2021 Volume 70 Issue 4 Pages 73-81
2021 Volume 70 Issue 4 Pages 73-81
Smallpox, which was eradicated globally in 1980, was brought to the indigenous people of South America by the Spaniards and decreased the population of Native Americans to roughly one-eighth in 50 years. The bubonic plague, also known as the “Black Death,” reduced the population of Europe by one-third after the invasion by Genghis Khan. Cholera, a disease that was brought to Japan from overseas by the “black ships” at the end of the Tokugawa shogunate, resulted in many deaths. All these historical pandemics show that major human migrations are accompanied by pandemics. Looking back over the first 20 years of the 21st century, we have seen five major pandemics: H5N1, the highly-pathogenic avian influenza in 1997; SARS in 2003; a novel strain of H1N1 influenza in 2009; MERS in 2012; and now in 2020, COVID-19. In light of the past two decades during which vast numbers of people have travel globally, we have faced with a pandemic every 4 or 5 years.
Before discussing the COVID-19 pandemic, let us briefly review the Spanish flu of 1918–1920, which resulted in a devastating pandemic. Spanish flu caused about 40 million deaths around the world and finally attenuated after 3 years. Because a virus can persist only as a parasite in human beings or animals, its best strategy for survival is to ensure that it does not terminate the hosts’ lives.
We have also seen that the number of patients and deaths from influenza in 2020 dropped drastically compared with previous years (Table 1, Fig. 1) thanks to the newly introduced practices of wearing face masks all the time and washing hands carefully after touching objects.
| Average of 1st to 4th week | Average of 5th to 8th week | Average of 9th to 12th week | Average of 49th to 52nd week | |
|---|---|---|---|---|
| 2017 | 23.5 | 26.9 | 10.7 | 10.6 |
| 2018 | 36.8 | 38.0 | 10.9 | 6.1 |
| 2019 | 41.5 | 22.8 | 3.9 | 17.4 |
| 2020 | 16.7 | 9.2 | 2.4 | 0.0 |
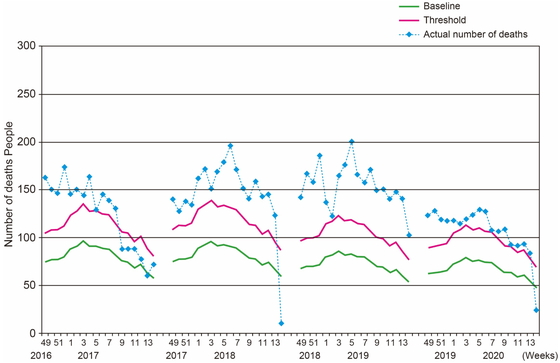
Number of deaths in Tokyo due to influenza from the 2016–2017 season to the 2019–2020 season.
Source: Infectious Disease Surveillance Center, National Institute of Infectious Diseases https://www.niid.go.jp/niid/ja/from-idsc/9627-jinsoku-qa.html
Usually, about 3000 people die from seasonal influenza every year, but this figure dropped significantly in 2020, as can be estimated from the Tokyo statistics shown in Fig. 1. Conversely, about 1800 people had died from COVID-19 as of November 2020; I believe that we need to keep this comparison in mind, while recognizing the serious risk posed by COVID-19.
One worrying aspect of the SARS-CoV-2 virus that causes COVID-19 disease is that there is a risk of becoming infected from people who appear to be healthy. This is in contrast with the seasonal influenza for which infectiousness peaks during the symptomatic stage; consequently, infection from seasonal influenza can be avoided as long as we stay clear of people coughing. Because the greatest risk of COVID-19 infectiousness is in the incubation period, the strategy of avoiding symptomatic patients is not a sufficient approach to minimizing COVID-19 infections.
There was a wave of COVID-19 infections in April 2020 and again in the summer, and now we are in the midst of yet another wave. The number of infections in countries such as France and Italy skyrocketed again in November 2020. The excess mortality rates in the United States and many countries in Europe are generally 60% higher than the annual mortality rates. Germany and Denmark are exceptions; there, the excess mortality rates had reached only 5% in April 2020. Consequently, deaths can be reduced even in countries evenly affected by the pandemic.
