Article ID: 2017-0014-OA
Article ID: 2017-0014-OA
Obturator hernia (OH) is a rare condition that accounts for 0.073–1% of abdominal hernias and 0.48% of bowel obstructions. OH frequently occurs in elderly women, with an incidence that increases with age. The only treatment for OH is surgical intervention, and the approaches used vary greatly. Consequently, a well-defined consensus has not yet emerged. We assessed the efficiency and safety of the midline extraperitoneal approach for OH. Six patients with OH repaired using the midline extraperitoneal approach at KKR Sapporo Medical Center between April 2011 and January 2016 were included in the study. We retrospectively evaluated the patient characteristics, intraoperative findings, and the postoperative course. All patients were elderly women [median age, 90 (range, 79–92) years], with a median body mass index of 17.0 (range, 15.6–18.3) kg/m2 at presentation. All had symptoms associated with bowel obstruction: two patients presenting with leg pain had the Howship–Romberg sign. In two patients, bowel resection was required because of irreversible ischemic changes. Five patients had coexisting femoral and inguinal hernias that were repaired by bilateral mesh repair. One patient had aspiration pneumonia as a postoperative complication. All patients were discharged alive, without infection or recurrence. OH can be efficiently and safely repaired using the midline extraperitoneal approach. This approach establishes the diagnosis of OH, avoids injuring obturator vessels, gives improved exposure of the obturator canal, enables identification and simultaneous repair of other pelvic hernias, and facilitates bowel resection. This approach reduces the risk of mesh infection in patients undergoing bowel resection.
Obturator hernia (OH) is a rare condition that accounts for 0.073–1% of all abdominal hernia cases and 0.48% of all bowel obstruction cases.1,2 OH frequently occurs in elderly women, with an incidence that increases with age. The only treatment for such patients is surgical repair, and the approaches used vary greatly, e.g., laparotomy, inguinal approach, and the midline extraperitoneal approach, among others. Consequently, a clear consensus on the management of OH has not yet emerged. This study aimed to determine the efficiency and safety of midline extraperitoneal repair of OH.
Six patients with OH repaired using the midline extraperitoneal approach at KKR Sapporo Medical Center during a 5-year period from April 2011 to January 2016 were included. From the hospital records, we retrospectively investigated the patients’ age, sex, body mass index (BMI), preexisting illness, symptoms, affected side, computed tomography (CT) findings, laboratory data, intraoperative findings, postoperative course, and complications. The protocol for this research project was approved by a suitably constituted Ethics Committee of the institution and it conformed with the provisions of the Declaration of Helsinki. Informed consent was obtained from all subjects and/or their guardians.
Surgical techniqueFor the midline extraperitoneal approach, the abdomen was accessed from a lower midline incision, followed by extraperitoneal separation of the preperitoneal space from the lateral suprapubic edge. This was followed by midline separation of the pubis and the bladder. The internal obturator muscle was exposed from the Cooper ligament, and the obturator canal was approached for extraperitoneal insertion of the prosthetic mesh. Concomitantly, the presence of other pelvic hernias, such as inguinal and femoral hernias, could be observed and repaired with the same mesh. The obstructed small bowel segment was located and replaced easily by laparotomy through the same incision (Fig. 1). During replacement, we employed the water pressure method.
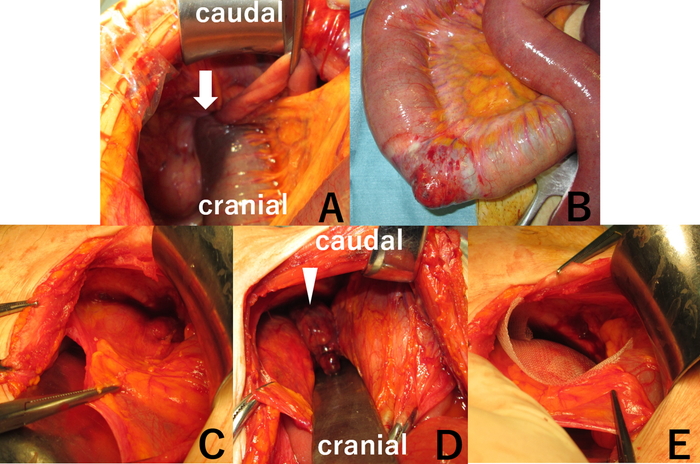
Midline extraperitoneal approach for obturator hernias.
(A) The incarcerated small intestine is observed in the abdominal cavity (arrow). (B) The small intestine was replaced without injury and was ischemic at the incarcerated part. (C) The preperitoneal space was separated from the lateral suprapubic edge. This was followed by midline separation of the pubis and the bladder. (D) The hernia sac was observed (arrowhead). (E) The internal obturator muscle was exposed from the Cooper ligament, and the obturator canal was approached for extraperitoneal insertion of the prosthetic mesh.
