2018 Volume 64 Issue 2 Pages 54-59
2018 Volume 64 Issue 2 Pages 54-59
Background: Laminoplasty is widely accepted as a standard treatment of cervical compressive myelopathy. However, due to the risk of postoperative complications such as neck symptoms, segmental partial laminectomy (SPL) is performed instead, which results in fewer postoperative symptoms. The aim of this study was to describe the difference in the incidence and severity of postoperative neck symptoms between traditional C3-C7 expansive open-door laminoplasty (ELAP) and SPL.
Methods: A retrospective and comparative study was performed regarding neck complications following the two surgical procedures. Twenty patients underwent SPL, and an additional 20 age- and gender-matched patients underwent traditional C3-C7 ELAP. Preoperative and postoperative JOA scores were measured, and postoperative neck symptoms in both groups were evaluated using a self-administered questionnaire, according to the Neck Pain and Disability Scale.
Results: The total incidence of postoperative neck symptoms in the SPL group was similar to that in the ELAP group; however, the severity of symptoms was remarkably lower in the SPL group than in the ELAP group.
Conclusions: SPL seems to be a better procedure for reducing postoperative neck symptoms, when compared with C3-C7 ELAP.
Laminoplasty is an accepted procedure for the treatment of cervical compressive myelopathy induced by spondylosis and ossification of the posterior longitudinal ligament. However, laminoplasty has some disadvantages, such as postoperative neck and/or shoulder complaints (axial symptoms)1-3). On the other hand, segmental partial laminectomy (SPL) has been used to treat cervical spondylotic myelopathy (CSM) and avoid postoperative problems associated with laminoplasty. The concept of SPL is that the posterior decompression of the spinal cord associated with CSM can be achieved by the decompression of the articular segment only. Our previous cadaver study showed that the removal of the ligamentum flavum and the superior edge of the lower lamina is sufficient to achieve minimum posterior decompression4). Thus, an indication for SPL is patients with CSM in whom the spinal compression is located only in the articular segment but not in the osseous segment, that is, those with the continuous or mixed type of ossification of the posterior longitudinal ligament (OPLL).
Our previous study also showed that patients who underwent SPL and those who underwent expansive open-door laminoplasty (ELAP) showed similar recovery rate, according to the Japanese Orthopedic Association (JOA) score, a scoring system developed by the JOA for cervical myelopathy4,5). However, the maintenance of the sagittal alignment and the range of motion were better after SPL. Additionally, postoperative neck and/or shoulder complaints reduced after SPL compared to ELAP4). However, the details of postoperative neck pain have not yet been clarified. This report describes the differences in incidence and magnitude of postoperative neck pain between patients who underwent SPL and those who underwent ELAP.
This was a retrospective study using medical records, and the protocol was approved by the ethical committee of Fukushima Medical University (No. 2592).
The subjects were 20 patients (14 males, 6 females) with CSM who underwent SPL between 1993 and 1999 (SPL group). The level of decompression was determined by the posterior indentation of the dural sac on either myelography or MRI in the extension position5-7). The ages of the patients in this group ranged from 47 to 80 years (mean 68±9). Twenty age- and gender-matched patients with CSM or segmental type cervical OPLL who underwent C3-C7 ELAP between 1989 and 19948) were used as controls (ELAP group). In the current study, any segmental type OPLL in the ELAP group was so small that both plain x-ray and MRI could not detect it but CT could. The ages of the patients in this group ranged from 54 to 75 (mean 65±6). In both groups, no patients met our institute’s criteria for anterior decompression and fusion during the postoperative observation period. The number of posteriorly compressed segments in the extension position were 3.1±1.3 and 2.5±1.7 in the SPL and ELAP groups, respectively. In addition, no statistically significant differences were observed regarding duration of symptoms and the number of posteriorly compressed segents between the two groups (Table 1). Postoperative care was the same in both groups; the patients were allowed to walk by themselves one day postoperatively, and used a Sternal-Occipital-Mandibular Immobilizer (SOMI) brace for two months postoperatively, followed by a soft neck collar for the third month.
