2022 Volume 47 Issue 4 Pages 147-149
2022 Volume 47 Issue 4 Pages 147-149
A patient who survived acute paraquat (PQ) poisoning for more than 5 years was followed up in the emergency room. The patient had recurrent coughing and wheezing one month after discharge. Re-examination of chest CT showed increased dual lung texture. Spirometry suggested severe ventilatory dysfunction while bronchial dilation test was positive. The serum IgE level was significantly high. It is considered that patients with acute PQ poisoning may develop asthma in the long term.
Patients who experienced acute paraquat (PQ) poisoning always present with acute respiratory distress syndrome in the early stage that gradually progresses to pulmonary fibrosis in the subacute stage. Most patients die from respiratory failure. In survivors, lung imaging and respiratory functions revealed partial recovery 2–3 years after poisoning (Lee et al., 2009). However, few studies have reported pulmonary function changes in patients who have survived for a longer time, especially those who have lived for more than 5 years after poisoning. In our emergency room (ER), a patient who experienced PQ poisoning with no underlying pulmonary disease was followed up for more than 5 years to evaluate long-term changes in pulmonary function and lung imaging findings. The presenting symptoms were repeated asthma attacks with severe ventilatory disorder, but chest computed tomography (CT) did not detect interstitial fibrosis or other structural disorders. This case will help clinicians gain a better understanding of the long-term outcomes of patients who experienced PQ poisoning, especially the effects of poisoning on airway function.
