Abstract
Some patients with hypertrophic cardiomyopathy (HCM) develop systolic dysfunction, called
the dilated phase of HCM (d-HCM), which is associated with increased morbidity and
mortality. We conducted a retrospective study using an HCM database to clarify the
incidence, clinical characteristics, and long-term outcomes of d-HCM. We analyzed an HCM
cohort consisting of 434 patients (273 with apical HCM and 161 with non-apical HCM; 18 had
obstructive HCM, 16 had dilated HCM, and 127 had other HCM) diagnosed by echocardiography
in our hospital between 1991 and 2010. The follow-up period was 8.4 ± 6.7 years. The mean
age at final follow-up was 67 ± 14 years, and 304 patients (70%) were men. The mean age of
the 16 d-HCM patients at the initial visit was 45 ± 17 years, the age at final follow-up
was 59 ± 18 years, and 13 were men. Thirteen d-HCM patients developed atrial fibrillation
and six patients developed ischemic stroke. Twelve d-HCM patients were implanted with
cardiac devices: one pacemaker, nine implantable cardioverter-defibrillators, and two
cardiac resynchronization therapy with defibrillator. Five patients died of progressive
heart failure at the age of 61 ± 23 years. The age at the initial visit and final
follow-up were lower and the NYHA class, brain natriuretic peptide levels, and left
ventricular function at initial evaluation were worse in the d-HCM group. Univariate
analysis demonstrated that a lower age at the initial visit was associated with d-HCM
(hazard ratio 0.955/1 year increase; 95% CI 0.920–0.991, P = 0.015). In
our HCM cohort, the incidence of d-HCM was 4%. A high prevalence of atrial fibrillation
and cerebral infarction and poor prognosis were noted in this group, despite patients
undergoing medication and device implantation.
Introduction
Hypertrophic cardiomyopathy (HCM) is a genetically determined heart muscle disease
characterized by left ventricular hypertrophy of various morphologies with a wide range of
clinical manifestations and hemodynamic disturbances.1,2,3,4,5 Patients
with HCM develop various symptoms, including dyspnea, fatigue, chest pain, palpitations,
syncope due to diastolic dysfunction, myocardial ischemia, and atrial or ventricular
arrhythmias. For the majority of HCM patients, disease progression is not aggressive. The
annual mortality rate of HCM patients is estimated to be about 1%. Sudden cardiac death
(SCD) and embolic stroke caused by atrial fibrillation are major causes of death in patients
with HCM. However, some patients with HCM develop systolic dysfunction, called dilated-phase
HCM (d-HCM), which is associated with increased morbidity and mortality.6,7,8 Dilatation
of the cardiac cavity and thinning of the ventricular wall as a result of extensive
myocardial fibrosis is the underlying pathogenesis of d-HCM. The exact clinical
characteristics, proper pharmacological treatment, and long-term prognosis of d-HCM remain
unclear. We conducted a retrospective study to investigate the clinical characteristics and
predictive factors for the development of d-HCM.
Subjects and Methods
We retrospectively analyzed a cohort consisting of 434 patients diagnosed with HCM by
echocardiography at Keio University hospital between 1991 and 2010. Of the 434 patients, 273
had apical HCM and 161 had non-apical HCM; of the 161 non-apical HCM cases, 18 were
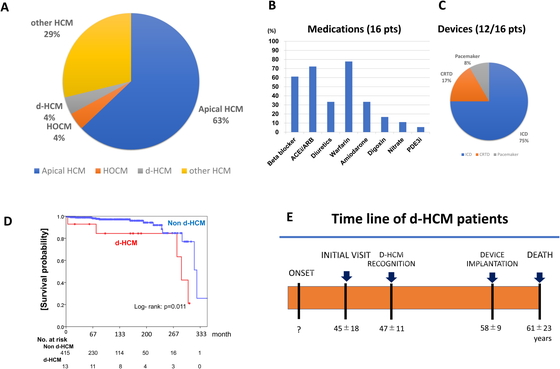
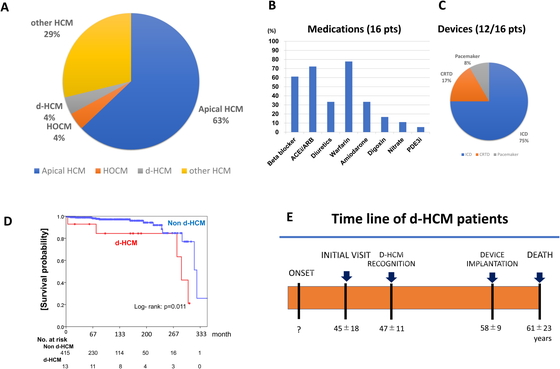
obstructive HCM, 16 were dilated HCM, and 127 were other HCM (Fig. 1A). The baseline demographic and clinical data were collected
for all patients using electronic medical records or clinical charts. The clinical
information acquired during routine follow-up was also collected. The mean follow-up period
was 8.4 ± 6.7 years. The mean age at final evaluation was 67 ± 14 years, and 304 patients
(70%) were men. The diagnosis of HCM was based on echocardiographic documentation indicating
a hypertrophied left ventricle (LV) in the absence of other cardiac or noncardiac diseases.
