Abstract
Background: Male sex is associated with a worse clinical course and outcomes of COVID-19, particularly in older patients. However, studies on COVID-19 patients with cardiovascular disease and/or risk factors (CVDRF), which are representative risk factors of COVID-19, are limited. In this study, we investigated the effect of sex on the outcomes of hospitalized COVID-19 patients with CVDRF.
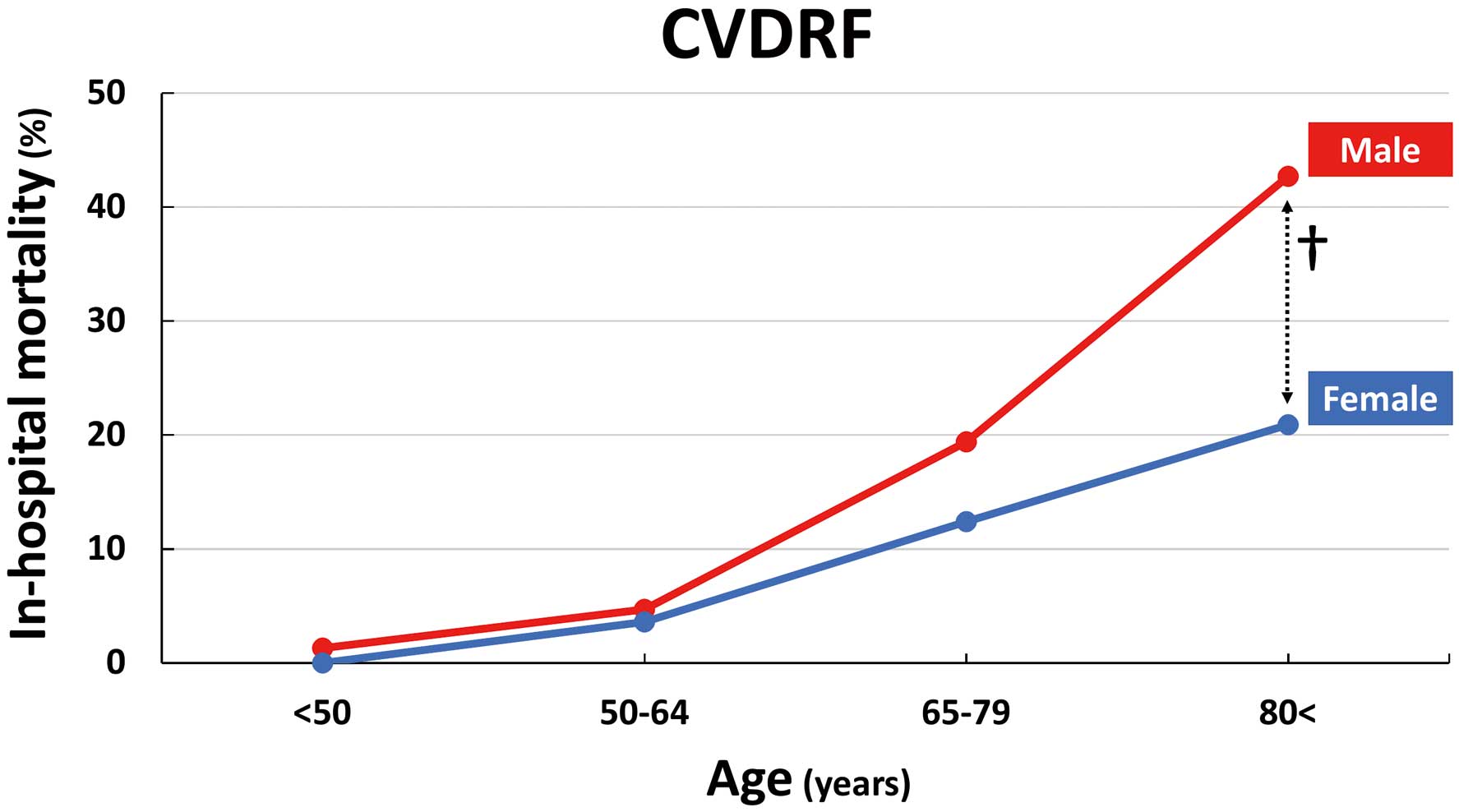
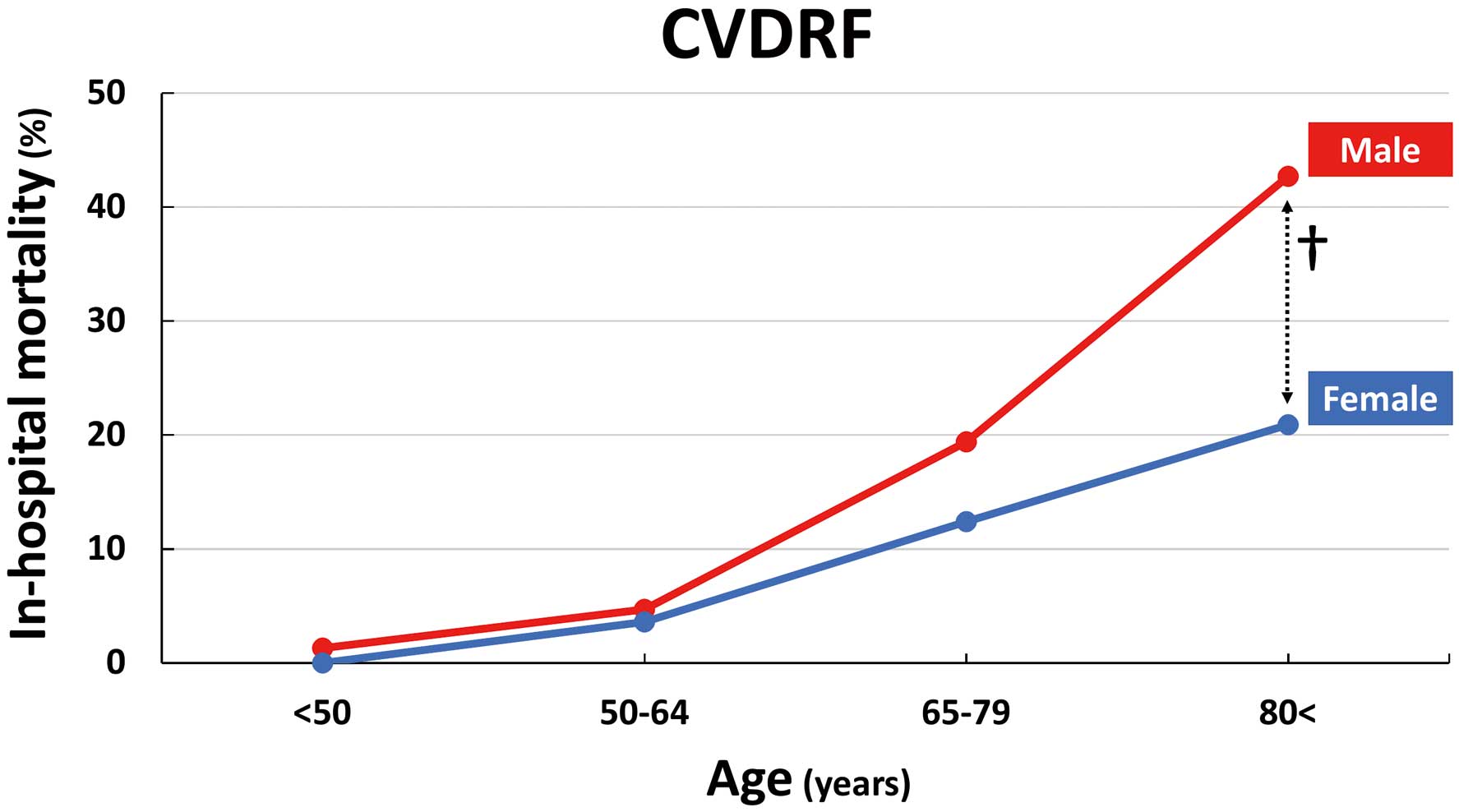
Methods and Results: We analyzed 693 COVID-19 patients with CVDRF. Patients were divided into 2 groups based on sex, and baseline characteristics and in-hospital outcomes were compared between the 2 groups. The mean age of the 693 patients was 68 years; 64.8% were men and 96.1% were Japanese. In a univariate analysis model, sex was not significantly associated with in-hospital mortality (odds ratio [OR] 1.22; 95% confidence interval [CI] 0.74–2.02; P=0.43). However, men had higher in-hospital mortality than women, especially among older (age ≥80 years) patients (OR 2.21; 95% CI 1.11–4.41; P=0.024). After adjusting for age and pivotal risk factors (hypertension, diabetes, heart failure, coronary artery disease, chronic lung disease, and chronic kidney disease), multivariate analysis suggested that male sex was an independent predictor of in-hospital mortality (OR 2.20; 95% CI 1.23–3.92; P=0.008).
