Abstract
Background: Cardiogenic unilateral pulmonary edema (UPE) has been reported as an unusual condition and to occur in association with severe mitral regurgitation (MR). However, the prevalence of UPE in patients with severe MR remains unknown.
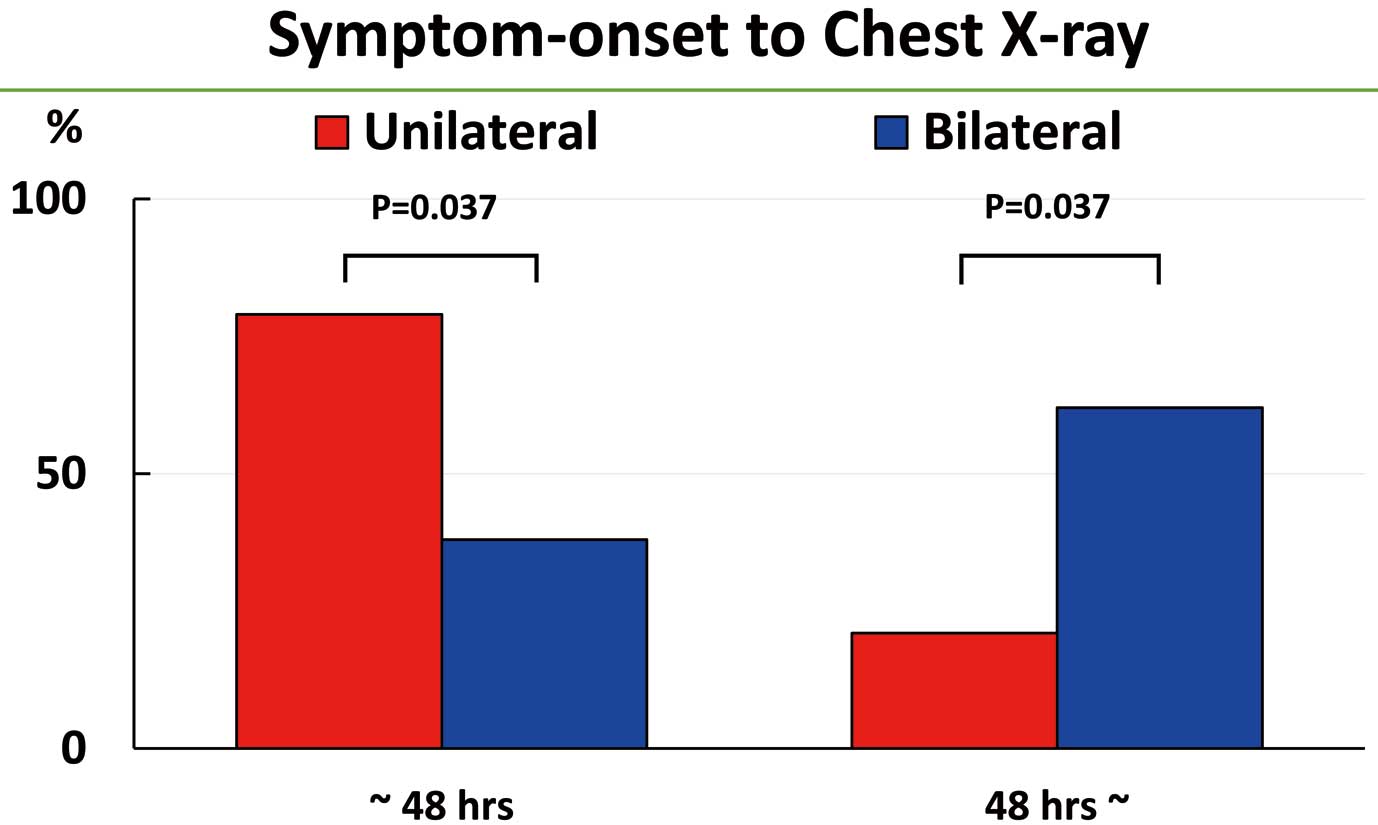
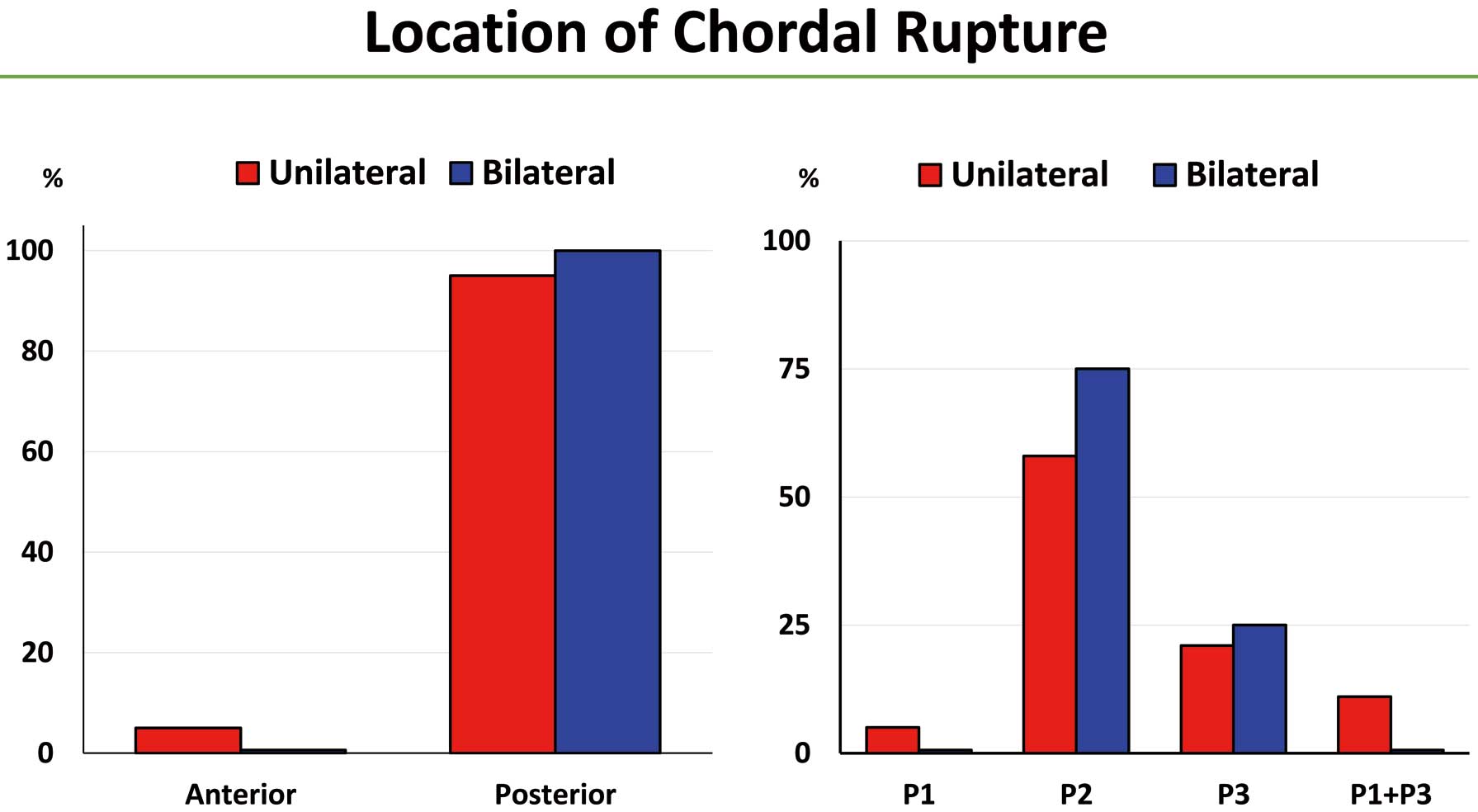
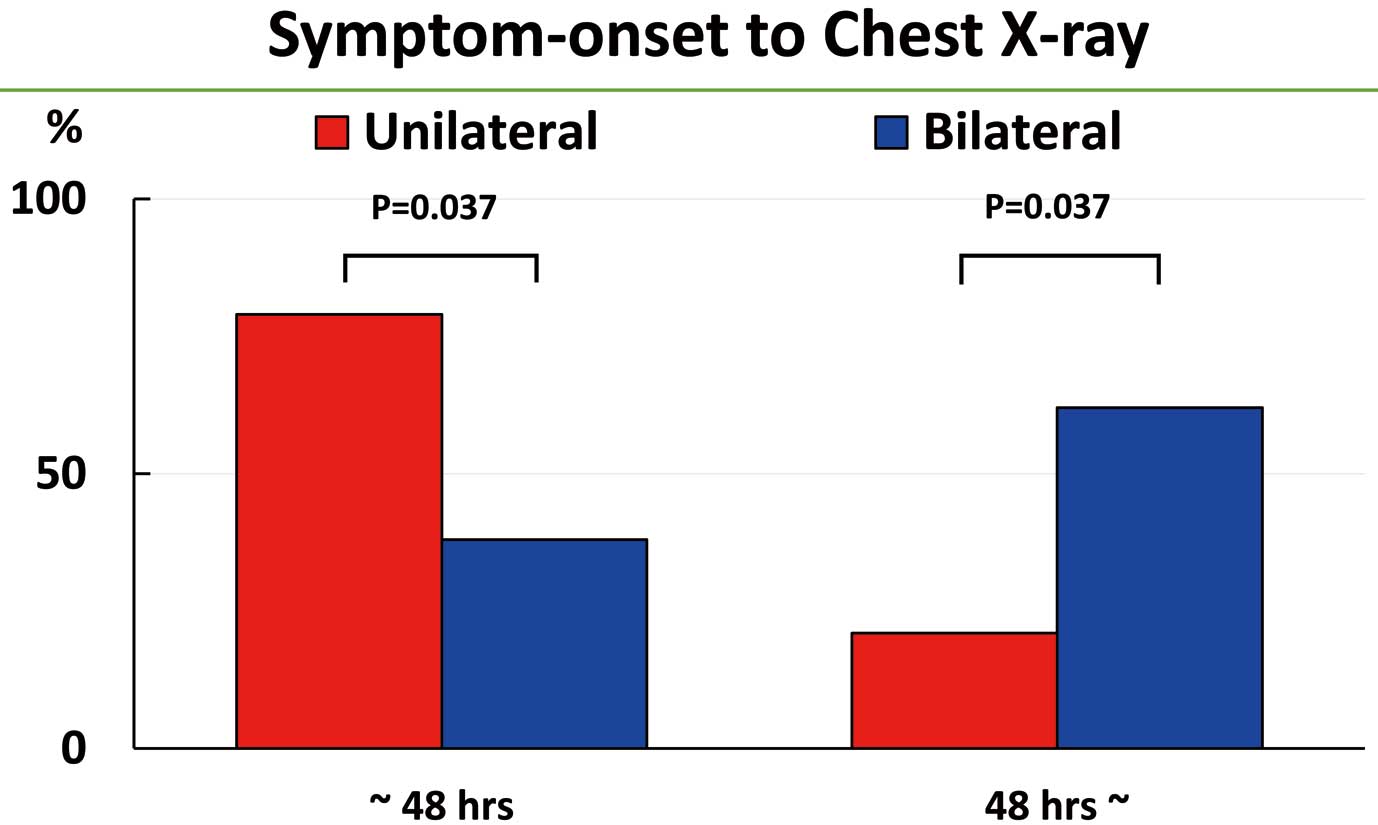
Methods and Results: Among 143 consecutive patients with chordal rupture and significant MR, 38 patients with acute severe MR were studied. The prevalence of UPE was 50% (19 patients); all these patients had right-sided UPE. Eight (21%) patients had bilateral pulmonary edema (BPE). All 8 patients with BPE and 18 of 19 patients with UPE had chordal rupture of the posterior leaflet. All patients with UPE and BPE had severe MR with similar left atrial size. Chest radiographs taken ≤48 h from symptom onset diagnosed UPE in 15 of 19 (79%) patients and BPE in 3 of 8 (38%) patients (P=0.037). Chest radiographs taken >48 h from symptom onset diagnosed UPE in 4 (21%) patients and BPE in 5 (62%) patients (P=0.037).
