001 |
| VT/VF |
109 (7.6) |
56 (2.1) |
<0.001 |
| Chronic lung disease† |
214 (14.8) |
322 (12.3) |
0.03 |
| Liver cirrhosis |
16 (1.1) |
39 (1.5) |
0.40 |
| Malignancy |
220 (15.3) |
365 (14.0) |
0.26 |
| Dementia |
294 (20.4) |
476 (18.2) |
0.09 |
| Social backgrounds |
| Poor medical adherence |
273 (18.9) |
401 (15.3) |
0.004 |
| Living alone† |
295 (20.5) |
571 (21.8) |
0.32 |
| Employed |
121 (8.4) |
389 (14.9) |
<0.001 |
| Public financial assistance |
103 (7.1) |
131 (5.0) |
0.006 |
| Daily life activities |
| Ambulatory† |
1,068 (74.9) |
2,081 (80.4) |
<0.001 |
| Use of wheelchair (outdoor only) |
138 (9.7) |
167 (6.5) |
<0.001 |
| Use of wheelchair (outdoor and indoor) |
165 (11.6) |
223 (8.6) |
0.003 |
| Bedridden |
55 (3.9) |
117 (4.5) |
0.33 |
| Vital signs at presentation |
| SBP (mmHg) |
142±34 |
150±36 |
<0.001 |
| SBP <90 mmHg† |
55 (3.8) |
71 (2.7) |
0.06 |
| Heart rate (beats/min) |
92±25 |
98±29 |
<0.001 |
| Heart rate <60 beats/min† |
72 (5.0) |
193 (7.4) |
0.003 |
| NYHA class III or IV |
1,267 (88.3) |
2,270 (87.3) |
0.37 |
| Tests at admission |
| LVEF (%) |
45.0±16.7 |
46.6±16.0 |
0.005 |
| LVEF <40%† |
597 (41.5) |
954 (36.7) |
0.002 |
| BNP (pg/mL) |
757 (445–1,334) |
696 (380–1,289) |
0.008 |
| Serum creatinine (mg/dL) |
1.31 (0.97–1.92) |
1.02 (0.79–1.47) |
<0.001 |
| eGFR <30 mL/min/1.73 m2 † |
548 (38.1) |
570 (21.9) |
<0.001 |
| BUN (mg/dL) |
29 (20–43) |
22 (17–32) |
<0.001 |
| Sodium <135 mEq/L† |
198 (13.8) |
321 (12.3) |
0.20 |
| Anemia†,‡ |
1,078 (74.8) |
1,627 (62.4) |
<0.001 |
| Albumin <3.0 g/dL† |
188 (13.5) |
379 (14.9) |
0.24 |
| Medication at admission |
| ACEI or ARB† |
750 (52.0) |
1,100 (42.1) |
<0.001 |
| β-blocker† |
840 (58.3) |
720 (27.5) |
<0.001 |
| MRA† |
434 (30.1) |
299 (11.4) |
<0.001 |
| Loop diuretics† |
1,123 (77.9) |
853 (32.6) |
<0.001 |
| Tolvaptan† |
139 (9.6) |
31 (1.2) |
<0.001 |
| Length of hospital stay (days) |
16 (11–26) |
16 (11–24) |
0.85 |
Data given as mean±SD, median (IQR) or n (%). †25 risk-adjusting variables selected for multivariable Cox proportional hazard modeling. ‡Defined using the World Health Organization criteria (hemoglobin <12.0 g/dL in women and <13.0 g/dL in men). ACEI, angiotensin-converting enzyme inhibitor; ACS, acute coronary syndrome; ADHF, acute decompensated heart failure; AF, atrial fibrillation; AFl, atrial flutter; ARB, angiotensin receptor blocker; BMI, body mass index; BNP, brain-type natriuretic peptide; BP, blood pressure; BUN, blood urea nitrogen; CABG, coronary artery bypass graft; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; LVEF, left ventricular ejection fraction; MI, myocardial infarction; MRA, mineralocorticoid receptor antagonist; NYHA, New York Heart Association; PCI, percutaneous coronary intervention; SBP, systolic blood pressure; VT/VF, ventricular tachycardia/fibrillation.
