2021 Volume 67 Issue 3 Pages 102-106
2021 Volume 67 Issue 3 Pages 102-106
Background: Our previous report described the development of a self-administered questionnaire to screen patients for cervical myelopathy (SQC). For clinical application, the characteristics of the SQC should be verified.
Methods: Participants comprised 129 patients (94 men, 35 women) with cervical myelopathy who underwent operative treatment. SQC score was calculated before surgery and patients were divided into a positive group (score ≥6) and negative group (score <6). Sex, age, pathologies of cervical myelopathy, Japanese Orthopaedic Association (JOA) score, 10-s grip-and-release test (10-s test), grip strength, number of levels decompressed, most cranial level of damage, and presence of diabetes mellitus (DM) were compared between groups.
Results: The sensitivity was 89.9% with 116 positive cases and 13 negative cases (10.1%). JOA score was significantly higher and 10-s test and grip strength significantly better in the negative group than in the positive group. No significant differences in sex, age, pathologies of cervical myelopathy, number of spinal levels decompressed, most rostral level of damage, or presence of DM were seen between groups.
Conclusions: Screening for cervical myelopathy using SQC had a high sensitivity of 89.9%. However, SQC should be used with caution because it may miss mild cervical myelopathy with low JOA scores.
Diagnosing cervical myelopathy accurately is often difficult in primary care, with potentially irreversible consequences from delays in treatment1). To screen for cervical myelopathy more easily and avoid oversight, we have developed a screening tool, the self-administered questionnaire to screen patients for cervical myelopathy (SQC)2) .(Table 1). Questionnaire items were taken from the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ)3-5)., with score assignment derived through statistical analyses. Patients are diagnosed with cervical myelopathy if the total score is ≥6. This questionnaire offers a high sensitivity of 93.5% and 67.3% specificity. However, the characteristics of the SQC for clinical application has not been evaluated. The aim of this study was to investigate characteristics of the questionnaire for clinical application using patients with cervical myelopathy who underwent surgery to evaluate its utility in practice.
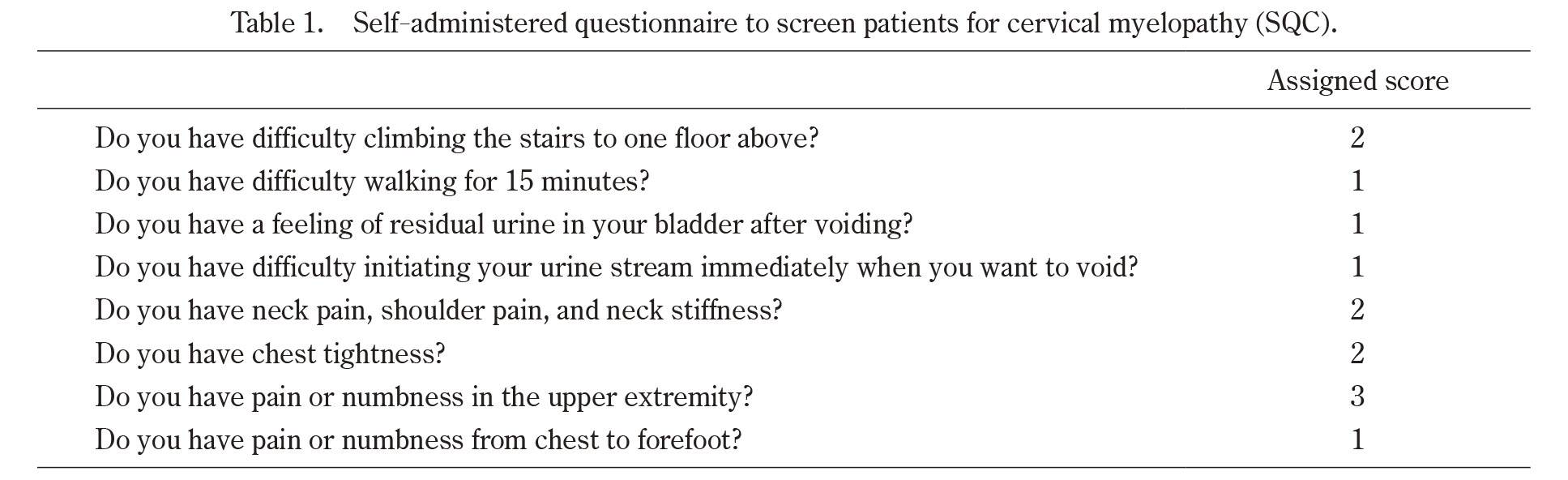
Total score cut-off point: ≥ 6
Sensitivity: 93.5%
Specificity: 67.3%
Positive likelihood ratio: 2.96
Negative likelihood ratio; 0.096
*The 4th question in the previous report, “Can you initiate (start) your urine stream immediately when you want to void?” was revised to “Do you have difficulty initiating your urine stream immediately when you want to void?” in this article.