The diagnosis of d-HCM was based on echocardiographic analysis indicating the development of
global systolic dysfunction over time after the initial diagnosis of HCM. This study was
approved by the Internal Board of Keio University School of Medicine. (Approval number:
20100171)
Statistical analysis
Continuous variables are presented as the mean ±SD, and categorical variables as numbers
and proportions. Continuous variables were compared using a Mann–Whitney U test. Categorical
variables were compared between groups using the chi-square test. Univariate analysis was
performed, and all variables with a P value of <0.2 were included in the
multivariate analysis using Cox-regression analysis. The survival rates of the patients were
evaluated using the Kaplan–Meier method and compared between groups defined by several
different parameters using the log-rank test. Statistical analyses were performed using IBM
SPSS Statics software (Version 23). A P value of <0.05 was considered
statistically significant.
Results
Table 1 shows the clinical characteristics of
the 16 d-HCM patients. Two of the 18 patients initially diagnosed. The mean age of the 16
d-HCM patients at the initial visit to our hospital was 45 years, and the mean age at final
evaluation was 60 years. Of this group, 72% were male, the mean ejection fraction (EF) at
the time of evaluation was 46%, atrial fibrillation (AF) was noted in 72%, and stroke was
noted in 44%. The mean CHADS score was 1.6, and ventricular tachycardia/ ventricular
fibrillation (VT/VF) developed in 11 patients. Finally, 6 of the 16 patients died of
progressive heart failure at the mean age of 61 years. The reasons for the initial hospital
visit were electrocardiogram (ECG) abnormality identified during a health check in two
patients; chest pain in two patients; and syncope, congestive heart failure, palpitation,
atrio-ventricular block, and VT in one patient each.
Table 1.
Clinical characteristics of the 16 d-HCM patients
| No |
Age I/ II (years) |
Sex |
NYHA |
LVDd (cm) |
LVDs
(cm) |
LVEF
(%) |
AF |
Stroke |
CHADS2
/VASc |
VT/VF |
Device |
F/U
(years) |
Out-come
(age, years) |
| 1 |
48/62 |
M |
2 |
7.8 |
6.9 |
24 |
- |
- |
0/0 |
VT |
ICD |
14 |
Alive |
| 2 |
44/52 |
M |
1 |
4.7 |
3.3 |
49 |
CAF |
+ |
4/4 |
VF |
ICD |
8 |
Alive |
| 3 |
63/71 |
M |
3 |
5.8 |
5.4 |
19 |
CAF |
- |
1/1 |
VT/VF |
ICD |
18 |
Dead, 72 |
| 4 |
46/63 |
F |
3 |
7 |
6.1 |
27 |
PAF |
- |
1/2 |
VT |
CRTD |
17 |
Alive |
| 5 |
20/45 |
F |
1 |
4.8 |
3.9 |
39 |
CAF |
+ |
2/3 |
- |
- |
15 |
Alive |
| 6 |
48/73 |
M |
2 |
5.7 |
4.9 |
26 |
CAF |
- |
2/2 |
VT |
ICD |
25 |
Alive |
| 7 |
62/68 |
M |
2 |
6.6 |
5.5 |
42 |
CAF |
+ |
1/1 |
- |
- |
8 |
Dead, 75 |
| 8 |
73/78 |
M |
1 |
4.6 |
3.2 |
50 |
PAF |
+ |
2/3 |
- |
- |
5 |
Dead, 68 |
| 9 |
26/40 |
M |
1 |
6.4 |
4.9 |
55 |
CAF |
- |
2/2 |
VT |
ICD |
14 |
Alive |
| 10 |
52/70 |
M |
2 |
5.5 |
3.7 |
57 |
- |
- |
1/2 |
VT |
CRTD |
18 |
Alive |
| 11 |
39/61 |
M |
1 |
6 |
3.7 |
48 |
CAF |
+ |
1/1 |
VT |
ICD |
22 |
Alive |
| 12 |
73/88 |
M |
2 |
5.2 |
4 |
54 |
PAF |
- |
3/4 |
- |
- |
15 |
Alive |
| 13 |
45/68 |
F |
2 |
4.5 |
3.5 |
53 |
CAF |
+ |
1/2 |
VT |
ICD |
23 |
Alive |
| 14 |
55/68 |
F |
1 |
6.1 |
5.1 |
42 |
- |
- |
3/4 |
- |
- |
13 |
Dead, 69 |
| 15 |
1/15 |
M |
1 |
6.6 |
5.6 |
39 |
PAF |
- |
1/1 |
VT |
ICD |
14 |
Dead, 15 |
| 16 |
44/58 |
M |
1 |
6.3 |
5.2 |
36 |
PAF |
- |
2/2 |
VT |
ICD |
14 |
Alive |
Age I, age at initial visit; Age II, age at final evaluation; CAF, persistent atrial
fibrillation; F/U, follow up; PAF, paroxysmal atrial fibrillation.