We further explored the effects of the number of previous HF hospitalizations on clinical outcome. Patients were divided into 5 groups on the basis of the number of previous HF hospitalizations: none, once, twice, three times, and four times or more, according to a previous study.5
Comparison of the 5 groups was performed using the chi-squared test for categorical variables and one-way analysis of variance in addition to the Cochran-Armitage trend test in order to assess the trend across the 5 groups. After proportional hazard assumptions for the 5 groups were assessed on the plots of log (time) vs. log [−log (survival)] stratified by the variables and were verified to be acceptable, we used a multivariable Cox proportional hazard model including the number of prior HF hospitalizations as a continuous variable to estimate the impact on the primary outcome measure.
In additional analysis where we regarded the date of discharge as time zero for clinical follow-up, we further explored the effects of the number of previous HF hospitalizations on mortality in 3,728 patients discharged alive and with available follow-up data (Supplementary Figure 1). To adjust for the confounders, we included the aforementioned clinically relevant risk-adjusting variables and medication at discharge14
instead of medication at admission in the multivariable Cox proportional hazards models (Supplementary Table 1).
All statistical analyses were conducted by physicians (K.S. and T. Kato) and a statistician (T. Morimoto) using JMP 14.0 or SAS 9.4 (both SAS Institute, Cary, NC, USA). Two-tailed P<0.05 was considered statistically significant.
Results
Patient Characteristics
Of the 4,065 study patients (median age, 80 years; IQR, 72–86 years; men, 55%; ischemic etiology, 33%; LVEF <40%, 38%), 1,442 patients (35.4%) had at least 1 previous HF hospitalization (previous hospitalization group), while 2,614 patients (64.5%) did not have a history of HF hospitalization (de novo hospitalization group;