Fatality rates among different age groupsFatality rates differ depending on the age group of the patients. While there are very few deaths in patients in their 20s to 50s, COVID-19 is more likely to be fatal in patients over the age of 60. In Germany, where there is a significant number of patients over 60 years of age, the fatality rate among the elderly is relatively low. In Fig. 2, which was prepared by the Japan International Cooperation Agency (JICA: Fighting Against COVID-19 in Developing Countries), the horizontal axis shows the proportion of elderly people in the population and the vertical axis the number of deaths per million people. While most countries’ data fall around a rising line, there is one exception − Japan. Although the elderly account for the largest percentage of the population in Japan, compared to the other countries reported, Japan has a mortality rate that lies more or less similar to countries with young populations in regions such as Africa and Asia.
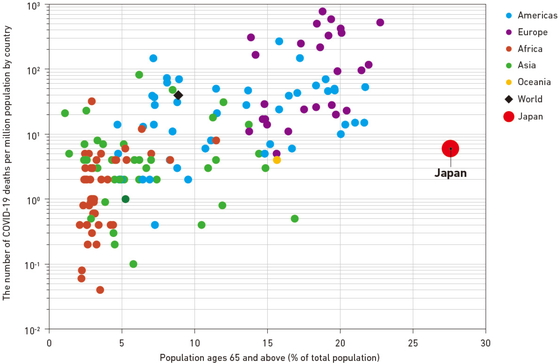
Association between the mortality rate from Covid-19 and the proportion of the population aged 65 years or more.
Source: Japan International Cooperation Agency https://www.jica.go.jp/COVID-19/en/responses/research/adtkbc00000005xc-att/JICA_COVID19.pdf
Ethnic differences play significant roles. The number of Black and Hispanic people who have been hospitalized was high in New York City. It is unclear whether such ethnic differences reflect biologic factors or socioeconomic factors. The difference between Caucasians and Asians is a matter of debate. Genetic differences in TMPRSS2 gene expression may be a contributing factor to the vulnerability of African-Americans, who have significantly higher expression of TMPRSS2 compared with other ethnicities and might be especially prone to infection as a result.
Stringency of countermeasuresLet us review whether the stringency of countermeasures, including school and restaurant closures and travel restrictions, affects the fatality rate. Because Sweden’s COVID-19 policy aimed for herd immunity, no strict measures were taken. Because Japan did not establish any punitive rules with penalties, the country also scores low on the scale of stringency of anti-COVID-19 measures. Of course, although there are some countries that enforced extreme lockdowns and achieved low fatality rates, looking at the mortality rates for Belgium, Spain, Italy and France, which enforced hard lockdowns, we can see that hard lockdowns do not necessarily mean that deaths can be prevented.
What are the reasons for the low mortality rate in Japan? One plausible explanation may be cross-immunity. The “Corona cold,” i.e., a relatively mild corona viral infection, was likely prevalent in East Asia a few years ago. Many people in East Asia could have contracted the disease and developed a certain degree of immunity. If such a mild immunity exists in East Asia, it may account for the low number of deaths due to COVID-19 infection. More than half of the elderly people who died in Italy and Spain had been resident in long-term care facilities; however, in Japan, many such deaths were circumvented by banning family visits to care facilities in the early stages of the pandemic.
Bacillus Calmette-Guérin vaccineThe low mortality rate in Japan may relate to the use of the Bacillus Calmette-Guérin [BCG] vaccine. Compared to America and Europe, where the BCG vaccine is not used any more, we see a low number of COVID-19 cases in countries in East Asia that use BCG. This fact led to the hypothesis that the BCG vaccine may be effective against COVID-19. In Israel, however, we can see that there is almost no difference in the prevalence between BCG-vaccinated birth cohorts born between 1979 and 1981 and non-BCG-vaccinated cohorts born between 1983 and 1985; this finding suggests that the BCG vaccine has little concrete effect in preventing COVID-19.