Conclusions: In this post hoc analysis of a nationwide registry focusing on patients with COVID-19 and CVDRF, men had higher in-hospital mortality than women, especially among older patients.
Evidence suggests that clinical outcomes in patients with COVID-19 depends on sex.1–4 Sex influences the outcomes of COVID-19, with men having higher mortality rates than women, especially among older adults.1–5 The sex-specific outcomes of COVID-19 results from the pathophysiological background that women mount stronger immune responses against viruses and vaccines and exhibit superior immune-mediated tissue repair capacities.5 In addition, the effect of sex on outcomes seems to be greater in COVID-19 than in other viral infections.3 Sex also plays a key role in cardiovascular disease and/or risk factors (CVDRF), which are common risk factors of COVID-19.6–8 For example, acute coronary syndrome due to atherosclerosis is more common among men, although coronary artery spasm or microvascular dysfunction, which are presumed to be caused by endothelial dysfunction, are more common among women.9 The sex difference in CVDRF may be attributed to multiple factors, such as genetic mechanisms, epigenetic mechanisms, and sex hormones.10
Sex difference is a pivotal prognostic factor for both COVID-19 and CVDRF; however, the effect of sex on outcomes in patients with COVID-19 and CVDRF has not been fully investigated. A better understanding of the role of sex in prognosis in a specific population would contribute to appropriate management of COVID-19. In addition, the prognosis of COVID-19 has been scarcely reported in Japan, where the distribution of CVDRF is known to differ significantly from that in Western countries.11
In this study, we investigated the effect of sex on outcomes in patients with COVID-19 and CVDRF through a post hoc analysis of the Clinical Outcomes of COVID-19 Infection in Hospitalized Patients with Cardiovascular Diseases and/or Risk Factors (CLAVIS-COVID) registry, a Japanese nationwide study focusing on patients with COVID-19 and CVDRF.
Methods
IRB Information
This investigation conformed to the principles outlined in the Declaration of Helsinki. The study protocol, including the use of an opt-out consent method, was approved by the ethics committee of Toho University Omori Medical Center (No. M20253) and the local ethics committees of all participating institutions. Furthermore, this clinical study was registered with the University Hospital Medical Information Network (UNIM) Clinical Trial Registry (UMIN40,598) before the first patient was enrolled.
Study Design and Data Collection
The CLAVIS-COVID was a Japanese nationwide multicenter retrospective study sponsored by the Japanese Circulation Society. The registry investigated the characteristics and outcomes of patients hospitalized with COVID-19 between January 1, 2020 and May 31, 2020. For all patients, the presence of COVID-19 was defined as a positive polymerase chain reaction test result on nasal or pharyngeal swab specimens. All patients enrolled in this study were discharged by November 8, 2020, which was the deadline for data transfer.
The CLAVIS-COVID registry enrolled 1,518 patients with COVID-19, including 693 patients with underlying CVDRF.
In the present study, we analyzed 693 patients with COVID-19 and CVDRF. The study population was divided into 2 groups according to sex. The patient characteristics and in-hospital outcomes were evaluated according to sex. Underlying cardiovascular diseases included heart failure, coronary artery disease, myocardial infarction, peripheral artery disease, valvular heart disease, cardiac arrhythmia, pericarditis, myocarditis, congenital heart disease, pulmonary hypertension, deep vein thrombosis, pulmonary embolism, aortic dissection, aortic aneurysm, cerebral infarction/transient ischemic attack, use of cardiac devices (pacemaker, implantable cardioverter defibrillator, cardiac resynchronization therapy, and left ventricular assist device), heart transplantation, and cardiac arrest. Cardiovascular risk factors included hypertension, diabetes, and dyslipidemia.
Statistical Analysis
Patients with CVDRF were divided into 2 groups (men and women), and their baseline characteristics were compared. Categorical variables are presented as frequencies and percentages, whereas continuous variables are presented as the mean±SD or median with interquartile range. To evaluate significant difference between groups, Fisher’s exact test was used for categorical variables, and Student’s t-test or the Mann-Whitney test was used for continuous variables. Logistic regression analysis was used to estimate sex-specific differences in in-hospital outcomes. All analyses were performed using Stata version 17 (StataCorp, College Station, TX, USA).