The preoperative JOA score4) was collected from each patient’s medical record. Outcome assessment was performed five years postoperatively, including measuring JOA score and conducting a self-administrated questionnaire (10 items, Table 2)9), during regular follow-up at the outpatient clinic. The JOA score was assessed by two observers (K.O. and M.I.) who participated in neither the surgery nor the postoperative care of any of the included patients. The self-administrated questionnaire was conducted to assess neck symptoms on the Neck Pain and Disability Scale; neck pain today, neck pain on average, neck pain at its worst, sleep interference, daily living activity interference, personal relationship interference, stiffness of the neck and shoulders, neck-turning limitations, looking up or down limitations and working overhead limitations9). Each of the 10 items were scored using an 11-point numerical rating scale (NRS; 0: no pain/no interference, 10: worst pain/interference imaginable). Items were considered to be positive when their score was two or more points. The incidence and severity of the 10 items were compared between the SPL and ELAP groups.
All statistical analyses were performed using the STAT View software package (version 5.0, SAS Institute Inc., Cary, NC, The United States). Chi-square and Mann-Whitney U-tests were used in the statistical analysis. A p-value of less than 0.05 was considered to be statistically significant.
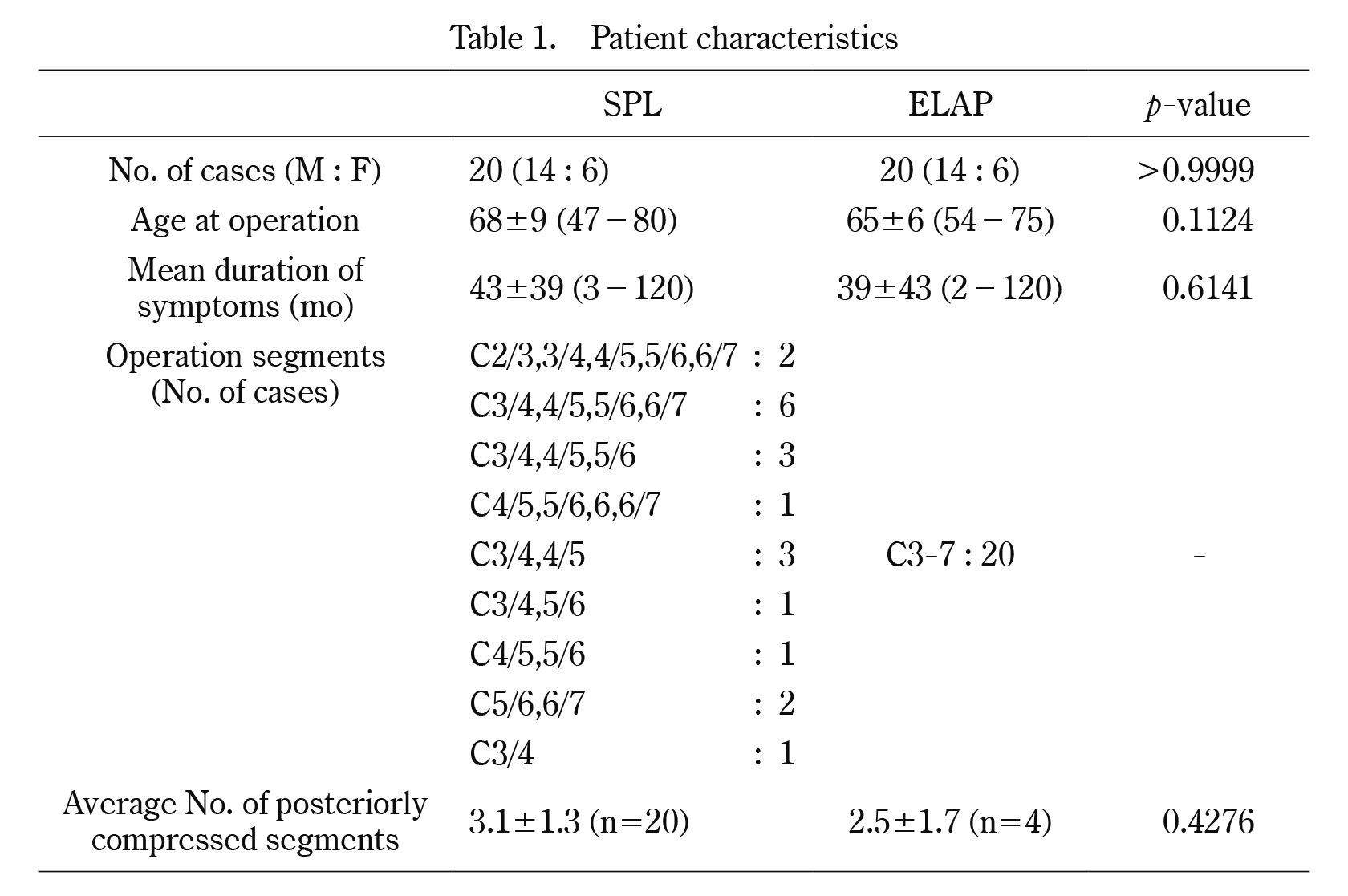
Patient characteristics
SPL: Segmental partial laminectomy
ELAP: Expansive open-door laminoplasty
Mean±standard deviation
There were no statistical differences in patient characteristics between the SPL and ELAP groups. The number of posteriorly compressed segments could be retrospectively confirmed only in 4 patients in the ELAP group because of the expiration of the designated storage period of the document.