Adherence to face mask useThe relatively strict adherence to face mask use in Japan may also account for the low mortality rate. Although there has been one domestic infection in every four families when there is an infected family member within the household, this figure drops by about 80% when masks are worn by the patient at home. In testing with hamsters, if infected and uninfected hamsters are housed together, about two thirds become infected, but this figure drops by about half if protective masks are applied. However, if infected hamsters are masked, not to avoid becoming infected, but to prevent infection spreading to non-infected hamsters, it has been reported that the number of infections drops to about one-quarter, proving that masks are more effective in curbing the spread of infection than in preventing infection in the mask wearer. Furthermore, when masked and unmasked hamsters infected unmasked hamsters, whereas hamsters infected from unmasked hamsters developed serious symptoms, hamsters infected from masked hamsters developed only mild symptoms. Consequently, the number of shed virus particles is likely to be decreased in an infected person wearing a mask.
These experimental observations give further credence to the notion that COVID-19 can also be avoided if everyone wears masks; avoids closed spaces, crowded places, and close-contact settings; and washes their hands frequently. These measures have the positive externality of decreasing seasonal influenza infections.
Retrospective contact tracingWhen an infected person undergoes contact tracing, the person’s close contacts are identified because they potentially have been infected by the person of interest. However, in Japan, investigations go further back to find where infected persons could have become infected, e.g., closed spaces, crowded places, and close-contact settings, such as, live music clubs, tents at festivals, or pleasure boats with restaurants in winter when all the windows are closed. All these places have been identified as risky settings to be avoided by people at large. This method of retrospective contact tracing has been one of the successful approaches adopted in Japan.
Decreasing case fatality rate of COVID-19Figure 3 shows the pandemic waves in Japan with the number of infections shown in blue and the number of deaths in orange. Looking at the case fatality rate, i.e., the number of deaths in proportion to the number of infections, we can see that the figure to the middle of June 2020 was about 5%, and this subsequently dropped to 1%. This reduction likely indicates that the means to detect infections at an early stage and to provide effective treatment have been established, leading to a significant reduction in the case fatality rate.
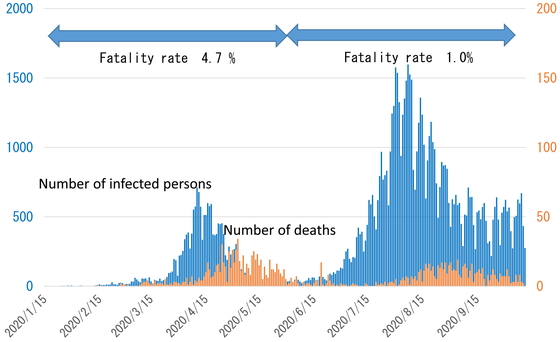
Number of infected people and deaths in Japan.
Source: Ministry of Health, Labour and Welfare
In Fig. 4, the number of COVID-19 infections in September 2020 are shown as green bars according to age group, and we can see that the numbers of infections of people in their 20s and 30s were extremely high. The case fatality rate is shown as a red line. We can see that the case fatality rate among those infected in their 80s was extremely high at 17.3%. Those in their 40s or older accounted for about 20% of total infections in July 2020, going on to rise to around half in late August, indicating that infections were gradually spreading from young people to older people.

Number of cases and fatality rate by age group in Japan.
Source: Trends in domestic outbreaks of new coronavirus infections (September 2, 2020)
*The “fatality rate” of new coronavirus infections here refers to the ratio of reported deaths to the total number of reports of designated infectious diseases in Japan by September 2, 2020. The number of deaths is thought to be almost entirely known, but the scale of the number of infected people who have not been diagnosed is unknown.
The death rate among severe COVID-19 patients aged 70 years or older dropped to about two-thirds of the previous figure after June 5, 2020. One of the reasons for this is that the use of steroids, for example, roughly doubled after June 5. Moreover, the use of remdesivir, almost nil before its approval in May 2020, subsequently came to be used in 20% of patients, and this may be a significant factor.