In most d-HCM patients, adequate medical therapy was administered, as shown in Fig. 1B. Among the 16 d-HCM patients, implantable
cardioverter-defibrillators (ICDs) were implanted in 9 patients, cardiac resynchronization
therapy with defibrillator (CRTDs) in 2 patients, and a pacemaker in 1 patient, as shown in
the Fig. 1C. In most patients, medications, mainly
for controlling congestive heart failure and anticoagulation for atrial fibrillation, were
strengthened after the transition to d-HCM. Table
2 shows the baseline characteristics at the initial visit of patients with d-HCM
and with HCM. Patients were younger at the initial visit and at final evaluation in the
d-HCM group. The New York Heart Association (NYHA) classification; the CHADS score; and the
incidence of syncope, heart failure, AF, stroke, and ICD implantation was higher in the
d-HCM group. Table 2 also shows the laboratory,
echocardiographic, and ECG data at the initial visit of patients with d-HCM and with HCM.
Brain natriuretic peptide (BNP) levels, the left atrial dimension (LAD), left ventricular
end-diastolic dimention (LVDd), and left ventricular end-systolic dimention (LVDs) were
larger in the d-HCM group. The EF and the amplitude of RV5 plus SV1 were smaller in the
d-HCM group. Table 3 shows Cox proportional
hazards regression analysis to determine which parameters predict the development of d-HCM.
A younger age at the initial visit and at the final evaluation and the presence of syncope
and heart failure were associated with developing d-HCM. The following parameters were
associated with the development of d-HCM: a higher (eGFR); a larger LAD, LVDd, or LVDs; a
smaller EF; and a wide QRS. Fig. 1D shows
Kaplan–Meyer survival curves for d-HCM patients compared with non-d-HCM patients. d-HCM
patients had a significantly worse prognosis than that of non-d-HCM patients. The average
timeline of d-HCM patients is presented in Fig.
1E. The mean age at the initial visit was 45 years and that at recognition of d-HCM
was 47 years. Device implantation was performed at a mean age of 58 years, and death
occurred at a mean age of 61 years. We could not obtain the actual age at disease onset in
these patients.
Table 2.
Baseline characteristics of patients with d-HCM vs. HCM at initial visit
|
Overall
(n=434) |
d-HCM
(n=16) |
Non-d-HCM
(n=418) |
P value |
| F/U period (day) |
2928 ± 2400 |
4901 ± 3084 |
2862 ± 2349 |
0.011 |
| Male, n (%) |
304 (70) |
13 (72) |
291 (70) |
0.8369 |
| Age at initial visit (years) |
59.1 ± 13.9 |
45.2 ± 17.3 |
59.6 ± 13.5 |
0.001 |
| Age at final evaluation (years) |
67.2 ± 14.0 |
58.6 ± 17.6 |
67.5 ± 13.7 |
0.026 |
| Body length (cm) |
162.8 ± 8.9 |
162.9 ± 6.9 |
162.8 ± 9.0 |
0.815 |
| Body weight (kg) |
63.9 ± 12.1 |
65.5 ± 12.1 |
63.8 ± 12.1 |
0.616 |
| BMI (kg/m2) |
24.0 ± 3.6 |
23.8 ± 4.1 |
24.0 ± 3.6 |
0.967 |
| SBP (mmHg) |
138 ± 21 |
139 ± 20 |
138 ± 21 |
0.108 |
| DBP (mmHg) |
81 ± 14 |
78 ± 13 |
81 ± 14 |
0.542 |
| HR (bpm) |
70 ± 13 |
70 ± 18 |
70 ± 13 |
0.901 |
| NYHA |
1.1 ± 0.3 |
1.3 ± 0.5 |
1.1 ± 0.3 |
0.015 |
| Syncope, n (%) |
37 (9) |
4 (22) |
33 (8) |
0.038 |
| Heart failure, n (%) |
96 (22) |
10 (56) |
86 (21) |
<0.001 |
| Hypertension, n (%) |
272 (63) |
8 (44) |
264 (63) |
0.1024 |
| Diabetes, n (%) |
77 (18) |
4 (22) |
73 (18) |
0.6113 |
| AF, n (%) |
162 (37) |
