2020 Volume 2 Issue 9 Pages 526-530
2020 Volume 2 Issue 9 Pages 526-530
Background: COVID-19 is fatal to patients with pulmonary hypertension (PH), so preventive actions are recommended. This study investigated the effectiveness of telemedicine and effects on quality of life (QOL) in the treatment of patients with PH.
Methods and Results: Japanese patients with PH (n=40) were recruited from one referral center. Patient self-reported anxiety worsened significantly and elderly patients in particular experienced detrimental lifestyle changes under COVID-19. Telemedicine worked well to decrease the frequency of going out.
Conclusions: Telemedicine is effective in reducing travel distances, and frequent remote interventions may be desirable for older, anxious patients.
Pulmonary hypertension (PH) is a rare disease, but in recent years the survival of patients with pulmonary arterial hypertension (PAH) or chronic thromboembolic PH (CTEPH) has improved.1,2 Thus, it has become increasingly important to assess patients’ long-term quality of life using indicators for patient-reported outcomes (PRO) as well as prognostic assessment.3,4
In addition to frequently causing pneumonia, COVID-19 infection causes thrombosis and pulmonary circulatory disorders.5 Thus, COVID-19 is considered to present a high risk of mortality if a patient with PH is infected.6 Patients with PH also know that their disease reduces the pulmonary circulation, so they try to reduce their own risk of infection by making lifestyle changes and reinforcing preventive health behaviors. In this context, telemedicine is expected to be effective as a means of reducing the risk of infection for patients.6,7
In this study we investigated the lifestyle changes of PH patients resulting from the COVID-19 outbreak in Japan and whether these changes had negative or positive effects on patients with PH. We also analyzed the role of telemedicine in treating PH patients by examining modality, distance patients would have traveled, and frequency of use.
Japanese patients with PH (including PAH and CTEPH) aged ≥18 years were recruited to the study. Patients were excluded from the study if their World Health Organization (WHO) functional class was expected to change or PH-specific treatment was expected to start or change during the study. In addition, patients who were unable to understand and respond to the questionnaire due to comorbidities were excluded from the study.
Data CollectionA questionnaire investigating the effects of COVID-19 was administered to patients between 17 and 23 May 2020 at a center for PH in Japan (the International University of Health and Welfare Mita Hospital).
This study was conducted in accordance with the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects. The study was approved by the International University of Health and Welfare Ethics Review Board (No. 5-16-30) and the procedures followed the ethical standards of the local responsible committee on human experimentation. Informed consent was obtained by allowing patients to opt-out of the study on the website. Patients who declined to participate were excluded from the study.
MeasuresParticipating physicians collected data on patient demographics and clinical characteristics and asked patients to complete questionnaires by mail. The questionnaire consisted of three separate self-administered questionnaires: (1) the Japanese emPHasis-10;4 (2) the Hospital Anxiety and Depression Scale (HADS);8 and (3) a survey prepared especially for this study. In the case of participants who had completed the questionnaire prior to the spread of COVID-19, scores for each item were compared before and after the spread of COVID-19. Information regarding clinical characteristics, clinical classification of PH,9 and WHO functional class10 was obtained from patients’ medical records.
emPHasis-10The Japanese version of emPHasis-10 is a multiparameter 10-item questionnaire that measures the physical and psychological state of patients with PH.3 The Japanese version of emPHasis-10 has been examined for both linguistic and psychometric validation.4 The total emPHasis-10 score is the sum of scores for each item (between 0 and 5) and ranges from 0 to 50. Higher scores indicate impaired conditions associated with PH.
HADSHADS is a 14-item tool measuring a person’s state of anxiety and depression.8 Seven items assess anxiety and depression subscales. The total HADS score is the sum each scores for item (between 0 and 3) and ranges from 0 to 42. Higher scores indicate greater emotional distress. A validated Japanese version of HADS11,12 was used in this study.
Original QuestionnaireThe original questionnaire consisted of nine self-assessed items to evaluate the effect of the spread of COVID-19 on PH patients.
Q1. Fewer trips out for work (e.g., telework).
Q2. Fewer trips out for shopping.
Q3. I did not to go to places where there were a lot of people, except for work and shopping.
Q4. My family has become more willing to help me with household chores.
Q5. I began to actively watch medical information on the TV news and other media.
Q6. I take fewer opportunities to watch the TV and Internet because too much information is more concerning.
Q7. I have more opportunities to reflect on my physical condition and overall condition, such as weight, swelling, blood pressure, and oxygen levels.
Q8. It is easier to be sensitive to my own symptoms, such as shortness of breath and heart palpitations.