Results
Patient Characteristics
Of 1,518 patients with COVID-19, 693 (45.7%) patients with a history of CVDRF were selected for the analysis in the present study (Figure 1). Of the 693 patients with CVDRF, 64.8% were men and 96.1% were Japanese. The mean age of the 693 patients was 68 years.
Table 1 presents the baseline characteristics of patients with CVDRF stratified by sex. The mean age was significantly higher among women than men. Men were more likely than women to have a history of smoking, diabetes, ischemic heart disease, and chronic lung disease. The prevalence of hypertension and dyslipidemia did not differ significantly according to sex. The use of angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, β-blockers, and antiplatelet agents was comparable between men and women; however, loop diuretic use was significantly higher among women than men.
Table 1. Patient Characteristics on Admission According to Sex
| |
No. patients
with data |
Male
(n=449) |
Female
(n=244) |
P value |
| Age (years) |
693 |
66.2±14.3 |
72.2±15.0 |
<0.001 |
| BMI (kg/m2) |
580 |
24.5±4.8 |
24.0±5.5 |
0.28 |
| Smoking |
655 |
237 (55.2) |
33 (14.6) |
<0.001 |
| Comorbidities |
| Hypertension |
693 |
327 (72.8) |
186 (76.2) |
0.37 |
| Diabetes |
693 |
185 (41.2) |
81 (33.2) |
0.041 |
| Dyslipidemia |
693 |
172 (38.3) |
97 (39.8) |
0.74 |
| Heart failure |
693 |
37 (8.2) |
23 (9.4) |
0.67 |
| Ischemic heart disease |
693 |
64 (14.3) |
21 (8.6) |
0.039 |
| Cardiac arrhythmia |
693 |
44 (9.8) |
26 (10.7) |
0.79 |
| CI/TIA |
693 |
31 (6.9) |
21 (8.6) |
0.45 |
| Chronic lung disease |
693 |
30 (6.7) |
5 (2.0) |
0.006 |
| CKD |
693 |
30 (6.7) |
18 (7.4) |
0.76 |
| Cancer |
693 |
49 (10.9) |
18 (7.4) |
0.14 |
| Baseline medication |
| ACEI/ARB |
693 |
165 (36.8) |
100 (41.0) |
0.29 |
| β-blocker |
693 |
76 (16.9) |
35 (14.3) |
0.39 |
| Loop diuretic |
693 |
28 (6.2) |
28 (11.5) |
0.019 |
| Anticoagulants |
693 |
36 (8.0) |
16 (6.6) |
0.55 |
| Corticosteroids |
693 |
23 (5.1) |
14 (5.7) |
0.73 |
| Symptoms |
| Cough |
693 |
212 (47.2) |
121 (49.6) |
0.58 |
| Sputum |
693 |
79 (17.6) |
46 (18.9) |
0.68 |
| Fatigue |
693 |
157 (35.0) |
71 (29.1) |
0.13 |
| Dyspnea |
693 |
155 (34.5) |
71 (29.1) |
0.15 |
| Anosmia |
693 |
33 (7.3) |
16 (6.6) |
0.76 |
| No symptoms |
693 |
26 (5.8) |
21 (8.6) |
0.21 |
| Physical findings |
| Maximum body temperature (℃) |
644 |
38.1±0.9 |
37.9±0.9 |
0.002 |
| Heart rate (beats/min) |
687 |
87.9±19.0 |
83.6±14.9 |
0.002 |
| Systolic BP (mmHg) |
688 |
132.9±21.8 |
133.3±21.7 |
0.85 |
| Respiratory rate (/min) |
540 |
21.0±6.2 |
20.6±6.0 |
0.44 |
| SpO2 (%) |
689 |
94.8±4.6 |
95.2±5.0 |
0.28 |
| Oxygen on administration |
672 |
174 (40.4) |
88 (36.5) |
0.36 |
Data are given as the mean±SD or n (%). ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; BMI, body mass index; BP, blood pressure; CI, cerebral infarction; CKD, chronic kidney disease; SpO2, peripheral oxygen saturation; TIA, transient ischemic attack.
The most common symptom at the time of admission was cough, which was confirmed in 48.1% of patients; 6.8% of patients did not present any symptoms on admission. The proportions of typical symptoms of COVID-19, such as cough, the presence of sputum, fatigue, dyspnea, and anosmia, did not differ between men and women. Maximum body temperature during hospitalization and baseline heart rate were significantly higher in men, whereas systolic blood pressure, respiratory rate, and peripheral oxygen saturation did not show significant differences according to sex (Table 1).