Polymerase chain reaction, antigen testing, and antibody testingFor diagnostic testing, the polymerase chain reaction (PCR) is most widely used. Antigen testing offers prompt qualitative/quantitative measures of the presence of the virus, whereas antibody testing determines whether the subject has been infected in the past. Although antibody testing is extremely fast, a negative result does not necessarily mean that the subject is not infected when tested, because one of the characteristics of antibodies is that it takes some time after infection for them to appear in the blood.
PCR testingPCR testing is extremely sensitive, and a person can test positive even if he or she has only limited virus particles in their swab. Based on the following two-scenarios, this could give a false-positive result. One scenario is that even after an infection has come to an end, non-viable fragments of the virus may remain in the throat or pharynx, yielding a positive result. One other possibility is that virus particles became trapped in the mucosal mucus and the infection was unsuccessful, but the trapped mucosal viruses were transferred to the sample swab. I believe that we must keep in mind that cases like this may produce a false positive result. Conversely, in the case of false negatives, taking a swab from an infected person from an area where there are no viruses may produce a negative result. This means that, at the initial stage of infection, the ratio of false negatives is extremrely high, and 20% at the lowest; in other words, at most, only 80% of cases of infection will be identified. Taking the possibilities of false positives and false negatives into consideration, we can see that this type of testing is not perfect.
Figure 5 shows different types of institutions where testing has been performed: the pink area shows public-sector testing and the cream-colored area private-sector testing, and we can clearly see that after mid-2020, private-sector testing had become more extensive than public-sector testing. The number of tests per population and the number of infections per population almost all fall in a band rising to the right. In other words, the number of tests increases linearly with the increase in the infected population, and in Japan, the number of tests in the early stages was certainly very low. While, of course, we can’t say the number of tests in Japan is extremely high compared to the number of infections thereafter, I believe that the number is not terribly low compared to global trends.

Number of PCR tests performed in different institutions.
Source: Ministry of Health, Labour and Welfare: https://www.mhlw.go.jp/stf/covid-19/kokunainohasseijoukyou.html
In the early stages of testing, a swab had to be inserted deep into the nose and this caused sneezing, so that medical workers taking samples had to wear proper personal protective equipment. Recently, however, for antigen and nucleic acid testing, adequate samples can be obtained by simply rotating a swab five times in the nasal cavity or nostrils. This being the case, rather than sampling being performed by medical workers, people wishing to be tested can simply take their own samples by rotating a swab in their nostrils five times, as long as they have been given clear instructions on what to do.
Former Prime Minister Abe said that the PCR testing pipeline had become clogged; this was because, in April 2020, PCR testing capacity was insufficient, and health centers were overworked. Also, there was a shortage of personal protective equipment. It is also noted that pre-pandemic preparations for PCR testing were not in place, and the number of health centers had been roughly halved as a result of a restructuring program; however, all kinds of tasks emerged that needed to be carried out to cope with the COVID pandemic. Public Health Centers take calls from residents requesting tests, make arrangements for callers who want to be tested, and decide at which hospitals persons testing positive will be hospitalized. Because ambulances will not transport persons testing positive to hospitals, public health centers have to take patients to hospitals and then also perform follow-up health checks. As well as all this, the various investigations mentioned above all have to be performed for each patient. With the exception of epidemiological surveillance, I believe that most tasks can be transferred elsewhere, or to the facility concerned, and I think that this is extremely important for preventing workflows from becoming overloaded.
There are protuberances on the SARS-CoV-2 virus called spikes, and when these spikes neatly fit into Y-shaped cellular transmembrane proteins such as TMPRSS2 (as mentioned above) they open as if someone had said “open sesame” and the virus enters the cell. Then, viral RNA emerges, is replicated, and returns to outer cellular layer where new viral particles are assembled. Because the genotypic composition of COVID-19 was first identified only in January 2020, no drugs have been specifically developed to treat COVID-19. However, drug repositioning has taken place to use drugs developed for other diseases in order to fight COVID-19. Among these drugs, dexamethasone, a steroid medication used to stop a runaway immune response, and remdesivir, a drug developed to treat Ebola hemorrhagic fever, are currently in use, whereas Avigan is still undergoing clinical trials.