Conclusions: The prevalence of UPE was estimated as 50%; it was most frequently right sided and almost always associated with chordal rupture of the posterior leaflet. UPE is not rare, but common, particularly shortly after the development of acute severe MR caused by chordal rupture.
Unilateral pulmonary edema (UPE), localized to the right upper lobe, is known as an unusual condition1–5 and was reported to represent 2.1% of cardiogenic pulmonary edemas in a previous study.1 Cardiogenic UPE has been reported, mostly in sporadic case reports, in association with severe mitral regurgitation (MR).1,2,6–9 An eccentric direction of the MR jet is considered responsible for this unusual radiographic finding.9
However, the prevalence of UPE in patients with severe MR remains unknown. Therefore the aim of the present study was to determine the prevalence and characteristics of UPE, specifically in patients with severe MR caused by chordal rupture.
Methods
Study Population
This study enrolled 143 consecutive patients with chordal rupture and significant MR who were hospitalized at Chikamori Hospital during a 15-year period between 2006 and 2020. The initial evaluation in the present study was regarded as the first clinical assessment during which an echocardiographic diagnosis of chordal rupture and significant MR was made. From the 143 consecutive patients, 38 who had an initial chest radiographic examination within 72 h of the onset of symptoms were enrolled in the present study. All 38 patients underwent clinical evaluation at the time of admission and received appropriate and best possible management during hospitalization. The characteristics of patients with UPE were compared with those of patients with bilateral pulmonary edema (BPE).
Definitions
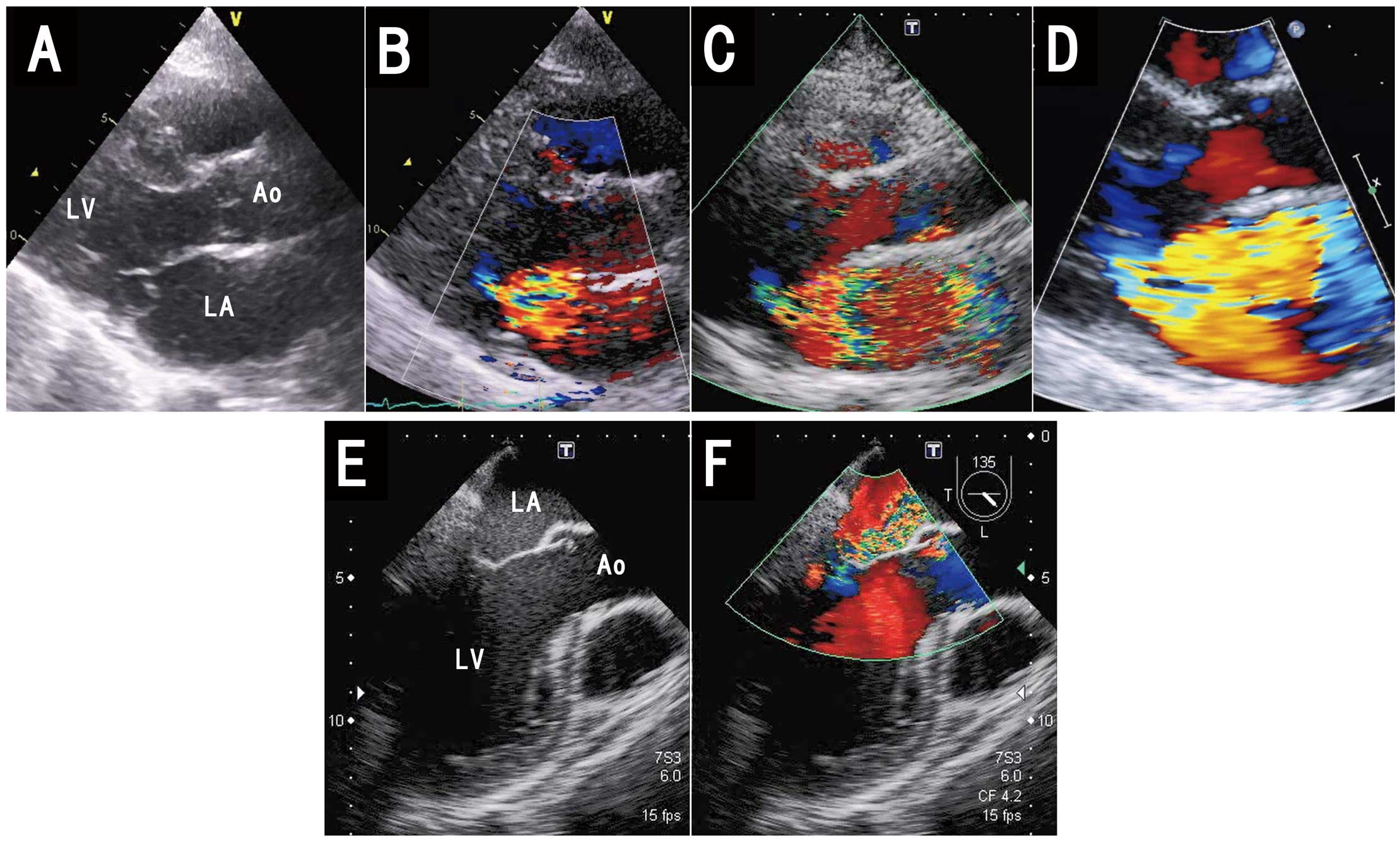
Chordal Rupture and Acute MR The diagnosis of chordal rupture and MR was based on transthoracic echocardiographic and color Doppler echocardiographic identification of ruptured chordae, leaflet prolapse, and significant MR.10 The diagnosis was made at the time of admission. Transesophageal echocardiography was performed later to precisely identify the location of the chordal rupture. Severe MR identified within 72 h of symptom onset was arbitrarily defined as acute MR.