Q9. Select the answer that best describes your perception of the effects of COVID-19-induced lifestyle changes on your management of PH:
A. COVID-19 has had a very bad effect
B. It has had a bad effect
C. Nothing has changed
D. It has had a good effect
E. It has had a very good effect
Telemedicine for Patients With PHTelemedicine was administered by telephone or through a common Internet social networking application, namely LINE (LINE Corporation). The distances covered by telemedicine were measured using Google Maps, measuring a straight line between the patient’s home and the hospital, and summing the straight-line distances for each visit. In addition, the application of telemedicine was analyzed in relation to age, primary disease, and the use of parenteral prostaglandin medications.
Statistical AnalysisParticipant demographic and clinical characteristics were analyzed descriptively. For item analyses of the Japanese version of emPHasis-10, the total score was calculated. The validity of emPHasis-10 was assessed based on known-group validity, and total emPHasis-10 scores were calculated for different groups of participants based on WHO functional classification. A linear trend was tested across groups with different levels of functional status using the Jonckheere-Terpstra test, with significance set at 2-tailed P<0.05. It was hypothesized that participants with a higher (worse) functional status would have a higher emPHasis-10 score. Unanswered questionnaire items were treated as missing data. The significance of differences in data about telemedicine was determined using Student’s t-test with unequal variances. All analyses were performed using SPSS version 25 or later (IBM Corp., Armonk, NY, USA). Unless indicated otherwise, data are presented as the mean±SD.
Of the 45 patients who received telemedicine after the spread of the COVID-19 pandemic, 40 took part in this study (Supplementary Figure). Participant demographic and clinical characteristics are summarized in Table 1. Mean patient age was 54.9±15.5 years, and most patients were women (85.0%). The most common PH classification was idiopathic PAH and most patients were categorized as WHO functional class II (69.3%).
| Age (years) | 54.9±15.5 |
| Female sex | 34 (85.0) |
| Classification of pulmonary hypertension (Nice, 2013) | |
| 1. PAH | |
| Idiopathic/heritable PAH | 20 (50.0) |
| Associated PAH | |
| Connective tissue disease | 5 (12.5) |
| Portal hypertension | 1 (2.5) |
| Congenital heart disease | 6 (15.0) |
| 1’. Pulmonary veno-occlusive disease and/or pulmonary capillary hemangiomatosis | 1 (2.5) |
| 4. Chronic thromboembolic pulmonary hypertension | 7 (17.5) |
| WHO functional class | |
| I | 5 (12.5) |
| II | 20 (50.0) |
| III | 13 (32.5) |
| IV | 2 (5.0) |
| Patients receiving parenteral prostacyclin analogs | 7 (17.5) |
| Plasma BNP (pg/mL) | 48.2±97.7 |
| Serum creatinine (mg/dL) | 0.83±0.26 |
Data are given as the mean±SD or as n (%). BNP, B-type natriuretic peptide; PAH, pulmonary arterial hypertension; WHO, World Health Organization.
The mean total score on the Japanese version of emPHasis-10 after the spread of COVID-19 was 17.6±9.7. Mean scores for the anxiety and depression subscales on the HADS and the total HADS score were 4.3±2.8, 4.4±2.6, and 8.7±4.6, respectively. Data on the HADS was missing for 3 patients. A linear increasing trend was observed in the total emPHasis-10 score across the 4 WHO functional classes (Jonckheere-Terpstra test, P=0.003; Figure 1).