13 (72) |
149 (36) |
0.018 |
| CHADS2 |
1.2 ± 1.0 |
1.9 ± 1.0 |
1.2 ± 1.0 |
0.017 |
| CHA2DS2-VASc |
2.1 ± 1.5 |
2.3 ± 1.1 |
2.1 ± 1.5 |
0.377 |
| Stroke, n (%) |
45 (10) |
8 (44) |
37 (9) |
<0.001 |
| Pacemaker, n (%) |
30 (7) |
1 (6) |
29 (7) |
0.8167 |
| ICD, n (%) |
25 (6) |
11 (61) |
14 (3) |
<0.001 |
| FH |
22 (5) |
1 (6) |
21 (5) |
0.9234 |
| Laboratory data |
| Creatinine (mg/dl) |
0.9 ± 0.5 |
0.9 ± 0.2 |
1.0 ± 0.5 |
0.689 |
| eGFR (ml/min/1.73m2) |
65 ± 20 |
71 ± 29 |
65 ± 20 |
0.797 |
| BNP (pg/ml) |
249 ± 296 |
432 ± 332 |
241 ± 292 |
0.005 |
| Echocardiographic data |
| LAD (cm) |
4.0 ± 0.7 |
4.6 ± 0.8 |
4.0 ± 0.7 |
0.003 |
| LVDd (cm) |
4.7 ± 0.6 |
5.3 ± 0.8 |
4.7 ± 0.5 |
0.003 |
| LVDs (cm) |
2.8 ± 0.5 |
3.9 ± 0.8 |
2.8 ± 0.5 |
<0.001 |
| EF (%) |
78 ± 8.8 |
60 ± 14 |
78 ± 7.3 |
<0.001 |
| IVS (cm) |
1.3 ± 0.3 |
1.3 ± 0.2 |
1.3 ± 0.3 |
0.785 |
| PW (cm) |
1.0 ± 0.1 |
1.0 ± 0.1 |
1.0 ± 0.1 |
0.952 |
| ECG parameters |
| QRS (ms) |
100 ± 21 |
113 ± 33 |
100 ± 20 |
0.081 |
| QT (ms) |
412 ± 40 |
414 ± 57 |
413 ± 40 |
0.911 |
| QTc (ms) |
427 ± 30 |
432 ± 36 |
426 ± 29 |
0.71 |
| RV5+SV1 (mV) |
4.5 ± 1.7 |
3.2 ± 1.4 |
4.5 ± 1.7 |
0.004 |
BMI, body mass index; CRT, cardiac resynchronization therapy; DBP, diastolic blood
pressure; FH, family history; HR, heart rate; IVS, interventricular septum; PW,
posterior wall; SBP, systolic blood pressure
Table 3.
Cox proportional hazards regression model to predict d-HCM
|
Univariate |
|
HR |
95%CI |
P |
| Male, n (%) |
0.788 |
0.245–2.533 |
0.689 |
| Age at initial visit (1 year increase) |
0.966 |
0.920–0.991 |
0.021 |
| Age at final evaluation (1 year increase) |
0.937 |
0.905–0.970 |
<0.001 |
| Body length (1 cm increase) |
1.035 |
0.943–1.136 |
0.465 |
| Body weight (1 kg increase) |
1.024 |
0.970–1.082 |
0.393 |
| BMI (1 kg/m2 increase) |
0.996 |
0.792–1.252 |
0.972 |
| SBP (1 mmHg increase) |
0.972 |
0.941–1.004 |
0.084 |
| DBP (1 mmHg increase) |
0.973 |
0.936–1.012 |
0.171 |
| Heart rate (1 bpm increase) |
1.002 |
0.956–1.050 |
0.944 |
| NYHA (1 increase) |
2.214 |
0.859–5.708 |
0.1 |
| Syncope, n (1% increase) |
3.75 |
1.148–12.242 |
0.029 |
| Heart failure, n (1% increase) |
6.272 |
1.996–19.711 |
0.002 |
| Hypertension, n (1% increase) |
2.518 |
0.808–7.847 |
0.111 |
| Diabetes, n (1% increase) |
1.156 |
0.345–3.871 |
0.814 |
| AF, n (1% increase) |
2.861 |
0.889–9.211 |
0.063 |
| CHADS2 (1 increase) |
1.592 |
0.930–2.728 |
0.09 |
| CHA2DS2-VASc (1 increase) |
1.196 |
0.796–1.797 |
0.388 |
| FH, n (1% increase) |
1.97 |
0.249–15.599 |
0.521 |
| Laboratory data |
| Creatinine(1 mg/dl increase) |
0.381 |
0.040–3.589 |
0.399 |
| eGFR (1 mL/min/1.73m2 increase) |
1.022 |
1.001–1.044 |
0.04 |
| BNP (1 pg/ml increase) |
1.001 |
1.000–1.002 |
0.13 |
| Echocardiographic parameters |
| LAD (1 cm increase) |
1.878 |
1.093–3.224 |
0.022 |
| LVDd (1 cm increase) |
11.073 |
4.148–29.560 |
<0.001 |
| EF (1% increase) |
0.868 |
0.826–0.912 |
<0.001 |
| IVS (1 cm increase) |
0.638 |
0.083–4.918 |
0.667 |
| PW (1 cm increase) |
0.293 |
0.002–35.736 |
0.617 |
| ECG parameters |
| QRS (1 ms increase) |
1.028 |
1.011–1.046 |
0.001 |
| QT (1 ms increase) |
1.004 |
0.991–1.017 |
0.521 |
| QTc (1 ms increase) |
1.01 |
0.992–1.027 |
0.278 |
| RV5+SV1 (1 mV increase) |
0.681 |
0.463–1.000 |
0.05 |
CI, confidence interval; HR, hazard ratio.