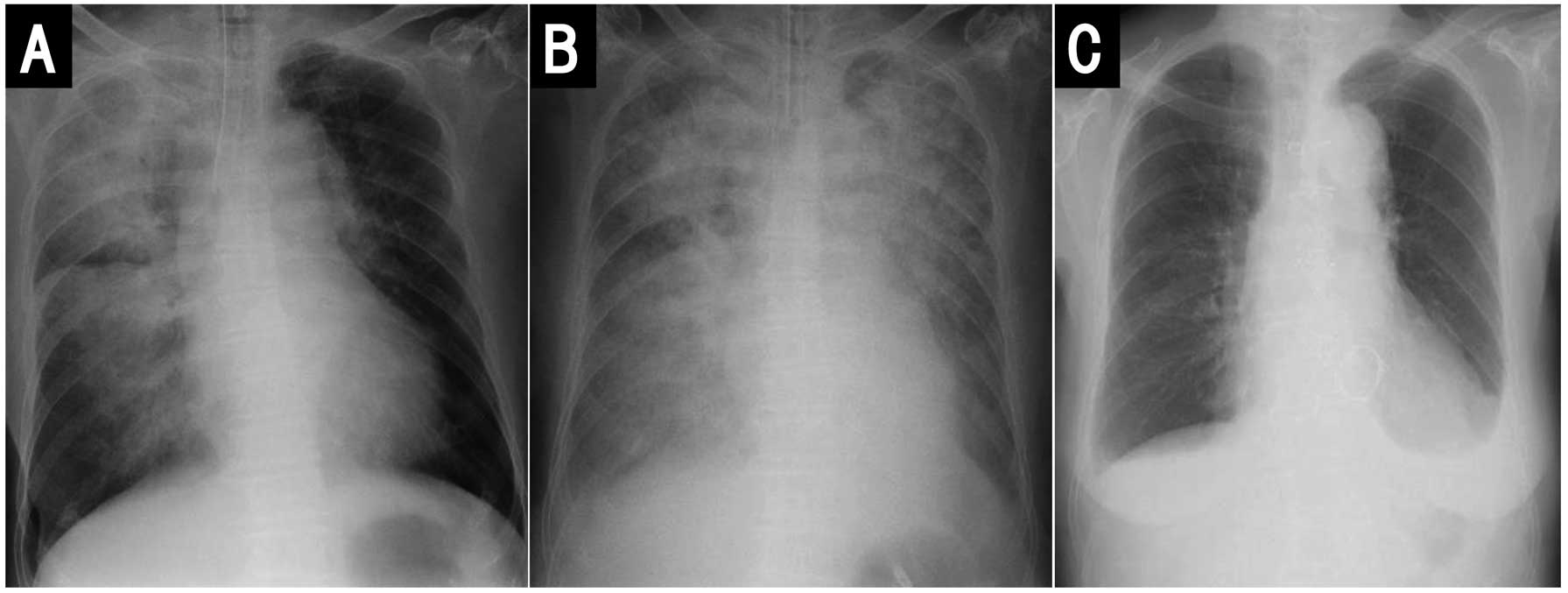
Unilateral Pulmonary Edema Chest radiographs were taken during the acute phase of pulmonary edema in the emergency department. The localization of pulmonary edema was systematically assessed, allowing UPE to be distinguished from BPE. All chest radiographs with suspicion of asymmetrical pulmonary infiltrates were reviewed by 2 investigators (Y. Nishimura, Y.D.) to confirm the final diagnosis of UPE (Figure 1A).
Echocardiographic Evaluation
Transthoracic echocardiographic and color Doppler echocardiographic studies were performed at the time of admission using commercially available ultrasound systems. The following echocardiographic parameters were systematically reviewed according to guidelines:11 left ventricular (LV) end-diastolic diameter, LV end-systolic diameter, and left atrial diameter in the parasternal long-axis view; and LV ejection fraction using the 2-dimensional Simpson method. Severe MR was defined by a Grade ≥3/4.12 Transesophageal echocardiography was performed during hospitalization within 72 h after admission to evaluate the exact location of the ruptured chordae and leaflet prolapse.
