2017 Volume 63 Issue 2 Pages 100-105
2017 Volume 63 Issue 2 Pages 100-105
Objective: To investigate the accuracy of cone beam CT (CBCT) to diagnose non-invasive chronic fungal rhinosinusitis.
Methods: Preoperative CT evaluation of non-invasive chronic fungal rhinosinusitis was performed by CBCT (3D Accuitomo 170®) and traditional multidetector CT (MDCT) (Aquilion 32®) in 13 and 38 patients with non-invasive chronic fungal maxillary sinusitis, respectively, in different facilities. Detection of intrasinus calcification was compared between these two groups.
Results: Detection of intrasinus calcification in patients with non-invasive chronic fungal maxillary sinusitis was higher in the MDCT group (84.2%) than the CBCT group (46.2%).
Conclusion: CBCT is inferior to MDCT in detection of intrasinus calcification in patients with non-invasive chronic fungal maxillary sinusitis. CBCT is frequently used in the screening of the paranasal lesion, but it is not enough to evaluate non-invasive chronic fungal maxillary sinusitis alone.
Study design: Retrospective study.
Cone beam CT (CBCT) consists of a cone-shaped X-ray beam and flat panel detector that moves around the patient’s head1). In Japan, a prototype CBCT (Ortho-CT) was developed in 19972) and its practical use was started in 2001, initially for dental imaging. Today, CBCT is widely used for otologic and rhinologic examination. CBCT provides higher resolution images with less radiation exposure than conventional multidetector CT (MDCT). Although CBCT is able to detect odontogenic maxillary sinusitis3), there is no data showing the accuracy of CBCT findings for the diagnosis of non-invasive chronic fungal rhinosinusitis. Intrasinus calcification is a common finding of fungal sinusitis, especially of aspergillosis4-7). To investigate the detection of intrasinus calcification in CBCT findings, we conducted a comparative study of CBCT findings and MDCT findings in patients with non-invasive chronic maxillary sinusitis.
Thirteen adult patients (four men, nine women) with non-invasive chronic fungal maxillary sinusitis who visited Fukushima Medical University Aizu Medical Center (FMU-AMC) from May 2013 to November 2015, and 38 adult patients (19 men, 19 women) with the same disease who visited Fukushima Medical University Hospital (FMUH) from January 2000 to December 2009 were selected8). CBCT was performed in FMU-AMC patients (CBCT group), and MDCT was performed in FMUH patients (MDCT group) before endoscopic sinus surgery (ESS). The average age of the CBCT group was 71.2 ranging from 43 to 84 years and that of the MDCT group was 66.4 ranging from 30 to 80 years. The average age showed no significant difference between the two groups (p=0.16, t-test).
CBCT was performed using 3D Accuitomo 170® (J. Morita Mfg. Corp., Kyoto, Japan) under the following conditions: tube voltage, 80 kV; tube current, 8 mA; voxel, 0.25 mm × 0.25 mm × 0.25 mm; slice thickness, 1 mm; exposure time, 17.5 sec.; rotation, 360 degrees. CT images of the paranasal sinuses were taken as a column with a diameter of 14 cm and a height of 10 cm.
MDCT was performed using Aquilion 32® (Toshiba Medical Systems, Otawara, Japan) under the following conditions: tube voltage, 135 kV; tube current, 260 mA; rotation time, 0.5 sec; helical pitch, 21; C-FOVS (max 24 cm); slice thickness, 0.5 mm.
All CT examinations were conducted without contrast material and evaluated in the axial plane parallel to the hard plate, and in the coronal planes perpendicular to the hard plate. CBCT and MDCT images were obtained with the patient sitting and lying prone, respectively.
Intrasinus calcification was considered to be present if the focal CT attenuation was higher than the surrounding inflammatory soft tissue and fluid in the maxillary sinus. Intrasinus calcification was considered to be absent when the calcification was not found even if viewer’s window level (brightness) and window width (contrast) were changed to optimize the image.
Hounsfield Unit (HU) of intrasinus calcification was measured using DICOM viewer Array AOC (Array Corporation, Tokyo, Japan). Region of interest was placed within the calcification. Mean HU was used as a HU of each case.
MRI was also performed in both groups when there was no intrasinus calcification or when further evaluation of maxillary sinus was required.
Pathological diagnoses of fungal sinusitis were made using hematoxylin-eosin stain as a routine staining, and Periodic acid-Schiff stain and Grocott stain as needed.