To summarize, in our cohort, the incidence of d-HCM in HCM patients was 4%. Of the 16 d-HCM
patients, 13 developed AF and 6 developed ischemic stroke. Twelve d-HCM patients were
implanted with cardiac devices: 1 pacemaker, 9 ICDs, and 2 CRT-Ds. Five d-HCM patients died
from progressive heart failure (HF) at a mean age of 61 ± 23 years. In the d-HCM group, the
age at the initial visit and at the final evaluation were lower, and the NYHA class, BNP
levels, and LV function at initial evaluation were worse. Univariate analysis demonstrated
that a younger age at the initial visit and a younger age at final evaluation were
associated with d-HCM. Catheter ablation was performed in two patients (patient 1 and 11,
Table 1) for VT and in one patient for AF
(patient 16, Table 1).
Discussion
The clinical manifestations of HCM can be categorized as those related to heart failure,
myocardial ischemia, thromboembolic stroke, palpitations, or SCD due to arrhythmia. The
pharmacological treatment of HCM is based on clinical experience and observational research
data. Beta blockers and calcium channel blockers (most commonly verapamil) are usually used
to treat symptomatic HCM patients. For HCM patients with symptoms of heart failure,
diuretics are used with caution due to potential exacerbation of left ventricular outflow
tract (LVOT) obstruction. Vasodilators such as nitroglycerin, angiotensin converting enzyme
inhibitors, and angiotensin II receptor blockers must also be used with caution in patients
with significant LVOT obstruction. Adequate medical therapy was administered to our d-HCM
patients. ICD therapy is useful for preventing SCD due to ventricular tachyarrhythmias both
for secondary prevention after cardiac arrest and primary prevention with risk factors.
Although ICDs were implanted in nine patients, CRTDs were implanted in only two patients.
The reason for the low rate of CRTD implantation was that most patients presented here did
not fulfil the standard indications of CRTD.
Some patients with HCM develop a systolic dysfunction called d-HCM that is associated with
increased morbidity and mortality. Previous studies characterized d-HCM as an LV ejection
fraction <50% at rest (reflecting global systolic dysfunction) at study entry or during
follow-up using two-dimensional echocardiography.9 However, there is no definitive definition of d-HCM, and diagnosis is
challenging. In the current study, the screening of d-HCM from an HCM registry was based on
echocardiographic reports (a formal document in our university hospital) produced by
echocardiology specialists. Previous studies have indicated that the incidence of d-HCM is
3.5–5.7%.6,9 The average time from the onset of HCM to the
diagnosis of d-HCM was 14 years, and 66% of patients progressed to death from progressive
HF, SCD, or transplantation over a mean of 2.7 years. SCD occurred at a rate of 11%/year,
and the incidence of appropriate ICD shocks was 10%/year. The predictive factors for d-HCM
are a younger age at initial visit, a family history of HCM/d-HCM/SCD, and a greater wall
thickness.6,9 Compared with dilated cardiomyopathy (DCM)
patients, d-HCM patients were more symptomatic at diagnosis; more likely to be male; more
likely to have had prior stroke, AF, and VT/VF; and had a higher mortality risk.10,11 Doi et al. reported decreases in left ventricular ejection
fraction (LVEF) and SV1+RV5 and an increase in left ventricular diastolic dysfunction during
the early phase of follow up.12 Our study
demonstrated that a younger age at the initial visit and at final evaluation, a high eGFR,
the presence of syncope, heart failure, worse echocardiographic parameters (LAD, LVDd, EF),
a wider QRS duration, and decreased RV5+SV1 were associated with the development of
d-HCM.