Case introduction Acute poisoning phaseA 62-year-old female farmer without chronic respiratory disease or allergy history intentionally drank approximately 10 g of paraquat on June 16, 2015. The patient was presented to our ER 2 hr after poisoning, with SpO2 of 98%. The arterial blood gas analysis (ABG) showed PO2/FiO2 of 381.0 mmHg and Lac of 2.9 mmol/L (Fig. 1). The urine semiquantitative method result was dark blue color. On day 1 of poisoning, she was immediately given gastric lavage and catharsis. Afterwards, she underwent blood perfusion and was given methylprednisolone intravenously. The patient gradually developed chest tightness and shortness of breath, with decreased SpO2. The worst SpO2 was 92% on day 7 of poisoning. At the same time, chest CT showed increased and disordered texture of both lungs, with a small amount of bilateral pleural effusion (Fig. 2). On day 14 of poisoning the patient was discharged with improved SpO2 of 97%. ABG showed PO2/FiO2 of 414.3 mmHg and Lac of 2.6 mmol/L. Chest CT showed the increased lung texture was partially dissipated, and the pleural fluid was absorbed on both sides (Fig. 2). During the whole hospitalization, the patient never received any oxygen therapy or ventilation.
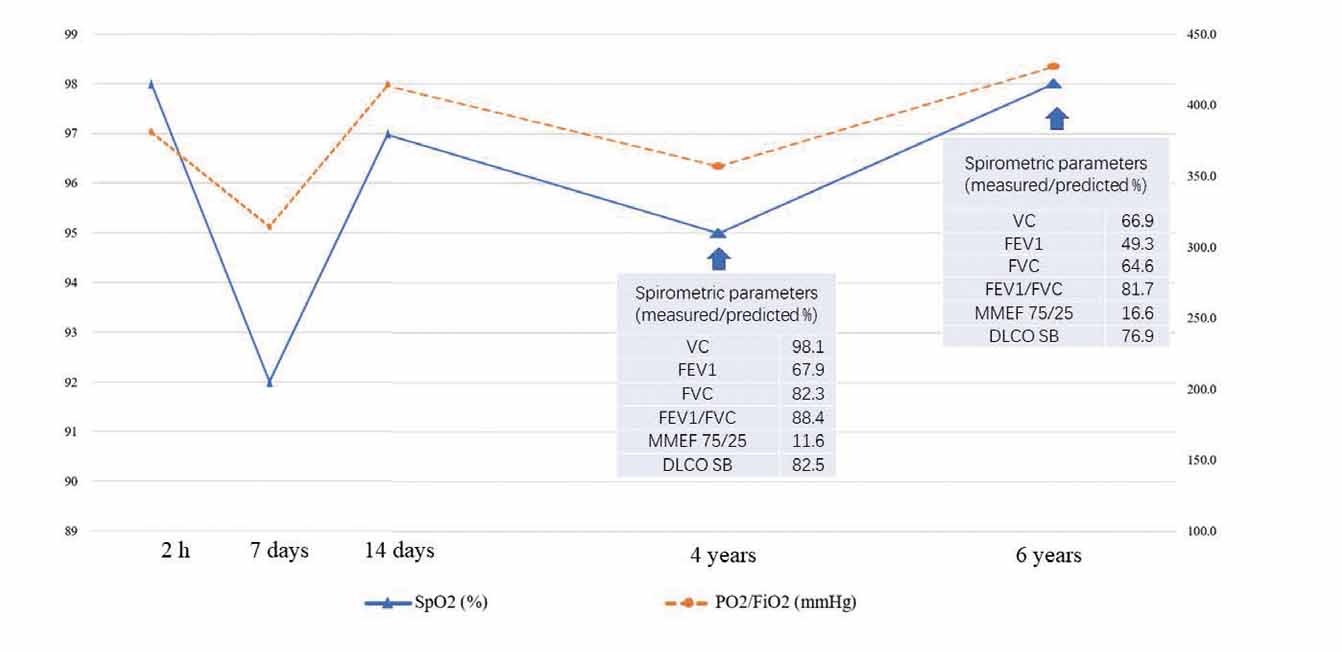
The SpO2, PO2/FiO2 and lung function changes of the patient from 2 hr to 6 years after paraquat poisoning. VC, Vital capacity; FEV1, Forced expiratory volume in the first second; FVC, Forced vital capacity; MMEF 75/25, Maximal mid expiratory flow 25%–75%; DLCO-SB, Diffusion capacity for carbon monoxide in single breath.
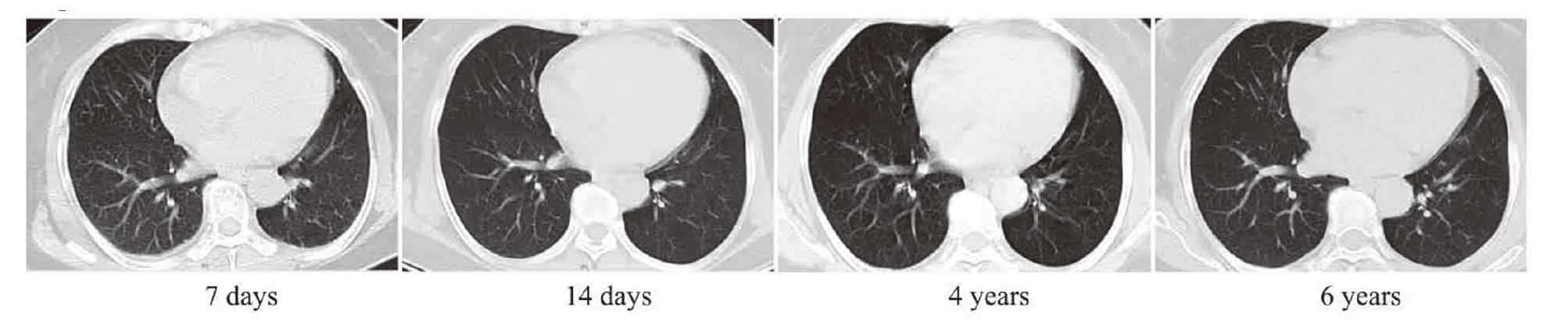
The lung images of the patient from 7 days to 6 years after paraquat poisoning. Chest CT on day 7 after paraquat poisoning revealed obviously increased and disordered texture of both lungs, with a small amount of bilateral pleural effusion. On day 14 after poisoning, the increased lung texture was partially dissipated and the pleural effusion had been absorbed. The chest CT in 4 years and 6 years after poisoning showed mildly increased texture of both lungs.
