2018 年 4 巻 4 号 p. 97-102
2018 年 4 巻 4 号 p. 97-102
Objective: Accidents that occurred during rehabilitation training were retrospectively analyzed to understand the risks involved in rehabilitation training.
Methods: Subjects were 33,905 patients who underwent rehabilitation training at an acute-care hospital over an 8-year period. In total, 457 accidents occurred during rehabilitation training and were analyzed. Data collected were: accident incidence rate, patient’s position/behavior at the time of the accident, state of assistance/supervision by the therapist in charge, and annual number of accidents per therapist by years of experience.
Results: Most accidents that occurred during rehabilitation training involved bleeding, falls, and route-related accidents (accidents related to use of catheters, intravenous lines, or nasogastric tubes), in that order. Half of the accidents occurred in a training room. Bleeding was associated with a variety of behaviors, including lying, sitting, and walking, and 40% of falls occurred while walking. Examination of the number of accidents per therapist by years of experience showed patients tended to experience accidents when being assisted/supervised by therapists with 1–4 years of experience.
Conclusions: Many accidents that occurred during rehabilitation training at this acute-care hospital involved bleeding or falls. Accidents were more common when a therapist with only a few years of experience was conducting the training.
Rehabilitation training is intrinsically a high-risk field. Most patients needing such training have some kind of musculoskeletal disorder, and systemic complications are common. It has also been reported that patients with cognitive dysfunction are often unable to manage risk properly.1 The main objectives of rehabilitation training are maximizing patients’ abilities and helping them rebuild their lives so that they can participate in society. Reacquiring or improving the ability to walk is often an important goal of rehabilitation training. Progress from being unable to stand to being able to walk, involves a stage in which the patient walks unsteadily.2 A patient’s range of life activities also expands when impairments improve in the acute and recovery stages, which is another time when the risk of falling increases. Moreover, in acute-care hospitals where patients are often in an unstable condition, patients’ physical status is changeable, even before and after training. Therefore, there must be a trade-off between expanding activities and minimizing risk.
A variety of research has been conducted on falls during rehabilitation training, from the acute stage to home care.2–22 This includes analyses of factors related to falls, reports on initiatives for preventing falls, and studies on the fear of falling. Falls have been reported in hospital settings, at home, and outdoors. Various other accidents may occur in addition to falls, including bleeding, bruising, and aspiration; however, there are few available reports on accidents other than falls.
This study clarified the risks involved in rehabilitation training by retrospectively analyzing falls and other accidents that occurred during rehabilitation training based on accident reports submitted by therapists at an acute-care hospital.
Data for 33,905 patients who underwent rehabilitation training from April 1, 2007, to March 31, 2015 were extracted from the Fujita Health University Hospital database. A breakdown based on medical compensation subdivisions showed there were: 15,161 cerebrovascular patients, 4,863 post-cerebrovascular accident or disuse syndrome patients, 6,907 patients with musculoskeletal disorder I, 2,057 patients with musculoskeletal disorder II, 4,635 patients with diseases of the respiratory system, and 282 patients with cancer. With one unit defined as 20 min of rehabilitation training, study subjects received 1,866,255 units in total.
Analysis conditionsInformation was obtained from reports submitted when accidents occurred, including: number of accidents, content, medical accident level, location, time, patient’s posture/behavior, state of assistance/supervision by the therapist in charge, and years of experience of the therapist in charge.
Incidence rate and contentThe accident incidence rate was calculated by dividing the total number of accidents over the 8-year period by the total number of units over the same period to determine the incidence rate per thousand units. The proportion of each type of accident (content) was calculated based on the total number of accidents.
Category of medical accidentPercentages by level of accident were calculated based on the classification of medical accident level at Fujita Health University Hospital (Table 1).
| Level | Patient impact level |
|---|---|
| 0 | When an error occurred or a medical product or piece of equipment malfunctioned but was not used on the patient. |
| 1 | When an error occurred or a medical product or piece of equipment malfunctioned and was used on the patient, but did not cause any harm. |
| 2 | When a change in the patient’s vital signs was observed that necessitated an examination. |
| 3a | When mild therapy or treatment was necessary (e.g., disinfection, compress, anesthetic). |
| 3b | When intensive therapy or treatment was necessary (e.g., unplanned therapy or treatment, hospitalization, prolongation of hospitalization). |
| 4 | When permanent aftereffects occurred. |
| 5 | When death occurred (except if due to a primary disease or natural course). |
| Complaint | Different from a medical accident. When a patient complained about something despite the absence of negligence/malpractice by a medical care provider. |
The place of accident occurrence was classified as: the training room where the rehabilitation training was conducted, bedside, corridor, outdoors, and others. The percentage of accidents in each place was calculated. Proportions of accident by time period were calculated on a per-hour basis from 09:00 to 18:00, which were the hours when rehabilitation training was conducted.