The exact risk of developing d-HCM from each subtype of HCM has not been clarified. In our
cohort, the initial HCM types of d-HCM patients were apical in 3, hypertrophic obstructive
cardiomyopathy (HOCM) in 2, and other HCM 13. The risk of developing d-HCM among HOCM
patients may be high but was not evaluated in this study.
Matoh et al. reported the usefulness of delayed enhancement (DE) magnetic resonance imaging
to differentiate d-HCM and DCM. The HCM patients had more DE than the DCM patients did, and
the DE volume correlated to lower global function and local LV function.13 Iida et al. examined autopsied d-HCM hearts
and found that the percentage area of myocardial fibrosis was higher than that for HCM
hearts.14 Zen et al. analyzed the
plasma levels of soluble Fas (sFas) or Fas ligand, tumor necrosis factor-alpha, and
interleukin-6 in patients with d-HCM and found that d-HCM patients with high plasma sFas
levels had a significantly higher cumulative incidence of worsening heart failure.15 Therefore, proinflammatory cytokines may play
a role in the development of d-HCM.
Because more than half of HCM patients have a family history, genetic abnormalities are
associated with HCM.5,16,17,18,19 So far,
HCM has been linked to more than 11 genes encoding proteins of contractile filament
components of the cardiac sarcomere or the adjacent X-discs.20 Mutated beta myosin heavy chain (MYH7) and
myosin-binding protein C (MYBPC3) are the most common disease-causing genes
for HCM and account for 30% of consecutively screened patients with HCM and 70% of those
genotyped patients. The most frequently affected genes in Japanese patients with familial
hypertrophic cardiomyopathy were also identified as MYBPC3 and
MYH7.20 Additionally,
in Japan, there are several reports that suggest a relationship between mutations in the
cardiac troponin T gene (TNNT2) or the cardiac troponin I gene
(TNNI3) and d-HCM.21,22,23 Kubo et
al. reported that a frameshift mutation in the MYBPC gene may contribute to
the development of d-HCM in elderly patients.8 Sato et al. reported a d-HCM patient carrying two different mutations in
MYBPC3: the Arg835Leu missense mutation and the IVS11+1G>T splicing
mutation.24 In this patient, LV
reconstruction surgery and CRT were effective for controlling repeat hospitalizations for
heart failure. Hitomi et al. identified an R945fs/105 mutation in the MYBPC
gene in six patients with HCM and DCM. They concluded that this mutation may lead to LV
systolic dysfunction and to patients suffering from cardiovascular events through mid-life
and beyond.25 In our d-HCM cohort, a
family history of SCD, HCM, and DCM was noted in one patient each. An
MYBPC3 mutation was found in patient 5 (Table 1), but genetic abnormalities were not identified in the
other patients.
Despite the poor prognosis of d-HCM described in sporadic and serial case
studies,12,26 evidence regarding the optimal treatment for
d-HCM patients is limited. Heart transplantation is the only definite therapy for
drug-resistant d-HCM.27 However, it is
difficult to perform heart transplantation in these patients because there are few heart
donors, and recipients are restricted to younger patients in Japan.
The current study had several limitations. This was a retrospective study in a single
center. The overall number of patients with d-HCM was small, which complicated the detailed
analysis to identify which parameters were predictive factors. It is possible that
abnormalities in the genes coding for sarcomeric contractile proteins might be involved in
the development of d-HCM. However, genetic screening was not performed in all patients in
the present study. A systematic study to elucidate d-HCM development, risk stratification,
and the management of d-HCM should be attempted.
Conclusion
In our HCM cohort, the incidence of d-HCM was 4%. A high prevalence of atrial fibrillation
and cerebral infarctions were noted and prognosis was poor, despite the administration of
medication and device implantation.
Acknowledgements
We are grateful to Mr. John Martin for reading this manuscript. This work was supported by
MEXT KAKENHI Grant Number 17K09524.
Conflicts of Interest
The authors have no conflicts of interest to report.
References
- 1. Maron BJ, Towbin JA, Thiene G, Antzelevitch C,
Corrado D, Arnett D, Moss AJ, Seidman CE, Young JB; American Heart Association; Council on
Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and
Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary
Working Groups; Council on Epidemiology and Prevention: Contemporary definitions and
classification of the cardiomyopathies. Circulation 2006; 113: 1807–1816. PMID:16567565,
DOI:10.1161/CIRCULATIONAHA.106.174287
- 2. Maron BJ, Maron MS: Hypertrophic cardiomyopathy.