Questionnaire for measuring neck symptoms
Each patient evaluated themselves using an 11-point numerical rating scale (NRS; 0: no pain/no interference, 10: worst pain/interference imaginable).
The average JOA score in the SPL group was 10.5±2.8 points preoperatively and 13.2±1.9 points at five years postoperatively. In the ELAP group, the average JOA score was 10.4±2.9 points preoperatively and 13.1±2.5 points at five years postoperatively. There were no statistically significant differences in the average JOA scores between the two groups.
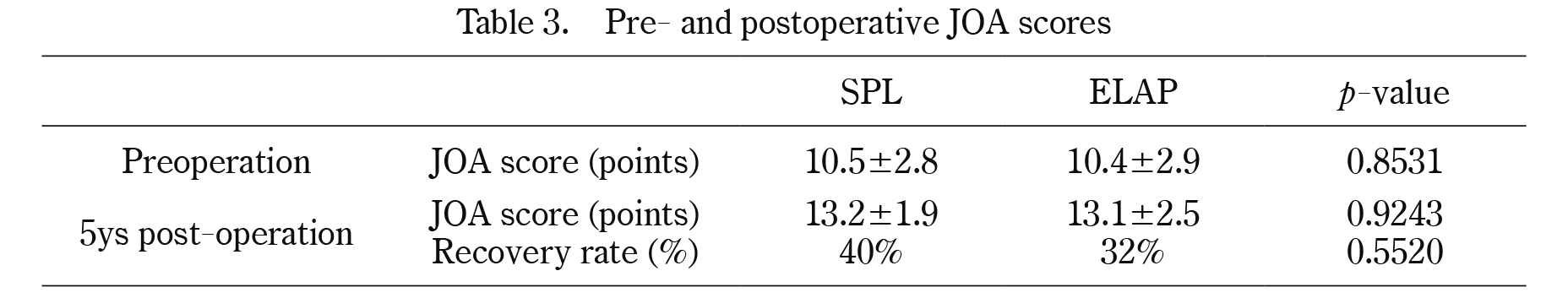
Pre- and postoperative JOA scores
JOA score: Japanese Orthopaedic Association score
SPL: Segmental partial laminectomy
ELAP: Expansive open-door laminoplasty
mean±standard deviation
Recovery rate (%)=(Post op. JOA score-pre op. JOA score) / (17-pre op. JOA score)×100.
There were no significant differences between the SPL and ELAP groups regarding preoperative and five-year postoperative JOA scores, or recovery rate.
Twelve patients (60%) in the SPL group and 14 patients (70%) in the ELAP group had one or more positive items. No statistically significant difference was observed between the two groups (p=0.7403). On the other hand, the average number of positive items (1.9±2.6 in SPL, 4.6±4.0 in ELAP) was statistically different between the two groups (p=0.0387). In the SPL group, 19 of the 20 (95%) patients had fewer than six positive items, whereas only 11 of the 20 (55%) ELAP patients had fewer than six positive items (Table 4). Similarly, the average NRS scores of all 10 items in the SPL group were lower than those in the ELAP group (Table 5). These results indicate that SPL may reduce the severity of postoperative neck symptoms in comparison to ELAP.