Patient and therapist statusProportions for accidents involving each category of posture/behavior of the patient (e.g., walking, standing, sitting) at the time of the accident were calculated. The assistance/supervision status of the therapist in charge at the time of the accident was calculated as percentages in terms of assistance (maximum, moderate, mild), surveillance (close, distant), and others.
Accidents per therapist by years of experienceThe number of accidents per therapist was calculated as the average number of annual accidents by the number of years of experience.
Relationship between patient’s posture/behavior and accident contentTo evaluate the relationship between the accident content and patient posture/behavior, proportions for each type of posture/behavior were calculated for falls, bleeding, and route-related accidents.
Data analysisThe percentages for the accident occurrence rate and content, category of medical accident, place and time of occurrence, status of patient and therapist, number of accidents per therapist, and the relationship between patients’ posture/behavior and accident content were calculated. A comparative study was then conducted.
Definition of medical accidentThe Fujita Health University Hospital defines medical accidents as “All accidents that resulted in injury or death that were caused by a medical act performed by a medical care provider or medical institution’s equipment or systems. They include not only accidents that occurred from negligence by a provider or manager but also those that were beyond human control. They also include accidents that resulted in harm to a provider. Harm to a patient caused by a provider’s negligence is considered medical malpractice.” Based on this definition, there are seven medical accident level categories that reflect the degree of impact to the patient or victim (Table 1). Complaints were excluded from this study.
Ethical considerationsThis study was conducted after being screened and approved by the Ethics Committee at Fujita Health University Hospital (No. HM17-083). As the accident reports at the time of rehabilitation training were retrospectively analyzed and only data that could be concatenated anonymously were used, informed consent was not required. To secure opportunities for opting-out of this study, the following items are described on the Fujita Health University, University Rehabilitation Division website.
Over the 8-year study period, 457 accidents occurred during rehabilitation training, giving a mean annual incidence rate of 0.24‰ per unit (Figure 1). Bleeding was the most common type of accident during rehabilitation training (32.6%), followed by falls (30.6%), route-related accidents (20.8%), and other accidents (16.0%). Other accidents included pain and performing non-prescribed training.

Number of accidents and incidence rates. Over the 8-year study period, 457 accidents occurred during rehabilitation training, giving a mean annual incidence rate of 0.24‰ per unit.
Analysis by medical accident level showed 96.7% were level 1, 2.2% were level 2, and 1.1% were level 3b. Level 3b accidents included instances of swelling or pain that appeared after training, and in which radiography showed either fracture or dislocation.
Place and time of occurrenceIn 56.0% of accidents, the accident location was a rehabilitation training room, followed by bedside (21%), a hallway (5.0%), outdoors (2.0%), and others (16.0%). Other locations included the rehabilitation training reception desk and on the stairs. Of accidents in rehabilitation training rooms, 56.6% occurred in a physical therapy room, 38.7% in an occupational therapy room, and 4.7% in a speech and language therapy room.
The timing of accidents varied: 12.1% of accidents occurred during 09:00–9:59, 15.1% during 10:00–10:59, 17.9% during 11:00–11:59, 7.1% during 12:00–12:59, 9.9% during 13:00–13:59, 13.5% during 14:00–14:59, 3.0% during 15:00–15:59, 9.3% during 16:00–16:59, and 2.1% during 17:00–17:59. Accidents occurred most frequently in the period during 11:00–11:59, followed by 10:00–10:59 and 14:00–14:59.
Patient and therapist statusThe patient’s posture/behavior when the accident occurred was most frequently walking (20.0% of accidents), followed by reclining (16.7%) and sitting (14.7%) (Figure 2). When the accident occurred, the therapist in charge was supervising the patient in 47.6% of accidents, assisting the patient in 36.2% of accidents, and doing something else in 16.2% of accidents. This indicates that about half of the accidents occurred under supervision, 39.5% under close supervision and 8.1% under distant supervision. Of the accidents that occurred when the therapist was providing assistance, 15.6% occurred during maximum assistance, 14.0% during mild assistance, and 6.6% during moderate assistance.