Figure 1). Patients in the previous hospitalization group were older, and more often had a smaller BMI, diabetes mellitus, prior MI, atrial fibrillation or flutter, and ventricular arrhythmias than those in the de novo hospitalization group (Table 1). Patients in the prior hospitalization group less often had hypertension and ACS as the underlying heart disease, and less often were current smokers, and ambulatory. Regarding social background, patients with previous hospitalization more often had poor medical adherence and received public financial assistance, and less often were employed. Patients with prior hospitalization had lower systolic blood pressure, and lower LVEF, and more often had renal dysfunction, anemia, and higher brain natriuretic peptide than those without prior hospitalization (Table 1).
Clinical Outcomes
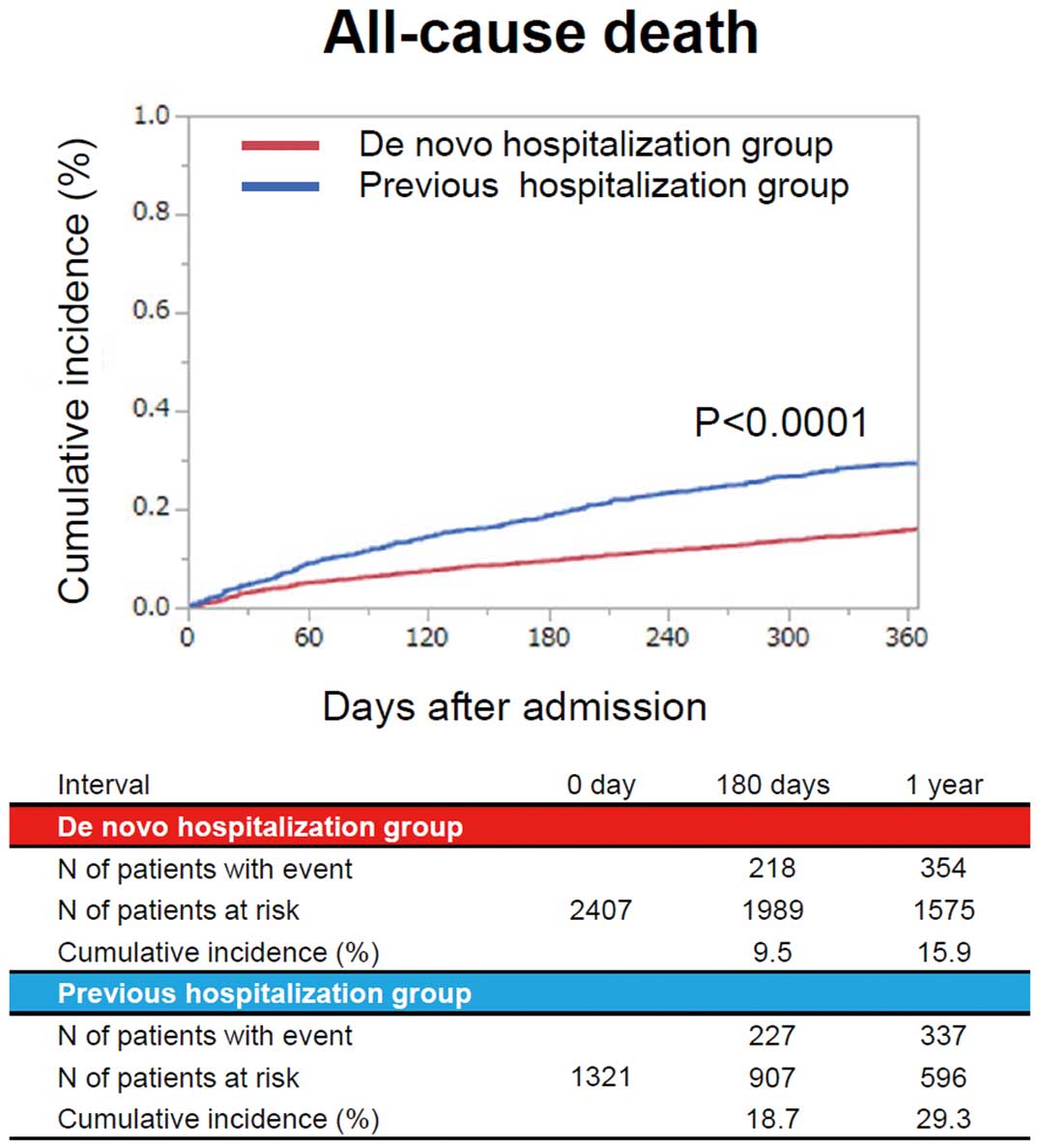
Follow-up rate at 1 year was 94%. The cumulative 1-year incidence of all-cause death was significantly higher in the previous hospitalization group than in the de novo hospitalization group (28% vs. 19%, P<0.001;
Figure 2). After adjusting for confounders, the excess risk of the previous hospitalization group relative to the de novo hospitalization group for all-cause death remained significant (HR, 1.28; 95% CI: 1.10–1.50, P=0.001;
Table 2).
Table 2.
Primary and Secondary Outcomes in ADHF Patients
| |
Previous
hospitalization
group |
De novo
hospitalization
group |
Unadjusted HR
(95% CI) |
P-value |
Adjusted HR
(95% CI) |
P-value |
No. patients with event/no. patients at risk
(cumulative 1-year incidence, %) |
| All-cause death |
495/1,442 (27.9) |
628/2,614 (18.5) |
1.52 (1.35–1.71) |
<0.001 |
1.28 (1.10–1.50) |
0.001 |
ADHF, acute decompensated heart failure; CI, confidence interval; HR, hazard ratio.