If CBCT or MDCT findings demonstrated signs of invasive fungal sinusitis (e.g. massive bone destruction, orbital invasion, and intracranial extension), the patient was excluded from the study.
Fisher’s exact test was used for statistical analysis of the detection of intrasinus calcification. Student-t test was used for the analysis of HU. Differences were considered to be statistically significant if p<0.05.
All the study protocols were approved by the ethical committee in Fukushima Medical University.
Intrasinus calcification was present in six of the 13 patients (46.2%) and 32 of the 38 patients (84.2%) in the CBCT and MDCT groups, respectively. Detection of intrasinus calcification was higher in the MDCT group (p=0.01) (Table 1). The CT and MRI findings in the CBCT group are summarized in Table 2, which also includes MDCT findings of the following patients; four patients who had been received MDCT by neighborhood otolaryngologists before the referral and two patients who received MDCT (Aquilion ONE®) to confirm the absence of intrasinus calcification as that was not detected on CBCT.
In the MDCT group, MRI was performed in 28 patients, which revealed hypointense signals on T1-weighted images, and hypointense signals or signal void areas on T2-weighted images in all patients (100%). Those findings were compatible with fungal sinusitis. Among the 28 patients, intrasinus calcification was detected on MDCT in 25 patients (89.3%).
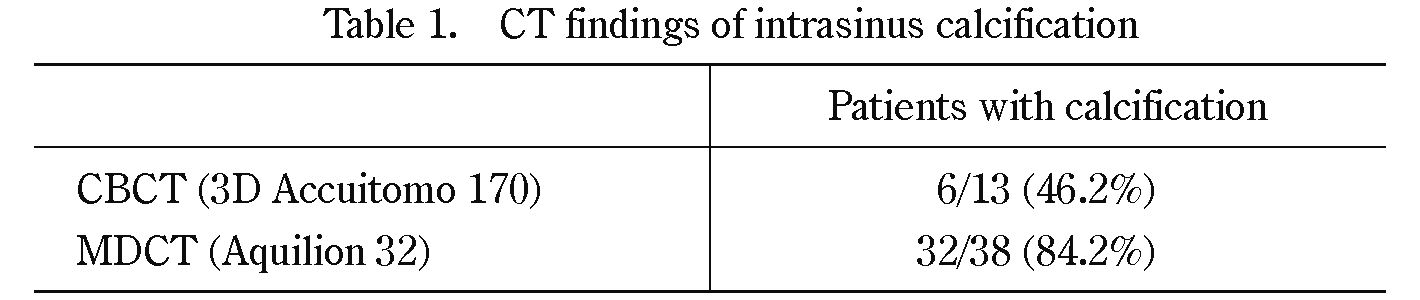
CT findings of intrasinus calcification
(P=0.011<0.05, Fisher’s exact test)
In the CBCT group, pathological diagnoses were aspergillosis in 12 patients (92.3%) and non-specific fungal sinusitis in 1 patient (7.7%). In the MDCT group, aspergillus was found in 27 patients (71.1%), candida was found in 6 patients (15.8%), and mucor was found in 5 patients (13.2%). All the pathological diagnoses were non-invasive chronic fungal sinusitis in both CT groups.
HUMean HU of intrasinus calcification in CBCT group was 796±300, and that in MDCT group was 398±207. HU of intrasinus calcification is higher in CBCT group than that in MDCT group (p=0.02) (Fig. 1).
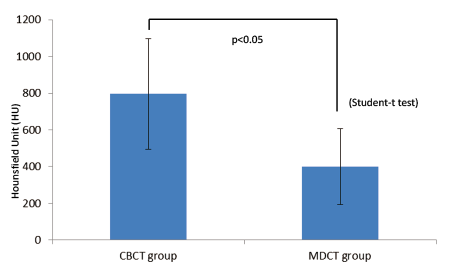
Hounsfield Unit of intrasinus calcification is higher in CBCT group than that in MDCT group. (Mean ± SD)
CT findings for intrasinus calcification in fungal sinusitis were first reported by Kopp et al. in 19854). In previous literature using conventional CT (non-CBCT), the detection of intrasinus calcification in fungal sinusitis cases was reported to be between 51 and 77%4-7). In the present study, 46.2% of patients in the CBCT group showed intrasinus calcification, which is lower than that reported in previous studies.