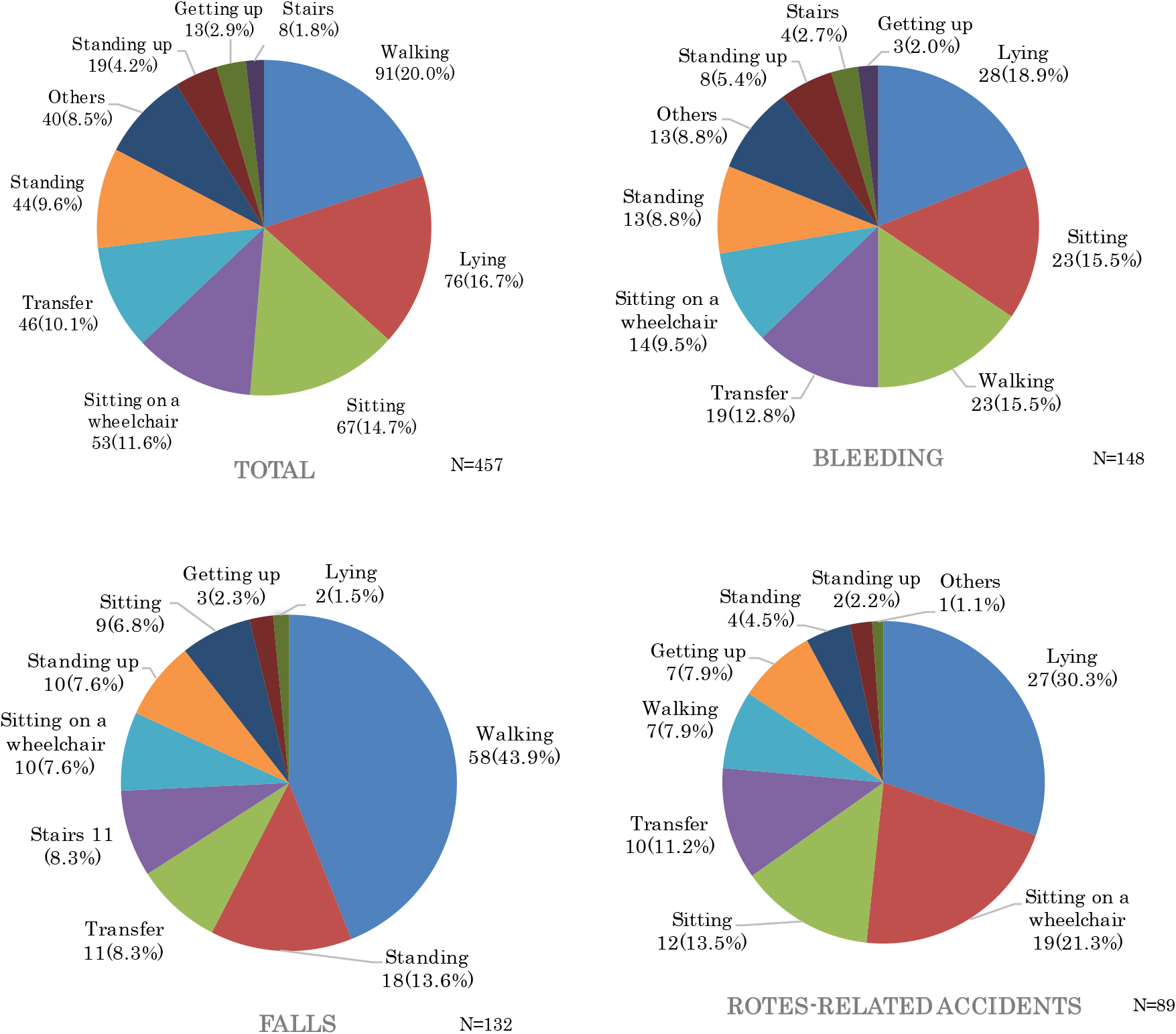
Patients’ posture/behavior at the time of accidents. Bleeding, falls, and route-related accidents differed in terms of the relationships between type of accident and posture/behavior.
Analysis of the number of accidents per therapist by years of experience showed that there were 1.36 accidents per therapist for those in year 1, 1.23 in year 2, 1.21 in year 3, 1.22 in year 4, 0.61 in year 5, and 0.53 in year 6 or more (Figure 3). The number of accidents per therapist was higher for therapists with 1–4 years of experience but tended to decrease once therapists reached 5 years of experience.