Laboratory Findings
Table 2 shows laboratory and imaging findings at the time of admission. There was no significant difference in the white blood cell count between men and women, although the proportion of lymphocytes and neutrophils were significantly higher in men than in women. Hemoglobin and hematocrit were higher in men than in women, whereas the platelet count was significantly higher in women. The values of circulating inflammatory biomarkers, such as lactate dehydrogenase, C-reactive protein, and ferritin, were significantly higher in men than in women. Baseline serum albumin concentrations and estimated glomerular filtration rate were comparable between the 2 groups.
Table 2. Examination Findings on Admission According to Sex
| |
No. patients
with data |
Male
(n=449) |
Female
(n=224) |
P value |
| Laboratory findings |
| White blood cells (/μL) |
678 |
5,800 [4,400–7,430] |
5,570 [4,260–7,800] |
0.66 |
| Lymphocytes (%) |
646 |
15.3 [10–22.2] |
18.6 [12–28.2] |
<0.001 |
| Neutrophils (%) |
602 |
76.0 [65.9–83.0] |
73.5 [62.3–81.4] |
0.007 |
| Hemoglobin (g/dL) |
679 |
14.0 [12.2–15.2] |
12.3 [11.3–13.6] |
<0.001 |
| Hematocrit (%) |
667 |
41.0 [36.2–44.2] |
37.2 [33.8–40.8] |
<0.001 |
| Platelets (×104/μL) |
676 |
17.7 [14.0–24.4] |
20.1 [16.1–25.6] |
<0.001 |
| LDH (IU/L) |
617 |
297 [233.0–423.5] |
269 [211.3–379.8] |
0.004 |
| CRP (mg/L) |
667 |
6.7 [2.7–12.4] |
3.8 [0.7–10.2] |
<0.001 |
| Ferritin (ng/mL) |
317 |
701.5 [377.8–1,333.5] |
232.0 [139.0–568.0] |
<0.001 |
| Albumin (g/dL) |
639 |
3.3 [2.8–3.7] |
3.3 [3.0–3.8] |
0.61 |
| eGFR (mL/min/1.73 m2) |
679 |
85.3 [64.8–105.3] |
89.0 [66.7–107.4] |
0.39 |
| Positive cTn |
147 |
56 (52.3) |
23 (57.5) |
0.71 |
| BNP (pg/mL) |
217 |
28.8 [10.3–111.2] |
70.7 [16.9–170.7] |
0.027 |
| Imaging findings |
| Chest X-ray |
| GGO/consolidation/alveolar opacity |
630 |
325 (78.1) |
150 (70.1) |
0.032 |
| Chest CT |
| GGO/consolidation |
543 |
344 (93.2) |
154 (88.5) |
0.068 |
| GGO |
543 |
271 (73.4) |
121 (69.5) |
0.36 |
| Consolidation |
543 |
170 (46.1) |
71 (40.8) |
0.27 |
| Pleural effusion |
543 |
52 (14.1) |
24 (13.8) |
0.99 |
Data are given as the median [interquartile range] or n (%). BNP, brain natriuretic peptide; CRP, C-reactive protein; CT, cardiac tomography; cTn, cardiac troponin; eGFR, estimated glomerular filtration rate; GGO, ground-glass opacity; LDH, lactate dehydrogenase.
A high-sensitivity assay was used to measure cardiac troponin in 129 patients (92.1%). There were no significant difference in cardiac troponin according to sex. Baseline brain natriuretic peptide concentrations were significantly higher in female than male (Table 2).
Imaging Findings
Of the 693 patients with CVDRF, 630 (90.9%) underwent chest radiography and 543 (78.4%) underwent cardiac computed tomography (CT) on admission. The proportion of patients with ground-glass opacity (GGO)/consolidation/alveolar opacity on chest radiography and cardiac CT was 75.4% and 91.7%, respectively. The proportion of patients with GGO/consolidation/alveolar opacity on chest X-ray was significantly higher among men than women. The presence of GGO/consolidation on cardiac CT at the time of admission was also more common in men, but the difference was not statistically significant (P=0.068).
Treatments and In-Hospital Outcomes
Table 3 presents the treatment and in-hospital outcomes of patients after admission. There were no missing data on prognosis during the index hospitalization. During the hospital course, mechanical ventilation, renal replacement therapy, and extracorporeal membrane oxygenation were significantly more prevalent among men than women. The incidence rates of acute kidney injury, pulmonary embolism, and other embolisms were significantly higher among men than women.