The Research Ethics Committee of our institute approved our study protocol. Informed consent was obtained in the form of an opt-out on the website.
Participants comprised 129 patients (94 men, 35 women) with cervical myelopathy who underwent operative treatment in our hospital between May 2008 and January 2013. The indication for surgery was determined with the consent of at least three board-certified spine surgeons.
Mean age was 65.4 ± 13.0 years (range, 16-88 years; Table 2). Subjects comprised 76 patients (58.8%) with cervical myelopathy, 39 patients (30.2%) with ossification of the posterior longitudinal ligament (OPLL), 5 patients (3.9%) with cervical disc herniation, and nine patients (7.0%) with some combination of these pathologies. Exclusion criteria included a history of cervical operations, rheumatoid arthritis, infectious spondylitis, cervical amyotrophy, tumor, or trauma.
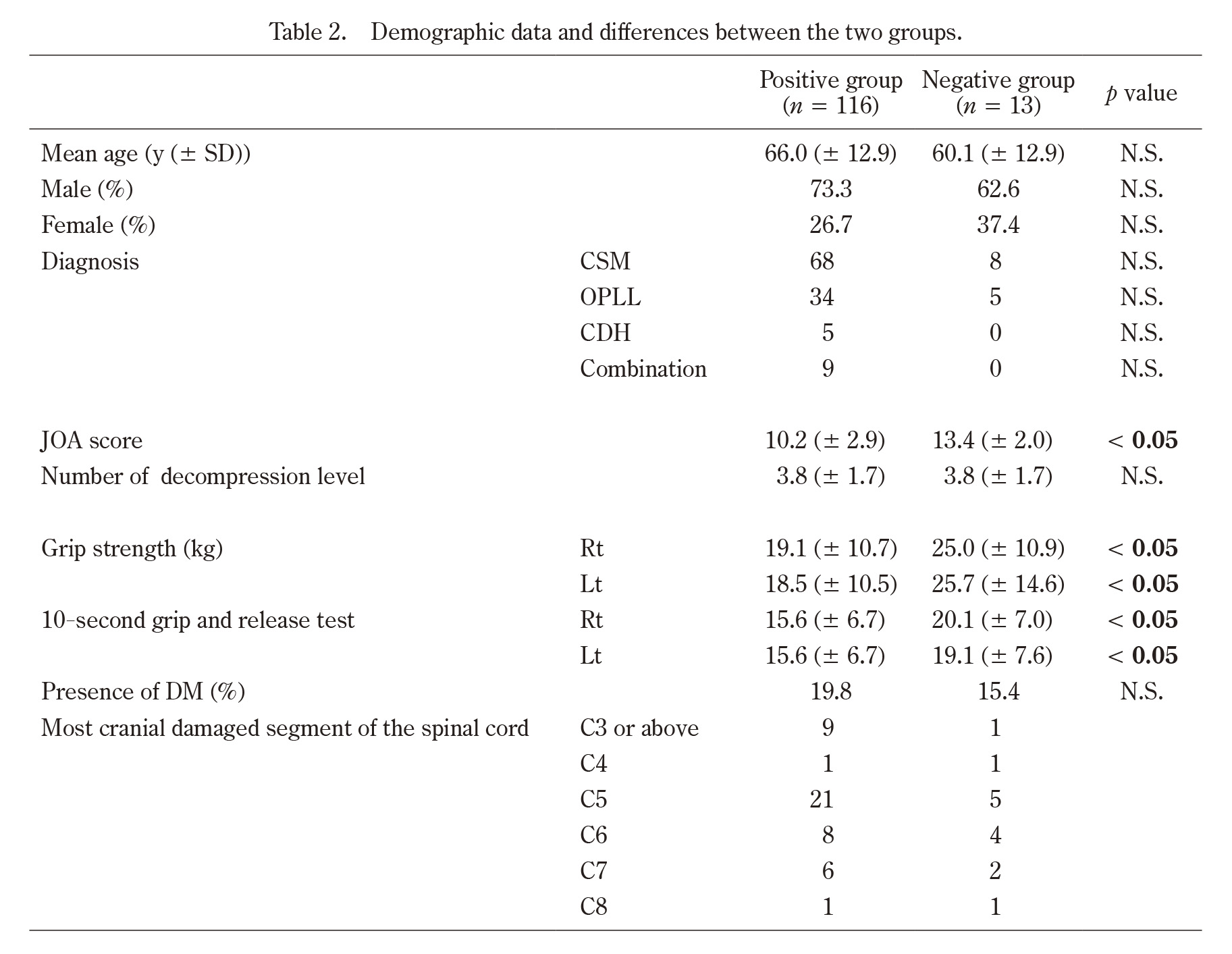
CSM: Cervical Spondylotic Myelopathy
OPLL: Ossification of Posterior Longitudinal Ligament
CDH: Cervical Disc Herniation
Combination: Combination of CSM, OPLL, or CDH
JOA: Japanese Orthopaedic Association
DM: Diabetes Mellitus
The SQC was assessed at the time of admission one to two months prior to surgery. The SQC score was calculated before surgery and patients were divided into a positive group (score ≥6) and a negative group (score <6) according to our previous report2). The demographic data for these two groups are shown in Table 2. No significant differences in mean age, sex, or diagnosis were evident between groups. We then compared sex, age, diagnosis, Japanese Orthopaedic Association (JOA) score6), which is widely used as a functional scale in cervical spine disease across the world, 10-s grip-and-release test (10-s test)7) which evaluates