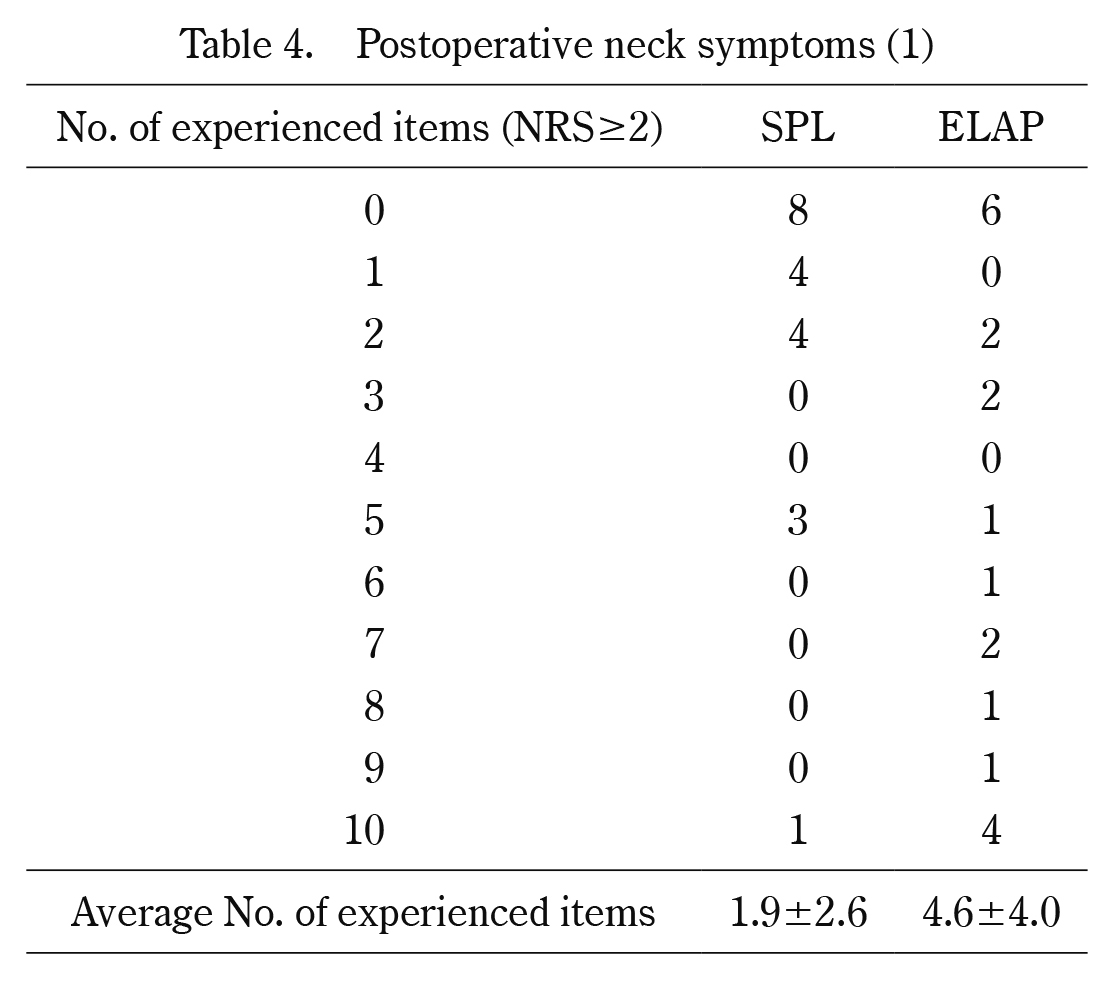
Postoperative neck symptoms (1)
p=0.0387 (Mann-Whitney U test)
NRS: Numenical rating scale
SPL: Segmental partial laminectomy
ELAP: Expansive open-door laminoplasty
In the SPL group and ELAP group, 12 patients (60%) and 14 patients (70%) had one or more positive items, respectively. No statistical difference was observed. On the other hand, the average incidence of all 10 items in the SPL group was statistically lower than that in the ELAP group (p=0.0387).