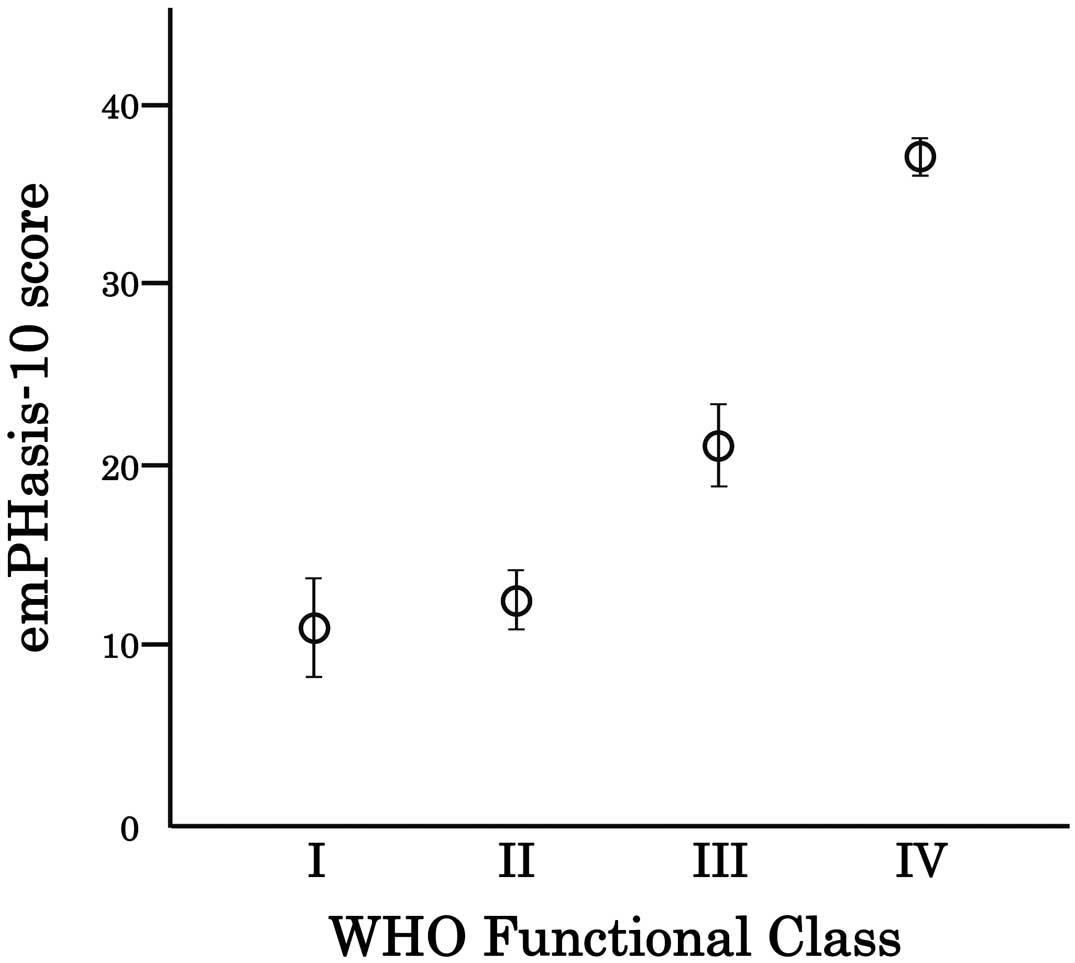
Known-group validity of emPHasis-10 according to the World Health Organization (WHO) functional class. The significance of differences in emPHasis-10 scores between the WHO functional classes was tested using the Jonckheere-Terpstra test (P=0.003). Data are the mean±SEM.
Previous emPHasis-10 and HADS scores before the spread of COVID-19 were available for 18 PAH patients in this study (Supplementary Figure). The mean age of these 18 patients was 56.1±12.6 years, and most (88.9%) were female. Comparing scores before and after the spread of COVID-19 revealed no significant changes in total emPHasis-10 scores (from 20.1±10.8 to 17.9±9.4; paired t-test, P=0.416), HADS depression subscale scores (from 4.0±3.0 to 4.5±2.3; paired t-test, P=0.487), or HADS total scores (from 7.8±5.3 to 9.7±4.4; paired t-test, P=0.115). However, the spread of COVID-19 significantly increased the HADS anxiety subscale scores (from 3.8±2.9 to 5.2±3.0; paired t-test, P=0.035).
Effects of COVID-19 on Daily Life With PHThe results of the questionnaire investigating the changes in daily life after the spread of COVID-19 are summarized in Table 2. The answers to Q1–Q8 indicated that many patients were strictly abstaining from going out, and some indicated they were more attentive to their symptoms than usual. The responses to questions assessing comprehensive changes in the overall health and wellbeing of patients with PH following the spread of COVID-19 revealed that 30.0% of patients felt that COVID-19 had had a negative effect on their personal health care, whereas almost the same number of patients (32.5%) felt that it had had a positive effect on their daily life. For the 39 patients who answered the question about changes in daily life, correlations were analyzed between the answers and age, sex, primary disease, and WHO functional class; these analyses revealed that only age had an effect. A linear trend was found in that the older patients were, the worse they felt about the items listed in the original questionnaire (Jonckheere-Terpstra test, P=0.002; Figure 2).
