Article ID: 2014-3
Article ID: 2014-3
Acute focal bacterial nephritis (AFBN) is a localized bacterial infection of the kidney presenting as an inflammatory mass without frank abscess formation. We report a case of acute focal bacterial nephritis without pyuria in a five-month-old boy presenting with high urinary β2-microglobulin (β2-MG) and N-Acetyl-β-(D)-Glucosaminidase (NAG) levels. The infant initially presented with high-grade fever, and plain computed tomography (CT) showed a nearly isodense mass, and contrast-enhanced abdominal CT showed a wedge-shaped hypodense lesion. Enterococcus was detected in the subsequent urine culture. A diagnosis of AFBN was made on the basis of his high inflammatory reaction, contrast-enhanced abdominal CT findings and high urinary β2-MG and NAG levels. He was treated with Ceftriaxone and subsequent improvement in inflammatory reaction and contrast-enhanced CT findings were observed. Voiding cystourethrogram (VCUG) showed a grade V right VUR. This case suggests that urinary β2-MG and NAG levels may be useful additional markers for the diagnosis of AFBN without pyuria.
Acute focal bacterial nephritis (AFBN) is a localized bacterial infection of the kidney presenting as an inflammatory mass without frank abscess formation1-5). AFBN is considered to be a midpoint in the spectrum of upper urinary tract infections, ranging from pyelonephritis to intrarenal abscess, and may represent a relatively early stage of renal abscess2,6-10). The typical clinical presentations of AFBN include fever, flank pain, leukocytosis, pyuria, and bacteriuria, which are similar to those for renal abscess. The diagnosis of acute renal inflammatory disease can be made on a clinical basis in a patient with fever, flank pain, and pyuria.
Results of urinary examination demonstrate that most patients with AFBN show pyuria. However, 5-10% of patients with AFBN have normal urinalysis findings and, for these patients, the diagnosis of AFBN may be delayed5-7).
On the other hand, urinary N-Acetyl-β-(D)-glucosaminidase (NAG) and β2-microglobulin (β2-MG) have been reported as indicators of proximal tubular dysfunction11-13). NAG is a lysosomal brush border enzyme expressed/localized in the proximal renal tubular cells and a more established urinary marker of kidney injury. In addition, β2-MG is a 12-kDa polypeptide chain that is constantly synthesized throughout the body. Impairment of tubular cell uptake elevates urinaryβ2-MG concentration up to several hundred fold. Jantausch BA et al. reported that urinary NGA and β2-MG were useful markers for the diagnosis of urinary tract infection11). However, there have been no reports on the relationship between urinary levels of NAG and β2-MG, and AFBN activity.
We report a case of acute focal bacterial nephritis without pyuria in a five-month-old boy presenting with high urinary β2MG and NAG levels.
A five-month-old boy presented with high-grade fever, and was initially diagnosed with an upper respiratory tract infection. He remained febrile for 5 days and was referred to our hospital. The pharynx, chest and abdomen showed no abnormal findings with respect to percussion or auscultation. Laboratory tests revealed a leukocyte count of 23,600/mm3, erythrocyte count 492×104/mm3, platelet count 41.4×104/mm3, serum total protein 7.1 g/dl, serum albumin 3.6 g/dl, serum creatinine 0.47 mg/dl and serum C-reactive protein (CRP) 9.3 mg/dl. Urinalysis was positive for protein and revealed an NAG level of 87.3 U/l, and β2-MG 68211 μg/ml, with sediment containing 0-1 erythrocytes per high-power field, 0-l leukocytes, and no granular casts (Figure 1). An abdominal ultrasonogram showed an echogenic mass lesion and plain abdominal computed tomography (CT) showed a nearly isodense mass, and contrast-enhanced abdominal CT showed a wedge-shaped hypodense lesion (Figure 2-a, b). Enterococcus was detected in the subsequent urine culture, but no bacteria were detected in the blood culture. A diagnosis of AFBN was made on the basis of his high inflammatory reaction, contrast-enhanced abdominal CT findings and high urinary β2-MG and NAG levels. The patient was treated with ceftriaxone (100 mg/kg/day) as antibiotics. The changes of laboratory findings in the clinical course of this patient were showed (Figure 1). On day 4 of hospitalization, no fever was observed and the inflammatory reaction was gradually diminished. On day 10 of hospitalization, leukocyte count and serum CRP level were 5,600/mm3 and 0.2 mg/dl, respectively, and urinalysis revealed NAG and β2-MG levels of 5.3 U/l and 0.5 μg/ml, respectively. An abdominal ultrasonogram showed decreasing of an echogenic mass lesion. Follow-up contrast-enhanced CT was performed on day 17 of hospitalization. Enhanced CT showed a slightly wedge-shaped hypodense lesion (Figure 2-c). Voiding cystourethrogram (VCUG) on day 28 of hospitalization showed a grade V right VUR, (Figure 2-d). No subsequent recurrence of urinary tract infection has been observed for 6 months, and re-evaluation by VCUG showed no VUR.