The characteristics and CT findings of all patients are shown in Table 1. The patients were elderly women with a median age of 90 years (range, 79–92 years) and a median BMI of 17.0 kg/m2 (range, 15.6–18.3 kg/m2) at presentation. Four patients were multiparous. Five patients (all excluding case 1) suffered from preexisting illness. Two patients had undergone previous abdominal surgeries. All patients were symptomatic for bowel obstruction at a median duration of 47.5 h (range, 25–90 h). The incarcerated organ was the small intestine in all cases. On CT scans, the contrast effect of the incarcerated small intestine was weakened in two cases, and ascites was recognized. Two patients presented with leg pain, and both were positive for the Howship–Romberg sign.
| Case | Age (years) | Sex | BMI (kg/m2) |
Pre-existing illness | Prior abdominal operation | Number of children |
Symptoms | Duration of symptoms (hours) | Howship– Romberg sign | Affected side | Contrast effect on CT |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 89 | F | 16.4 | – | – | 2 | Vomiting, abdominal pain |
90 | – | Right | + |
| 2 | 90 | F | 15.9 | PD | – | 3 | Vomiting, abdominal pain |
80 | – | Right | + |
| 3 | 79 | F | 15.6 | HT | – | 1 | Nausea, leg pain | 65 | + | Light | Weakened |
| 4 | 92 | F | 18.3 | HT | – | 3 | Vomiting | 30 | – | Light | N/A |
| 5 | 91 | F | 18.1 | HT, DM | Appendectomy | 5 | Nausea, leg pain | 30 | + | Right | Weakened |
| 6 | 90 | F | 17.6 | Af, PPM, AMI (PCI and anticoagulant agent) |
Appendectomy | 1 | Vomiting, abdominal pain |
25 | – | Light | + |
PD, Parkinson’s disease; HT, hypertension; DM, diabetes mellitus; Af, atrial fibrillation; PPM, permanent pace maker; AMI, acute myocardial infarction; PCI, percutaneous coronary intervention
Intraoperative findings, the duration of hospitalization, and postoperative complications are shown in Table 2. In five cases, Richter’s hernia was observed and the OH canal could be recognized. Bowel resection as a result of irreversible ischemic changes was required in two cases. Five patients (all except case 4) had coexisting femoral and/or inguinal hernias. Mesh repair was performed unilaterally in one patient and bilaterally in five patients. The median duration of hospitalization was 15.5 days (range, 7–24 days). Case 4 had aspiration pneumonia as a postoperative complication. All patients were discharged without infection or recurrence of the hernias as of 10–31 months postoperatively.
| Case | Hernia type | Hernia canal | Bowel resection | Coexisting hernia | Hospitalization (days) | Complication |
|---|---|---|---|---|---|---|
| 1 | Richter | Bilateral | – | Bilateral femoral | 13 | – |
| 2 | Richter | Bilateral | – | Right inguinal, left femoral | 24 | – |
| 3 | Richter | Left | + | Left femoral | 17 | – |
| 4 | Richter | Bilateral | – | – | 22 | Aspiration pneumonia |
| 5 | Total | Bilateral | + | Bilateral femoral | 14 | – |
| 6 | Richter | Bilateral | – | Bilateral inguinal | 7 | – |
OH is a rare form of abdominal wall hernia that accounts for 0.073–1% of all hernias.1,2 OH occurs most commonly in emaciated, elderly, multiparous women as a result of the decrease of fat tissue around the obturator canal (caused by aging), the slackness of pelvic-supporting tissues and the peritoneum (caused by childbirth), and a wide and strongly inclined pelvis.3 Similar to the findings of previous reports, our series showed that all patients were women with BMIs <18.5 who had experienced childbirth. In recent reports, 63% of patients had bilateral OH, and 88% had associated inguinal hernias.4 In our patients, other hernias and bilateral OH were recognized in five cases. Therefore, we recommend the assessment of the opposite side and other hernia canals during surgery.
OH is an important cause of bowel obstruction. It has been reported that 90% of OH patients present with symptoms of bowel obstruction, and the mortality rate varies from 12% to as high as 70%, likely as a result of delayed diagnosis.5,6,7,8 Moreover, we consider that the poor physiologic reserve in elderly people and preexisting medical conditions complicating perioperative management also contribute to the high mortality rate of OH. In our study, five patients had preexisting illnesses and all patients were emaciated because they could not consume enough food and water because of the bowel obstruction.
The diagnosis of OH is challenging because the symptoms and clinical signs are not specific. Particularly, in elderly patients, pain can be induced by spine and hip arthropathy. CT plays an important role in the preoperative diagnosis and early treatment of OH. The diagnostic accuracy of OH is 80%–100% with the use of CT, but only 5% without CT. Moreover, the use of CT can improve preoperative planning, reduce the need for bowel resection, and reduce mortality and the risk for postoperative complications.2,8,9,10,11,12 Importantly, we can evaluate the viability of the incarcerated intestine by the degree of contrast effect on CT scans. In fact, in all our patients, we were able to successfully diagnose OH and evaluate the viability of the incarcerated intestine early using CT scans.