Table 3. Treatments and In-Hospital Outcomes According to Sex
| |
No. patients
with data |
Male
(n=449) |
Female
(n=224) |
P value |
| Treatments |
| Mechanical ventilation |
693 |
125 (27.8) |
27 (11.1) |
<0.001 |
| Renal replacement therapy |
693 |
24 (5.3) |
2 (0.8) |
0.002 |
| ECMO |
693 |
23 (5.1) |
2 (0.8) |
0.002 |
| In-hospital outcomes |
| ARDS |
693 |
70 (15.6) |
27 (11.1) |
0.11 |
| Sepsis |
693 |
38 (8.5) |
17 (7.0) |
0.56 |
| Acute kidney injury |
693 |
48 (10.7) |
13 (5.3) |
0.017 |
| MOF |
693 |
32 (7.1) |
10 (4.1) |
0.13 |
| Embolism (any) |
693 |
28 (6.2) |
2 (0.8) |
<0.001 |
| CI/TIA |
693 |
4 (0.9) |
1 (0.4) |
0.66 |
| Pulmonary embolism |
693 |
12 (2.7) |
0 |
0.011 |
| Total hospital LOS (days) |
693 |
24.3±23.7 |
24.1±21.4 |
0.89 |
Data are given as the mean±SD or n (%). ARDS, acute respiratory distress syndrome; CI, cerebral infarction; ECMO, extracorporeal membrane oxygenation; LOS, length of stay; MOF, multiple organ failure; TIA, transient ischemic attack.
In the overall population with COVID-19 and CVDRF (n=693), univariate analysis showed that sex was not significantly associated with in-hospital mortality (odds ratio [OR] 1.22; 95% confidence interval [CI] 0.74–2.02; P=0.43), whereas male sex was significantly associated with higher mortality than female sex in a multivariate analysis model adjusting for age and medical histories (Table 4). Figure 2 shows that the effect of sex on in-hospital mortality differed according to age, and male sex was significantly associated with worse outcomes in older (age ≥80 years) patients. Univariate and multivariate analysis models focusing on older (age ≥80 years) patients showed that male sex was an independent predictor of higher in-hospital mortality (Table 4).
Table 4. Univariate and Multivariate Analysis Models Evaluating the Effect of Sex on In-Hospital Mortality After Adjusting for Age and Medical Histories in the Overall Population and in Elderly (Age ≥80 Years) Patients Separately
| |
Univariate analysis |
Multivariate analysis |
| OR |
95% CI |
P value |
OR |
95% CI |
P value |
| Overall population (n=693, in-hospital deaths, n=108) |
| Male sex |
1.22 |
0.74–2.02 |
0.43 |
2.20 |
1.23–3.92 |
0.008 |
| Age |
1.10 |
1.07–1.12 |
<0.001 |
1.10 |
1.07–1.13 |
<0.001 |
| Hypertension |
1.46 |
0.82–2.60 |
0.20 |
0.88 |
0.46–1.68 |
0.69 |
| Diabetes |
0.70 |
0.43–1.16 |
0.17 |
0.93 |
0.53–1.62 |
0.80 |
| Heart failure |
2.91 |
1.54–5.51 |
0.001 |
0.99 |
0.47–2.08 |
0.98 |
| Coronary artery disease |
2.59 |
1.40–4.79 |
0.002 |
1.63 |
0.81–3.28 |
0.17 |
| Chronic lung disease |
2.41 |
1.06–5.51 |
0.037 |
1.19 |
0.48–2.99 |
0.71 |
| Chronic kidney disease |
3.20 |
1.62–6.36 |
0.001 |
1.96 |
0.90–4.24 |
0.09 |
| Elderly patients (n=172; in-hospital deaths, n=48) |
| Male sex |
2.21 |
1.11–4.41 |
0.024 |
2.55 |
1.22–5.36 |
0.01 |
| Age |
1.05 |
0.98–1.12 |
0.19 |
1.07 |
0.99–1.15 |
0.09 |
| Hypertension |
1.35 |
0.51–3.59 |
0.55 |
– |
– |
– |
| Diabetes |
0.45 |
0.19–1.06 |
0.07 |
– |
– |
– |
| Heart failure |
0.87 |
0.37–2.02 |
0.75 |
0.76 |
0.30–1.89 |
0.55 |
| Coronary artery disease |
1.28 |
0.53–3.06 |
0.59 |
1.16 |
0.45–2.95 |
0.76 |
| Chronic lung disease |
0.93 |
0.28–3.09 |
0.91 |
0.73 |
0.21–2.56 |
0.62 |
| Chronic kidney disease |
1.75 |
0.64–4.83 |
0.28 |
1.64 |
0.56–4.80 |
0.36 |
CI, confidence interval; OR, odds ratio.