Statistical Analysis
Normally distributed continuous variables are presented as the mean±SD, whereas continuous variables that were not normally distributed are presented as the median and interquartile range (IQR). Categorical variables are reported as frequencies and percentages. Data were analyzed using the 2-sample Student’s t-test and Chi-squared test, as appropriate. Two-tailed P<0.05 was considered statistically significant.
Results
Patient Characteristics
The initial study population included 143 consecutive patients (median age, 71 years [IQR 61–79 years]; 67 women, 76 men). The baseline characteristics of the 143 patients with chordal rupture, with and without acute MR, are presented in Table 1. The cause of chordal rupture was mostly spontaneous (primary; 132/143 patients [92%]). The causes of secondary chordal rupture included myxomatous valve in 7 (5%) patients and infective endocarditis in 4 (3%) patients.
Table 1. Baseline Characteristics of the 143 Patients
| |
Total (n=143) |
MR due to chordal rupture |
P value |
| Acute (n=38) |
Chronic (n=105) |
| Age (years) |
71 [61–79] |
73 [59–80] |
70 [61–79] |
0.970 |
| Sex |
| Male |
76 (53) |
19 (50) |
57 (54) |
0.650 |
| Female |
67 (47) |
19 (50) |
48 (46) |
0.650 |
| Medical history |
| Prior heart failure |
17 (12) |
3 (8) |
14 (13) |
0.375 |
| Current smoker |
55 (38) |
15 (39) |
40 (38) |
0.881 |
| Diabetes |
17 (12) |
2 (5) |
15 (14) |
0.141 |
| Hypertension |
75 (52) |
21 (55) |
54 (51) |
0.685 |
| Dyslipidemia |
51 (36) |
13 (34) |
38 (36) |
0.827 |
| Coronary artery disease |
14 (10) |
5 (13) |
9 (9) |
0.415 |
| Atrial fibrillation |
31 (22) |
3 (8) |
28 (27) |
0.016 |
| COPD |
2 (1) |
1 (3) |
1 (1) |
0.450 |
| CKD (eGFR <30 mL/min/1.73 m2) |
0 (0) |
0 (0) |
4 (4) |
0.222 |
| Treatment before admission |
| β-blockers |
15 (10) |
2 (5) |
13 (12) |
0.220 |
| ACEI/ARB |
52 (36) |
13 (34) |
39 (37) |
0.747 |
| Aspirin/clopidogrel |
12 (8) |
3 (8) |
9 (9) |
0.897 |
| Statins |
26 (18) |
5 (13) |
21 (20) |
0.349 |
| Warfarin |
17 (12) |
1 (3) |
16 (15) |
0.040 |
| NOAC |
9 (6) |
1 (3) |
8 (8) |
0.278 |
| Diuretics |
58 (41) |
8 (21) |
50 (48) |
0.004 |
| Electrocardiogram |
| Sinus rhythm |
107 (75) |
30 (79) |
77 (73) |
0.494 |
| Atrial fibrillation |
34 (24) |
6 (16) |
28 (27) |
0.177 |
| Complete AV block |
2 (1) |
2 (5) |
0 (0) |
0.018 |
| LVH |
27 (19) |
9 (24) |
18 (17) |
0.377 |
| LBBB |
2 (1.4) |
1 (3) |
1 (1) |
0.450 |
| RBBB |
20 (14) |
3 (8) |
17 (16) |
0.206 |
| Pulmonary edema |
| UPE |
19 (13) |
19 (50) |
0 (0) |
<0.001 |
| BPE |
8 (6) |
8 (21) |
0 (0) |
<0.001 |
| Other: pleural effusion |
56 (39) |
11 (29) |
45 (43) |
0.132 |
| None |
60 (42) |
0 (0) |
60 (57) |
<0.001 |
| Initial diagnosis |
| Pulmonary edema/CHF |
128 (90) |
23 (60) |
105 (100) |
<0.001 |
| Pneumonia |
9 (6) |
9 (24) |
0 (0) |
<0.001 |
| Others |
6 (4) |
6 (16) |
0 (0) |
<0.001 |
| Cause of chordal rupture |
| Spontaneous |
132 (92) |
35 (92) |
97 (92) |
0.956 |
| Myxomatous valve |
7 (5) |
0 (0) |
7 (7) |
0.103 |
| Infective endocarditis |
4 (3) |
3 (8) |
1 (1) |
0.026 |
| Location of chordal rupture |
| Posterior |
119 (83) |
36 (95) |
83 (79) |
0.027 |
| Anterior |
22 (16) |
2 (5) |
20 (19) |
0.044 |
| Posterior+anterior |
2 (1) |
0 (0) |
2 (2) |
0.392 |
| MR grade |
| 1/4 |
4 (3) |
0 (0) |
4 (4) |
0.222 |
| 2/4 |
26 (18) |
0 (0) |
26 (25) |
0.001 |
| 3/4–4/4 |
113 (79) |
38 (100) |
75 (71) |
<0.001 |
| Echocardiography |
| LVDd (mm) |
53 [48–58] |
49 [43–55] |
53 [49–59] |
0.003 |
| LVDs (mm) |
33 [29–37] |
32 [26–36] |
34 [31–39] |
0.019 |
| EF (%) |
67 [60–72] |
66 [60–73] |
67 [61–71] |
0.660 |
| LA (mm) |
45 [40–51] |
40 [36–45] |
47 [42–52] |
<0.001 |
| BNP (pg/mL) |
226 [83–466] |
321 [221–625] |
155 [63–442] |
0.043 |
| Surgery |
| Valve repair |
101 (71) |
24 (63) |
77 (73) |
0.238 |
| Valve replacement |
25 (17) |
8 (21) |
17 (16) |
0.499 |
| No surgery |
17 (12) |
6 (16) |
11 (11) |
0.386 |
Unless indicated otherwise, data are given as the median [interquartile range] or n (%). P values are for the comparison of acute vs. chronic mitral regurgitation (MR). ACEI, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; ARB, angiotensin receptor blocker; AV, atrioventricular; BNP, B-type natriuretic peptide; BPE, bilateral pulmonary edema; CHF, congestive heart failure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; EF, ejection fraction; eGFR, estimated glomerular filtration rate; LA, left atrium; LBBB, left bundle branch block; LVDd, left ventricular end-diastolic diameter; LVDs, left ventricular end-systolic diameter; LVH, left ventricular hypertrophy; NOAC, non-vitamin K antagonist oral anticoagulants; RBBB, right bundle branch block; UPE, unilateral pulmonary edema.