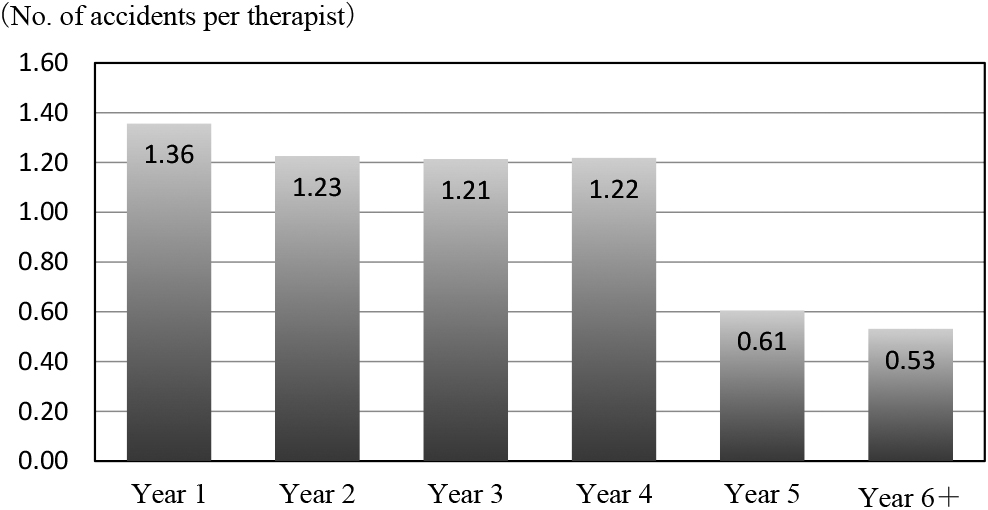
Annual number of accidents per therapist by years of experience. Patients tended to experience accidents when the therapists helping or supervising them had 1–4 years of experience.
Evaluation of the relationship between accident content and patients’ posture/behavior showed that 43.9% of falls occurred during walking, 13.6% when standing, and 8.3% during transfers or when going up/down stairs. For accidents involving bleeding, 18.9% of accidents occurred while lying, 15.5% while sitting or walking, and 12.8% during transfers. For route-related accidents, 30.3% of accidents occurred while lying, 21.3% while sitting on a wheelchair, and 13.5% while sitting (Figure 2).
Falls are defined in several ways. In 1987, the Kellogg International Working Group on the Prevention of Falls in the Elderly defined a fall as “unintentionally coming to ground or some lower level not as a consequence of sustaining a violent blow, loss of consciousness, or sudden onset of paralysis as in stroke or an epileptic seizure.” This definition became the foundation for research on preventing falls in older adults.3,4
In Japan, the Tokyo Fire Department describes three categories of falls: falls in the narrow sense of the word, falls, and drops.5 A fall in the narrow sense is defined as when a person “steps, stumbles, or slips on the same surface.” A fall is defined as occurring when a person is “injured by falling from a location of a different altitude to the ground or a stationary surface, or by tumbling while in contact with a slope or other surface.” Finally a drop is defined as a person “injured from falling from a high place to the ground or a stationary surface.” Furthermore, Suzuki et al.6 defined a fall as “unintentionally falling to the ground, floor, or some other low position, but excluding the intentional changing of the body position to sit or lie down on a piece of furniture, wall, or other object.” The Department of Rehabilitation Training in our hospital defines a fall as: “when a part of the body besides the soles of the feet unintentionally falls to the ground, floor, or other low position.”
Falls, even mild ones, can impede daily activities by creating a fear of falling. This is called “post-fall syndrome” and can delay progress in rehabilitation training. In addition, fractures due to falls are reported to be the third leading cause of people becoming bedridden.19 In Japan, falls are estimated to cost 340–500 billion JPY in medical and care expenses, highlighting that falls are a problem that cannot be ignored.20 Therefore, prevention is important, and considerable research on falls has been conducted.
The present study showed that falls were common among the accidents that occurred during rehabilitation training, which suggests there is a high risk for falling in the acute stage and until patients return to their community life. In most cases, the therapist was able to support the patient to prevent the fall from becoming serious. However, some falls caused pain and required radiography examination, and other falls caused bleeding that required treatment.
In 2003, a fact-finding survey was conducted involving 333 institutions that had received training certification from the Japanese Association of Rehabilitation Medicine. The survey examined areas such as the safety management and training systems of participating institutions (overall and in their rehabilitation training departments), safety problems by occupation, and involvement in safety management of rehabilitation training-related occupations. The survey found that falls were the most common type of accident, with other accidents including orthostatic hypotension, route-related accidents, accidents associated with physical therapy, and accidents during exercise therapy.1
In the present study involving an acute-care hospital, bleeding was the most common accident, followed by falls, and route-related accidents. In many cases, bleeding occurred when a patient’s leg struck a wheelchair footplate or the bed when transferring from the wheelchair to the bed, when a patient’s arm or leg struck a bed rail or wall when getting out of bed, or when a wound began bleeding during training. Many of the route-related accidents in this study occurred when patients who were not fully alert pulled out intravenous drips or nasogastric tubes because they found them uncomfortable, or when an intravenous drip or urinary catheter was pulled out during transfer from a wheelchair to a bed. The frequency of these kinds of route-related accidents suggests they are characteristic of acute-care hospitals.