VaccinationsThere are many kinds of vaccines in current use, ranging from those that give lifelong immunity to the measles to influenza vaccines that require annual inoculations and do not guarantee that recipients will not contract influenza, but may prevent serious symptoms. Vaccines for COVID-19, like influenza vaccinations, may require annual inoculations.
In addition, although vaccines have traditionally been prepared from inactivated viruses, this approach has proven not to be easy for COVID-19; consequently, vaccines that have been developed for COVID-19 have taken a genetic but somewhat untested approach. A typical example is the Pfizer vaccine that contains messenger RNA for the SARS-CoV-2 spike protein. Inoculated cells make and release the spike protein which the immune system identifies as alien and finally generates antibodies.
A number of COVID-19 vaccines have been developed by China and Russia, for example, countries not generally well-known in the field of innovative vaccines. Some vaccines require only a single inoculation, but many require two. Giving every citizen two inoculations with different intervals for different vaccines would be a daunting task, with difficulties such as temperature control of the vaccine vials. Also, looking at methods of inoculation, all the current COVID-19 vaccines require intramuscular injections. With the exception of the vaccine for human papillomavirus, injections we all receive nowadays are all via intradermal or subcutaneous injection. Giving two intramuscular injections, which can be painful, and the fact that the elderly will be the first to be vaccinated, vaccine rollout is an extremely challenging experience in Japan.
Once treatment capacity has been exceeded by the speed and magnitude of the pandemic, the health care system will collapse. When such a crisis becomes imminent, a state of emergency will be declared, and this measure, called a hammer, will reduce the number of infections. However, because a high-level state of emergence will render society incapable of functioning, measures to relax restrictions such as the “Go to Travel” campaign and shortening business hours are being taken to allow the “dance” to continue. It is considered that the resulting increases in the number of infections will lead to a repeated cycle of the hammer followed by the relaxation of restrictions (Fig. 6).

Countermeasures against coronavirus infections based on the number of new infections.
Source: Expert Meeting on Novel Coronavirus Disease Control – Status analysis and recommendations for countermeasures against new coronavirus infections (May 14, 2020): https://www.niph.go.jp/h-crisis/wp-content/uploads/2020/06/20200601111718_content_10900000_000630600.pdf
Looking at measures to cope with infections down the line, if we consider that such infectious diseases will emerge every 4 or 5 years, we need to be constantly aware of what capacity is available, even in “peace time.” A surge capacity is needed to get to grips with infectious diseases as soon as possible after they appear. I believe that it is worth considering measures such as the recruitment of non-active nurses as a reserve self-defense force; these nurses account for one-third of all nurses, and could be deployed to facilities such as health care centers. In addition, in countries and regions that we often consider to be successful in controlling COVID-19, such as Korea, Taiwan, and Singapore, the use of smartphone GPS for COVID-19 surveillance has been instigated by governments. While this may be characteristic of countries/regions with security concerns, the result has been that people with mild symptoms who are supposed to self-isolate at home can be quickly identified if they leave home. However, in Japan, to protect civil liberties, such steps would probably not be allowed; consequently, health care centers have to make calls to ensure that people are staying at home.
In circumstances where vaccines were not readily available, it was extremely important to wear masks and avoid closed spaces, crowded places, and close-contact settings. Consequently, risk communication was of prime importance to foster behavioral changes in the public. In situations where the number of available respirators and ECMOs is limited, it is particularly important to decide who will be treated with such equipment.
Shortage of personal protective equipmentThe shortage of personal protective equipment in April and May of 2020 caused a great deal of inconvenience, but the reason for this was that, although, for economic reasons, such equipment is mostly imported from the cheapest good-quality sources, the export of such equipment to Japan became prohibited when exporting countries were hit by the pandemic. At the same time, the demand-supply gap widened because demand drastically increased during the Japan’s pandemic. What we are doing now is, firstly, making a certain amount of equipment in domestic plants that still have sufficient capacity by providing subsidies, even it is economically inefficient. Also, sources of imports have been diversified to more than one country. Lastly, as with petroleum, we are stockpiling equipment over a certain scale so that no supply problems will be caused even if imports stop.