On subgroup analyses, the excess risk of the previous hospitalization group relative to the de novo hospitalization group for all-cause death was significant in patients ≤80 years of age, patients without anemia, and patients without renal failure, but not significant in patients >80 years of age, patients with anemia, and patients with renal failure, with significant interaction. There was no interaction between the subgroup factors LVEF, diabetes, prior MI, and atrial fibrillation, and the effect of previous hospitalization relative to de novo hospitalization for all-cause death (Table 3).
Table 3.
Subgroup Analysis for All-Cause Death in ADHF Patients
| |
Previous
hospitalization
group |
De novo
hospitalization
group |
Unadjusted |
Adjusted |
No. patients with event/no.
patients at risk (cumulative
1-year incidence, %) |
HR
(95% CI) |
P-value |
HR
(95% CI) |
P-value |
P-value for
interaction |
| Age |
| >80 years |
342/821
(33.9) |
458/1,326
(26.3) |
1.27
(1.11–1.47) |
<0.001 |
1.14
(0.94–1.37) |
0.16 |
0.005 |
| ≤80 years |
153/621
(20.0) |
170/1,288
(10.7) |
1.95
(1.57–2.43) |
<0.001 |
1.73
(1.29–2.31) |
<0.001 |
| LVEF |
| LVEF <40% |
212/597
(31.8) |
228/954
(19.6) |
1.58
(1.31–1.91) |
<0.001 |
1.98
(1.58–2.47) |
<0.001 |
0.49 |
| LVEF ≥40% |
280/841
(25.3) |
395/1,649
(17.8) |
1.46
(1.25–1.70) |
<0.001 |
1.41
(1.08–1.86) |
<0.001 |
| AF |
| With AF |
264/756
(27.2) |
210/925
(18.8) |
1.64
(1.37–1.98) |
<0.001 |
1.18
(0.94–1.48) |
0.15 |
0.93 |
| Without AF |
231/686
(28.5) |
418/1,689
(18.1) |
1.43
(1.22–1.68) |
<0.001 |
1.14
(0.93–1.41) |
0.21 |
| DM |
| With DM |
180/599
(24.9) |
208/911
(17.9) |
1.37
(1.12–1.68) |
0.002 |
1.00
(0.77–1.30) |
0.99 |
0.38 |
| Without DM |
315/843
(30.0) |
420/1,703
(18.9) |
1.63
(1.41–1.89) |
<0.001 |
1.32
(1.10–1.60) |
0.004 |
| Prior MI |
| With prior MI |
149/441
(28.2) |
127/467
(21.3) |
1.26
(1.00–1.60) |
0.05 |
1.00
(0.74–1.35) |
0.999 |
0.13 |
| Without prior MI |
346/1,001
(27.8) |
501/2,147
(17.9) |
1.59
(1.38–1.82) |
<0.001 |
1.25
(1.05–1.49) |
0.014 |
| Anemia |
| With anemia |
399/1,078
(29.8) |
492/1,627
(23.1) |
1.26
(1.10–1.43) |
<0.001 |
1.10
(0.93–1.30) |
0.29 |
0.003 |
| Without anemia |
95/363
(22.1) |
136/981
(11.2) |
2.05
(1.58–2.66) |
<0.001 |
1.65
(1.16–2.35) |
0.006 |
| Renal failure |
eGFR
<30 mL/min/1.73 m2 |
234/548
(35.0) |
212/570
(29.7) |
1.17
(0.97–1.41) |
0.10 |
1.03
(0.81–1.32) |
0.80 |
0.04 |
eGFR
≥30 mL/min/1.73 m2 |
260/892
(23.5) |
414/2,039
(15.4) |
1.51
(1.29–1.76) |
<0.001 |
1.26
(1.03–1.53) |
0.02 |
Abbreviations as in Tables 1,2.