By using CBCT, it is possible to obtain high resolution images with a minimum voxel size of 80 μm (3D Accuitomo 170®). Moreover, the level of radiation exposure to the head and neck region is less than one-seventh of that from a conventional CT scan9). Compared to MDCT, CBCT has better spatial resolution, but limited contrast resolution. There are three possible reasons for this. First, the flat panel detector in CBCT has a wide surface area, and tends to detect more scattered radiation than the detector used for MDCT. Scattered radiation causes image noise, limits the signal-to-noise ratio, and lower the contrast resolution. Second, the level of radiation exposure in CBCT is lower than that of MDCT, but basically, low radiation dose increase in image noise. Image noise tends to be worse if there are fewer x-ray photons passing through the voxel. In CBCT, the voxel size is smaller (spatial resolution is higher), and radiation exposure is lower than MDCT, resulting in fewer x-ray photons passing through the voxel. Third, using CBCT, influence of radiation absorption outside the field of view (especially the absorption by bone) could not be calculated. This may increase the noise in CBCT. The limited contrast resolution makes it difficult to differentiate calcification from surrounding soft tissue and fluid. These mechanisms make the detectability of intrasinus calcification lower in CBCT than MDCT.
Although it is not the direct comparison of CBCT and MDCT using the same patients, density of intrasinus calcification in CBCT group was higher than that in MDCT group (Fig. 1). Limited contrast resolution could be the reason of the result, because if the density of calcification is low in CBCT, it could be difficult to distinguish calcification from surrounding soft tissue. In other words, there is a possibility that CBCT could not detect faint calcification. Indeed, in three patients of CBCT group (23.1%), CBCT could not detect calcification but MDCT could (Table 2). In these cases, mean HU of calcification detected by MDCT was 118±45.