hand clumsiness, grip strength, number of levels decompressed, most cranial level of damage, and presence of diabetes mellitus (DM) between the positive and negative groups. DM was defined on the basis of diagnosis by a physician. First, we calculated the sensitivity. Sex, age, pathologies of cervical myelopathy, JOA score, 10-s test, grip strength, number of decompressions, most cranial level of damage, and presence of DM were then compared between groups.
Statistical analysesAll statistical analyses were performed using SPSS version 11.0.1 software (SPSS, Chicago, IL). Student’s t-test was used to compare age, JOA score, grip strength, 10-s test, and presence of DM. Fisher’s exact test were used to compare sex. Values of p <0.05 were considered statistically significant.
The 129 patients included 116 positive patients (89.9%) and 13 negative patients (10.1%), leading to a sensitivity of 89.9% (Figure 1). No significant differences were observed regarding sex, age, pathologies of cervical myelopathy , number of levels decompressed, or presence of DM between groups (Table 2). JOA score was significantly higher in the negative group (13.4 ± 2.0) than in the positive group (10.2 ± 2.9). Grip strength was significantly stronger in the negative group (right: 25.0 ± 10.9 kg, left: 25.7 ± 14.6 kg) compared to the positive group (right: 19.1 ± 10.7 kg, left: 18.5 ± 10.5 kg). Similarly, results for the 10-s test were significantly better in the negative group (right: 20.1 ± 7.0, left: 19.1 ± 7.6) compared to the positive group (right: 15.6 ± 6.7, left: 15.6 ± 6.7).
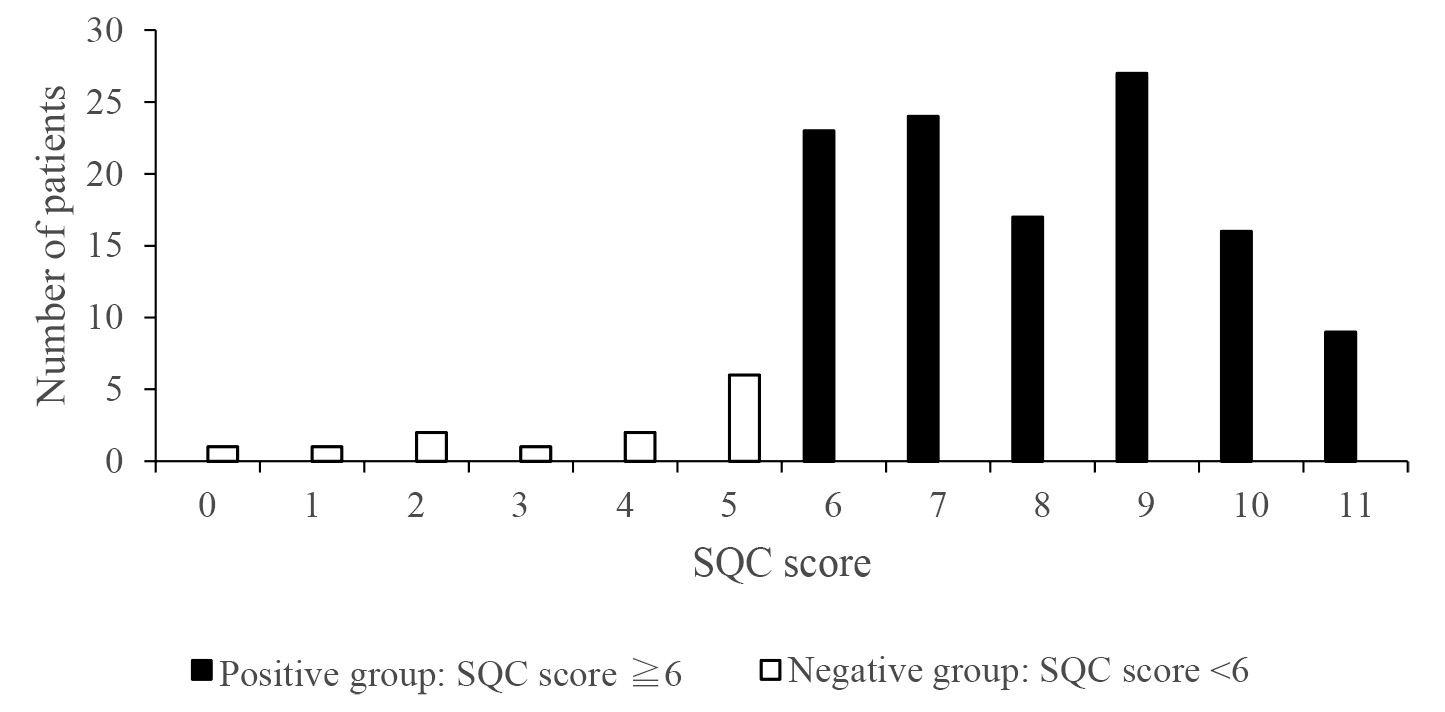
SQC: Self-administered questionnaire to screen patients for cervical myelopathy