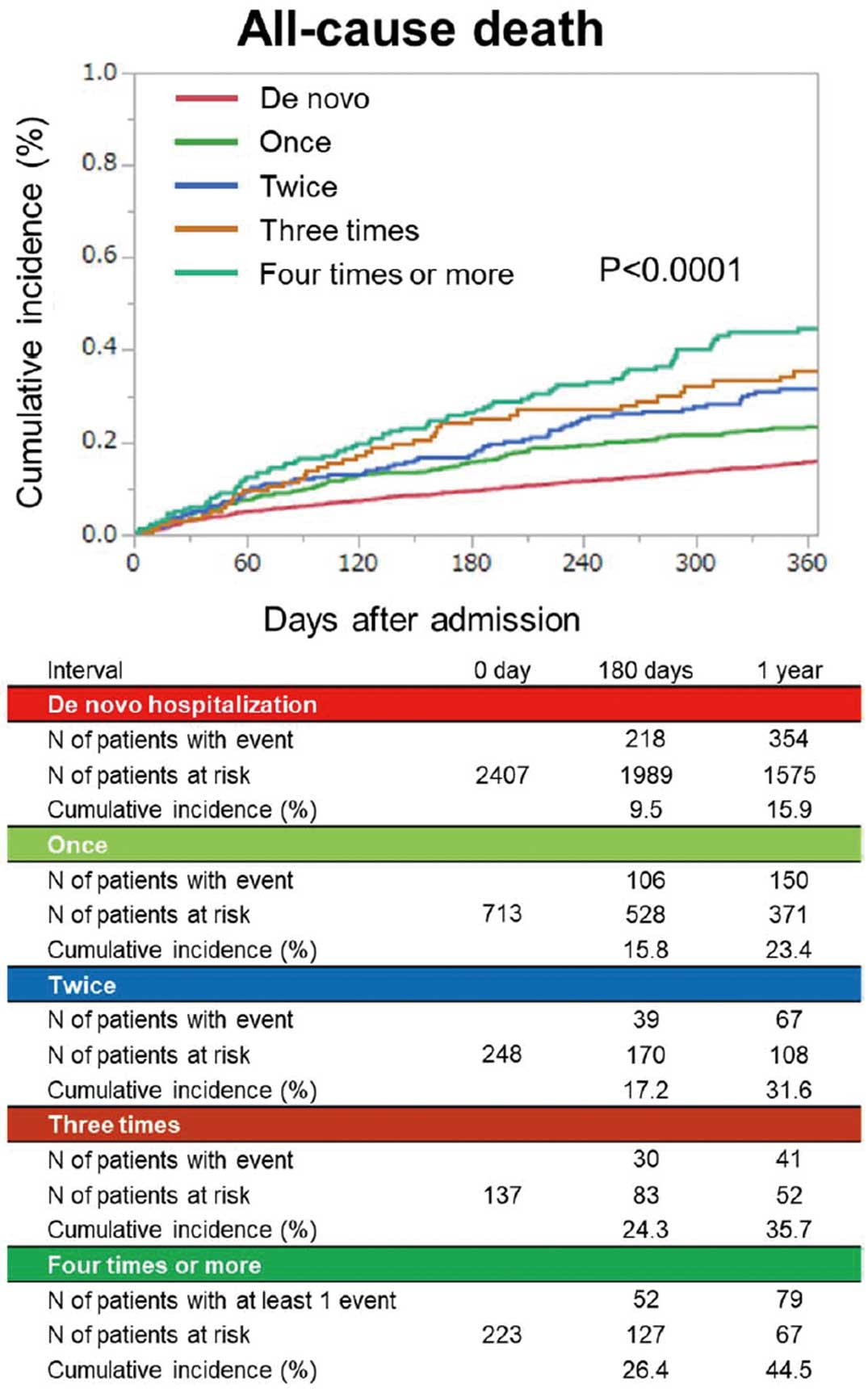
Patients were classified based on the number of previous hospitalizations: none, n=2,614 (64.5%); once, n=767 (18.9%); twice, n=277 (6.8%); three times, n=150 (3.7%); and four times or more, n=248 (6.1%;
Supplementary Table 2). Baseline characteristics in the 5 groups based on the number of previous hospitalizations are listed in
Supplementary Table 1. The cumulative 1-year incidence of all-cause death was higher as the number of previous hospitalizations increased (Figure 3). The increasing number of hospitalizations was associated with an increasing higher risk for all-cause death (HR per 1-grade increase, 1.12; 95% CI: 1.05–1.19, P<0.001).