Of the 143 consecutive patients, 38 with chest radiographs taken within 72 h of the onset of symptoms (median age 73 years [IQR 59–80 years]; 19 women, 19 men) were evaluated according to the presence of UPE (19 patients) and BPE (eight patients; Table 2). Eleven patients did not have pulmonary edema.
Table 2. Characteristics of Patients With Acute MR: UPE vs. BPE
| |
UPE (n=19) |
BPE (n=8) |
P value |
| Age (years) |
70 [59–79] |
74 [61–78] |
0.831 |
| Sex |
| Male |
9 (47) |
3 (38) |
0.637 |
| Female |
10 (53) |
5 (62) |
0.637 |
| Prevalence (%) |
50.0 |
21.1 |
|
| Time from symptom onset to chest X-ray (h) |
| ≤48 |
15 (79) |
3 (38) |
0.037 |
| >48 |
4 (21) |
5 (62) |
0.037 |
| Initial diagnosis |
| Pulmonary edema/CHF |
11 (58) |
4 (50) |
0.706 |
| Pneumonia |
7 (37) |
1 (13) |
0.206 |
| Other |
1 (5) |
3 (37) |
0.031 |
| Serial changes in hemodynamics |
| SBP (mmHg) |
| Day 1 |
138 [113–155] |
123 [106–135] |
0.169 |
| Day 2 |
109 [100–119] |
102 [89–114] |
0.173 |
| Day 3 |
108 [93–124] |
107 [99–103] |
0.413 |
| DBP (mmHg) |
| Day 1 |
79 [69–87] |
73 [59–86] |
0.211 |
| Day 2 |
65 [54–69] |
62 [53–68] |
0.280 |
| Day 3 |
65 [59–73] |
65 [54–70] |
0.457 |
| Heart rate (beats/min) |
| Day 1 |
103 [96–107] |
97 [86–100] |
0.267 |
| Day 2 |
84 [75–95] |
80 [69–87] |
0.255 |
| Day 3 |
90 [80–100] |
81 [70–93] |
0.115 |
| Location of chordal rupture |
| Posterior |
18 (95) |
8 (100) |
– |
| Anterior |
1 (5) |
0 (0) |
– |
| MR Grade 3/4–4/4 |
19 (100) |
8 (100) |
– |
| Echocardiography |
| LVDd (mm) |
48 [41–52] |
48 [46–54] |
0.434 |
| LVDs (mm) |
29 [25–32] |
32 [27–34] |
0.352 |
| EF (%) |
69 [64–74] |
66 [59–70] |
0.889 |
| LA (mm) |
38 [37–45] |
37 [36–43] |
0.170 |
| BNP (pg/mL) |
350 [259–581] |
273 [227–513] |
0.691 |
| Serial changes in inflammatory markers |
| WBC (/μL) |
| Day 1 |
14,200 [10,500–17,500] |
10,700 [7,550–12,625] |
0.052 |
| Day 2 |
12,800 [9,675–16,150] |
10,400 [6,600–13,800] |
0.132 |
| Day 3 |
11,400 [8,700–14,800] |
7,700 [5,100–10,400] |
0.028 |
| CRP (mg/L) |
| Day 1 |
4.9 [0.2–9.0] |
3.8 [0.2–6.9] |
0.286 |
| Day 2 |
8.2 [2.7–14.0] |
6.9 [4.7–8.2] |
0.328 |
| Day 3 |
10.7 [1.9–18.1] |
7.9 [6.2–10.2] |
0.252 |
| Urgent mitral surgery |
16 (84) |
8 (100) |
0.233 |
| Valve repair |
9 (47) |
7 (87) |
0.053 |
| Valve replacement |
7 (37) |
1 (13) |
0.206 |
| No surgery |
3 (16) |
0 (0) |
0.233 |
Unless indicated otherwise, data are given as the median [inter quartile range] or n (%). P values are for comparisons of UPE vs. BPE. CRP, C-reactive protein; DBP, diastolic blood pressure; SBP, systolic blood pressure; WBC, white blood cell. Other abbreviations as in Table 1.
The prevalence of UPE among 38 patients presenting with chordal rupture and acute MR was 50% (19 patients). The baseline characteristics of these 19 patients are presented in Table 2. All patients had right-sided UPE (Figures 1A,2) and presented with severe MR of Grade ≥3/4. A representative case of severe MR showing the sequence of changes during the acute phase is presented in Figure 3.