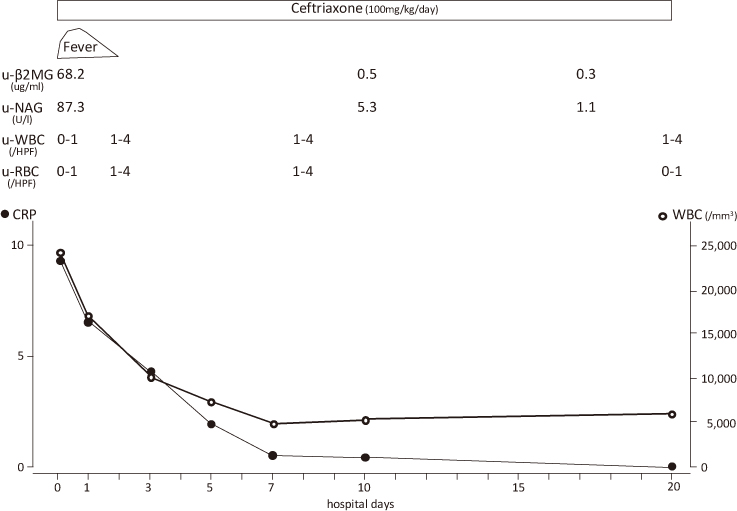
The changes of laboratory findings in the clinical course of this patient.

Contrast-enhanced abdominal CT and VCUG findings
Fig. 2-a, b. Contrast-enhanced CT findings on day 4 of hospitalization
Fig. 2-a. A wedge-shaped hypodense lesion and nephromegaly can be observed in transverse section.
Fig. 2-b. A wedge-shaped hypodense lesion and nephromegaly can be observed in sagittal section.
Fig. 2-c. Contrast-enhanced CT findings on day 17 of hospitalization
A slightly wedge-shaped hypodense lesion can still be observed.
Fig. 2-d. VCUG findings on day 28 of hospitalization
A grade V right VUR can be seen.
AFBN is a focal upper urinary tract infection presenting as an inflammatory mass not containing drainable pus. Rosenfield et al. originally designated it acute lobar nephronia1). It has since been referred to as acute focal bacterial nephritis and acute lobar nephronia. It is considered to be a midpoint in the spectrum of upper urinary tract infections, ranging from pyelonephritis to intrarenal abscess. It is frequently found in childhood and is a rare manifestation of renal cortical infection in adults.
Seidel et al reported that AFBN diagnosis is often delayed due to nonspecific symptoms. All children later diagnosed with AFBN were admitted with septic temperatures and a rapid deterioration of clinical condition10). Young infants presented with vomiting, diarrhea, poor feeding, dehydration, paraumbilical pain, or lethargy-symptoms that could easily be attributed to other more common causes, and flank pain was found only in older children (mean age of 8 years).
As to the clinical manifestations in AFBN, Rathore NH et al. reported that all patients with AFBN had fever, and 59% of patients complained of either back or flank pain or flank tenderness was only presented in 29% of patients, and 6% of patients with AFBN had no pyuria7). Furthermore, Kline MW et al. reported that one of two children with AFBN had no pyuria5). It is speculated that the reason for normal urine in patients with AFBN and associated urinary tract infection is that the bacterial infection in AFBN is localized in the kidney. Thus, diagnosis of AFBN may be often delayed in patients with nonspecific symptoms or normal urine. In our case, in which, urinalysis was normal and there was no flank pain, the high urinary NAG and β2-MG levels provided the basis for our diagnosis of AFBN as well as the finding of abdominal CT and ultrasonogram. Further, the urinary NAG and β2-MG levels were found to be associated with the serum CRP level, the findings of echo, and the improvement in AFBN.
NAG is a lysosomal brush border enzyme of the proximal renal tubular cells and a more eastablished urinary marker of kidney injury. Recently, Liangos et al. reported that urinary NAG can predict adverse clinical outcomes in patients with acute renal failure13).
In addition, β2-MG is a 12-kDa polypeptide chain that is constantly synthesized throughout the body. It is filtered by the glomeruli and nearly completely reabsorbed and catabolized by tubular cells so that only 0.3% of the filtered β2-microglobulin is found in the urine. Impairment of tubular uptake elevates the urinary β2-MG level by up to several hundred fold.
Jantausch BA et al. reported that urinary NGA and β2-MG were useful markers for the diagnosis of urinary tract infection11). However, there had been no reports on the relationship between the urinary levels of NAG and β2-MG, and AFBN activity. Our case with AFBN had no pyuria and showed high urinary β2MG and NAG levels at onset.
The mechanism of high urinary β2-MG and NAG levels in our case with AFBN is speculated as follows: The pathological condition of AFBN is a localized bacterial infection of the kidney presenting as an inflammatory mass without frank abscess formation and this is thought to represent the early stage of renal abscess. Thus, we think that glomerular alterations and damage by AFBN may cause β2-MG leakage from serum to urine, and interstitial alterations and damage by AFBN cause the inhibition of tubular uptake of β2-MG. In addition, interstitial alterations and damage by AFBN may cause increase of urinary NAG levels.
Our case suggests that urinary β2-MG and NAG levels are useful additional markers for the diagnosis of AFBN without pyuria and for the improvement in AFBN from the onset of symptoms.
We reported a case of acute focal bacterial nephritis without pyuria in a five-month-old boy presenting with high urinary β2-MG and NAG levels, and our case suggests that urinary β2-MG and NAG levels may be useful additional markers for the diagnosis of AFBN without pyuria.