Additional Analysis
When we analyzed 3,728 patients discharged alive, the trend was fully consistent with the main analysis (Supplementary Figure 2;
Supplementary Table 3).
Discussion
The main findings of the present study are as follows: (1) previous history of HF hospitalization in patients hospitalized for ADHF was associated with a higher risk for mortality; (2) on subgroup analysis, the excess risk of previous hospitalization relative to de novo hospitalization for all-cause death was significant in patients ≤80 years of age, patients without anemia, and patients without renal failure, but not significant in patients >80 years of age, patients with anemia, and patients with renal failure, with significant interaction; and (3) the cumulative 1-year incidence of all-cause death increased with increasing number of previous hospitalizations.
The mean age of patients hospitalized for ADHF is getting older, with a larger proportion of HF with preserved ejection fraction.9,15
The average age of patients enrolled in REALITY-AHF conducted in 2014–2015 was 78 years,16
and the median age of patients enrolled in the present study was 80 years. The proportion of previous hospitalizations for HF was 36% in the ATEND registry conducted in 2007–2011,17
and 30% for the WET-HF registry conducted in 2011–2015,18
which is similar to the 35% in the present study. From the WET-HF registry, Akita et al reported that a history of multiple previous HF admissions was an independent and strong risk factor for adverse events in ADHF patients discharged alive.19
The present result is in line with the previous studies.4–6,19
The present findings, however, are novel in Japan because we analyzed the association between the history of previous hospitalization and mortality, starting from presentation to hospital, in conjunction with social background, and found that an increasing number of prior hospitalizations was associated with an increasing, higher mortality during a relatively short follow-up duration of 1 year. Therefore, the prevention of ADHF, regardless of whether the episode is the first or second or more, would be critically important in the management of HF. The threshold for the decision on hospitalization can be influenced by severity of HF and comorbidity, as well as by differences in practice pattern between hospitals, physicians, or locality. We adjusted for the former by including those baseline covariates that affected death in the overall multivariable mortality model. The present data are in line with evidence in Canada and the USA,4–6
and can be generalized, although the previous studies analyzed chronic HF patients6
or patients discharged alive in ADHF;4,5
and none analyzed the entire clinical course starting from presentation to hospital.
In patients <80 years of age and in those without anemia or without renal failure, prior history of HF hospitalization was associated with a significantly higher 1-year mortality. This indicates that young patients without anemia or without renal failure need special attention to prevent HF deterioration before they develop symptoms and need hospitalization. Regarding the LVEF, several drugs for HF (e.g., angiotensin-converting enzyme inhibitors,20,21
β-blockers,22,23
and mineralocorticoid receptor antagonists24) have been proven to reduce mortality in patients with HF with reduced LVEF, and have been widely applied in daily practice. Previous hospitalization was still associated with mortality regardless of LVEF after adjustment for these drugs. The trend was consistent with a previous Japanese study,19
except for the interaction when we stratified by age, renal dysfunction, and anemia. The discrepancy may be due to the difference in the endpoint of all-cause death alone or a composite endpoint of death and HF hospitalization, along with the number of patients with events or enrolled.