Zinreich et al. reported that remarkably hypointense signals on T2-weighted images were characteristic MRI findings of the fungal sinusitis5). In our study, nine out of the 13 patients in the CBCT group and 28 out of 38 patients in the MDCT group underwent MRI, and all the patients showed hypointense signals or signal void areas on T2-weighted images. Although sensitivity of these MRI findings was 100% in our series, the sensitivity of MRI in the previous literature varies from 50%10) to 100%5,11). As Nicolai and Nomura mentioned, these MRI findings is not specific to fungus ball. The presence of air, acute hemorrhage or eosinophilic mucin might decrease the signal intensity in T2-weighted images10,11). In our series, these factors decreasing the signal intensity in T2-wheighted images were excluded from preoperative CT images, intraoperative findings and pathological diagnoses. In our facility, CBCT is conducted as the first step of image evaluation for sinusitis due to the low radiation dose and excellent spatial resolution of bone lesions. MRI is performed as the second step when intrasinus calcification is absent or detailed soft tissue evaluation is necessary (Fig. 2). If intrasinus calcification is not found on CBCT findings, MDCT is not the second choice because radiation exposure will be higher if both CBCT and MDCT are performed. At present, MDCT as the second step is justified only when MRI is contraindicated or malignancy is highly suspected. In these settings, MDCT should be performed with contrast medium.
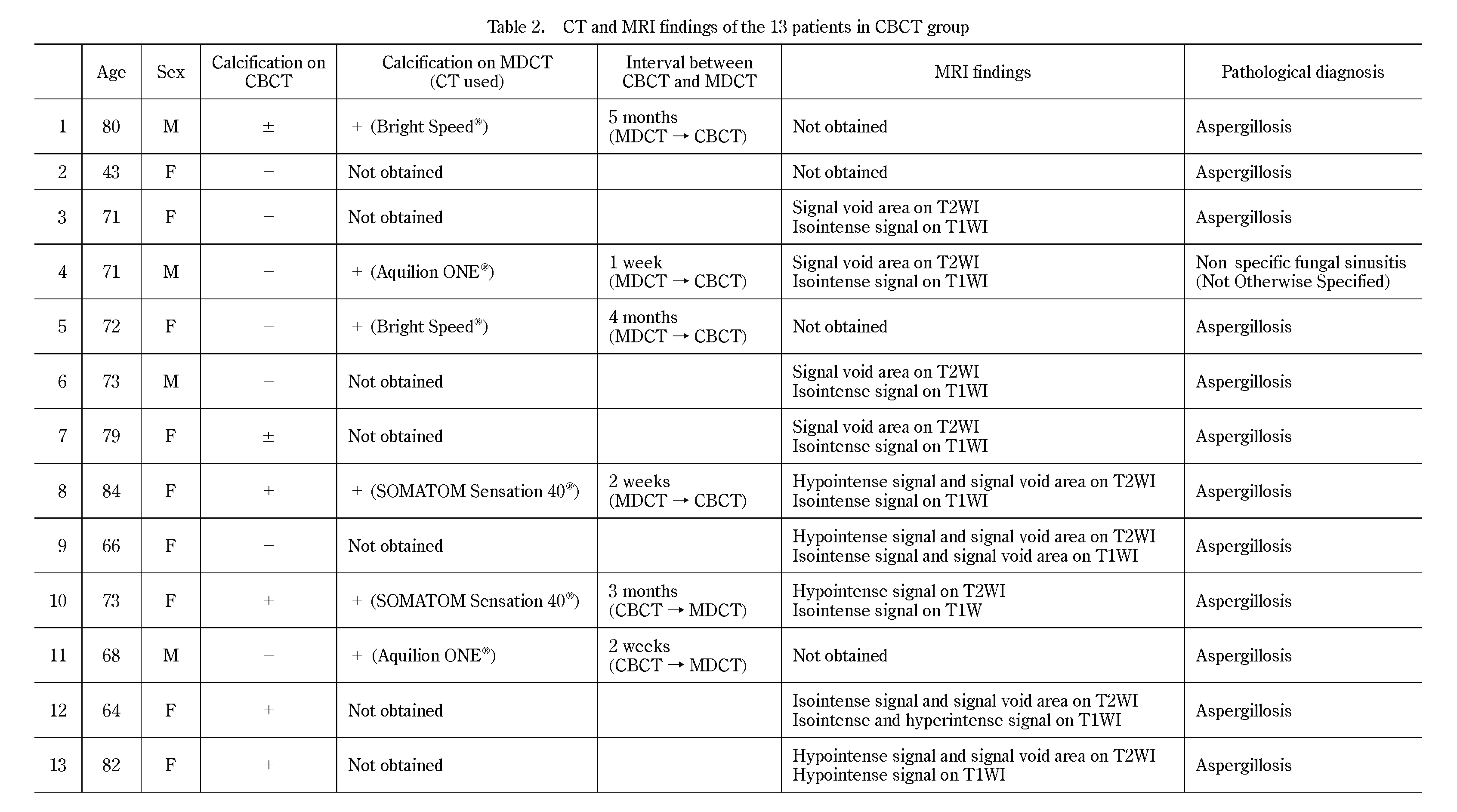
CT and MRI findings of the 13 patients in CBCT group
M: male, F: female, -: no calcification, ±: vague calcification, +: clear calcification, T2WI: T2-weighted image, T1WI: T1-weighted image
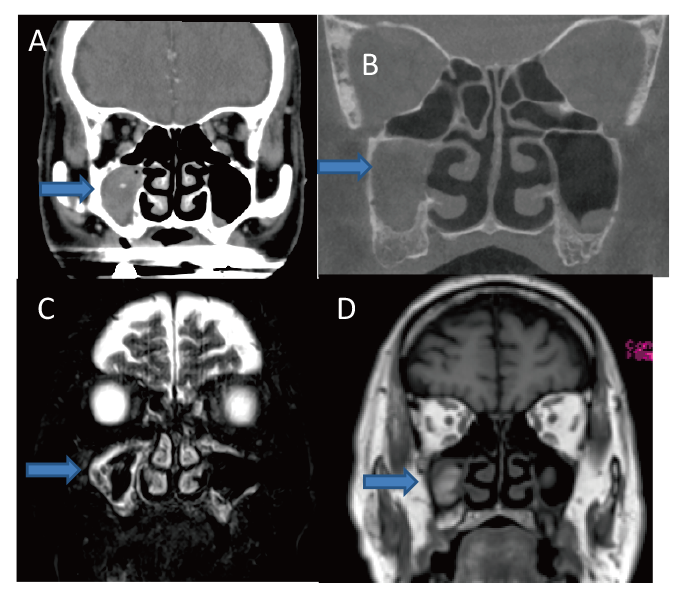
71-year-old male. (A) MDCT showing intrasinus calcification in the right maxillary sinus. (B) CBCT showing no intrasinus calcification. (C) MRI showing hypointense signal mass on T2-weighted image. (D) MRI showing isointense signal mass on T1-weighted image.
Detection of intrasinus calcification in patients with non-invasive chronic fungal maxillary sinusitis was higher in the MDCT group than the CBCT group. The lower detectability in the CBCT group was thought to result from CBCT’s limited contrast resolution. CBCT is frequently used in the screening of the paranasal lesion, but it is not enough to evaluate non-invasive chronic fungal maxillary sinusitis alone. MRI is recommended as a second-line analysis to counteract the CBCT’s low detectability of intrasinus calcification.
The authors declare no conflict of interests in association with this study.