Lancet 2013; 381: 242–255. PMID:22874472,
DOI:10.1016/S0140-6736(12)60397-3
- 3. Alcalai R, Seidman JG, Seidman CE: Genetic basis
of hypertrophic cardiomyopathy: from bench to the clinics. J Cardiovasc Electrophysiol
2008; 19: 104–110. PMID:17916152
- 4. Maron BJ, Maron MS, Semsarian C: Genetics of
hypertrophic cardiomyopathy after 20 years: clinical perspectives. J Am Coll Cardiol 2012;
60: 705–715. PMID:22796258, DOI:10.1016/j.jacc.2012.02.068
- 5. Kimura A: Molecular genetics and pathogenesis of
cardiomyopathy. J Hum Genet 2016; 61: 41–50. PMID:26178429,
DOI:10.1038/jhg.2015.83
- 6. Biagini E, Coccolo F, Ferlito M, Perugini E,
Rocchi G, Bacchi-Reggiani L, Lofiego C, Boriani G, Prandstraller D, Picchio FM, Branzi A,
Rapezzi C: Dilated-hypokinetic evolution of hypertrophic cardiomyopathy: prevalence,
incidence, risk factors, and prognostic implications in pediatric and adult patients. J Am
Coll Cardiol 2005; 46: 1543–1550. PMID:16226182,
DOI:10.1016/j.jacc.2005.04.062
- 7. Thaman R, Gimeno JR, Murphy RT, Kubo T, Sachdev
B, Mogensen J, Elliott PM, McKenna WJ: Prevalence and clinical significance of systolic
impairment in hypertrophic cardiomyopathy. Heart 2005; 91: 920–925. PMID:15958362,
DOI:10.1136/hrt.2003.031161
- 8. Kubo T, Kitaoka H, Okawa M, Matsumura Y, Hitomi
N, Yamasaki N, Furuno T, Takata J, Nishinaga M, Kimura A, Doi YL: Lifelong left
ventricular remodeling of hypertrophic cardiomyopathy caused by a founder frameshift
deletion mutation in the cardiac myosin-binding protein C gene among Japanese. J Am Coll
Cardiol 2005; 46: 1737–1743. PMID:16256878,
DOI:10.1016/j.jacc.2005.05.087
- 9. Harris KM, Spirito P, Maron MS, Zenovich AG,
Formisano F, Lesser JR, Mackey-Bojack S, Manning WJ, Udelson JE, Maron BJ: Prevalence,
clinical profile, and significance of left ventricular remodeling in the end-stage phase
of hypertrophic cardiomyopathy. Circulation 2006; 114: 216–225. PMID:16831987,
DOI:10.1161/CIRCULATIONAHA.105.583500
- 10. Hamada T, Kubo T, Kitaoka H, Hirota T, Hoshikawa
E, Hayato K, Shimizu Y, Okawa M, Yamasaki N, Matsumura Y, Yabe T, Takata J, Doi YL:
Clinical features of the dilated phase of hypertrophic cardiomyopathy in comparison with
those of dilated cardiomyopathy. Clin Cardiol 2010; 33: E24–E28. PMID:20641106,
DOI:10.1002/clc.20533
- 11. Goto D, Kinugawa S, Hamaguchi S, Sakakibara M,
Tsuchihashi-Makaya M, Yokota T, Yamada S, Yokoshiki H, Tsutsui H, JCARE-CARD
Investigators: Clinical characteristics and outcomes of dilated phase of hypertrophic
cardiomyopathy: report from the registry data in Japan. J Cardiol 2013; 61: 65–70.
PMID:23078864, DOI:10.1016/j.jjcc.2012.08.010
- 12. Doi K, Toda G, Iliev ILIEV I, Hayano M, Yano K:
Clinical analysis of hypertrophic cardiomyopathy which evolved into dilated phase during
long-term follow-up. Jpn Heart J 1999; 40: 579–587. PMID:10888378,
DOI:10.1536/jhj.40.579
- 13. Matoh F, Satoh H, Shiraki K, Saitoh T, Urushida
T, Katoh H, Takehara Y, Sakahara H, Hayashi H: Usefulness of delayed enhancement magnetic
resonance imaging to differentiate dilated phase of hypertrophic cardiomyopathy and
dilated cardiomyopathy. J Card Fail 2007; 13: 372–379. PMID:17602984,
DOI:10.1016/j.cardfail.2007.02.001
- 14. Iida K, Yutani C, Imakita M, Ishibashi-Ueda H:
Comparison of percentage area of myocardial fibrosis and disarray in patients with
classical form and dilated phase of hypertrophic cardiomyopathy. J Cardiol 1998; 32:
173–180. PMID:9783238
- 15. Zen K, Irie H, Doue T, Takamiya M, Yamano T,
Sawada T, Azuma A, Matsubara H: Analysis of circulating apoptosis mediators and
proinflammatory cytokines in patients with idiopathic hypertrophic cardiomyopathy:
comparison between nonobstructive and dilated-phase hypertrophic cardiomyopathy. Int Heart
J 2005; 46: 231–244. PMID:15876807, DOI:10.1536/ihj.46.231
- 16. Seidman JG, Seidman C: The genetic basis for
cardiomyopathy: from mutation identification to mechanistic paradigms. Cell 2001; 104:
557–567. PMID:11239412, DOI:10.1016/S0092-8674(01)00242-2
- 17. Kimura A: [Molecular pathogenesis of primary
cardiomyopathy and calcium sensitivity]. Clin Calcium 2013; 23: 551–560.