An increase in mortality with the increasing number of hospitalizations might indicate the importance of decreasing the number of hospitalizations even once. Some patients who tolerate repeated admissions are called “frequent flyers”, but they are progressing toward death.5
We assessed medical adherence, public financial support, living alone, cognitive dysfunction, and physical status. Consistently with previous studies,25–28
patients with prior HF hospitalization more often had poor medical adherence; further, they more often received social support and less often were employed compared with patients with de novo hospitalization. The present results might have significant implications for the clinical care for HF in Japan. The cause-effect relationship between these unfavorable social conditions and repeated hospitalizations was not determined in the present study, but patients with recurrent HF admissions would need to be carefully evaluated to determine whether they have poor health literacy, and should be educated on the prevention of HF exacerbation,25,27
and, in some cases, should be supported physically or financially by public resources to improve medical adherence,26,29
and ultimately to maintain the compensated state of HF.30
Study Limitations
There were several notable limitations in the present study. The primary variable was the previous hospitalization, and therefore, milder forms of ADHF that are managed without hospitalization were not taken into consideration in the present study. In addition, we did not collect data on the interval from the previous hospitalization to the index hospitalization.
It is likely that additional factors beyond HF severity and clinical practice might have been related to the repeated hospitalizations, such as the lower threshold for hospitalization in patients with prior hospitalization. Nonetheless, repeated hospitalization was independently associated with all-cause death. Finally, there are unmeasured confounders that influence the effect of previous hospitalization on mortality.
Conclusions
In a contemporary ADHF cohort in Japan, repeated hospitalization was directly proportional to a higher risk for 1-year mortality.
Disclosures
This study is supported by a grant from the Japan Agency for Medical Research and Development (18059186) to T. Kato, K.K., N.O. The founder had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication. K.K. is a member of
Circulation Reports
’ Editorial Team.
Supplementary Files
Please find supplementary file(s);
http://dx.doi.org/10.1253/circrep.CR-19-0054
References
- 1.
Chioncel O, Collins SP, Greene SJ, Pang PS, Ambrosy AP, Antohi EL, et al. Predictors of post-discharge mortality among patients hospitalized for acute heart failure. Card Fail Rev 2017; 3: 122–129.
- 2.
Gheorghiade M, Shah AN, Vaduganathan M, Butler J, Bonow RO, Rosano GM, et al. Recognizing hospitalized heart failure as an entity and developing new therapies to improve outcomes: Academics’, clinicians’, industry’s, regulators’, and payers’ perspectives. Heart Fail Clin 2013; 9: 285–290, v–vi.
- 3.
Goodlin SJ. Palliative care in congestive heart failure. J Am Coll Cardiol 2009; 54: 386–396.
- 4.
Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J 2007; 154: 260–266.
- 5.
Lee DS, Austin PC, Stukel TA, Alter DA, Chong A, Parker JD, et al. “Dose-dependent” impact of recurrent cardiac events on mortality in patients with heart failure. Am J Med 2009; 122: 162–169.e161.
- 6.
Solomon SD, Dobson J, Pocock S, Skali H, McMurray JJ, Granger CB, et al. Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation 2007; 116: 1482–1487.
- 7.
Mills RM. The heart failure frequent flyer: An urban legend. Clin Cardiol 2009; 32: 67–68.
- 8.
Yamamoto E, Kato T, Ozasa N, Yaku H, Inuzuka Y, Tamaki Y, et al. Kyoto Congestive Heart Failure (KCHF) study: Rationale and design. ESC Heart Fail 2017; 4: 216–223.
- 9.
Yaku H, Ozasa N, Morimoto T, Inuzuka Y, Tamaki Y, Yamamoto E, et al. Demographics, management, and in-hospital outcome of hospitalized acute heart failure syndrome patients in contemporary real clinical practice in Japan: Observations from the prospective, multicenter Kyoto Congestive Heart Failure (KCHF) Registry. Circ J 2018; 82: 2811–2819.
- 10.
Ministry of Education, Culture, Sports, Science and Technology; Ministry of Health, Labour and Welfare. Japan’s ethical guidelines for epidemiologic research. http://www.lifescience.mext.go.jp/files/pdf/n796_01.pdf (accessed September 20, 2019).
- 11.
National Institute of Population and Social Security Research. Social security in Japan 2014. http://www.ipss.go.jp/s-info/e/ssj2014/006.html (accessed September 20, 2019).
- 12.
Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: A comprehensive review of recent literature. J Clin Psychiatry 2002; 63: 892–909.