Discussion
This study demonstrated sex-specific features and outcomes of patients with COVID-19 and CVDRF using post hoc analysis of CLAVIS-COVID, a nationwide Japanese registry focusing on individuals with COVID-19 and CVDRF. We found that male sex, especially in older (age ≥80 years) patients, was an independent predictor of higher in-hospital mortality in patients with COVID-19 and CVDRF after adjusting for age and medical histories, which are widely acceptable predictors of worse outcomes in COVID-19.2,3,12–14
According to previous reports, approximately 60% of patients with COVID-19 are men, and the fatality rate is higher for men than women (2.8% and 1.7%, respectively).2,7,12 Furthermore, men require intensive care more frequently than women.15,16 In the present study, men had higher requirements for intensive care, such as mechanical ventilation, renal replacement therapy, and extracorporeal membrane oxygenation. A higher proportion of comorbidities, including cardiovascular diseases, may be associated with worse clinical courses and outcomes in men than in women, similar to findings reported previously.1,17
We could not reveal the reason behind the increased death rate in older men with COVID-19 and CVDRF than in women; however, some previous studies proposed hypotheses related to the occurrence of COVID-19.1,18 Of these hypotheses, differences in the immune response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are considered one of the important factors contributing to the clinical course in each sex. In general, women have more robust immune systems than men. Estrogen and X chromosomes in women play a key role in the development of a stronger response to infectious disease.18 Women are protected by stronger immune responses against viruses and exhibit superior immune-mediated tissue repair capacities than men.5,19 Similarly, proinflammatory innate immunity chemokines and cytokines, such as interleukin (IL)-8, IL-18, and chemokine (C-C motif) ligand 5 (CCL5), are higher in men than women with COVID-19.20 The T cell response to SARS-CoV-2 is more robust in women, and an increase in CD8 T cells compared with that in healthy volunteers is observed only in women.20 These immunological differences between men and women may be associated with the different clinical courses and outcomes of COVID-19. Furthermore, the men had higher levels of C-reactive protein, lactate dehydrogenase, and ferritin, as well as higher rates of pulmonary complications at the time of admission, suggesting higher inflammation status in men than in women.
The T cell response to SARS-CoV-2 is negatively correlated with patient age in men, whereas the association between immune response and aging is not observed in women.20 In addition, men aged >65 years have a relative deficiency of proinflammatory genomic signatures and plasma concentrations of inflammatory cytokines, such as IL-6.21 The immunological background of vulnerability in older men leads to significantly higher in-hospital mortality. The weak response to SARS-CoV-2 supports the hypothesis that older men are expected to be good therapeutic targets for vaccines and therapies to increase their immune responses to SARS-CoV-2. Furthermore, given that the COVID-19 mortality rate is higher in patients with than without CVDRF,2,12,14 these specific prevention and treatment strategies for COVID-19 may be more beneficial in older men with CVDRF, which is a more vulnerable population.
Study Limitations
This was a retrospective study, therefore we could not assess a considerable number of baseline serum biomarkers. The relatively small sample size compared with other nationwide registries in other countries6,8,22 may have led to statistical non-significance in the univariate analysis model that evaluated the effect of sex on outcomes in patients with CVDRF. In addition, the Japanese government mandated the hospitalization of all patients with COVID-19 regardless of disease severity during patient enrollment, which may have consequently been associated with different prognosis in Japan.23
Conclusions
This post hoc analysis of the CLAVIS-COVID registry revealed that male sex, especially among older patients, was an independent predictor of higher in-hospital mortality. Older men constitute a specific population that is vulnerable to COVID-19; therefore, strict prevention and management strategies against COVID-19 are needed for this group.
Sources of Funding
This CLAVIS-COVID registry received financial supports from the Japanese Circulation Society.