PMID:23545745
- 18. Kimura A: Molecular basis of hereditary
cardiomyopathy: abnormalities in calcium sensitivity, stretch response, stress response
and beyond. J Hum Genet 2010; 55: 81–90. PMID:20075948,
DOI:10.1038/jhg.2009.138
- 19. Kimura A. Molecular etiology and pathogenesis of
hereditary cardiomyopathy. Circ J 2008;72 Suppl A:A38-48.
- 20. Otsuka H, Arimura T, Abe T, Kawai H, Aizawa Y,
Kubo T, Kitaoka H, Nakamura H, Nakamura K, Okamoto H, Ichida F, Ayusawa M, Nunoda S, Isobe
M, Matsuzaki M, Doi YL, Fukuda K, Sasaoka T, Izumi T, Ashizawa N, Kimura A: Prevalence and
distribution of sarcomeric gene mutations in Japanese patients with familial hypertrophic
cardiomyopathy. Circ J 2012;76(2):453–61.
- 21. Fujita E, Nakanishi T, Nishizawa T, Hagiwara N,
Matsuoka R: Mutations in the cardiac troponin T gene show various prognoses in Japanese
patients with hypertrophic cardiomyopathy. Heart Vessels 2013; 28: 785–794. PMID:23494605,
DOI:10.1007/s00380-013-0332-3
- 22. Kimura A, Harada H, Park JE, Nishi H, Satoh M,
Takahashi M, Hiroi S, Sasaoka T, Ohbuchi N, Nakamura T, Koyanagi T, Hwang TH, Choo JA,
Chung KS, Hasegawa A, Nagai R, Okazaki O, Nakamura H, Matsuzaki M, Sakamoto T, Toshima H,
Koga Y, Imaizumi T, Sasazuki T: Mutations in the cardiac troponin I gene associated with
hypertrophic cardiomyopathy. Nat Genet 1997; 16: 379–382. PMID:9241277,
DOI:10.1038/ng0897-379
- 23. Kokado H, Shimizu M, Yoshio H, Ino H, Okeie K,
Emoto Y, Matsuyama T, Yamaguchi M, Yasuda T, Fujino N, Ito H, Mabuchi H: Clinical features
of hypertrophic cardiomyopathy caused by a Lys183 deletion mutation in the cardiac
troponin I gene. Circulation 2000; 102: 663–669. PMID:10931807,
DOI:10.1161/01.CIR.102.6.663
- 24. Sato A, Sakamoto N, Ando K, Kaneshiro T, Uekita
H, Sugimoto K, Yamaki T, Kunii H, Nakazato K, Suzuki H, Saitoh S, Sato M, Tamagawa K,
Arimura T, Kimura A, Takeishi Y: Dilated phase of hypertrophic cardiomyopathy caused by
two different sarcomere mutations, treated with surgical left ventricular reconstruction
and cardiac resynchronization therapy with a defibrillator. Intern Med 2012; 51:
2559–2564. PMID:22989827, DOI:10.2169/internalmedicine.51.7684
- 25. Hitomi N, Kubo T, Kitaoka H, Hirota T, Hamada T,
Hoshikawa E, Hayato K, Okawa M, Kimura A, Doi YL: A frameshift deletion mutation in the
cardiac myosin-binding protein C gene associated with dilated phase of hypertrophic
cardiomyopathy and dilated cardiomyopathy. J Cardiol 2010; 56: 189–196. PMID:20605413,
DOI:10.1016/j.jjcc.2010.04.003
- 26. Kawai M, Kihara Y, Hasegawa K, Matsumori A,
Sasayama S: Dilated phase of hypertrophic cardiomyopathy with mid-ventricular obstruction
after 20-year follow-up. Jpn Circ J 2000; 64: 623–626. PMID:10952162,
DOI:10.1253/jcj.64.623
- 27. Spirito P, Seidman CE, McKenna WJ, Maron BJ: The
management of hypertrophic cardiomyopathy. N Engl J Med 1997; 336: 775–785. PMID:9052657,
DOI:10.1056/NEJM199703133361107