Characteristics of Patients With UPE and BPE
Of the 38 patients with chordal rupture and acute severe MR, 19 (50%) presented with UPE and 8 (21%) presented with BPE. The clinical characteristics were similar between patients with UPE and those with BPE, except for the time interval from the onset of symptoms to diagnosis based on chest radiographs (Table 2). Specifically, diagnoses based on chest radiographs taken ≤48 h after the onset of symptoms were made for 15 of 19 (79%) patients with UPE, 13 of whom showed UPE within 24 h, compared with 3 of 8 (38%) patients with BPE (P=0.037; Figure 4). Diagnoses based on chest radiographs taken >48 h after symptom onset were made for 4 of 19 (21%) patients with UPE, compared with 5 of 8 (62%) patients with BPE (P=0.037). As far as initial diagnoses were concerned, a diagnosis of pneumonia was inadequately made in 7 of 19 (37%) patients with UPE, although a correct diagnosis of pulmonary edema was made in 11 (58%) of these patients (Figure 5). Regarding echocardiographic localization of chordal rupture, 18 patients with UPE showed chordal rupture of the posterior leaflet (95%; 11 P2, 4 P3, 2 P1+P3, 1 P1) and 1 patient with UPE had chordal rupture of the anterior leaflet (5%); in contrast, all 8 patients with BPE had chordal rupture of the posterior leaflet (6 P2, 2 P3; Figure 6). All 19 patients with UPE and 8 patients with BPE had severe MR of Grade ≥3/4. Left atrial size was also similar between the 2 groups and was not significantly enlarged. Urgent surgery was performed in 16 (84%) patients with UPE and 8 (100%) patients with BPE (P=0.233; Table 2).
Of 19 patients who initially presented UPE, 17 had serial chest radiograph examinations, with 12 showing progression from UPE to BPE (Figure 1B), mostly within 24 h. Thereafter, with time, 11 of these 12 patients gradually developed pleural effusion (Figure 1C) after the disappearance of BPE.
In addition, 7 of 8 patients who initially presented with BPE subsequently developed pleural effusion.
Discussion
The main results of the present study are as follows. First, UPE was not rare, but common, in patients with acute severe MR caused by chordal rupture, particularly shortly after the onset of symptoms, suggesting that the interval from the onset of severe MR to the time of chest radiographic examination is an important determinant of this distinctive radiographic finding. Second, the actual prevalence of UPE was 50.0% in those with acute severe MR with chest radiographs taken within 72 h of symptom-onset, whereas it was 13.3% among the entire population of 143 patients with chordal rupture and significant MR.
Cardiogenic UPE has been reported, mostly in the form of sporadic case reports, as an unusual condition1–5 and to occur in association with severe MR.1,2,6–9 However, the prevalence of UPE in patients with severe MR remains unknown. In the present study, we sought to assess the prevalence and characteristics of UPE specifically in patients with severe MR caused by chordal rupture. From the entire population of 143 patients with chordal rupture and significant MR, 38 patients diagnosed within 72 h of symptom onset were studied. The characteristics of patients with UPE were compared with those of patients with BPE. Although Attias et al studied 869 consecutive patients admitted for cardiogenic pulmonary edema and reported that UPE represented approximately 2.1% of cardiogenic pulmonary edemas,1 at the same time they reported that UPE represented 25% of pulmonary edema with severe MR. The present study specifically investigating patients with severe MR secondary to chordal rupture indicated that the prevalence of cardiogenic UPE was common (13.3%) among the entire population of 143 patients with significant MR. Furthermore, in 38 patients with chest radiographs taken within 72 h of symptom onset, the prevalence of UPE was much greater (50%). These results are supported by 3 previous small studie,6–8 which found that 9%, 22%, and 38% of patients presenting with severe MR and congestive heart failure showed radiological signs of UPE, mainly in the right upper lobe. Schnyder et al retrospectively reviewed the chest radiographs of 131 patients with severe MR and reported that the prevalence of UPE predominantly in the right lung was 9%,6 and suggested that UPE occurred more frequently than previously assumed. Grenon and Bilodeau studied 21 cases of acute MR secondary to rupture or dysfunction of the papillary muscle or rupture of the chordae tendineae.7 In that study, pulmonary edema was unilateral and localized preferentially in the right lung in 8 of the 21 (38%) patients.7 These 8 patients had myocardial infarction and acute MR secondary to rupture or dysfunction of the papillary muscle. Therefore, it is important to recognize that cardiogenic UPE is not rare and can often be found in patients with acute severe MR caused by chordal rupture, particularly shortly after the onset of acute MR.
Several mechanisms have been suggested as causing UPE in the setting of acute severe MR. The eccentric MR jet may be directed towards the superior right pulmonary veins in patients with severe MR from the posterior leaflet.9,13–15 The anatomic position of pulmonary veins in the left atrium may also contribute to the development of UPE.16 In addition, the present study suggests that the time interval from the onset of severe MR to chest radiographic diagnosis is an important determinant contributing to the identification of this distinctive radiographic finding. This assumption is supported, in part, by the fact that in the present study, most patients with this radiographic finding of UPE subsequently showed progression to BPE within a short period of time. In addition, as shown in the present study, the main cause of acute severe MR associated with right-sided UPE seems to be severely disrupted posterior chordae tendineae.