Disclosures
T.Y. is associated with endowed departments of Abbott Vascular Japan, Boston Scientific Japan, Japan Lifeline, WIN International, and Takeyama KK. S. Kohsaka has received unrestricted research grants from the Department of Cardiology, Keio University School of Medicine provided by Daiichi Sankyo Co., Ltd. and Bristol-Meyers Squibb, as well as lecture fees from AstraZeneca and Bristol-Meyers Squibb. Y.I. has received lecture fees from Asteras, Amgen Biopharma, AstraZeneca, Sanofi, Daiichi Sankyo Co., Ltd., Bayer, and Bristol Myers Squib, as well as research grants from Boston Scientific, Daiichi Sankyo Co., Ltd., and Japan Mediphysics. Y.M. is affiliated with a department endowed by Philips Respironics, ResMed, Teijin Home Healthcare, and Fukuda Denshi, and has received honoraria from Otsuka Pharmaceutical Co. and Novartis Japan, consultant fees from Otsuka Pharmaceutical Co., and joint research funds from Otsuka Pharmaceutical Co. and Pfizer Inc.
Y.I., S. Kohsaka, and K.N. are members of Circulation Reports’ Editorial Team.
Data Availability
The deidentified participant data will not be shared.
References
- 1.
Bienvenu LA, Noonan J, Wang X, Peter K. Higher mortality of COVID-19 in males: Sex differences in immune response and cardiovascular comorbidities. Cardiovasc Res 2020; 116: 2197–2206.
- 2.
Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical characteristics of COVID-19 in New York City. N Engl J Med 2020; 382: 2372–2374.
- 3.
Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ 2020; 11: 29.
- 4.
Jin JM, Bai P, He W, Wu F, Liu XF, Han DM, et al. Gender differences in patients with COVID-19: Focus on severity and mortality. Front Public Health 2020; 8: 152.
- 5.
Bunders MJ, Altfeld M. Implications of sex differences in immunity for SARS-CoV-2 pathogenesis and design of therapeutic interventions. Immunity 2020; 53: 487–495.
- 6.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 323: 1239–1242.
- 7.
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol 2020; 92: 577–583.
- 8.
Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Cardiovascular disease, drug therapy, and mortality in COVID-19. N Engl J Med 2020; 382: e102.
- 9.
Bugiardini R, Bairey Merz CN. Angina with “normal” coronary arteries: A changing philosophy. JAMA 2005; 293: 477–484.
- 10.
Regitz-Zagrosek V, Kararigas G. Mechanistic pathways of sex differences in cardiovascular disease. Physiol Rev 2017; 97: 1–37.
- 11.
Ohira T, Iso H. Cardiovascular disease epidemiology in Asia: An overview. Circ J 2013; 77: 1646–1652.
- 12.
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382: 1708–1720.
- 13.
Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA 2020; 323: 1574–1581.
- 14.
Matsumoto S, Kuroda S, Sano T, Kitai T, Yonetsu T, Kohsaka S, et al. Clinical and biomarker profiles and prognosis of elderly patients with coronavirus disease 2019 (COVID-19) with cardiovascular diseases and/or risk factors. Circ J 2021; 85: 921–928.
- 15.
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med 2020; 8: 475–481.
- 16.
Yoshida N, Iwata S, Ogawa M, Izawa KP, Kuroda S, Kohsaka S, et al. Intensive care unit admission for moderate-to-severe COVID-19 patients with known cardiovascular diseases or their risk factors: Insights from a nationwide Japanese cohort study. Circ Rep 2021; 3: 375–380.
- 17.
Pastor-Barriuso R, Perez-Gomez B, Hernan MA, Perez-Olmeda M, Yotti R, Oteo-Iglesias J, et al. Infection fatality risk for SARS-CoV-2 in community dwelling population of Spain: Nationwide seroepidemiological study. BMJ 2020; 371: m4509.
- 18.
Papadopoulos V, Li L, Samplaski M. Why does COVID-19 kill more elderly men than women? Is there a role for testosterone? Andrology 2021; 9: 65–72.
- 19.
Vom Steeg LG, Klein SL. Sex and sex steroids impact influenza pathogenesis across the life course. Semin Immunopathol 2019; 41: 189–194.
- 20.
Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature 2020; 588: 315–320.
- 21.
Marquez EJ, Chung CH, Marches R, Rossi RJ, Nehar-Belaid D, Eroglu A, et al. Sexual-dimorphism in human immune system aging. Nat Commun 2020; 11: 751.
- 22.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020; 323: 2052–2059.
- 23.
Matsunaga N, Hayakawa K, Terada M, Ohtsu H, Asai Y, Tsuzuki S, et al. Clinical epidemiology of hospitalized patients with COVID-19 in Japan: Report of the COVID-19 Registry Japan. Clin Infect Dis 2021; 73: e3677–e3689.