In this study, we surveyed surgical cases of cervical myelopathy using the SQC, a newly developed self-administered questionnaire for the screening of cervical myelopathy, to investigate its sensitivity and to examine and characterize false-negative cases.
Patients with cervical myelopathy exhibit various symptoms, such as numbness, pain, hypesthesia, weakness of the extremities, pain and stiffness of the neck, manual clumsiness, walking disturbance, and urinary disturbance8,9). The prevalence is not very low and is estimated to increase with the aging of a society10,11).
Many sources of information must be examined to reach an accurate diagnosis, such as the case history, physical examination (including neurological examination), and imaging tests.
Generally, numbness of the upper extremities is one of the chief symptoms of cervical myelopathy. Patients with cervical myelopathy who show this numbness frequently consult a general outpatient clinic or primary care practitioner. However, accurate diagnosis is not always easy because numbness of the upper extremities may also result from entrapment neuropathies such as carpal or cubital tunnel syndromes.
On the other hand, misdiagnosis and delayed treatment of cervical myelopathy can result in irreversible consequences, such as paralysis, urinary disturbance, and walking disturbance1). Accurate diagnosis and early treatment by a specialist are therefore central to a good outcome.
We recently developed a brief, self-administered screening questionnaire for cervical myelopathy, the SQC2). This tool offers a high sensitivity of 93.5% and a specificity of 67.3%. We emphasized sensitivity, as this questionnaire is designed to screen for cervical myelopathy. Patients could quickly complete the questionnaire while waiting for primary care. Also, it is possible that they could answer the SQC as part of self-regulation at home.