The patient went back to work 3 months after discharge. Her living and working environment did not change compared with that before the poisoning. The patient presented with intermittent attacks of coughing and wheezing about one month after discharge, which always occurred when she had a cold or felt tired. Over time, the symptoms gradually became more frequent and severe, but she barely sought medical consultation or any treatment. The patient was followed up in the 4th and 6th year after poisoning, with the symptoms of coughing and wheezing. Physical examination found diffuse wheezing sound in both lungs. The patient’s symptoms were alleviated after administration of glucocorticoids and β -receptor agonists. The results of PO2/FiO2 were normal but spirometry revealed obstructive ventilatory dysfunction in the 4th and 6th year after poisoning (Fig. 1). The CT images showed mildly increased texture of lungs at both timepoints (Fig. 2). The bronchial dilation tests were both positive, with improvement rate of FEV1 of 36.3% and 31.1%, respectively. In the 6th year follow-up, the patient’s blood eosinophil count was 0.07 × 10^9/L, and the serum IgE level was 459.96 KU/L.
Acute paraquat poisoning often develops acute pulmonary edema within 1 week, which rapidly progresses to pulmonary fibrosis within 3–4 weeks. Chronic occupational exposure to PQ cannot only cause lung fibrosis but also increase the incidence of asthma (Díaz-Criollo et al., 2020). In this report, the patient had no history of respiratory disease and developed symptoms of bronchial asthma during follow-up after acute PQ poisoning. The lung images did not show interstitial fibrosis or any other severe structural disorders. But spirometry suggested obstructive ventilatory dysfunction, with positive result of bronchial dilation test and high level of serum IgE. To the best of our knowledge, reports of such cases are scarce since most patients with PQ poisoning died due to respiratory failure and the surviving ones have barely been followed up for such a long-period. This report filled in the blank of long period follow-up for patients with PQ poisoning and highlights changes in airway function, especially identifying asthma attacks as complications of PQ poisoning.
Previous studies have proposed the concept of reactive airway dysfunction syndrome (RADS), which is referred to as the sudden onset of “acute irritant asthma” after a single exposure to high levels of irritating gas, vapor, or smoke (Brooks, 2013). Despite a single exposure, patients can have asthma-like attacks that can last for months or even years. In the present case, the patient took PQ orally. Although she was not exposed to toxic gas, the clinical features were similar to RADS.
The pathological mechanism of PQ induced asthma is not clear, the disease may develop through the following points: (1) Paraquat poisoning activates the release of various inflammatory mediators in lung tissues, increases microvascular permeability and promotes secretion of bronchial mucous cells (Chen et al., 2021). Excessive inflammation and mucus increase airway resistance. Meanwhile, airway inflammation can induce the release of smooth muscle contractile mediators like leukotrienes, histamine and endothelin-1, leading to airway hyperresponsiveness. (2) Paraquat poisoning leads to the formation of oxygen free radicals and lipid peroxidation (Blanco-Ayala et al., 2014). Excessive intracellular oxidative stress can also induce allergic airway inflammation (Cho et al., 2008). Moreover, oxygen free radicals could stimulate airway contraction and induce the proliferation of tracheal smooth muscle cells. The radicals can also indirectly increase the sensitivity of the airway to contractile mediators, further aggravating airway hyperresponsiveness (Vasconcelos et al., 2021). (3) This patient had a high level of serum IgE after PQ poisoning. IgE is a well-known factor that participates in asthma pathology. It initiates allergic reaction and increases prostaglandin D2 production from mastocytes. IgE also promotes the proliferation of the smooth muscle cells and collagen deposition during airway remodeling (Novosad and Krčmová, 2020).
The present case suggests that acute paraquat poisoning could not only cause pulmonary interstitial fibrosis as described in most studies, but also induce bronchial asthma attacks. However, not all patients present asthma symptoms, which may be related to the specificity of the lung injury repair process and individual genetic susceptibility. Thus, regular follow-up of the respiratory function for patients who survived PQ poisoning is necessary. For patients with complicated asthma symptoms, timely treatment and rehabilitation guidance need to be considered.
This work was supported by the Jiangsu Provincial key clinical specialty funds.
Conflict of interestThe authors declare that there is no conflict of interest.