| Question | No. patients answering “yes” (%) |
|---|---|
| Q1. Fewer trips out for work (telework etc.). | 10 (25.0) |
| Q2. Fewer trips out for shopping. | 38 (95.0) |
| Q3. I did not to go to places where there were a lot of people except for work and shopping. | 39 (97.5) |
| Q4. My family has become more willing to help me with household chores. | 19 (47.5) |
| Q5. I began to actively watch medical information on TV news and other media. | 32 (80.0) |
| Q6. I take fewer opportunities to watch TV and the Internet because too much information is more worrying. |
1 (2.5) |
| Q7. I have more opportunities to reflect on my physical condition and condition, such as weight, swelling, blood pressure and oxygen levels. |
20 (50.0) |
| Q8. It’s easier to be sensitive to your own symptoms, such as shortness of breath and heart palpitations. |
13 (32.5) |
| Q9. Please select one item that best describes your perception of the effect of the COVID-19-induced lifestyle changes on your life with pulmonary hypertension. |
|
| A. COVID-19 has had a very bad effect. | 3 (7.5) |
| B. It has had a bad effect. | 9 (22.5) |
| C. Nothing has changed. | 14 (35.0) |
| D. It has had a good effect. | 12 (30.0) |
| E. It has had a very good effect. | 1 (2.5) |
| No answer | 1 (2.5) |
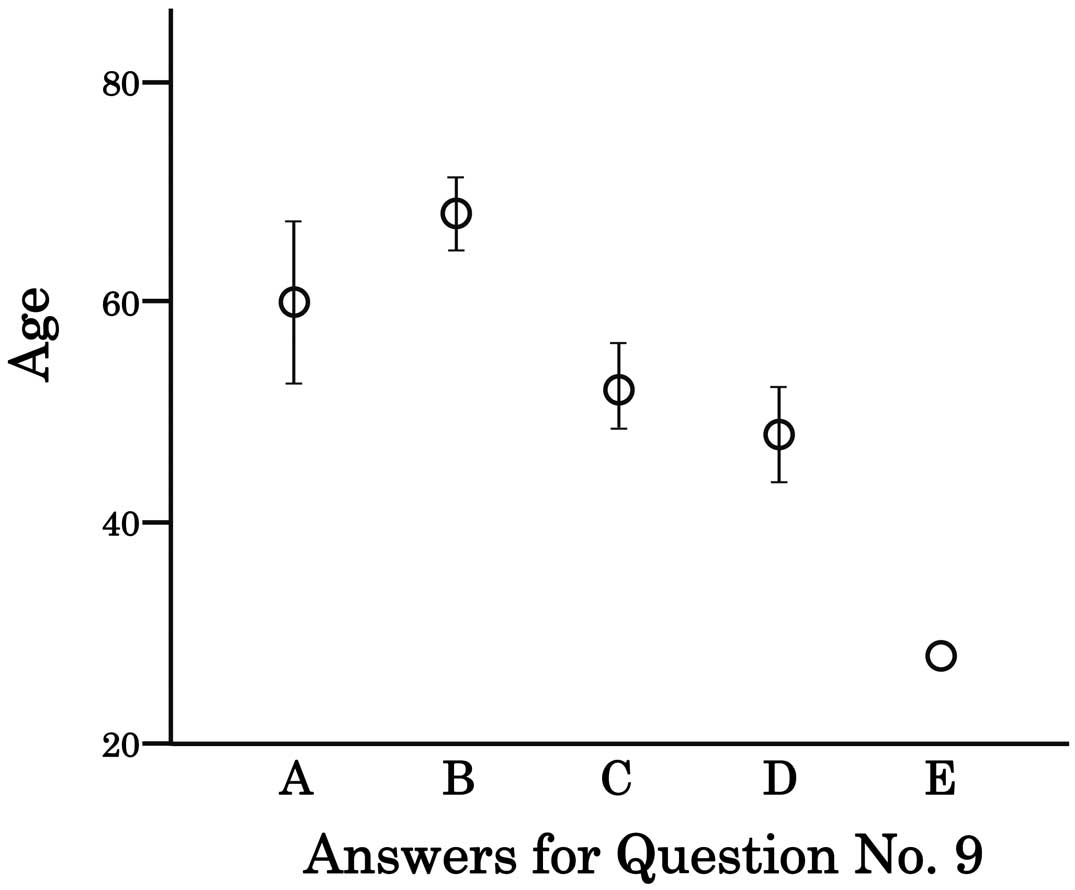
Validity of age according to Q9 on the original questionnaire that evaluated the effects of COVID-19. Participants were asked to select the answer that best described their perception of the effects of COVID-19-induced lifestyle changes on their management of pulmonary hypertension: A, COVID-19 has had a very bad effect; B, it has had a bad effect; C, nothing has changed; D, it has had a good effect; or E, it has had a very good effect. The significance of differences in the age of respondents for each option was tested using the Jonckheere-Terpstra test (P=0.002). Data are the mean±SEM.