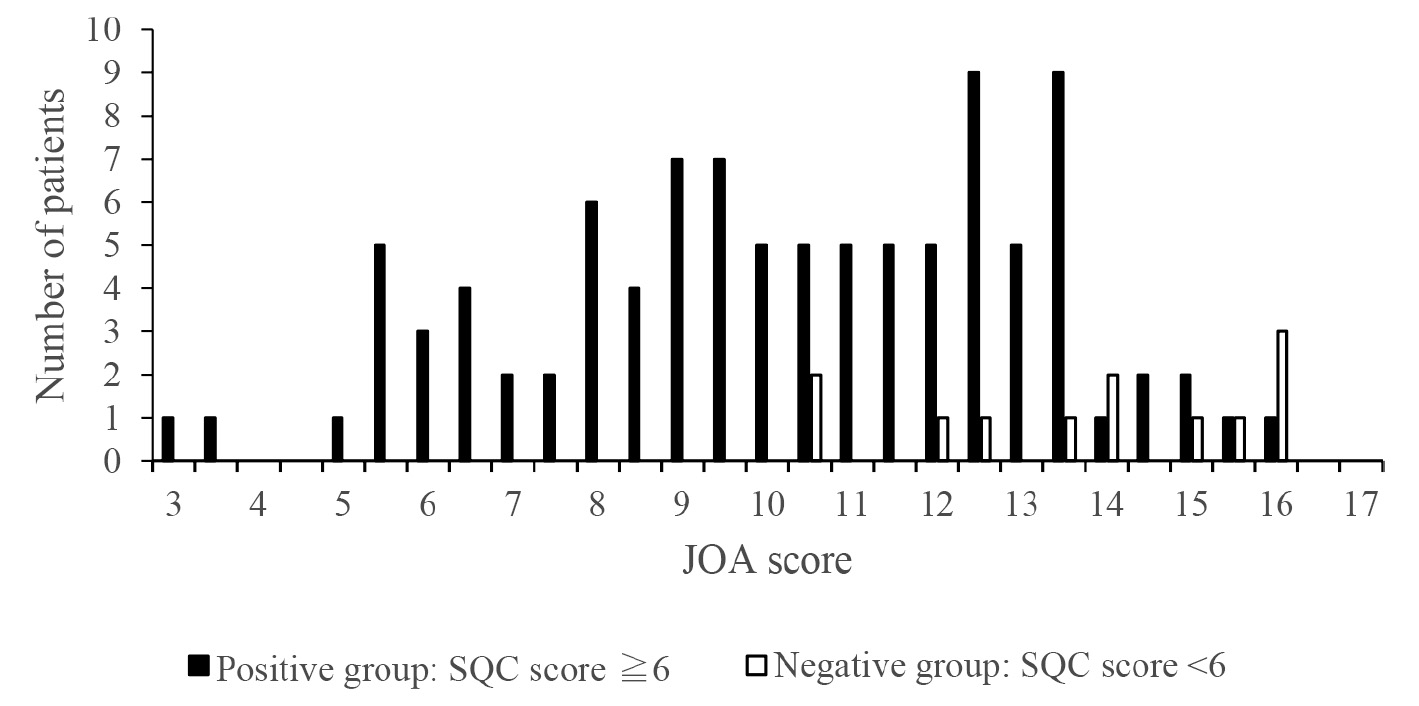
The present study investigated the utility of the SQC by calculating the sensitivity and also compared several items between positive and negative groups to clarify the characteristics of patients showing a false negative result on the SQC. We found that JOA scores were significantly higher in the negative group.
Interestingly, most patients in the negative group (11/13, 84.6%) showed a JOA score ≥12 (Figure 2). This result corresponds with the fact that a JOA score ≥12 indicates a mild case of cervical myelopathy12). Similarly, results for grip strength and the 10-s test were superior in the negative group. These results mean that patients with mild cervical myelopathy can present false-negative results in this questionnaire. Since the purpose of screening with SQC is to narrow down the list of cervical myelopathy patients in primary care, it is thought that a certain number of false negatives will inevitably occur. In order to reduce the number of false positives, repeated evaluation by SQC for cases of suspected mild cervical myelopathy could be considered as a useful option.
Several limitations must be considered in this study. First, this self-administered questionnaire was developed based on a case-control study of patients treated surgically and patients with peripheral nerve entrapment such as carpal tunnel syndrome. Healthy volunteers were not included in the development of SQC. However, the median score of healthy volunteers in SQC is available from the past report showing the median JOACMEQ score of healthy volunteers13) because SQC consists of items of JOACMEQ, which suggests that the result of SQC in healthy volunteers should be negative. Secondly, all participants in this study were patients who were treated surgically. We consider that this questionnaire might be beneficial in primary care situations to screen for cervical myelopathy requiring surgical intervention. Further studies that include patients who were treated conservatively would be needed in the future. Finally, this SQC does not contain the item which asks about hand clumsiness and muscle weakness of hands. Therefore, complementary tests such as the grip and release test would be needed additionally for more sensitive screening. As a result, clinicians should use this questionnaire with caution.
In conclusion, the SQC showed a high sensitivity of 89.9%. Clinicians need to be aware that the SQC may show false-negative results for patients with mild cervical myelopathy.
SQC: Self-administered questionnaire to screen patients for cervical myelopathy
The authors thank the patients who participated in the study.
The authors declare no conflicts of interest in this work.