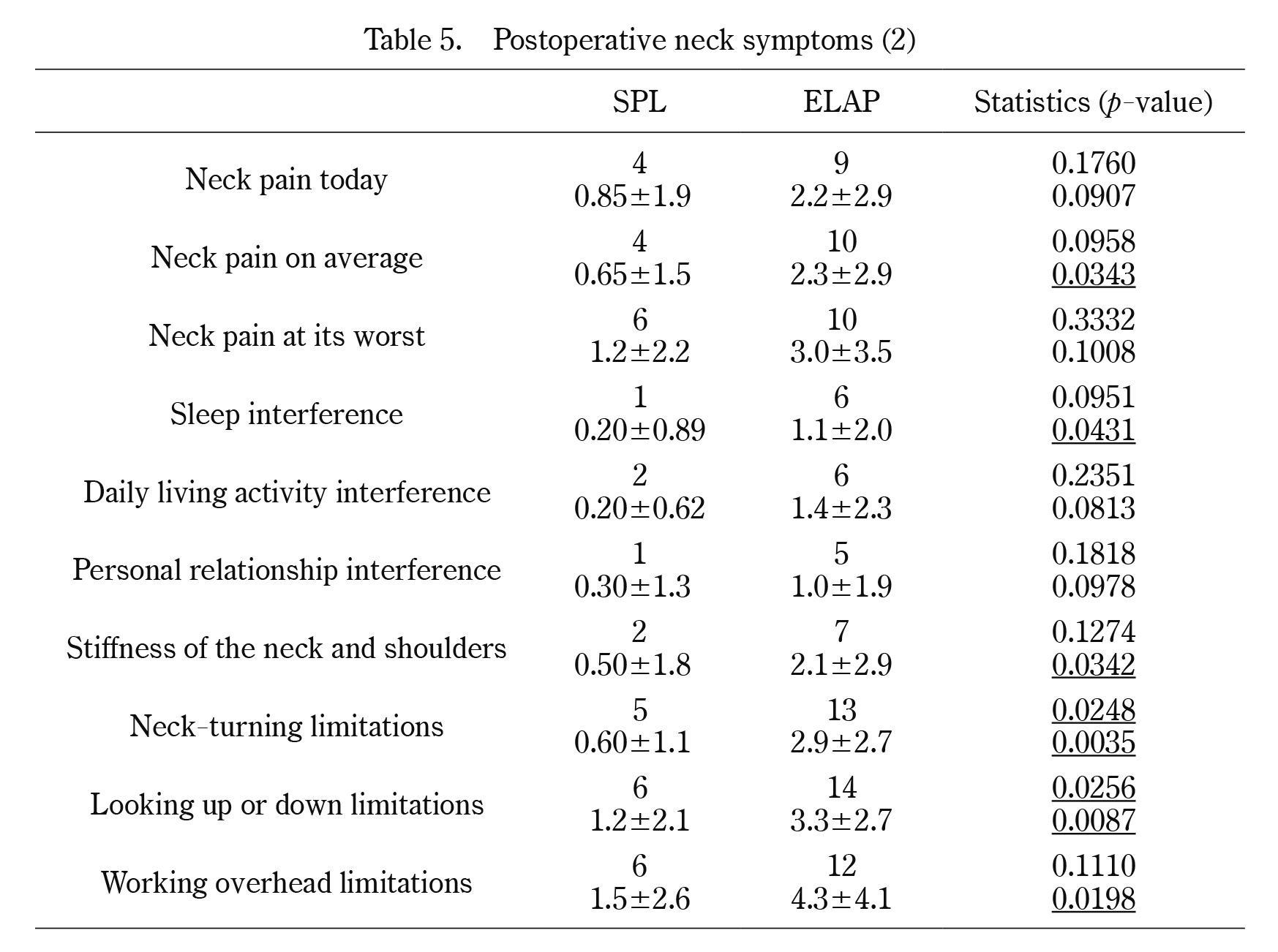
Postoperative neck symptoms (2)
Upper: No. of patients (NRS≥2),
Lower: mean±standard deviation of NRS (all 20 patients)
SPL: Segmental partial laminectomy
ELAP: Expansive open-door laminoplasty
NRS: Numerical rating scale
The incidence and average NRS of the 10 items in the SPL group were lower than those in the ELAP group.