- 13.
Prado JC Jr, Kupek E, Mion D Jr. Validity of four indirect methods to measure adherence in primary care hypertensives. J Hum Hypertens 2007; 21: 579–584.
- 14.
Yaku H, Kato T, Morimoto T, Inuzuka Y, Tamaki Y, Ozasa N, et al. Association of mineralocorticoid receptor antagonist use with all-cause mortality and hospital readmission in older adults with acute decompensated heart failure. JAMA Netw Open 2019; 2: e195892.
- 15.
Shiraishi Y, Kohsaka S, Sato N, Takano T, Kitai T, Yoshikawa T, et al. 9-year trend in the management of acute heart failure in Japan: A report from the National Consortium of Acute Heart Failure Registries. J Am Heart Assoc 2018; 7: e008687.
- 16.
Matsue Y, Damman K, Voors AA, Kagiyama N, Yamaguchi T, Kuroda S, et al. Time-to-furosemide treatment and mortality in patients hospitalized with acute heart failure. J Am Coll Cardiol 2017; 69: 3042–3051.
- 17.
Sato N, Kajimoto K, Asai K, Mizuno M, Minami Y, Nagashima M, et al. Acute decompensated heart failure syndromes (ATTEND) registry. A prospective observational multicenter cohort study: Rationale, design, and preliminary data. Am Heart J 2010; 159: 949–955.e941.
- 18.
Shiraishi Y, Kohsaka S, Abe T, Mizuno A, Goda A, Izumi Y, et al. Validation of the Get With The Guideline-Heart Failure risk score in Japanese patients and the potential improvement of its discrimination ability by the inclusion of B-type natriuretic peptide level. Am Heart J 2016; 171: 33–39.
- 19.
Akita K, Kohno T, Kohsaka S, Shiraishi Y, Nagatomo Y, Goda A, et al. Prognostic impact of previous hospitalization in acute heart failure patients. Circ J 2019; 83: 1261–1268.
- 20.
The Consensus Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure: Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med 1987; 316: 1429–1435.
- 21.
Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991; 325: 293–302.
- 22.
Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure: US Carvedilol Heart Failure Study Group. N Engl J Med 1996; 334: 1349–1355.
- 23.
The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): A randomised trial. Lancet 1999; 353: 9–13.
- 24.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure: Randomized Aldactone Evaluation Study Investigators. N Engl J Med 1999; 341: 709–717.
- 25.
Mayberry LS, Schildcrout JS, Wallston KA, Goggins K, Mixon AS, Rothman RL, et al. Health literacy and 1-year mortality: Mechanisms of association in adults hospitalized for cardiovascular disease. Mayo Clin Proc 2018; 93: 1728–1738.
- 26.
Granger BB, Swedberg K, Ekman I, Granger CB, Olofsson B, McMurray JJ, et al. Adherence to candesartan and placebo and outcomes in chronic heart failure in the CHARM programme: Double-blind, randomised, controlled clinical trial. Lancet 2005; 366: 2005–2011.
- 27.
Michalsen A, Konig G, Thimme W. Preventable causative factors leading to hospital admission with decompensated heart failure. Heart 1998; 80: 437–441.
- 28.
Potter EL, Hopper I, Sen J, Salim A, Marwick TH. Impact of socioeconomic status on incident heart failure and left ventricular dysfunction: Systematic review and meta-analysis. Eur Heart J Qual Care Clin Outcomes 2019; 5: 169–179.
- 29.
Wu JR, Frazier SK, Rayens MK, Lennie TA, Chung ML, Moser DK. Medication adherence, social support, and event-free survival in patients with heart failure. Health Psychol 2013; 32: 637–646.
- 30.
Heisler M, Choi H, Rosen AB, Vijan S, Kabeto M, Langa KM, et al. Hospitalizations and deaths among adults with cardiovascular disease who underuse medications because of cost: A longitudinal analysis. Med Care 2010; 48: 87–94.