Since the spread of COVID-19, 45 patients with PH were referred to a PH center using telemedicine between March and May 2020 (Supplementary Figure). Consultations were conducted by telephone or a web-based social networking application (LINE), whichever the patient preferred. Twenty-three patients received telephone consultations, whereas the other 22 patients were examined via an Internet video system using the LINE application on their own smartphones. The mean age of patients who used the telephone was 64 years, whereas the patients who used LINE were significantly (P<0.001) younger with a mean age of 42 years. There was no difference in the mean distance from the hospital to the patient’s residence between the telephone and LINE groups (25.3±28.7 vs. 19.7±20.3 km, respectively; P=0.45), but the number of telemedicine sessions during the same period was greater among the LINE users group (1.0±0.2 vs. 1.9±0.5 sessions; P<0.001). In addition, patients using parenteral prostanoids, who needed to be visually observed for catheter insertion site care, were significantly more likely to use LINE (n=10) than the telephone (n=2; P=0.006). Finally, we analyzed the distance that patients could avoid traveling to the hospital during this period. The mean distance that each patient would have traveled was longer in the LINE than telephone group (28.4±36.3 vs. 38.0±41.5 km; P=0.41), although the difference did not reach statistical significance. In addition, the total distance accumulated during this period was longer for the LINE than telephone group (835.0 vs. 652.5 km).
In this study we evaluated PRO in patients with PH as a result of the spread of the COVID-19 infection. When assessed on a comprehensive disease-specific scale, emPHasis-10 trend tests showed an association with exercise tolerance similar to previous reports, whereas no effect of COVID-19 was found on emPHasis-10 scores (comparing scores before and after the spread of COVID-19). Conversely, although there was no effect of COVID-19 on the depression subscale of the HADS, the spread of COVID-19 worsened HADS anxiety scores. It was previously reported that the emPHasis-10 evaluation among Japanese patients with PH was poorly correlated with HADS.4 The analysis of HADS scores in the present study revealed that the spread of COVID-19 affected patients in terms of increasing anxiety, which was not represented by symptoms or the comprehensive PRO.
Interestingly, the results of the original questionnaire revealed an almost equal proportion of patients thought that the lifestyle changes due to the spread of the COVID-19 infection had positive and negative effects on their own recuperation with PH (32.5% and 30.0%, respectively). Like in previous reports,13 it was understandable that patients would have negative perceptions of the lifestyle changes caused by COVID-19. Conversely, there are patients who perceived their current social life favorably. This could be due to patients with PH following a recuperative lifestyle that encourages rest and avoids overactivity, thus improving subjective symptoms and not reducing quality of life because it is easier for them to avoid going out.14 It was also interesting to note that age was the only factor affecting the perception of this change in living environment, with no effect of symptoms or sex. In other words, younger patients perceived lifestyle changes more favorably and positively, whereas older patients perceived the effects of COVID-19 on their lives more negatively.
Telemedicine has been found to assist in the appropriate management of patients with a severe disease in situations where it is difficult to be outside. Although telephone calls have been reported to be useful for assessing outpatients,15 this study suggested that social networking-based video calls over the Internet may be useful, especially for patients who need advanced care. Conversely, the elderly had a difficult time adjusting to the new technology, so they had to settle for traditional telephone consultations. This also suggests that the more elderly the patients were, the more traditional were the alternatives they selected when hospital visits became difficult.
These results suggest that elderly and anxious patients with PH have fewer patient care alternatives and experience a lower quality of life due to COVID-19. Therefore, it is likely that proactive nursing interventions, such as frequent telephone contact, will be necessary and it is important to continue advanced care for this group of patients.
The findings of this study suggest that telemedicine is effective in reducing travel distance for patients with PH during the spread of COVID-19. Although the spread of COVID-19 had no observable effect on the comprehensive PRO scale, worsened anxiety was revealed on psychological evaluation. Because older patients have a more negative view of the spread of COVID-19, frequent remote interventions, such as telephone calls, may be desirable for older, more anxious patients.
The authors are greatful to Ms. Itaya and Ms. Shimomura for assistance with the questionnaire.
This research was supported by a Health and Labor Sciences Research grant and AMED (Grant no. JP19lk1601003 h0002).
Y.T. has received lecture fees from Actelion Pharmaceuticals Japan and Nippon Shinyaku and research funding from Actelion Pharmaceuticals Japan and Nippon Shinyaku. The other authors have no conflicts of interest to declare.
Ethics approval was obtained from the International University of Health and Welfare Mita Hospital (5-16-30).
Individual deidentified participant data will not be shared.
Please find supplementary file(s);
http://dx.doi.org/10.1253/circrep.CR-20-0088