Traditionally, there are two possible types of surgical procedures for cervical compressive myelopathy: anterior procedures and posterior procedures. However, selecting which procedure to employ remains controversial. Generally, anterior surgeries are performed if myelopathy is present at one or two compressive segments of the spinal cord, while posterior surgeries, such as laminoplasty, are performed regardless of the number of compressive segments10,11). Regarding a case in which anterior OPLL occupies more than 60% of the spinal canal, an increasing number of reports have demonstrated better outcomes of anterior procedures than posterior procedures. However, anterior procedures are known to be difficult and the frequency of complications is high12-14). Dysphagia, pseudarthrosis and adjacent deterioration are well known postoperative complications of anterior procedures. On the other hand, posterior procedures have no risk for dysphagia and the incidence of pseudarthrosis and adjacent deterioration is extremely low. There are various operation procedures and a surgical strategy should be selected according to individual patient condition and needs12-16).
Laminoplasty is the most commonly performed posterior procedure11). Numerous laminoplasty procedures have been developed for the treatment of cervical compressive myelopathy. These procedures have been reported to yield sufficient clinical outcomes over a long period of time3,17-19). However, there are some disadvantages, namely neck and/or shoulder complaints, known as “axial neck symptoms”1-3). SPL has been developed to resolve such disadvantages5) based on the observation that compression of the spinal cord is present in the articular segment, but not in the intra-osseous segment. The removal of the ligamentum flavum and the superior edge of the lower lamina is sufficient for minimal posterior decompression of the cervical spinal cord. We reported in a previous study that patients who underwent SPL showed a similar improvement in their JOA scores to that in the scores of patients who underwent C3-C7 ELAP; however, the maintenance of the sagittal alignment and the range of motion were observed to be better after SPL5). Similarly, postoperative neck complaints also seemed to be reduced after SPL according to our study5). However, the details of neck complaints such as pain, stiffness and disturbance of activity of daily life have not been reported.
The present study found that the incidence of postoperative neck symptoms was similar in both the SPL and ELAP groups. However, the magnitude in each of the 10 items was significantly different between the two groups. SPL reduced the severity of postoperative neck symptoms in comparison to ELAP. Postoperative care is thought to affect postoperative neck symptoms20); however, in the present study, postoperative care was the same in both groups (wearing a SOMI brace for two months postoperatively and a soft neck collar for the third month). Although the pathogenesis of postoperative neck symptoms after laminoplasty, including ELAP, is still unclear, there are a few possible reasons why the SPL group showed reduced postoperative neck symptoms in comparison to the ELAP group. First, the surgical field of the SPL group was smaller than that of the ELAP group. In the present study, ELAP was performed from C3 to C7, and the semispinal muscle of the neck was stripped from the C2 spinous process. In addition, the nuchal ligament was also cut between C7 and T1, and the C7 spinous process, to which the nuchal ligament is attached was removed. Stripping of the semispinal muscle of the neck from the C2 spinous process may affect the progression of kyphosis and postoperative axial symptoms21,22). Invasion of the C7 spinous process, which occurs if the caudal portion of the nuchal ligament is injured, may have a negative effect on postoperative neck symptoms23-25). On the other hand, the expansion of the laminae of the vertebral arch and neck extensor musculature is dependent on the operational segment level in SPL. SPL is a less invasive procedure because spinal cord compression is usually located below C3/4, and exposure of the C2/3 interlaminar space is unnecessary, thus preserving the attachment of the neck’s semispinal muscle at the C2 spinous process, in contrast to ELAP. Furthermore, when the lower part of the spinal cord compression is located above C5/6, exposure of the C6/7 interlaminar space is unnecessary, thus preserving the caudal attachment of the nuchal ligament at the C7 and T1 spinous processes. These factors of exposure can influence the incidence and/or severity of postoperative neck symptoms. Second, SPL can preserve the anatomical position of the spinous process. This may have some advantages for the reattachment of the extensor musculature to the spinous process and the lamina to maintain lordosis5). Third, SPL could preserve the sagittal alignment and range of motion of the cervical spine. This may have some advantages in reducing postoperative neck symptoms2).
There are some limitations in the present study: it was a retrospective observational study, the sample size was relatively small, it was not a randomized controlled trial, and no comparisons were made between pre- and postoperative neck symptoms. Future studies are needed to clarify the relationship between pre- and postoperative neck symptoms.
In conclusion, the total incidence of neck symptoms following SPL was similar to that experienced after traditional C3-C7 ELAP, but the severity of these symptoms was significantly lower after SPL. Therefore, we believe SPL to be a better procedure for reducing postoperative neck symptoms.
The authors have no conflicts of interest.