Many operative approaches have been reported for OH repair; these include transabdominal, inguinal, retropubic, laparoscopic, and extraperitoneal approaches. Each approach has its own merits and demerits; consequently, a standard approach has not yet been established. The retropubic approach enables identification of the bilateral obturator canals; however, because of the potential risk for infection of prosthetic materials, the retropubic approach may not be appropriate for patients who require bowel resection. The thigh and inguinal approaches enable easy access to the OH and help reduce the damage of the obturator nerve and vessels. Nevertheless, in these approaches, the peritoneal cavity cannot be observed directly; therefore, the viability of the intestine and the side opposite the OH cannot be inspected.
The laparoscopic approach, including the transabdominal and extraperitoneal approaches, lessens postoperative pain, enables earlier oral intake, shortens hospitalization, and decreases the risk for incisional hernia because of smaller wounds compared with laparotomy. However, OH patients usually have bowel obstruction; therefore, sufficient visualization to rule out bowel necrosis and allow hernia repair is often difficult because of the dilated intestine and the limited intraabdominal space. Tucker et al. reported that complications occur in 5.3% of patients as a result of technical difficulty and poor visibility.13 In most studies, laparoscopic OH repair has been limited to cases that were found coincidentally during repair of other hernias or during other pelvic procedures and in those undergoing elective repair.14,15
The abdominal approach is via a low midline incision and is commonly favored because it enables immediate release of small bowel obstruction.16 Consequently, we perform laparotomy via a midline incision. Moreover, with this approach, the hernia canal can be accessed extraperitoneally after inspection and resection of the intestine. We call this technique the midline extraperitoneal approach. The advantages of this approach include the ability to establish the diagnosis of OH and other hernias, the avoidance of injury to obturator vessels, easy exposure of the obturator canal, the simultaneous repair of other pelvic hernias, and the safe resection of the intestine as necessary. Moreover, in cases in which entering the abdominal cavity is not necessary, this approach can minimize damage of the intestine and prevent adhesion in the abdominal cavity, thereby facilitating future surgery.
The obturator artery has some variations, such as the corona mortis, or “crown of death,” which is a variant connecting the inferior epigastric and obturator artery.17 Using our approach, this vessel can be observed easily to reduce the risk of damage. In our series, the presence of post-laparotomy adhesions did not affect this approach. Moreover, postoperative hemorrhage, which may cause prosthetic mesh infection, was not observed even in the patient on antithrombotic therapy. This was because our approach enabled good visualization and efficient operation and we performed safe and effective hemostasis.
Protective replacement of the incarcerated intestine plays an important role in avoiding injury to the intestine and avoiding contamination of the surgical field, thereby facilitating effective use of prosthetic mesh. Hayama et al. reported the feasibility of the water pressure procedure.18 In this method, a narrow Nelaton catheter is inserted into the obturator foramen followed by replacement of the intestine by gradual water injection to create an internal pressure in the hernia space. Using this method, we could replace the incarcerated intestine conservatively without injuring the intestine because the increase in the OH sac pressure as a result of water injection is gradual and uniform. In this study, we performed this technique routinely during OH repair and successfully replaced the intestine without bowel injury.
Various procedures have been reported for the closure of OH defects; these include simple peritoneal suture; closure with a local flap using the peritoneum, bladder, or ligaments; and permanent prosthesis.8,19,20 The recurrence rate of nonmesh repair after 3 years is reportedly 22%.21 Most reports describe use of the Kugel patch or flat meshes.20,22,23 Mesh plug repair may worsen obturator neuralgia because the device shrinks and forms a rigid prosthetic tumor.24 Therefore, we routinely use flat meshes, such as Bard mesh (CR Bard Inc., Murray Hill, NJ, USA) or ULTRAPROTM (Ethicon, Somerville, MA, USA), that we can trim to fit the preperitoneal space and cover other hernias simultaneously. The use of prosthetic mesh in patients undergoing bowel resection runs the risk of mesh infection. Therefore, procedures should be performed to reduce the risk of infection; these include protection of the wound, disposal of the instruments used during bowel resection, changing gloves after bowel resection, closure of the parietal peritoneum before mesh insertion, and placement of an indwelling drainage catheter in the preperitoneal space, as necessary. In our study, mesh infection did not occur. This is because the meshes were not inserted in the abdominal cavity and we performed the above-mentioned procedures. Although accumulation of further evidence is needed, mesh repair even in OH cases with bowel resection may be feasible.
OH mainly affects elderly patients who have reduced cardiopulmonary function. Moreover, these patients are often severely dehydrated and malnourished as a result of delayed diagnosis. The patients in this study all had severe dehydration, malnutrition, and poor physical status. However, although our patients needed relatively prolonged hospitalization for rehabilitation, they all survived. Therefore, we consider that the midline extraperitoneal approach is feasible, less invasive, and safe.
This retrospective study had limitations in terms of small sample size and the short follow-up period. Furthermore, in the future, we need to accumulate more cases and follow up the patients for a longer period.
The midline extraperitoneal approach for repair of OH was feasible and safe, enabled simultaneous repair of all coexisting hernias, and resulted in no short-term recurrence. Mesh infection did not occur, even in patients undergoing bowel resection. Moreover, we could simultaneously repair all coexisting hernias.
We would like to thank our surgical colleagues at KKR Sapporo Medical Center. We received no funding for this work.
The authors declare no conflicts of interest in relation to this article.