This distinctive pattern of right-sided UPE can simulate pneumonia, hemorrhage, or neoplasia,7 and may thus often be misdiagnosed initially as a respiratory diseases, such as pneumonia,2–4 as occurred in the present study. In order to differentiate cardiogenic UPE from acute pneumonia, it is helpful to obtain clinical information, such as sudden onset of symptoms in the absence of fever, perihilar consolidation in the right lung field, the absence of significant inflammatory signs, and elevated plasma concentrations of B-type natriuretic peptide. Physical examinations attempting to detect a murmur may be problematic because the systolic murmur of acute MR may be soft, and even be absent, and it is often difficult to detect the murmur in the setting of patients presenting with respiratory distress. Thus, it is important to perform bedside transthoracic echocardiography, which will guide clinicians to a correct diagnosis of cardiogenic UPE.1,2
Computed tomography may also be helpful in differentiating pneumonia from cardiogenic UPE (Supplementary Figure).
Although transesophageal echocardiography is useful in determining more precisely the cause, severity, and mechanism of MR, it may often be practically difficult to perform on an emergency basis at many facilities. Thus, it is very important to initially anticipate cardiogenic UPE when unilateral infiltration of the lung is seen in association with significant MR without obvious dilatation of the left atrium on transthoracic echocardiography, regardless of the cause and mechanism of MR. This may pave the way to an early diagnosis of cardiogenic UPE secondary to acute severe MR. Then, early initiation of appropriate treatment may reduce the risk of mortality in patients.
Study Limitations
The main limitation of the present study is that it is a retrospective study from a single institution. Second, the number of study patients was relatively small, although the entire population of 143 patients with chordal rupture, a relatively uncommon disease, is modestly large. Third, long-term prognostic information was not obtained.
Conclusions
In the population of patients with acute severe MR caused by chordal rupture, UPE was not rare, but common, particularly shortly after the development of acute severe MR. The time interval from the onset of severe MR to diagnosis based on chest radiography seems an important determinant of this distinctive radiographic finding.
Acknowledgments
The authors thank Hiroyuki Irie and his surgical team for their excellent surgical work on the study patients.
Sources of Funding
This study did not receive any specific funding.
Disclosures
All authors have no conflict of interest to disclose.
IRB Information
This study was approved by the Ethics Committee of Chikamori Hospital (Reference no. 445).
Supplementary Files
Please find supplementary file(s);
https://doi.org/10.1253/circrep.CR-22-0090
References
- 1.
Attias D, Mansencal N, Auvert B, Vieillard-Baron A, Delos A, Lacombe P, et al. Prevalence, characteristics, and outcomes of patients presenting with cardiogenic unilateral pulmonary edema. Circulation 2010; 122: 1109–1115.
- 2.
Inotani S, Kubokawa S, Nakaoka Y, Kotani T, Matsuda H, Yamamoto S, et al. Unilateral cardiogenic pulmonary edema. J Cardiol Cases 2018; 17: 85–88.
- 3.
Nitzan O, Saliba WR, Goldstein LH, Elias MS. Unilateral pulmonary edema: A rare presentation of congestive heart failure. Am J Med Sci 2004; 327: 362–364.
- 4.
Choi HS, Choi H, Han S, Kim HS, Lee C, Kim YY, et al. Pulmonary edema during pregnancy: Unilateral presentation is not rare. Circ J 2002; 66: 623–626.
- 5.
Kashiura M, Tateishi K, Yokoyama T, Jujo M, Tanabe T, Sugiyama K, et al. Unilateral cardiogenic pulmonary edema associated with acute mitral regurgitation. Acute Med Surg 2017; 4: 119–122.
- 6.
Schnyder PA, Sarraj AM, Duvoisin BE, Kappenberger L, Landry MJM. Pulmonary edema associated with mitral regurgitation: Prevalence of predominant involvement of the right upper lobe. AJR Am J Roentgenol 1993; 161: 33–36.
- 7.
Grenon H, Bilodeau S. Pulmonary edema of the right upper lobe associated with acute mitral regurgitation. Can Assoc Radiol J 1994; 45: 97–100.
- 8.
Gudinchet F, Rodoni P, Sarraji A, Payot M, Schnyder P. Pulmonary edema associated with mitral regurgitation: Prevalence of predominant right upper lobe involvement in children. Pediatr Radiol 1998; 28: 260–262.
- 9.
Diana A, Guglielmini C, Pivetta M, Sanacore A, Di Tommaso M, Lord PF, et al. Radiographic features of cardiogenic pulmonary edema in dogs with mitral regurgitation: 61 cases (1998–2007). J Am Vet Med Assoc 2009; 235: 1–6.
- 10.
Izumi C, Eishi K, Ashihara K, Arita T, Otuji Y, Kunihara T, et al. JCS/JSCS/JATS/JSVS 2020 guidelines on the management of valvular heart disease. Circ J 2020; 84: 2037–2119.
- 11.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005; 18: 1440–1463.
- 12.
Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 2003; 24: 1231–1243.
- 13.
Miyatake K, Nimura Y, Sakakibara H, Kinoshita N, Okamoto M, Nagata S, et al. Localisation and direction of mitral regurgitation flow in mitral orifice studied with combined use of ultrasonic pulsed Doppler technique and two dimensional echocardiography. Br Heart J 1982; 48: 449–458.
- 14.
Raman S, Pipavath S. Asymmetric edema of the upper lung due to mitral valvular dysfunction. N Engl J Med 2009; 361: e6.
- 15.
Gurney JW, Goodman LR. Pulmonary edema localized in the right upper lobe accompanying mitral regurgitation. Radiology 1989; 171: 397–399.
- 16.
Marom EM, Herndon JE, Kim YH, McAdams HP. Variations in pulmonary venous drainage to the left atrium: Implications for radiofrequency ablation. Radiology 2004; 230: 824–829.