The annual number of accidents per therapist by years of experience in this study showed that patients tended to experience accidents when the therapists assisting or supervising them had 1–4 years of experience. Accidents were more common for therapists in the first year of experience compared with the second to fourth years of experience. This suggests a correlation between therapists’ years of experience and the accident incidence rate. A survey by Kubo et al.24 that examined accident rates by therapists’ years of experience found a 36.7% accident rate in the first year and a 12.4% rate thereafter. They suggested that the high rate of accidents during rehabilitation training among first-year therapists indicates that lack of skill in technical aspects makes accidents more likely. However, in the present study, even therapists with more than 5 years of experience had an accident rate of one accident every 2 years.
Although several studies found that accidents during rehabilitation training are more common among less experienced therapists,23–27 the results of the present study indicate that accidents happen even to experienced therapists (with 5 or more years of experience). As therapists gain experience, they are asked to handle more severe cases, which could be a reason accidents still occur among therapists with 5 or more years of experience.
Among the bleeding, falls, and route-related accidents that were most common at this acute-care hospital, there were differences in terms of patients’ postures and activities when the accidents occurred. Bleeding occurred in a variety of postures and activities, but 40% of falls occurred while walking. Half of the route-related accidents occurred while lying (30%) or during activities when seated on a wheelchair (20%). Bleeding occurred frequently in locations where the skin was not covered by clothing. Patients with thin or fragile skin may bleed from a small amount of friction, which is thought to be why bleeding occurs in a variety of postures. Before rehabilitation training, it is important to protect patients’ skin and create an environment where their arms and legs will not come into contact with walls, rails, or other objects during movements.
Falls often occurred while walking, indicating that walking can be considered a high-risk movement. Inoue et al.12 reported that “Falls are often caused by a patient’s impediments, and can occur due to multiple factors, particularly those related to the patient.” Furthermore, Hiyama9 noted that “Situations that involve a high risk of falling are daily activities and behaviors in which postural control is impeded. Impediments to postural control include gait disorders, symptoms, and the effects of drugs.”
Route-related accidents often occurred while reclining or sitting. At our acute-care hospital, rehabilitation training begins a few days after disease onset, so training is often conducted while intravenous drips, catheters, and other routes are in place. If a therapist moves a patient’s body without properly managing the attached tubes or catheters, one or more tubes or catheters may be pulled out. Furthermore, rehabilitation training is often started after surgery when patients are not fully awake. Because they are unable to make proper judgments, they sometimes pull out their own nasogastric tubes or intravenous drips if they feel uncomfortable. The present findings showed that patients’ postures and activities were related to the types of accidents that occurred, which suggests that risks can be anticipated based on a patient’s posture or activity.
A limitation of this study was that the annual accident incidence per unit (20 min) was calculated as the rate per thousand. The accident incidence rate based on the amount of training performed per patient from the start to completion of rehabilitation training was not determined. Therefore, it was not possible to analyze when accidents were more likely to occur, whether the amount of training affected the frequency of accidents, and similar factors. Moreover, while the accident incidence rates were calculated by therapists’ years of experience, individual therapists were not followed to determine if a therapist who was present at an accident during rehabilitation training was able to prevent further accidents in the future.
In a future study, we would like to determine incidence rates for accidents that occur during rehabilitation training at the bedside and in training rooms by disease and symptom categories and to analyze incidence rates for accidents that occur during range-of-motion training, strength training, thermotherapy, activities of daily living training, and other forms of rehabilitation training. Such research would help in predicting risks before rehabilitation training begins and could reduce accident incidence rates.
Analysis of accidents that occurred during rehabilitation training showed that many accidents involved bleeding, falls, and routes. Furthermore, an analysis of accidents per therapist by years of experience showed that many accidents occurred during rehabilitation training with therapists with fewer years of experience. However, accidents still occurred at a rate of one every 2 years among therapists with 5 or more years of experience.
The authors report no conflicts of interest.
The authors sincerely thank Masaki Kato, Head of the Department of Rehabilitation at Fujita Health University Hospital, for his assistance and advice in conducting this study. The authors would also like to thank the physical, occupational, and speech therapists in the Department of Rehabilitation at Fujita Health University Hospital for creating the rehabilitation training accident reports. Finally, the authors thank Audrey Holmes, MA, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.