Hospital operationRegarding the business analysis of hospital operation, the biggest slump was in May 2020, as one would expect, and, although the absolute numbers were small, the most affected sector was comprehensive health checkups because it was considered nonessential and nonurgent; it has now become really hard to make reservations for such health checkups within the same fiscal year. Concerning hospitalized patients and outpatients, while there was a big dip in outpatients in May 2020, the outpatient situation more or less returned to normal in June. Reasons for the inevitable drop in hospitalizations by several percent include the need to sterilize wards and beds and to give incoming patients PCR tests. This means that hospitals cannot function at their previous levels of patient turnover and usage.
There has been a big drop in the number of outpatients at departments such as otolaryngology and pediatrics. To address damage to the business operations of medical institutions, the Government prepared a ¥1.2 trillion fiscal package to support the cost of the business operations of medical institutions. This will be distributed through local authorities, so it will inevitably take some time. It is difficult to make money available simply to cover a slump in business operations, because if money were to be made available to cover such slumps in medical institutions, then the question arises of what to do for the financial losses in the hospitality and travel industries. Therefore, funds are provided on condition that recipients are admitting COVID-19 patients, or if not, then to support care institutions. Interest-free financing is expanded without collateral to medical institutions suffering financial losses.
Regarding hospital business management, patients may hesitate to go to hospitals because of the fear of nosocomial COVID-19 infection. Additionally, there are other various factors which led to a drop in revenue, such as the occurrence of clusters of COVID-19 cases in hospitals resulting in a drop in the number of outpatients and patients being hospitalized. Furthermore, costs increased to ensure the availability of vacant beds in case of emergency or to remodel buildings to accept more COVID-19 patients. Looking at the situation before and after the advent of COVID-19, there have been winners and losers within medical institutions. This is especially the case with outpatient departments: the winners are trying to introduce proper appointment systems, zoned lines of patient flow, minimizing the accumulation of patients in waiting rooms. Therefore, these kinds of approaches are extremely important to facilitate the return of patients.
Concluding RemarksThere are four points to note, including views from specialists overseas. The first is that no one country can be safe unless all countries are safe, although this may not apply if we permanently closed our borders and shut off all exchanges with the outside world. The importance of interactions with the outside world is especially relevant for Japan which hosted the Olympics Games in July 2021. We will be unable to safeguard Japan unless steps are taken to ensure that vaccines and tests are available to developing countries equally.
The second is that we need the fire brigade when we encounter a fire. When novel influenza hit the globe in 2009, we put together a book of reflections on the pandemic that stated that the capacity of PCR testing and health center functions must be reinforced. However, we were unable to realize this at all over the following decade. Therefore, although we got off to a somewhat shaky start this time, we must take advantage of the current experience to prepare for future crises.
When Kiichi Nakai was awarded the Medal of Honor with Purple Ribbon, he said that what worried him was not only that the COVID-19 virus might penetrate the body, but also the heart and spirit. In other words, he was saying that excessive levels of fear and self-restraint will rob people of their enjoyment of life and, in one sense, damage society beyond reasonable limits.
On a final note, in 1962 when the Soviet Union deployed missiles in Cuba, thereby triggering the Cuban missile crisis, President Kennedy asked tired members of his cabinet and high officials after 13 days and nights without sleep, “Do you know what written characters the Chinese use to portray ‘crisis’?” He went on to say that it is written with two characters: the first meaning “danger” and the second, “opportunity.” While the crisis we are facing now is extremely dangerous, it is also an opportunity, and that, hopefully, opens the curtain to a more robust future. I hope that, armed with our experience of the current crisis, Japanese society and its medical system will develop and evolve to ever greater heights.
The author would like to express sincere condolences to the friends and family of those who lost their lives and are suffering from COVID-19 and gratitude to those health care professionals assisting patients and to public health workers fighting fiercely against this pandemic.